Abstract
Background and Purpose
In the US, about half of acute ischemic stroke patients treated with tissue plasminogen activator (tPA) receive treatment within 60 minutes of hospital arrival. We aimed to determine the proportion of patients receiving tPA within 60 minutes (DTNT≤60) and 45 minutes (DTNT≤45) of hospital arrival by race/ethnicity and sex and to identify temporal trends in DTNT≤60 and DTNT≤45.
Methods
Among 65,654 AIS admissions in the NINDS-funded FL-PR Collaboration to Reduce Stroke Disparities (CReSD) Study from 2010–2015, we included 6,181 IV tPA-treated cases (9.4%). Generalized estimating equations were used to determine predictors of DTNT≤60 and DTNT≤45.
Results
DTNT≤60 was achieved in 42% and DTNT≤45 in 18% of cases. After adjustment, women less likely received DTNT≤60 (OR=0.81, 95% CI 0.72–0.92) and DTNT≤45 (OR=0.73 95% CI 0.57–0.93). Compared to whites, Blacks less likely had DTNT≤45 during off hours (OR= 0.68, 95% CI 0.47–0.98). Achievement of DTNT≤60 and DTNT≤45 was highest in South Florida (50%, 23%) and lowest in West Central Florida (28%, 11%).
Conclusions
In the FL-PR Collaboration to Reduce Stroke Disparities, achievement of DTNT≤60 and DTNT≤45 remains low. Compared to Whites, Blacks less likely receive tPA treatment within 45 minutes during off hours. Treatment within 60 and 45 minutes is lower in women compared to men and lowest in West Central Florida compared to other Florida regions and Puerto Rico. Further research is needed to identify reasons for delayed thrombolytic treatment in women and Blacks and factors contributing to regional disparities in DTNT.
Subject Terms: Quality and Outcomes
Keywords: door-to-needle time, ischemic stroke, thrombolysis, disparities
INTRODUCTION
Stroke is the 5th cause of death in the United States[1] and a leading cause of long-term adult disability.[2] Many advancements have been made in the treatment of acute ischemic stroke (AIS) through programs that promote evidence-based best practices. The American Heart Association/American Stroke Association (AHA/ASA) developed Get with the Guidelines-Stroke (GWTG-S), a quality improvement program that has successfully improved acute stroke care, thus reducing morbidity and mortality after stroke. The Florida-Puerto Rico Collaboration to Reduce Stroke Disparities (FL-PR CReSD) Study is a NINDS-funded multi-center initiative, specifically designed to address race, ethnic, sex and regional disparities in stroke care in a diverse population with significant Hispanic representation. The FL-PR CReSD established the FL-PR Stroke Registry, a voluntary registry of GWTG-S-participating hospitals in FL and PR, to specifically address identified disparities in acute stroke care and to develop culturally tailored, targeted interventions to reduce stroke disparities in these understudied US regions.
Rapid administration of thrombolytic therapy is a prominent aspect of quality care for AIS. Stroke morbidity and mortality are lower in patients with faster treatment times, however this benefit has not been shown to persist beyond 4.5 hours of stroke onset.[3, 4] An important component of time to treatment is door-to-needle time, or DTNT (time from hospital arrival to administration of tissue plasminogen activator [tPA]). Shorter DTNT has been associated with fewer tPA complications,[5, 6] better ambulation at discharge,[6, 7] and lower in-hospital mortality.[5, 6, 8] In 2014, the AHA/ASA initiated Target: Stroke Phase II to optimize achievement of DTNT≤60 and to introduce the new goal of DTNT≤45.[9] Nationally, about 53% of tPA-treated AIS patients receive tPA within 60 minutes of hospital arrival[8] and presumably even fewer are treated within 45 minutes. While tPA administration rates have increased over time,[10] a large proportion of patients eligible for thrombolysis are still not treated within 60 minutes of hospital arrival.
Women and race/ethnic minority groups less frequently receive tPA and other life-saving GWTG-S interventions compared to men and whites.[11–13] Furthermore, achievement of DTNT≤60 may be lower in women and Blacks.[8] Using FL-PR Stroke Registry admissions to 84 GWTG-S hospitals from January 2010 to June 2015, we assessed race/ethnic and sex disparities in achievement of DTNT≤60 and DTNT≤45 and predictors of DTNT≤60 and DTNT≤45. We also assessed regional and temporal trends in achievement of DTNT≤60 and DTNT≤45.
METHODS
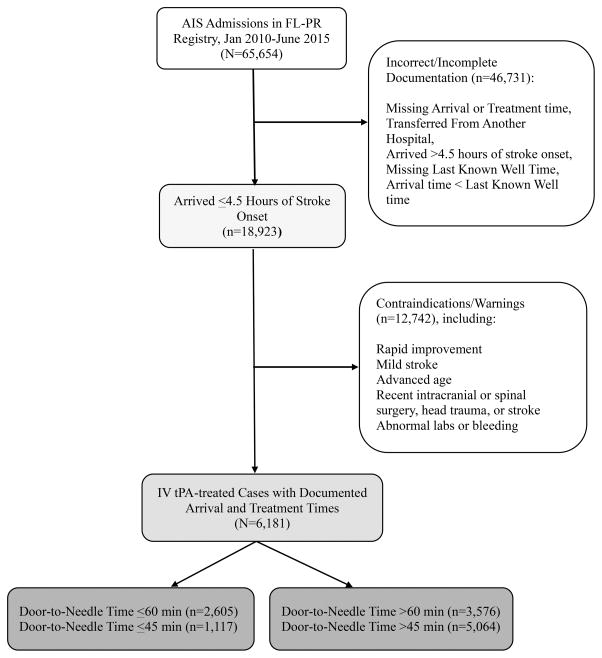
As of June 2015, the FL-PR Stroke Registry was comprised of 84 hospitals; 69 in Florida and 15 in PR. The Registry includes retrospective and prospective hospital-collected GWTG-S data on patients with a primary diagnosis of ischemic stroke, transient ischemic attack (TIA), subarachnoid hemorrhage, intracerebral hemorrhage and stroke not otherwise specified. Out of 65,654 AIS cases enrolled in the Registry from January 2010 to June 2015, records were excluded from analysis if last known well time, arrival time, or treatment time was undocumented [{Figure 1} 1]. Records were also excluded if arrival time was beyond 4.5 hours of stroke onset. Additionally, patients transferred from another hospital were excluded because treatment time could not be determined. Patients with contraindications to thrombolytic treatment were also excluded. The final study sample consisted of 6,181 tPA-treated cases. Complete data collection methods have been previously reported.[14]
Figure 1.
Derivation of the Analytic Sample
STATISTICAL ANALYSIS
DTNT was analyzed as a binary outcome: DTNT≤60 vs. DTNT>60 and DTNT≤45 vs. DTNT>45. Continuous variables were summarized as means with standard deviation (SD), or as medians with interquartile (IQR) for those with non-Normal distributions. Categorical variables were reported as frequencies with percentages. Patient groups were compared using Student’s t test for continuous variables and Pearson χ2 test for categorical variables. With generalized estimating equations (GEE) to account for within-hospital clustering, multivariable logistic regression models were used to examine disparities and factors related to DTNT≤60 (or DTNT≤45 alternatively) in a sequence of three models. Model 1 included sociodemographics: age, sex, race/ethnicity, and insurance status. Model 2 included Model 1 variables and hospital characteristics: stroke center certification, number of beds, proportion minority treated, and years in GWTG-S. Model 3 included Model 2 variables and ambulation status prior to stroke, arrival by emergency medical services (EMS), NIHSS (measure for stroke severity with increasing score indicating greater severity), EMS pre-notification, and cardiovascular risk factors: dyslipidemia, hypertension, diabetes mellitus, atrial fibrillation, smoking, coronary artery disease, peripheral vascular disease and history of stroke or transient ischemic attack (TIA). Patients were placed into one of four race/ethnic categories based on region of residence and self-identification: White, Black, FL Hispanic, and PR Hispanic. A race/ethnicity by sex interaction was tested in the fully adjusted models.
In a separate analysis, patients were stratified into 2 groups based on time of admission. Regular working hour admissions were from Monday to Friday 7:01AM to 5:59PM and off-hour admissions were anytime before 7AM or after 6PM Monday through Friday, all day Saturday, all day Sunday, and government holidays. GEE logistic regression was performed for both groups to identify predictors of DTNT≤60 and DTNT≤45 for regular and off-hour admissions. SAS v9.3 was used to perform all statistical analyses.
RESULTS
Among 65,654 AIS admissions, 6,181 (9.4%) received tPA and had documented arrival and treatment times. The sample was 52% male and 64% White, 14% Black, 14% FL Hispanic and 8% PR Hispanic, with a mean age of 71±14 years. Overall, median DTNT time was 67 (IQR 51–91) minutes. Among those with DTNT≤60 and DTNT≤45, the median was 48 and 37 minutes, respectively. Median DTNT was 68 (IQR 52–93) minutes in women and 65 (IQR 49–88) in men. FL Hispanics had the lowest median DTNT (58, IQR 43–79), followed by PR Hispanics (67, IQR 52–88), Whites (68, IQR 52–91), and Blacks (71, IQR 53–95).
DTNT≤60 was achieved in 42% of cases [Table 1] and DTNT≤45 in 18% of cases [Supplemental Table I]. Compared to men, women less often had DTNT≤60 (40% vs. 44%) and DTNT≤45 (16% vs. 20%). DTNT≤60 was greatest in FL Hispanics (56%), followed by PR Hispanics (44%), Whites (40%) and Blacks (39%). DTNT≤45 was also highest in FL Hispanics (28%), followed by Whites (17%), Blacks (14%) and PR Hispanics (14%). Patients with DTNT≤60 had more severe strokes, as measured by NIHSS 6–15 (45% vs. 42%) and NIHSS ≥16 (32% vs. 29%) and were less likely to ambulate independently prior to stroke (54% vs. 64%). They were also more likely to arrive by ambulance (82% vs. 77%) [Table 1]. After multivariate adjustment, women were less likely than men to receive DTNT≤60 (OR=0.81, 95% CI 0.72–0.92) and DTNT≤45 (OR=0.73, 95% CI 0.57–0.93) [Table 2]. Other predictors of DTNT≤60 and DTNT≤45 were no history of stroke or TIA, no history of CAD or MI, NIHSS >5, arrival by ambulance and treatment at a comprehensive stroke center [Supplement Table II].
Table 1.
Characteristics of IV tPA-treated Acute Ischemic Stroke Cases with Door-to-Needle time ≤60 minutes and Door-to-needle >60 minutes in the FL-PR Stroke Registry, 2010–2015
| DTNT ≤ 60 min (N=2605, 42%) | DTNT > 60 min (N=3576, 58%) | p | |
|---|---|---|---|
| Age (yrs), mean ± SD | 70.7 ± 8.2 | 70.7 ± 8.5 | |
| Women, n (%) | 1187 (46) | 1791 (50) | <.0001 |
| Race-ethnicity, n (%) | |||
| White | 1568 (60) | 2382 (67) | <.0001 |
| Black | 332 (13) | 530 (15) | |
| FL Hispanic | 499 (19) | 400 (11) | |
| PR Hispanic | 206 (8) | 264 (7) | |
| Region, n (%) | |||
| South FL | 1251 (48) | 1264 (35) | <.0001 |
| West Central FL | 334 (13) | 852 (24) | |
| East Central FL | 398 (15) | 588 (16) | |
| North & Panhandle | 416 (16) | 608 (17) | |
| Puerto Rico | 206 (8) | 264 (7) | |
| Vascular Risk Factor, n (%) | |||
| Hypertension | 1539 (59) | 2403 (67) | <.0001 |
| Diabetes mellitus | 538 (21) | 859 (24) | .002 |
| Medical History, n (%) | |||
| AF | 566 (22) | 795 (22) | 0.64 |
| CAD/prior MI | 496 (19) | 871 (24) | <.0001 |
| Previous stroke/TIA | 425 (16) | 806 (23) | <.0001 |
| NIHSS, n (%) | |||
| ≤5 | 512 (20) | 803 (22) | <.0001 |
| 6–15 | 1160 (45) | 1498 (42) | |
| ≥16 | 830 (32) | 1030 (29) | |
| Missing | 103 (4) | 245 (7) | |
| Arrival Mode, n (%) | |||
| EMS | 2144 (82) | 2736 (77) | <.0001 |
| Not by EMS | 222 (9) | 501 (14) | |
| Missing/Unknown | 239 (9) | 339 (9) | |
| Ambulation Status*, n (%) | |||
| Independent | 1410 (54) | 2280 (64) | <.0001 |
| With Assistance | 84 (3) | 163 (4) | |
| Missing/ND | 1111 (43) | 1133 (32) | |
| Hospital size, n (%) | |||
| Small (<250 beds) | 337 (13) | 560 (15) | .003 |
| Mid (≥250–450 beds) | 797 (31) | 992 (28) | |
| Large (>450 beds) | 1471 (56) | 2024 (57) | |
| Years in GWTG-S, mean±SD | 8.2 + 2.2 | 8.5 + 2.5 |
AF= Atrial fibrillation, CAD/MI=Coronary artery disease, MI=myocardial infarction, TIA=transient ischemic attack, NIHSS=National Institute of Health Stroke Scale, EMS=emergency medical services,
Ambulation prior to stroke
Table 2.
Door-to-Needle Time ≤60 minutes and Door-to-Needle Time ≤45 minutes by Sex and Race/ethnicity
| DTNT≤60 vs. DTNT>60 | DTNT≤45 vs. DTNT<45 | |||
|---|---|---|---|---|
| aOR1 (95% CI) | aOR2 (95% CI) | aOR3 (95% CI) | aOR3 | |
| Sex | ||||
| F (vs. M) | 0.82 (0.72–0.93) | 0.82 (0.72–0.93) | 0.81 (0.72–0.92) | 0.73 (0.57–0.93) |
| Race/ethnicity | ||||
| (ref: FL-W) | ||||
| FL-B | 0.89 (0.75–1.06) | 0.89 (0.75–1.04) | 0.88 (0.74–1.04) | 0.79 (0.59–1.05) |
| FL-H | 1.16 (0.91–1.47) | 1.15 (0.90–1.46) | 1.14 (0.92–1.41) | 0.94 (0.71–1.23) |
| PR-H | 1.06 (0.69–1.63) | 0.79 (0.44–1.40) | 0.76 (0.42–1.39) | 0.45 (0.17–1.22) |
aOR1: Model 1 adjusts for age, sex, race/ethnicity, and insurance status.
aOR2: Model 2 includes Model 1 + hospital academic status, number of beds, years in GWTG-S, and proportion minority treated.
aOR3: Model 3 includes Model 2 + smoking status, hypertension, diabetes mellitus, dyslipidemia, atrial fibrillation, coronary artery disease, peripheral vascular disease, history of stroke or TIA, ambulation status prior to stroke, NIHSS, arrival mode, EMS prenotification and stroke center certification.
After stratification by admission time, women less likely than men received DTNT≤60 during working hour- (OR=0.81, 95% CI 0.70–0.94) and off-hour admissions (OR=0.81, 95% CI 0.68–0.96). DTNT≤45 was less likely among women compared to men (OR=0.72, 95% CI 0.58–0.90) during working hours and less likely among Blacks compared to whites during off hours (OR=0.68, 95% CI 0.47–0.98) [Table 3]. There was no significant race/ethnicity*sex interaction for DTNT≤60 or DTNT≤45.
Table 3.
DTNT≤60 and DTNT≤45 during Working Hour- and Off Hour Admissions by Sex and Race/ethnicity
| DTN≤60 | DTN≤45 | |
|---|---|---|
| aOR (95% CI) | aOR (95% CI) | |
| WORKING HOURS | ||
| Sex | ||
| F v M | 0.81 (0.70–0.94) | 0.72 (0.58–0.90) |
| Race/Ethnicity | ||
| FL-B v FL-W | 0.99 (0.74–1.34) | 0.91 (0.64–1.30) |
| FL-H v FL-W | 1.17 (0.87–1.57) | 1.14 (0.84–1.56) |
| PR-H v FL-W | 0.93 (0.46–1.87) | 0.50 (0.17–1.45) |
| OFF HOURS | ||
| Sex | ||
| F v M | 0.81 (0.68–0.96) | 0.74 (0.52–1.05) |
| Race/Ethnicity | ||
| FL-B v FL-W | 0.79 (0.63–1.04) | 0.68 (0.47–0.98) |
| FL-H v FL-W | 1.17 (0.89–1.54) | 0.84 (0.58–1.24) |
| PR-H v FL-W | 0.60 (0.30–1.22) | 0.57 (0.19–1.65) |
Off hours=Monday through Friday 6PM to 7AM, Saturdays, Sundays, and government holidays.
Fully adjusted model for DTN<60 and DTN<45 includes age, race/ethnicity, sex, insurance status, hospital academic status, number of beds, years in GWTG-S, proportion minority treated, arrival mode, EMS prenotification, ambulation status prior to stroke, smoking status, history of stroke, coronary artery disease, diabetes mellitus, hypertension, dyslipidemia, and atrial fibrillation.
Achievement of DTNT≤60 and DTNT≤45 was highest in South Florida (50% and 23%, respectively) and lowest in West Central Florida (28% and 11%, respectively). There was a rise in achievement of DTNT≤60 and DTNT≤45 from 2010 to 2015. Temporal trends in DTNT by race/ethnicity, sex, and region are detailed in Supplemental Tables III and IV and Supplemental Figures I through VI.
DISCUSSION
In our FL-PR Stroke Registry, achievement of Door to Needle Time (DTNT) remains low. DTNT≤60 was achieved in 42% cases and DTNT≤45 in only 18% of cases. We also observed some race-ethnic and prominent sex disparities in DTNT. Blacks were less likely treated within 45 minutes during off hours. Women were less likely treated within 60 minutes regardless of admission time and also less likely treated within 45 minutes during working hours. We have also identified significant regional variation in DTNT. West Central FL had the lowest proportion of patients treated with DTNT≤60 and DTNT≤45. Our results add novel data to the literature on race/ethnic, sex, and regional disparities in DTNT.
We identified individual-level factors associated with DTNT≤60 and DTNT≤45 such as no history of prior stroke or coronary artery disease. These findings emphasize the importance of stroke and cardiovascular disease prevention. We also identified ambulance transport to the hospital and treatment in larger hospitals and comprehensive stroke centers as predictors of receiving tPA within 60 and 45 minutes. Achievement of goal DTNT may be enhanced by improving systems of care that include greater utilization of EMS and better implementation of EMS pre-notification.
Longer DTNT has been previously reported in women[6, 15] and Blacks[8] and may be due to delays at the time of admission. The stroke team was unable to determine tPA eligibility in 12.1% of Blacks compared to 9.7% of whites. Additionally, uncontrolled hypertension requiring aggressive control with IV medications was reported in 10% of Blacks compared to 5.5% of Whites. Delayed treatment in FL Hispanics may have been due to initial refusal of tPA, which was greatest among FL Hispanics (5.1% compared to 3.9% in FL Whites, 3.0% in FL Blacks, and 1.9% in PR Hispanics). These were noted as reasons for treatment delay beyond 60 minutes but likely contribute to delays beyond 45 minutes as well. Documented reasons for treatment delay were similar between men and women and likely did not account for sex disparities in DTNT in our study. However, women were more likely than men to present with altered consciousness (16% vs. 13%), which may have prolonged stroke diagnosis and treatment. In addition, the sex disparity in the present study was observed across all race/ethnic groups and most likely contributed to sex-specific differences in biological and sociocultural factors not investigated in our study.
Information gathering at time of admission may also affect time to treatment. Family members and caretakers, if present at the time of stroke onset, EMS arrival, and hospital admission, may provide patient medical histories and act as patient advocates, potentially leading to faster treatment. Also, the presence of stroke specialists and neurologists in the emergency department at admission and treatment by an attending physician may also contribute to faster DTNT. Currently, the FL-PR Registry does not contain data about information gathering at the time of admission, physicians present in the emergency department at the time of admission, or type of physicians that provided direct care (residents, attending physicians etc.). This data may highlight additional sources of treatment delays and should be collected in future projects.
Previous studies have identified similar patient-level characteristics related to timely treatment, including no prior history of stroke[6, 8] and greater stroke severity.[6, 15] In our study, a larger proportion of women and Blacks had NIHSS greater than 5, however stroke severity did not fully account for differences in DTNT<60 and DTNT<45. EMS arrival was associated with greater likelihood of DTNT≤60 in the present study and studies of national GWTG-S data.[6, 16] Despite women arriving by ambulance more often, DTNT≤60 was still less common in women. Lower use of EMS in Blacks also did not fully account for longer DTNT. Race/ethnic and sex disparities were still present after adjustment for EMS pre-notification. By-pass policy[17] is another possible mediator of sex and race/ethnic differences in DTNT and should be explored in future studies.
Stroke center type was an important hospital-level predictor of DTNT. Patients treated at comprehensive stroke centers were twice as likely to be treated within 60 minutes compared to those treated at primary stroke centers. The additional resources of comprehensive stroke centers, which include 24/7 availability of personnel and imaging facilities, availability of advanced imaging techniques, and expertise in treating large ischemic strokes, facilitate faster treatment in ischemic stroke.[18] DTNT≤60 was also more common in patients treated at larger hospitals. Hospitals with greater ischemic stroke admissions per year and greater volume of IV tPA treated patients per year[6, 8, 19] are more likely to treat within 60 minutes. Previous studies reported that hospitals that treat larger proportions of Black patients have better tPA administration rates for Blacks.[20–22] In our study, the race/ethnic disparity in DTNT≤45 during off hours persisted even after adjustment for proportion minority treated, stroke center certification and other hospital characteristics, which support our conclusion that admission factors likely account for delayed treatment in Blacks.
Multiple hospital-based initiatives have been implemented to improve processes of care and shorten time to treatment. Target: Stroke, a national quality improvement program, emphasizes 11 key best practice strategies to improve DTNT, including hospital pre-notification by EMS, rapid triage and stroke team notification, and rapid acquisition and interpretation of CT scans.[8, 23] Door to CT time is an understudied hospital process of care that directly affects DTNT. Currently, the Registry does not contain data on time of generation or interpretation of CT results or data regarding which physician (ED physician or neurologist) interpreted the CT scan, however these factors are important determinants of DTNT and should be examined in future studies.
The FL-PR CReSD has delivered two tools to hospitals in the Registry to improve acute stroke care—the hospital-specific Disparities Dashboards and the interactive Door to Needle educational module. The Disparities Dashboards allow hospitals to benchmark their adherence to GWTG-S metrics, door to needle time, and door to CT time and compare their performance to other hospitals in the region and state. The Door to Needle module is an interactive, web-based tool designed for emergency medical personnel, stroke neurologists, and emergency department physicians which emphasizes evidence-based, best practices to shorten door to needle time. The effect of the Dashboards and the Door to Needle module on DTNT has not yet been evaluated; therefore, DTNT improvements cannot be directly attributed to these interventions. Improvements in stroke care from 2010–2015 observed in our study are likely due to participation in the GWTG-S quality improvement program by increasing adherence to stroke performance measures as previously reported.[24]
There was substantial regional variation in DTNT, which may be partly due to regional variation in stroke mortality rates, concentration of neurologists, and hospital characteristics. In Florida, counties with the highest age-adjusted stroke morality rates and the lowest concentration of neurologists are located in North Florida and the Panhandle region.[25] In contrast, the highest concentrations of primary stroke centers, comprehensive stroke centers, academic institutions and neurologists are in the southern and central regions of Florida. Also, large hospitals (bed size ≥ 450) that have participated in GWTG-S ≥ 6 years are predominantly in southern and central Florida compared to the North and Panhandle.[26] Hospital size and time in the GWTG-S were not significant predictors of DTNT≤60 or DTNT≤45 in our study, but it has been shown that time in GWTG-S is associated with greater achievement GWTG-S predefined stroke performance measures, particularly in larger, teaching hospitals.[24] These factors do not fully explain low achievement of DTNT≤60 and DTNT≤45 in West Central FL. Future analysis of the hospital Disparities Dashboard data will clarify causes of regional disparities in DTNT.
The FL-PR Stroke Registry is an ongoing, growing registry, which supports the study of delivery of evidence-based best practices, identification of disparities, and development of future interventions to reduce disparities in acute stroke care. Data is systematically collected in the harmonized GWTG-S data entry system. In our future studies we plan to evaluate the effect of the Disparities Dashboards and Door to Needle Module interventions on adherence to stroke care measures in a clinical trial design. Current results will inform the development of broader hospital and community based-educational interventions to address disparities in stroke care.
Some limitations of the study should be noted. We were unable to assess the impact of many key best practice strategies for DTNT improvement (e.g., pre-mixing of tPA, time to generation of CT scan results) and sociocultural factors (e.g., whether patient lives alone) that are not included in our data collection. Also, we were unable to determine whether ER physicians or neurologists were the initial treating physicians because the registry does not contain this data. Our future interventions aim to extend data collection methods to include implementation of best practice strategies, use of the Disparities Dashboards and Door to Needle educational module, information on initial treating physicians, and sociocultural factors as these factors may explain some of the observed disparities in DTNT. Furthermore, the longitudinal effects of sex and race/ethnic differences in DTNT on long-term stroke outcomes including mortality, disability, and quality of life should be studied. Our goal for the second phase of the FL-PR Stroke Registry is to improve transition of care after discharge from acute stroke hospitalizations and reduce disparities in transition of stroke care. We also plan to develop, deliver and disseminate educational interventions that will affect post-discharge systems of care and long-term stroke outcomes in our Registry.
Supplementary Material
Acknowledgments
SOURCES OF FUNDING
The Florida Puerto Rico Collaboration to Reduce Stroke Disparities Study is supported by the National Institute of Health (NIH)/National Institute of Neurological Disorders (NINDS) and Stroke Prevention and Intervention Research Program (SPIRP) cooperative grant (grant number: U54NS081763). The women’s supplement is awarded from the Office of Research on Women’s Health (Grant Number: 3U54NS081763-01S1).
Footnotes
DISCLOSURES
Dr. Sacco is the recipient and the primary investigator of the SPIRP cooperative grant from the National Institute of Health (NIH)/ National Institute of Neurological Disorders (NINDs; Grant Number: U54NS081763). Dr Rundek receives research salary support from the SPIRP cooperative grant from the NIH/NINDS (grant number: U54NS081763) and the women’s supplement from the NIH, Office of Research on Women’s Health (grant number: 3U54NS081763-01S1). Dr Romano receives research salary support from the SPIRP cooperative grant from the NIH/NINDS (grant number: U54NS081763). Dr Koch receives research salary support from the SPIRP cooperative grant from the NIH/NINDS (grant number: U54NS081763). Dr. Waddy is the NIH scientific officer of the SPIRP program. The other authors report no conflicts.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016;133:e38–60. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 2.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 3.Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317–29. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]
- 4.Saver JL. Time is brain--quantified. Stroke. 2006;37:263–6. doi: 10.1161/01.STR.0000196957.55928.ab. [DOI] [PubMed] [Google Scholar]
- 5.Fonarow GC, Zhao X, Smith EE, Saver JL, Reeves MJ, Bhatt DL, et al. Door-to-needle times for tissue plasminogen activator administration and clinical outcomes in acute ischemic stroke before and after a quality improvement initiative. JAMA. 2014;311:1632–40. doi: 10.1001/jama.2014.3203. [DOI] [PubMed] [Google Scholar]
- 6.Saver JL, Fonarow GC, Smith EE, Reeves MJ, Grau-Sepulveda MV, Pan W, et al. Time to treatment with intravenous tissue plasminogen activator and outcome from acute ischemic stroke. JAMA. 2013;309:2480–8. doi: 10.1001/jama.2013.6959. [DOI] [PubMed] [Google Scholar]
- 7.Ido MS, Okosun IS, Bayakly R, Clarkson L, Lugtu J, Floyd S, et al. Door to Intravenous Tissue Plasminogen Activator Time and Hospital Length of Stay in Acute Ischemic Stroke Patients, Georgia, 2007–2013. J Stroke Cerebrovasc Dis. 2016;25:866–71. doi: 10.1016/j.jstrokecerebrovasdis.2015.12.025. [DOI] [PubMed] [Google Scholar]
- 8.Fonarow GC, Smith EE, Saver JL, Reeves MJ, Bhatt DL, Grau-Sepulveda MV, et al. Timeliness of tissue-type plasminogen activator therapy in acute ischemic stroke: patient characteristics, hospital factors, and outcomes associated with door-to-needle times within 60 minutes. Circulation. 2011;123:750–8. doi: 10.1161/CIRCULATIONAHA.110.974675. [DOI] [PubMed] [Google Scholar]
- 9.Target: Stroke Honor Roll - Recognition for Your Success. [Accessed March 18, 2016];The American Heart Association website. http://www.strokeassociation.org/STROKEORG/Professionals/TargetStroke/Target-Stroke-Honor-Roll---Recognition-For-Your-Success_UCM_432416_Article.jsp#.WNQYQIWcHIV.
- 10.Schwamm LH, Ali SF, Reeves MJ, Smith EE, Saver JL, Messe S, et al. Temporal trends in patient characteristics and treatment with intravenous thrombolysis among acute ischemic stroke patients at Get With The Guidelines-Stroke hospitals. Circ Cardiovasc Qual Outcomes. 2013;6:543–9. doi: 10.1161/CIRCOUTCOMES.111.000303. [DOI] [PubMed] [Google Scholar]
- 11.Reeves MJ, Fonarow GC, Zhao X, Smith EE, Schwamm LH. Quality of care in women with ischemic stroke in the GWTG program. Stroke. 2009;40:1127–33. doi: 10.1161/STROKEAHA.108.543157. [DOI] [PubMed] [Google Scholar]
- 12.Smith DB, Murphy P, Santos P, Philips M, Wilde M. Gender differences in the Colorado Stroke Registry. Stroke. 2009;40:1078–81. doi: 10.1161/STROKEAHA.108.541730. [DOI] [PubMed] [Google Scholar]
- 13.Schwamm LH, Reeves MJ, Pan W, Smith EE, Frankel MR, Olson D, et al. Race/ethnicity, quality of care, and outcomes in ischemic stroke. Circulation. 2010;121:1492–501. doi: 10.1161/CIRCULATIONAHA.109.881490. [DOI] [PubMed] [Google Scholar]
- 14.Asdaghi N, Romano JG, Wang K, Ciliberti-Vargas M, Koch S, Gardener H, et al. Sex Disparities in Ischemic Stroke Care: FL-PR CReSD Study (Florida-Puerto Rico Collaboration to Reduce Stroke Disparities) Stroke. 2016;47:2618–26. doi: 10.1161/STROKEAHA.116.013059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Strbian D, Ahmed N, Wahlgren N, Lees KR, Toni D, Roffe C, et al. Trends in Door-to-Thrombolysis Time in the Safe Implementation of Stroke Thrombolysis Registry: Effect of Center Volume and Duration of Registry Membership. Stroke. 2015;46:1275–80. doi: 10.1161/STROKEAHA.114.007170. [DOI] [PubMed] [Google Scholar]
- 16.Ekundayo OJ, Saver JL, Fonarow GC, Schwamm LH, Xian Y, Zhao X, et al. Patterns of emergency medical services use and its association with timely stroke treatment: findings from Get With the Guidelines-Stroke. Circ Cardiovasc Qual Outcomes. 2013;6:262–9. doi: 10.1161/CIRCOUTCOMES.113.000089. [DOI] [PubMed] [Google Scholar]
- 17.Higashida R, Alberts MJ, Alexander DN, Crocco TJ, Demaerschalk BM, Derdeyn CP, et al. Interactions within stroke systems of care: a policy statement from the American Heart Association/American Stroke Association. Stroke. 2013;44:2961–84. doi: 10.1161/STR.0b013e3182a6d2b2. [DOI] [PubMed] [Google Scholar]
- 18.Comprehensive Stroke Center Certification. [Accessed on September 12, 2016];The American Heart Association website. https://www.heart.org/HEARTORG/Professional/HospitalAccreditationCertification/ComprehensiveStrokeCenterCertification/Comprehensive-Stroke-Center-Certification_UCM_455446_SubHomePage.jsp.
- 19.Groot AE, van Schaik IN, Visser MC, Nederkoorn PJ, Limburg M, Aramideh M, et al. Association between i.v. thrombolysis volume and door-to-needle times in acute ischemic stroke. J Neurol. 2016;263:807–13. doi: 10.1007/s00415-016-8076-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hsia AW, Edwards DF, Morgenstern LB, Wing JJ, Brown NC, Coles R, et al. Racial disparities in tissue plasminogen activator treatment rate for stroke: a population-based study. Stroke. 2011;42:2217–21. doi: 10.1161/STROKEAHA.111.613828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johnston SC, Fung LH, Gillum LA, Smith WS, Brass LM, Lichtman JH, et al. Utilization of intravenous tissue-type plasminogen activator for ischemic stroke at academic medical centers: the influence of ethnicity. Stroke. 2001;32:1061–8. doi: 10.1161/01.str.32.5.1061. [DOI] [PubMed] [Google Scholar]
- 22.Jacobs BS, Birbeck G, Mullard AJ, Hickenbottom S, Kothari R, Roberts S, et al. Quality of hospital care in African American and white patients with ischemic stroke and TIA. Neurology. 2006;66:809–14. doi: 10.1212/01.wnl.0000203335.45804.72. [DOI] [PubMed] [Google Scholar]
- 23.American Heart Association; Clinical Resources and Tools. [Accessed March 7, 2017];Target: Stroke Phase II Manual, 11 Key Best Practice Strategies. 2014 https://www.heart.org/idc/groups/heart-public/@wcm/@mwa/documents/downloadable/ucm_486394.pdf.
- 24.Schwamm LH, Fonarow GC, Reeves MJ, Pan W, Frankel MR, Smith EE, et al. Get With the Guidelines-Stroke is associated with sustained improvement in care for patients hospitalized with acute stroke or transient ischemic attack. Circulation. 2009;119:107–15. doi: 10.1161/CIRCULATIONAHA.108.783688. [DOI] [PubMed] [Google Scholar]
- 25.Florida CHARTS: Community Health Assessment Resource Tool Set; Chronic Diseases; Stroke. [Accessed March 7, 2017];Florida Department of Health website. http://www.flhealthcharts.com/charts/ChronicDiseases/Default.aspx.
- 26.Ciliberti-Vargas MC, Gardener H, Wang K. Stroke Hospital Characteristics in the Florida-Puerto Rico Collaboration to Reduce Stroke Disparities (FL-PR CReSD) Study. South Med J. 2017 doi: 10.14423/SMJ.0000000000000667. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.