Summary
Background
Haiti has an integrated bite case management (IBCM) programme to counsel animal-bite victims on the risk of rabies and appropriate treatment, as well as the Haiti Animal Rabies Surveillance Program (HARSP) to examine the animals. We assessed the usefulness of the IBCM programme to promote best practices for rabies prophylaxis after exposure in a low-income rabies-endemic setting.
Methods
We did a retrospective follow-up survey of randomly selected bite victims who were counselled by Haiti's IBCM programme between May 15, 2014, and Sept 15, 2015. We classified participants by HARSP decisions of confirmed, probable, suspected, or non-rabies exposures. We compared health-care outcomes in people who sought medical care before IBCM counselling with those in people who sought care after counselling. We used decision trees to estimate the probability of actions taken in the health-care system, and thereby human deaths.
Findings
During the study period, 1478 dog bites were reported to HARSP for assessment. 37 (3%) were confirmed exposures, 76 (5%) probable exposures, 189 (13%) suspected exposures, and 1176 (80%) non-rabies exposures. 115 of these cases were followed up in the survey. IBCM counselling was associated with a 1.2 times increase in frequency of bite victims seeking medical care and of 2.4 times increase in vaccination uptake. We estimated that there would be four human rabies deaths among the 1478 people assessed by IBCM during the survey period, and 11 in the absence of this programme, which would equate to a 65% decrease in rabies deaths. Among three people dead at the time of the follow-up survey, one was deemed to be due to rabies after a probable rabies exposure.
Interpretation
Adherence to medical providers' recommendations might be improved through counselling provided by IBCM programmes.
Introduction
Rabies is the cause of around 59 000 deaths per year worldwide, and mortality is almost 100%.1,2 Numerous terrestrial carnivores (globally) and bat species (in the western hemisphere) are reservoirs for the rabies virus, but most human deaths are due to the rabies virus variant enzootic in domesticated dogs.3 Primary rabies interventions focus on controlling the disease in the reservoir host through vaccination, population management, and responsible ownership.4,5
Dog vaccination and other primary intervention techniques have been immensely successful in the western hemisphere, where reported canine-mediated human rabies deaths dropped from more than 300 in the 1980s to ten in 2013.6,7 These gains, however, have not been distributed evenly throughout all countries. Haiti, Guatemala, and Bolivia continue to report dog-mediated human rabies deaths.6,7 Building capacity for dog vaccination programmes capable of reaching more than 70% of the population, as recommended by the World Organisation for Animal Health, can be difficult in low-income countries.3,8 Development of the veterinary infrastructure and political support for effective mass vaccination campaigns can take years to accomplish. Additionally, effective vaccination levels must be maintained for 3–7 years to achieve elimination.3
For countries with high human rabies burdens, ignoring deaths associated with dog bites while effective canine vaccination programmes are being developed is unreasonable. Secondary interventions, such as postexposure prophylaxis, must be incorporated into rabies control strategies. WHO recommends that prophylaxis should be started immediately for any person suspected to have been exposed to the rabies virus (panel 1),3 and discontinued if rabies is ruled out through diagnostic testing or observational findings (ie, the animal passes a 10-day quarantine period). Many countries do not have qualified medical professionals to implement these recommendations, the laboratory capacity to make timely diagnoses, or the veterinary workforce to reliably assess animals suspected of having rabies.9 These issues might lead to a high demand for and overadministration of rabies vaccines, resulting in vaccine shortages. Improved use of human rabies vaccines and increased bite surveillance have been achieved through the development of integrated bite case management (IBCM) programmes that link the public health and veterinary sectors and enable collaboration in the investigation of suspected rabies exposures.10,11
Haiti has the highest burden of human rabies deaths in the western hemisphere, with 130 per year.1 An IBCM programme was introduced in Haiti in 2013 to formally link the human health sector to the Haiti Animal Rabies Surveillance Program (HARSP) and improve communication of rabies assessments in dogs to bite victims and their medical providers.10 All animal bites are notifiable to HARSP, but less than 15% of health-care professionals are trained in rabies prevention, and 77% do not know where to refer bite victims for rabies vaccination.12 Where reporting linkages have been established, the IBCM programme notifies HARSP of bite events. Although the intention is that HARSP would investigate all bite notifications and all animals with suspected rabies in regions where it is operational, roughly 76% of the bites seen in health-care facilities are investigated (unpublished national surveillance data). The incomplete investigation is thought to reflect non-uniform hospital participation rather than prioritisation of animals with suspected rabies. After implementation of the IBCM programme, Haiti reported an 18 times increase in the detection of rabid animals and 30% increase in the identification of bite victims.10 However, HARSP data collection focuses on the biting animals and does not routinely include information on the health-care-seeking behaviours of the bite victims. We did a follow-up survey to assess the health-care-seeking behaviours of individuals who had received IBCM counselling after receiving dog bites (ie, risk assessment, wound washing, and referral to a treatment facility) to investigate the usefulness of this programme in promoting best practices for administration of postexposure prophylaxis as a component of rabies control in a low-income country.
Methods
Study population
We did a retrospective follow-up survey among dog-bite victims living in the Artibonite, Centre, and Ouest departments of Haiti, who had been investigated by the national IBCM programme between May 15, 2014, and Sept 15, 2015. Bite victims were stratified into four rabies exposure categories based on the HARSP rabies status definitions for biting dogs: confirmed, probable, suspected, and non-rabies (panel 1).10 Respondents were randomly selected from the HARSP database with Microsoft Excel 2015 random number generator.
Survey
From Oct 15 to Dec 15, 2015, the national coordinator for HARSP contacted selected participants by telephone. People not reached after three telephone calls were visited in person by a Ministry of Agriculture, Natural Resources, and Rural Development animal rabies investigator. If a selected respondent was younger than 15 years or unavailable because they had died, the head of the household was asked to complete the survey as a proxy. Respondents were asked 12 semistructured interview questions in Creole. Details of health-care-seeking behaviour before IBCM counselling were obtained from the HARSP national database (appendix). Patients deceased at the time of the survey were classified as having had rabies.
Statistical analysis
We calculated the sample sizes for the exposure strata on the basis of the expected rate of non-adherence to HARSP recommendations (10%), precision (10%), and design effect (1.0).10 We aimed to include 20 people with confirmed rabies exposures (ie, animal positive on direct fluorescent antibody testing), 20 with probable rabies exposures, 30 with suspected rabies exposures, and 50 people with non-rabies exposures.
We used univariate analysis to assess demographic characteristics, patients' health-care-seeking behaviours, and treatment recommendations. Where indicated, we assessed differences between groups with the Cochran-Mantel-Haenszel test of significance.
Many bite notifications are made to HARSP through hospital-based reporting, but community members may contact the programme directly, and field investigations provide a further route of notifications. As a result, the timepoint at which the IBCM programme can affect health-care-seeking behaviours might differ by how bite victims are identified. Therefore, we assessed separately people who sought medical care before and after IBCM counselling.
We developed decision trees to estimate the probability of actions taken in the health-care system by people who received IBCM counselling. We calculated probability of seeking medical care, probability that vaccination was recommended, probability that vaccination was started, and probability that the vaccination series was completed (at least four doses). We assigned a decision tree to each exposure category that incorporated weighting for frequency of exposure type in the total population eligible for selection (n=1478) to calculate overall population-adjusted outputs.
Haiti adheres to the WHO recommendation of a series of five intramuscular doses of vaccine that should be discontinued if rabies is ruled out in the biting animal.3 Based on this guidance, the correct course of action within the decision tree algorithm is that all bite victims seek medical care, vaccination is recommended and started, and the vaccine series is completed if rabies is confirmed, probable, or suspected or is discontinued if a non-rabies status is reported. People in this study who sought care and started vaccination before receiving IBCM counselling were taken to represent health-care outcomes in the absence of the IBCM programme. This population is not reflective of a truly IBCM-naive population because people still received counselling and the biting animals were investigated, but the decisions to seek medical assessments and take the vaccine were made without IBCM involvement. The rate ratio, rate difference, and the 95% CIs for the rate difference were calculated with the Byar method,13 and adjustments were made for population differences.
The numbers of deaths with and without IBCM counselling were estimated based on the decision-tree probabilities with the addition of the probability of the biting dog having rabies and the probability of a person succumbing to rabies. By exposure category, the probability of the biting dog having rabies was fx=1.0 for confirmed, fx=0.5 for probable, fx=0.12 for suspected, and non-rabies fx=0.0, where fx means the given probability distribution function. By treatment status, the probability of succumbing to rabies was completed treatment fx=0.0, discontinued treatment fx=0.05, and treatment not started fx=0.17.14,15 The probabilities for the probable and suspected rabies exposure categories and the discontinued treatment category are informed values, but accuracy cannot be validated because no previous publications have described these rates.
We took p values less than 0.05 to be significant. All analyses were done with OpenEpi version 3.01.
Role of the funding source
There was no funding source for this study. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
During the study period, 1957 bites were reported to the IBCM in the three eligible departments, of which 1478 (76%) were reported to HARSP for animal investigation. 37 dogs (3%) had confirmed rabies, 76 (5%) had probable rabies, 189 (13%) had suspected rabies, and rabies was ruled out in 1176 (80%). From these bite victims, 120 eligible people were selected for the survey, which was completed by 115 respondents (96%, figure 1, table 1; five victims or close relatives could not be contacted). Three people selected to complete the survey were dead at the time of follow-up, among whom one had a history compatible with the WHO case definition for probable rabies, one had suspected rabies, and one had non-rabies illness (panel 2).
Figure 1. Map of animal bite victims by type of rabies exposure and study area.
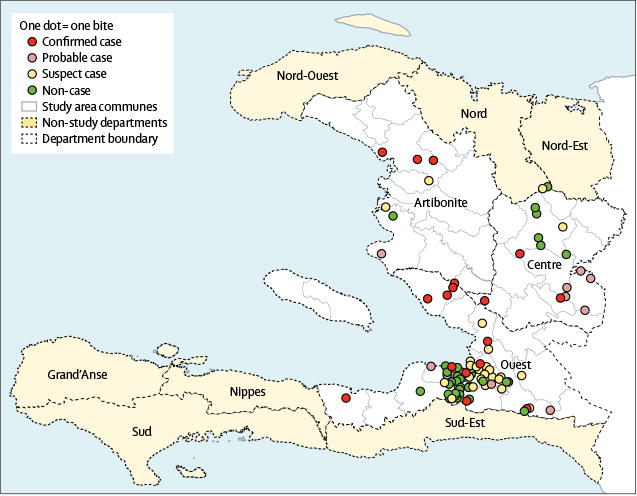
Table 1. Characteristics of bite victims who received counselling by an IBCM programme.
| Rabies case classification of dogs | Total population (n=115) | p value | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| Confirmed (n=18) | Probable (n=21) | Suspected (n=29) | Non-case (n=47) | |||
| Demographics | ||||||
|
| ||||||
| Men | 15 (83%) | 14 (67%) | 14 (48%) | 23 (49%) | 66 (57%) | 0.04 |
| Age (years) | 33 (3–87) | 29 (0–72) | 32 (5–80) | 25 (1–70) | 29 (0–87) | .. |
|
| ||||||
| Department of residence | ||||||
|
| ||||||
| Artibonite | 3 (17%) | 2 (10%) | 1 (3%) | 1 (2%) | 7 (6%) | 0.16 |
| Centre | 3 (17%) | 5 (24%) | 2 (7%) | 6 (13%) | 16 (14%) | |
| Ouest | 12 (67%) | 14 (67%) | 26 (90%) | 40 (85%) | 92 (80%) | |
|
| ||||||
| Health-care-seeking behaviours | ||||||
|
| ||||||
| Traditional healer | 2 (11%) | 3 (14) | 2 (7%) | 8 (17%) | 15 (13%) | 0.63 |
| Sought medical care before IBCM counselling | 8 (44%) | 9 (43%) | 26 (90%) | 39 (83%) | 82 (71%) | <0.0001 |
| Vaccination | ||||||
| Recommended before IBCM counselling | 4 (22%) | 8 (38%) | 14 (48%) | 14 (30%) | 40 (35%) | 0.24 |
| Total recommended vaccination | 17 (94%) | 15 (71%) | 27 (93%) | 37 (79%) | 96 (84%) | 0.09 |
| Started before IBCM counselling | 4 (22%) | 8 (38%) | 14 (48%) | 14 (30%) | 40 (35%) | 0.24 |
| Total started vaccination | 17 (94%) | 14 (67%) | 25 (86%) | 35 (75%) | 91 (79%) | 0.11 |
| Vaccine series completed (≥4 doses) | 15 (83%) | 11 (52%) | 10 (35%) | 20 (43%) | 56 (49%) | 0.0081 |
| Number of vaccine doses received | 4.3 (0-5) | 3.9 (0-5) | 3.0 (0-5) | 3.5 (0-5) | 37 (0-5) | .. |
| Received rabies immunoglobulin | 2 of 17 (12%) | 1 of 14 (7%) | 4 of 25 (16%) | 6 of 35 (17%) | 12 of 91 (13%) | 0.81 |
| Delay in starting vaccination (days) | 4.5 (0-13) | 1.5 (0-3) | 1.5 (0-11) | 2.9 (0-9) | 2.5 (0-13) | .. |
| Adverse reactions to vaccination | 2 of 17 (12%) | 1 of 14 (7%) | 0 | 3 of 35 (9%) | 6 of 91 (7%) | 0.43 |
| IBCM programme afected treatment decisions | 18 (100%) | 16 (76%) | 28 (97%) | 45 (957%) | 107 (93%) | 0.0087 |
Data are number (%) or mean (range). IBCM=integrated bite case management.
Significantly more confirmed rabies exposures than probable, suspected, and non-rabies exposures were in men (p=0.04), whereas non-rabies exposures were most common among women (figure 1, table 1). The mean age of bite victims was 29 years and most survey respondents were from the Ouest department (table 1), which is the most populated department in Haiti.
82 (71%) respondents sought medical care before receiving IBCM counselling and 40 (35%) started vaccination (table 1). Significantly fewer respondents in the confirmed and probable exposure groups sought medical care than respondents in the suspected and non-rabies exposure groups (table 1). The number of people who started vaccination before IBCM counselling was also lowest in the confirmed exposure group (table 1). After IBCM counselling, nearly all people sought medical care, in all exposure groups except the probable rabies exposure group, in which less than three-quarters sought care (table 1).
High proportions of people in all exposure groups started vaccination after IBCM counselling (table 1). Of those who started vaccination, people with confirmed and probable exposures were most likely to complete the series. Overall, 93% of respondents indicated that the IBCM programme had affected their health-care decisions, although this response was given by only 76% of respondents in the probable exposure group. 12 (13%) respondents received rabies immunoglobulin. Six (7%) of 91 respondents who started vaccination reported adverse vaccine reactions, including numbness at the injection site (n=2), lightheadedness (n=2), allergic reaction (n=2), and fever (n=1).
When we assessed the population-adjusted rates for health-care-seeking behaviours (figure 2), we estimated that the IBCM programme increased the frequency with which bite victims seek medical care by 1.2 times, start rabies vaccination by 2.4 times, and complete vaccination (when indicated) by 2.3 times (table 2). We also estimated that the rate of discontinuation of vaccination when rabies was ruled out in the biting animal was 14.8 times higher among people who started after IBCM counselling than among those who started before counselling (table 2). Without IBCM counselling, we estimated that only 6% of bite victims would follow the correct sequence of health-care events, compared with 35% with IBCM counselling (table 2).
Figure 2. Probabilities of selected health-care-seeking behaviours before and after IBCM counselling.
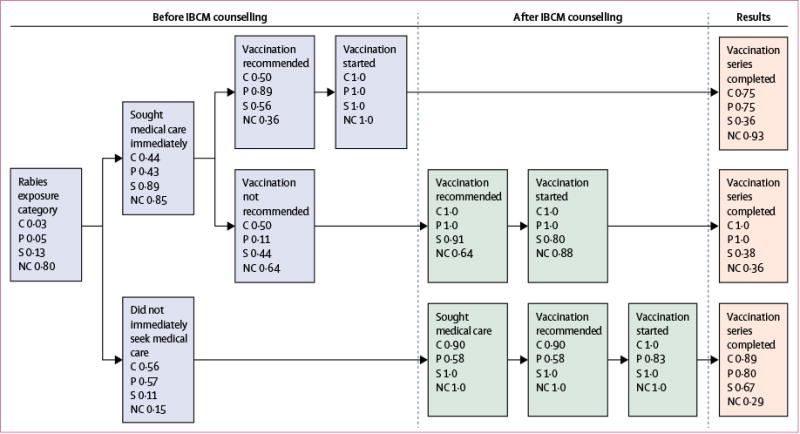
IBCM=integrated bite case management. C=confirmed exposure. P=probable exposure. S=suspected exposure. NC=non-case, exposure ruled out.
Table 2. Unadjusted and population-adjusted rates of health-care-seeking behaviours.
| Unadjusted rates
|
Population-adjusted rates*
|
|||||
|---|---|---|---|---|---|---|
| Before IBCM counselling | After IBCM counselling | Before IBCM counselling | After IBCM counselling | Times difference | Rate difference (95% CI) | |
| Sought medical care (n=115) | 82 (71%) | 108 (93%) | 82% | 99% | 1.2 | 16% (10–23) |
|
| ||||||
| Started vaccination (n=108) | 41 (38%) | 92 (85%) | 33% | 78% | 2.4 | 45% (39–50) |
|
| ||||||
| Completed vaccination, when indicated (n=66)† | 14 (21%) | 38 (58%) | 20% | 45% | 2.3 | 25% (16–34) |
|
| ||||||
| Discontinued vaccination, when recommended (n=35)‡ | 1 (3%) | 15 (43%) | 3% | 43% | 14.8 | 40% (36–44) |
|
| ||||||
| Adhered to recommended medical advice (n=115) | 15 (13%) | 51 (44%) | 6% | 35% | 6.0 | 29% (26–33) |
IBCM=integrated bite case management.
Because of the low frequency of true rabies exposures among bite victims, we did exposure-stratum sampling rather than random sampling from the entire eligible population. Therefore, population-adjusted rates reflect the likely rate of the event among all bite victims investigated by the Haiti Animal Rabies Surveillance Program.
People with confirmed, probable, and suspected rabies exposures were recommended to complete vaccination.
People for whom rabies was ruled out through observation or testing were recommended to discontinue vaccination.
The probabilities we calculated suggest that with IBCM counselling there would be four deaths among the 1478 people eligible for selection, and that the probability of death would be greatest for people in the probable rabies exposure group. By contrast, we estimated that without IBCM counselling 11 people in the eligible population would die from rabies, which represents a 65% decrease in the probability of dying from rabies under the IBCM programme.
Seven (33%) respondents with probable rabies exposures did not start vaccination, one of whom was a man aged 23 years who had died from an illness consistent with the WHO case definition for a probable human rabies case and was bitten by a dog that had a HARSP classification of probable rabies infection (panel 2). People with probable exposures who did not start rabies vaccination were older than people who completed vaccination, were more likely to be men than women, and were more likely to live in Carrefour than in other areas (table 3).
Table 3. Characteristics of people with probable rabies exposures.
| Rabies vaccination not started (n=7) | Rabies vaccination started but <4 doses completed (n=3) | Rabies vaccination started and ≥4 doses completed (n=11) | p value | |
|---|---|---|---|---|
| Men/women | 6 (86%)/1 (14%) | 2 (67%)/1 (33%) | 6 (55%)/5 (45%) | 0.22 |
|
| ||||
| Age (years) | 33 (23–42) | 18 (0–31) | 26 (0–48) | .. |
| Residence | ||||
| Artibonite department | 0 | 0 | 2 (18%) | 0.47 |
| Centre department | 2 (29%) | 1 (33%) | 2 (18%) | .. |
| Ouest department | 5 (71%) | 2 (67%) | 7 (64%) | .. |
| Carrefour commune | 5 (100%) | 0 | 2 (29%) | 0.0048 |
|
| ||||
| Sought medical care after IBCM intervention | 2 (29%) | 3 (100%) | 11 (100%) | 0.0025 |
|
| ||||
| IBCM affected decision to seek medical treatment | 2 (29%) | 3 (100%) | 11 (100%) | 0.0025 |
|
| ||||
| Bitten by a dog known to be owned | 3 (43%) | 2 (67%) | 8 (73%) | 0.26 |
|
| ||||
| Alive at follow-up | 4 (57%) | 3 (100%) | 11 (100%) | 0.0429 |
|
| ||||
| Health status unknown at follow-up | 2 (29%) | 0 | 0 | .. |
|
| ||||
| Dead at follow-up | 1 (14%) | 0 | 0 | .. |
Data are number (%) or mean (range). IBCM=integrated bite case management.
19 people with potential rabies exposures (one from a dog with confirmed rabies, seven with probable rabies, and 11 with suspected rabies) did not receive rabies vaccination. Assuming that rabies would be found in 100%, 50%, and 12.5% of the dogs, respectively, six of these bites were likely to be exposures from rabid dogs, which resulted in one death (table 3). Thus, mortality due to rabies among people with rabies exposures who did not seek medical treatment was 17% (95% CI <0.5–64).
Discussion
Mass vaccination of dogs is the only cost-effective rabies elimination measure,16,17 but many developing countries do not have the infrastructure and funding necessary to set up effective canine rabies vaccination programmes.9,18 IBCM programmes, such as the one developed in Haiti, can provide professional, community-based counselling for bite victims, which we found could significantly improve the number of people starting and completing vaccination while reducing the unnecessary use of vaccine for non-rabies exposures. IBCM programmes are not a substitution for mass vaccination of dogs, but should provide a complementary preventive measure against human rabies deaths.
WHO recommends that all victims of dog bites in areas with endemic canine rabies start vaccination.3 Only two studies have previously attempted to describe healthcare-seeking behaviours after dog bites in Haiti, both of which showed that few people sought care (34% and 54%) or started rabies vaccination (31% and 41%).10,12 Our assessment showed significant increases in health-care-seeking behaviour and starting rabies vaccination among people who received counselling through the IBCM programme (94% and 85%, respectively). This change in behaviour was probably due to community-based engagement and tailored risk assessments. Our findings support the idea that community-driven IBCM programmes that include assessment of biting animals and education bite victims can significantly improve health-care-seeking behaviours.
The effect of the IBCM on health-care-seeking behaviour could be inflated in this study because in reality some people might have delayed seeking medical treatment (ie, taken >48 h) irrespective of the programme. However, given previous reports of low health-care-seeking rates in Haiti and other countries with endemic rabies, we do not believe this behaviour would substantially alter our results. We attribute the high number of people seeking health care to one-to-one counselling provided by the IBCM programme. Nevertheless, convincing bite victims to seek medical care is only the first step in preventing human rabies deaths. Medical providers must make appropriate recommendations and bite victims must receive four or five doses of vaccine or discontinue when exposure is ruled out. The effect of the IBCM programme on this cascade of events is clearly positive, since the number of patients who followed the correct sequence of health-care actions increased by six times. Our findings are based on assessments of people who sought medical care or were found during a field investigation from a public health report. Therefore, they might not be generalisable to bite victims in Haiti who do not seek care after dog bites. We believe, however, that expansion of IBCM coverage to increase patients' adherence to vaccination and improved training of health-care providers on appropriate treatment recommendations would likely be associated with saved lives. Despite the potential benefits, relying only on treatment-based programmes in a setting like Haiti will not eliminate dog-mediated human rabies deaths, as indicated by the one probable rabies death in our study cohort.
Adherence can be defined in many ways, but two are important in terms of operating a rabies control programme: completion of at least four doses of vaccine when rabies cannot be ruled out, and discontinuation of vaccination when rabies is ruled out. The former saves lives and the latter ensures efficient use of rabies vaccine, which is often expensive and available in limited amounts in countries with endemic canine rabies. We found no other studies that had stratified adherence into these categories, which makes direct comparison of findings challenging. In studies that have reported adherence in countries with endemic rabies, it has been poor, with rates as low as 28% in Tanzania, 40% in Nepal, and 48% in the Ivory Coast,19–23 and only reaching 60% in Bhutan.22 Among respondents in our survey who sought medical care and for whom a rabies exposure could not be ruled out, 58% completed at least four doses of vaccine, with the proportion being 81% among those with confirmed or probable exposures.
Health-care-seeking behaviours and rabies vaccination rates were very low among respondents with probable rabies exposures. The animal rabies case definition for Haiti's IBCM programme has four tiers and is based on clinical and epidemiological factors (panel 1), which might have meant that these people were insufficiently counselled about risk, leading them to decline medical care. When the low vaccination rate in this group of respondents was revealed, IBCM programme managers held a workshop to retrain investigators in the proper use of the animal rabies case definition and developed a case-determination guide. Nevertheless, the IBCM programme was associated with a 1.9 times increase in health-care-seeking in this subgroup (table 1), and those who started vaccination were just as likely to complete the series as respondents with confirmed exposures, which suggests that factors other than insufficient counselling were involved.
People with probable rabies exposures had the lowest frequency of seeking health care before IBCM counselling (43%). An alternative cause for poor vaccination uptake in this group could be that they were averse to seeking treatment irrespective of whether they received IBCM counselling. People who did not start rabies vaccination were more likely to be older, male, and live in Carrefour commune, Ouest department, a densely populated community on the outskirts of the capital city, than those who did start vaccination. Carrefour's health centre does not routinely stock rabies vaccine, and bite victims are referred to other health centres for vaccination. Older men or members of this community might have difficulty travelling to secondary treatment centres. Whatever the reasons behind low vaccination adherence, these findings indicate important areas for improvement in Haiti's IBCM programme. A combination of improved training for investigators and counselling for bite victims could increase adherence and further decrease human deaths.
Our survey provides quantitative evidence that professional animal assessment of rabies exposures and tailoring of vaccine recommendations based on the findings improves the efficiency of IBCM. Most dog bites in Haiti are from non-rabid dogs, representing a substantial potential saving in vaccine if decisions about postexposure prophylaxis are based on HARSP investigation results.10
Distribution of rabies vaccine is restricted in Haiti, with only 16 hospitals routinely receiving stocks. When available, the vaccine in these centres is given free of charge, although there are often shortages. In 2014, for instance, Haiti received a sufficient stock of human rabies vaccines to treat 4000 people with suspected rabies exposure, yet an estimated 200 000 people experienced dog bites,24 meaning that many suspected rabies exposures probably went untreated. Private pharmacies charge around US$12 per vaccine dose. The restricted supply of rabies vaccines in Haiti and frequent hospital vaccine shortages underscore the need for improved efficiency in vaccine use. For countries with low stocks of rabies vaccines but also low rates of rabies in biting dogs, recommendations that delay starting vaccination in people at low risk of exposure might be necessary to avoid supply shortages. Furthermore, if triage was recommended worldwide, delaying the start of postexposure prophylaxis in people at low risk of exposure while animals were assessed under a reliable IBCM programme, might lead to substantial cost savings.25
Even under the most advanced IBCM programmes, not reporting cases and non-adherence to vaccination persist and result in human rabies deaths.26 To work, IBCM programmes rely on timely reporting of dog bites and a skilled workforce to assess animals, collect samples, and make timely diagnoses. Furthermore, bite victims must adhere to treatment recommendations. So long as canine rabies remains endemic, breakdowns in health-care delivery and adherence will result in human rabies deaths. Our survey, however, shows that IBCM can be extremely effective for reducing the burden of human rabies. The proportion of people with probable rabies exposures completing vaccination series was among the highest ever found among countries with endemic canine rabies. For this success to be replicated, scaling up of HARSP and improving access to rabies vaccines will need to be pursued. In countries such as Haiti, where the human rabies vaccine supply cannot satisfy the demand, triage of cases based on IBCM investigations to prioritise treatment might be necessary until successful mass vaccination programmes can eliminate the disease in dogs. We have shown the merits of temporising measures, and our findings can help serve as a guide for the development of future IBCM programmes.
Supplementary Material
Research in context.
Evidence before this study
In 2013, Haiti introduced an integrated bite case management (IBCM) programme that refers animals involved in bite events to the Haiti Animal Rabies Surveillance Program (HARSP), where they are either euthanised and tested or observed. Additionally, the IBCM programme offers rabies counselling to bite victims, typically within 48 h of the bite event. The IBCM programme has expanded to provide national coverage. Whether the programme had a quantifiable effect on rabies prevention in Haiti had never been assessed. We did a retrospective follow-up survey involving randomly selected bite victims who were investigated by Haiti's IBCM programme between May 15, 2014, and Sept 15, 2015. A literature review was done to identify peer-reviewed publications in English describing bite rates and rabies incidence in Haiti since 2000. We searched with the term “Haiti AND Rabies” (MeSH). Eight articles were identified, of which two contained relevant parameters. One reported around 5% incidence of rabies in biting dogs. We based the calculation of our sample size on this finding. The second study indicated that 3% of Haitian dog owners are bitten, which we used to estimate a human rabies disease burden specific to Haiti. To help estimate human rabies burden, we adapted a previously published formula to fit the specific parameters available in Haiti. Several reports have described health-care-seeking behaviours after dog bites in rabies endemic countries. We reviewed these papers to establish the crucial factors on which to collect data from survey respondents.
Added value of this study
Worldwide there is uncertainty about how people use health-care systems after receiving dog bites. Elimination of rabies in human beings has been most efficiently achieved through vaccination of dogs, but mass dog vaccination programmes take years to develop and implement. Unfortunately, few data are available on when, why, and how people use health-care facilities after a dog bite in most developing countries. Furthermore, only two publications have explored how IBCM programmes might perform in the context of developing nations' infrastructures. The survey and analytical design of our study helped to fill some of the gaps in knowledge, such as health-care-seeking behaviours in the absence of an IBCM programme, improvements in health care after the programme's introduction, the effects of discontinuing prophylaxis after exposure, and health outcomes of bite victims. Finally, we were able to analyse health outcomes by type of rabies exposure (confirmed, suspected, probable, or non-rabies) rather than classifying all dogs as having suspected rabies. Our findings are relevant to low-income nations with endemic animal rabies. We found that the IBCM approach was associated with one of the highest reported completion rates for rabies vaccination (81%) and potentially reduced the risk of dying from rabies by 65%.
Implications of all the available evidence
We believe this formal assessment of the effects of an IBCM programme will be useful to the international rabies community because it advances burden estimation. The IBCM approach improved health outcomes through assessment of biting dogs. WHO has set a target of eliminating dog-mediated human rabies deaths by 2030. This goal is likely to be achieved through a combination of IBCM and mass vaccination of dogs, and data such as ours are important to advocate for the continued investment into such programmes, particularly as WHO is setting up a formal working group to reassess the expert consultation on rabies. Currently, WHO recommends that all people bitten by dogs in countries with endemic rabies start postexposure prophylaxis, but provides little guidance on how IBCM programmes might affect this recommendation. We found quantifiable evidence that an IBCM programme can reduce human rabies deaths and provides a framework for developing countries with endemic rabies to follow for implementation of their own programmes. If other programmes are as successful as the IBCM has been for Haiti, global implementation might reduce human rabies deaths by 60% or more.
Panel 1: Haiti Animal Rabies Surveillance Program case definitions.
Confirmed rabies
Diagnostic confirmation of rabies virus by DFA test
Probable rabies
Animals that were not tested for rabies
AND
Died during observation
OR
Did not pass observation (unfound escaped animals)
OR
Developed at least one clinical sign and died after being bitten by an animal with suspected, probable, or confirmed rabies virus infection
Suspected rabies
Animals reported to the Haiti Animal Rabies Surveillance Program ofcers but could not be assessed
OR
Animals that had no or one sign of rabies and inconclusive test results
Non-cases
Animals healthy after 14 days of observation
OR
Negative DF Atest
DFA=direct fuorescent antibody.
Panel 2: Deaths at follow-up among people assessed by the Haiti Animal Rabies Surveillance Program.
A man aged 80 years died from what the family described as natural causes. He was bitten by a dog with suspected rabies virus infection and did not receive vaccination. His family stated that his age made it difficult for him to seek medical care for the bite wound. However, the family was unaware of any neurological symptoms before death and attributed his death to age-related causes. Therefore, this case did not meet WHO clinical case definition for human rabies virus infection.*
A man aged 42 years from Carrefour died around 2 months after a bite from a dog classified as probable for rabies virus infection, which is the second highest risk category. The dog showed signs of aggression and bit six people before it was killed and the body was destroyed. Hospital records showed that the man was treated for the bite wound, but he refused rabies vaccination. Family members told IBCM investigators that the man acutely developed neurological deficits, confusion, and inflammation of the testicles. The exposure, lack of vaccination, and clinical course indicated a probable rabies case.*
A man aged 23 years from Carrefour was bitten by a dog that tested negative for rabies at Haiti's national laboratory. The man and his family were unable to confirm whether he had received treatment for his bite wound. He developed an acute neurological illness leading to death 2 months after being bitten. Upon receiving this report, the Ministry of Agriculture, Natural Resources, and Rural Development immediately submitted the sample from the offending dog to the US CDC rabies laboratory for confirmatory testing. The CDC confirmed the results obtained in Haiti of no rabies virus in the sample. While the dog did not have rabies, it is possible that the deceased man had another exposure to rabies virus that was not reported. Due to the clinical presentation and abrupt death, this case is consistent with the WHO human rabies case definition for a suspected rabies case, but the death is not a result of the animal examined.
IBCM=integrated bite case management. CDC=Centers for Disease Control and Prevention. *The WHO clinical case definition of rabies describes a person presenting with an acute neurological syndrome (encephalitis) dominated by forms of hyperactivity (furious rabies) or paralytic syndromes (paralytic rabies) progressing towards coma and death, usually from respiratory failure, within 7-10 days after the first symptom without intensive care; case classifications are suspected (cases compatible with the clinical case definition), probable (a suspected case plus history of contact with a suspected rabid animal), and confirmed (laboratory confirmation of a suspected case).
Acknowledgments
Funding None.
We thank Terquana Sander, Centers for Disease Control and Prevention, Atlanta, GA, USA, for cleaning the database, the team at the Haitian Ministry of Agriculture of Haiti for canine rabies surveillance and data collection, and the team in Department of Epidemiology, Laboratory, and Research of the Haitian Ministry of Health for human rabies and dog bite surveillance and data collection. The views in this publication are those of the authors and do not necessarily represent the policy or recommendations of the US Centers for Disease Control and Prevention
Footnotes
Contributors: RMW developed and oversaw approval of the study protocol. PDA, LF, KC, and NF collected the data and PDA oversaw the telephone interviews. MM oversaw data ownership. MDE and RMW did the data analysis and JDB, BM, and MM reviewed the data. MDE, JDB, BM, and RMW interpreted and disseminated the results. BM created the study maps. MDE and RMW developed and MDE, MK, and RMW wrote and reviewed the paper.
Declaration of interests: We declare no competing interests.
Contributor Information
Melissa Dominique Etheart, Waterborne Disease Prevention Branch, Centers for Disease Control and Prevention in Haiti, Port-au-Prince, Haiti.
Maxwell Kligerman, Stanford University School of Medicine, Palo Alto, CA, USA.
Pierre Dilius Augustin, Ministry of Agriculture, Natural Resources and Rural Development, Port-au-Prince, Haiti.
Jesse D Blanton, Poxvirus and Rabies Branch, Centers for Disease Control and Prevention, Atlanta, GA, USA.
Benjamin Monroe, Poxvirus and Rabies Branch, Centers for Disease Control and Prevention, Atlanta, GA, USA.
Ludder Fleurinord, Ministry of Agriculture, Natural Resources and Rural Development, Port-au-Prince, Haiti.
Max Millien, Ministry of Agriculture, Natural Resources and Rural Development, Port-au-Prince, Haiti.
Kelly Crowdis, Christian Veterinary Mission, Port-au-Prince, Haiti.
Natael Fenelon, Pan American Health Organization, Port-au-Prince, Haiti.
Ryan MacLaren Wallace, Poxvirus and Rabies Branch, Centers for Disease Control and Prevention, Atlanta, GA, USA.
References
- 1.Hampson K, Coudeville L, Lembo T, et al. Estimating the global burden of endemic canine rabies. PLoS Negl Trop Dis. 2015;9:e0003709. doi: 10.1371/journal.pntd.0003709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fooks AR, Banyard AC, Horton DL, Johnson N, McElhinney LM, Jackson AC. Current status of rabies and prospects for elimination. Lancet. 2014;384:1389–99. doi: 10.1016/S0140-6736(13)62707-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO Expert consultation on rabies. Second report World Health Organ Tech Rep Ser. 2013;982:1–139. [PubMed] [Google Scholar]
- 4.Lembo T, on behalf of the Partners for Rabies Prevention The blueprint for rabies prevention and control: a novel operational toolkit for rabies elimination. PLoS Negl Trop Dis. 2012;6:e1388. doi: 10.1371/journal.pntd.0001388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lembo T, Hampson K, Kaare MT, et al. The feasibility of canine rabies elimination in Africa: dispelling doubts with data. PLoS Negl Trop Dis. 2010;4:e626. doi: 10.1371/journal.pntd.0000626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vigilato MA, Clavijo A, Knobl T, et al. Progress towards eliminating canine rabies: policies and perspectives from Latin America and the Caribbean. Philos Trans R Soc Lond B Biol Sci. 2013;368:20120143. doi: 10.1098/rstb.2012.0143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vigilato MA, Cosivi O, Knöbl T, Clavijo A, Silva HM. Rabies update for Latin America and the Caribbean. Emerg Infect Dis. 2013;19:678–79. doi: 10.3201/eid1904.121482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davlin SL, Vonville HM. Canine rabies vaccination and domestic dog population characteristics in the developing world: a systematic review. Vaccine. 2012;30:3492–502. doi: 10.1016/j.vaccine.2012.03.069. [DOI] [PubMed] [Google Scholar]
- 9.Taylor LH, Hampson K, Fahrion A, Abela-Ridder B, Nel LH. Difficulties in estimating the human burden of canine rabies. Acta Trop. 2017;165:133–40. doi: 10.1016/j.actatropica.2015.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wallace RM, Reses H, Franka R, et al. Establishment of a canine rabies burden in Haiti through the implementation of a novel surveillance program. PLoS Negl Trop Dis. 2016;10:e0004354. doi: 10.1371/journal.pntd.0004354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lapiz SM, Miranda ME, Garcia RG, et al. Implementation of an intersectoral program to eliminate human and canine rabies: the Bohol Rabies Prevention and Elimination Project. PLoS Negl Trop Dis. 2012;6:e1891. doi: 10.1371/journal.pntd.0001891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fenelon N, Dely P, Katz MA, et al. Knowledge, attitudes and practices regarding rabies risk in community members and healthcare professionals: Pétionville, Haiti, 2013. Epidemiol Infect J. 2017;145:1624–34. doi: 10.1017/S0950268816003125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martin DO, Austin H. Exact estimates for a rate ratio. Epidemiology. 1996;7:29–33. doi: 10.1097/00001648-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Shim E, Hampson K, Cleaveland S, Galvani AP. Evaluating the cost-effectiveness of rabies post-exposure prophylaxis: a case study in Tanzania. Vaccine. 2009;27:7167–72. doi: 10.1016/j.vaccine.2009.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Babes V. Traité de la rage. In: Fields BN, Knipe DM, editors. Virology. 2nd. New York, NY: Raven Press; 1990. pp. 883–930. [Google Scholar]
- 16.Fitzpatrick MC, Hampson K, Cleaveland S, et al. Cost-effectiveness of canine vaccination to prevent human rabies in rural Tanzania. Ann Intern Med. 2014;160:91–100. doi: 10.7326/M13-0542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sambo M, Cleaveland S, Ferguson H, et al. The burden of rabies in Tanzania and its impact on local communities. PLoS Negl Trop Dis. 2013;7:e2510. doi: 10.1371/journal.pntd.0002510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meslin FX, Briggs DJ. Eliminating canine rabies, the principal source of human infection: what will it take? Antiviral Res. 2013;98:291–96. doi: 10.1016/j.antiviral.2013.03.011. [DOI] [PubMed] [Google Scholar]
- 19.Mazigo HD, Okumu FO, Kweka EJ, Mnyone LL. Retrospective analysis of suspected rabies cases reported at bugando referral hospital, Mwanza, Tanzania. J Glob Infect Dis. 2010;2:216–20. doi: 10.4103/0974-777X.68530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mankeshwar R, Silvanus V, Akarte S. Evaluation of intradermal vaccination at the anti rabies vaccination OPD. Nepal Med Coll J. 2014;16:68–71. [PubMed] [Google Scholar]
- 21.Tenzin, Dhand NK, Gyeltshen T, et al. Dog bites in humans and estimating human rabies mortality in rabies endemic areas of Bhutan. PLoS Negl Trop Dis. 2011;5:e1391. doi: 10.1371/journal.pntd.0001391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tenzin, Dhand NK, Ward MP. Human rabies post exposure prophylaxis in Bhutan, 2005-2008: trends and risk factors. Vaccine. 2011;29:4094–101. doi: 10.1016/j.vaccine.2011.03.106. [DOI] [PubMed] [Google Scholar]
- 23.Tiembre I, Benie J, Attoh-Touré H, et al. Discontinuation of postexposure prophylaxis at the anti-rabies Center of Abidjan, Cote d'Ivoire. Bull Soc Pathol Exot. 2013;106:272–77. doi: 10.1007/s13149-013-0312-y. [DOI] [PubMed] [Google Scholar]
- 24.Schildecker S, Millien M, Blanton JD, et al. Dog ecology and barriers to canine rabies control in the republic of Haiti, 2014–2015. Transbound Emerg Dis. 2016 doi: 10.1111/tbed.12531. published online June 17. [DOI] [PubMed] [Google Scholar]
- 25.Dimaano EM, Scholand SJ, Alera MT, Belandres DB. Clinical and epidemiological features of human rabies cases in the Philippines: a review from 1987 to 2006. J Infect Dis. 2011;15:e495–99. doi: 10.1016/j.ijid.2011.03.023. [DOI] [PubMed] [Google Scholar]
- 26.Monroe BP, Yager P, Blanton J, et al. Rabies surveillance in the United States during 2014. J Am Vet Med Assoc. 2016;248:777–88. doi: 10.2460/javma.248.7.777. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


