Abstract
Introduction:
Metabolic syndrome (METS) represent a simultaneous presence of multiple metabolic disorders in one person. Prevalence is increasing worldwide, which is probably related to increased obesity and sedentary lifestyle. Non-alcoholic steatosis or “fatty liver” is a metabolic disease caused by fat dysfunction. It can be a sign of some other disease, and can often be found in patients with metabolic disorders. Ultrasound is an acceptable method for the identification of fatty steatosis. There is evidence that when turmeric is used as a herbal diet, with its active metabolite of curcumin, can repair fatty acidosis and thus prevent progression of fatty steatosis complications such as cirrhosis and liver cancer. Goal. The aim of the study was to determine the effects of 400 mg curcuminaddition to the nutrition on ultrasound morphological characteristics of the liver in METS patients.
Methodology:
A prospective cohort study was conducted on 100 subjects with METS, treated in the family medicine practice of the Tuzla Canton, aged 35-70 years. The therapeutic effects of 400 mg curcumin on ultrasound-morphological characteristics of the liver were followed, validated by ultrasound in 50 respondents of experimental groups with METS. The data were processed by the IBM SPSS Statistics 21 statistical analysis program using parametric techniques andStudent’s t-test for paired samples.
Results:
There were 65% of women in the study. There were no statistically significant differences in the age of respondents within the analyzed groups. The use of 400 mg curcumin per day was statistically significantly improved ultrasound morphological characteristics of the liver in subjects with METS.
Conclusion:
All respondents with METS who used curcumin had beneficial effects on the morphological characteristics of the liver. Curcumin had stronger effects on subjects with METS and DM type 2 than others.
Keywords: Metabolic syndrome, Liver steatosis, Curcumin, Diabetes
1. INTRODUCTION
1.1. Metabolic syndrome
Metabolic syndrome (METS) represent the association of multiple metabolic disorders in one person at the same time. Results of meta-analysis are showed that obesity, anomaloxidemia, hyperinsulinemia, hypertension, hyperglycemia, hyperuricemia, and myocardial represent risk factors for METS, which is associated with multi-pathotoxicity.METSaffect 20-30% of the population in middle and older age (1). Its prevalence is increasing worldwide, which is connected to increased obesity and sedentary lifestyle. In one Austrian study (2), METS was investigated in 750 patients with coronary disease and showed that these patients had a high prevalence of METS.
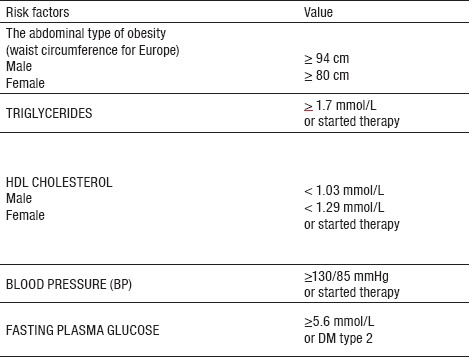
According to World Health Organization (WHO) criteria, METS is a set of metabolic risk factors: insulin resistance (IR), elevated blood pressure (BP) or hypertension, central obesity and dyslipidemia. According to this definition, the most important criterion is the presence of a glucose metabolism disorder with serum glucose levels (BG) ≥6.1 mmol/L or insulin resistance (HOMA-IR) model and/or insulin resistance and at least two other criteria: BMI ≥30 kg/m2 and/or hips to waist ratio for men>0.90 and for women>0.85, serum triglycerides (TG) ≥1.7 mmol/L or high density cholesterol (HDL) <0.9 mmol/L for men and <1.0 mmol/L for women, urinary albumin excretion>20µg/min, and blood pressure (BP) ≥140/90 mmHg. The definition offered by WHO has shown a limitation in clinical use due to the impossibility of measuring insulin resistance. In 2005, the International Diabetes Federation (IDF) proposed the latest consensus definition of METS (3). The main focus in this new definition is the central obesity(Figure 1). For a person to meet the METS criteria, it has to have a central obesitydefined by the waist circumference (WC) which is ethnically specific and for Europeans for men is ≥94 cm and for women ≥80 cm with at least two or more, of any of the following four criteria: TG ≥1.7 mmol/L, HDL-cholesterol for men <1.03 mmol/L and for women <1.29 mmol/L, systolic BP ≥130 mmHg and diastolic BP ≥85 mmHg, or use of antihypertensive therapy and BG ≥5.6 mmol/L or diagnosis of DM type 2 (Table 1). On the panel on the harmonization of diagnostic criteria between IDF and the American Heart Association/National Heart, Lung, and Blood Institute (AHA/NHLBI), both sides agreed that WC should not be a precondition for making a METS diagnosis. Based on this consensus, WC is one of the equal criteria in METS. Presence of three to five risk factors, represent the diagnosis of METS (4).
Figure 1.

Patient with severe liver steathosis and metabolic syndrome
Table 1.
Criteria for METS according to IDF (2005)
1.2. Non-alcoholic steatosis and non-alcoholic steatohepatitis
Non-Alcoholic steatosis or Non-Alcoholic Fatty Liver Disease (NAFLD) is a metabolic disease caused by fat tissue dysfunction. It is often a sign of some other disease, rather that it is a separate entity. The liver may be of normal size or enlarged to different degree, depending on the type and degree of pathological changes. Liver steatosiscan progress to fibrosis, or cirrhosis, with accompanyingliver function disorders. When liver steatosis is followed by liver function disorders and inflammatory changes present, Non-Alcoholic Steato-Hepatitis (NASH) is formed. In fibrous proliferation, liver cell stem cells (HSC) produce collagen, induced by various oxidative processes. NAFLD is the most common cause of chronic liver disease in the United States with an incidence of 10-24%. Steatosis is also present in about 35% of people with normal body weight. The amount of fat in the liver does not correlate with visceral and subcutaneous fatty tissue, but shows a significant correlation with the level of fasting insulin and triglycerides (5).
1.3. Ultrasound as a diagnostic method for non-alcoholic liver steatosis
Morphologically fatty liver is diagnosed by ultrasound (US) liver examination, and in case of special indications by magnetic resonance (MRI). Inflammatory changes in the liver are determined, according to indication, by histological examination of liver tissue obtained by liver biopsy and it is necessary to exclude other liver diseases. USdiagnostic is one of the methods that can visualize liver steatosis, it is inexpensive, and is a reliable diagnostic method that can provide qualitative liver characteristics. It requires a good resolution ultrasound machine and a well-trained physician that will detect changes in the liver and qualitatively characterize them. In addition to the ultrasound, a biopsy can be performed to confirm liver changes, followed by ultrasound examination. The ultrasound finding of liver steatosis depends on the intensity of fat infiltration and duration of the disorder, as well as on the extent of liver parenchyma affected. Changes in the liver become manifested when liver parenchyma is infiltrated with fatty tissue more than 10%. The intensity of hemangiogenicity of liver parenchyma cannot be objectively and quantitatively evaluated, only a qualitative description of the can be provided as: normal echogenicity, light, medium and very pronounced steatosis. Normal echogenicity implies that the liver tissue on ultrasound is without visible fattissue infiltration. Light steatosis is the first stage and liver on ultrasound finding is lighter, more gray compared to normal parenchyma. Medium pronounced steatosis has clear ultrasound image of “bright” liver. With very pronounced steatosis, the liver parenchyma on ultrasound appears to be very bright, and is also called a “shiny liver” (6).
1.4. Nutrition supplement–Curcumin and its mechanism of action
Turmeric or Siamese tulip (Curcumalonga) is a plant from a ginger family. It is cultivated in India and other parts of South Asia (7). It has a long tradition of use in ayurvedic medicine. Curcumin is the primary active ingredient of plant and it have intensive yellow color. It is used as a spice and dietary supplement, and was firstly identified in 1910 by Lampe and Milobedzka (8). To curcuminis attributed pharmacological activity, including antioxidative (9) and antimicrobial properties (10). By its chemical structure, curcumin is a polyphenol derivative. Curcumin has anti-tumor activity due to its ability to prevent tumor cell proliferation and the induction of their programmed death. Its antioxidant activity, curcumin, realizes by neutralizing free radicals that damage the body’s cells by oxidizing their structures, and in time lead to accelerated aging. The anti-inflammatory action of curcumin is based on the inhibition of leukotriene synthesis and in the changes in prostaglandin production. It blocks the proliferation of lymphocytes and reduces cell activity of natural cell killers. It binds to estradiol and progesterone receptors and may have mild estrogenic activity. Numerous clinical trials that are still ongoing need to provide even better understanding of its therapeutic potential (11).
In many chronic illnesses, in which is known that inflammation play an important role, it has been shown that curcumin exhibits therapeutic potential. These diseases include cardiovascular disease (CVD), allergies, asthma, bronchitis, colitis, rheumatoid arthritis, psoriasis, diabetes, obesity, or METS, liver diseases and AIDS. Curcumin can affect the prevention and alleviation of colorectal and some other cancers symptoms (12). In patients with inflammatory bowel disease (IBS), with the most common symptoms of abdominal pain and flatulence, may help to change the habits related to increasedfrequency of defecations (13, 14). Curcumincleans the liver of various harmful metabolites, is a natural painkiller, regulates metabolism and helps in weight loss. Curcumin may have an inhibitory effect on nauseous hyperplasia in case of pancreatitis, through serum amylase, trypsin neutrophils infiltration (15).
2. GOAL
The aim of the study was to determine the effects of the dietary supplement XY curcumin on ultrasonic morphological characteristics of the liver in the patients with METS.
3. MATERIAL AND METHODS
A prospective cohort study was conducted on 100 METS patients, who were treated in the Primary Health Care institutions of the Tuzla Canton, aged 35-70 years, during the period May 2013–April 2014. The METS criteria are set according to the IDF criteria. The therapeutic effects of the XY curcuminbased on ultrasound morphological characteristics of the liver were evaluated in the experimental group (N=50) patients with METS. Selection of respondents was based on inclusion and exclusion criteria. Inclusion criteria were: voluntaryconsent for inclusion in the study, age 35-70 years, diagnosis of METS according to IDF criteria (2005), duration of DM type 2 up to 10 years. Excluding criteria were the existence of acute illness, severe mental illness, gallstones, conditions immediately after surgery, acute bleeding conditions, use of anticoagulant therapy, duration of DM type 2 for more than 10 years. Based on these criteria, the respondents (N=100) were selected and divided into two groups by 50 respondents: group A (experimental–who used curcumin) and group B (control–who did not use curcumin). Within groups were created subgroups of 25 respondents: subgroup A1 (respondents with METS and pre-diabetes status) and subgroup A2 (respondents with METS and DM type 2). Diagnostic criteria for DM type 2 and prediabetes (PD) are shown in Table 2. Patients in the experimental group (A), during the study, besides nonpharmacological and pharmacological measures, took dietary supplement XY curcumin at a dose of 400 mg daily, while in control group (B) patients were treated with non-pharmacological and pharmacological measures without curcumin during the study. The treatment effects were monitored by ultrasoundtrough the examination of morphological characteristics of the liver at the beginning and end of the study after 12 months.
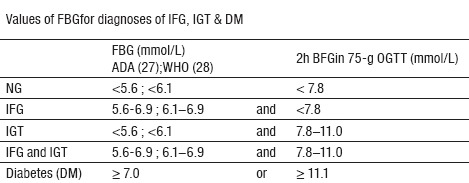
Table 2.
Diagnostic criteria for Glucose Tolerance Disorder and DM Type 2. Abbreviations: FBG – Fasting blood glucose; NG- Normal glucose; IFG–Impaired fasting glucose; IGT –Impaired glucose tolerance; DM – diabetes mellitus
3.1. Evaluation of ultrasound morphological characteristics of the liver
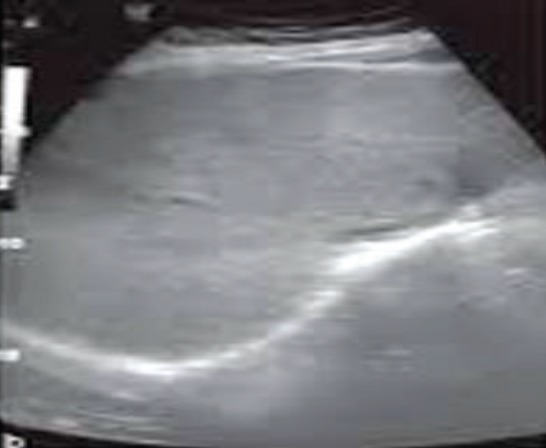
In assessing the morphological liver characteristics and diagnosis of NAFLD or NASH, was performed ultrasound examination using the SIMENS LOGIQ 3 expert brand ultrasound device, with 3.5MHz probe (Figure 2). Qualitative liver characteristics were expressed numerically, from 0-3, due to the statistical processing of parameters: 0-without steatosis (Figure 3); 1-initial steatosis (Figure 4); 2-moderate steatosis (Figure 5) and 3-expressed steatosis (Figure 6).
Figure 2.
Ultrasound machine used for estimation of presence and level of liver steatosis
Figure 3.

Ultrasound caption of morphological characteristics of a normal liver
Figure 4.

Ultrasound caption of the begining of liver steatosis (gradus 1)
Figure 5.

Ultrasound caption of moderate liver steatosis (gradus 2)
Figure 6.
Ultrasound caption of significant liver steatosis (gradus 3)
3.2. Statistical methods
Collected data was entered into a specially crafted database on a personal computer and statistical processing was performed using the appropriate software support in form of the IBM SPSS Statistics 21 statistical data processing program and they are presented in the work. For the purpose of analyzing the effect of curcumin on the morphological characteristics of the liver in METSpatients, Student’s t-test for paired samples was used. In practice, this technique is used to compare the mean values of the same group of people measured twice or when the subjects are paired. In this case, it is about comparing the liver characteristics at the beginning and at the end of the study. It was observed whether are significantly different morphological characteristics of the liver were measured in two measurements, depending on the use of XY curcumin as a dietary supplement. Both groups of respondents were examined for the existence of differences significance of the obtained ultrasonic morphological characteristics of the liver, where statistical significance was interpreted using p value. If the p value is <0.05, the statistical significance of the observed parameter is confirmed.
4. RESULTS
4.1. Distribution of subjects by sex
In total sample (N=100), there were 65 women and 35 men. There were significantly more women in comparison to men, which is in line with the fact that women are more likely to suffer from metabolic disorders.
4.2. Distribution of respondents by age
The age range of respondents in the study was 36-70 years. Ranked in 5 years spans, 29% of respondents were 66-70 years old. At age 61-65 there were 21%, age 56-60–18%, age 51-55 years were 19%, age 46-50 years 9%, and 2% at age 41-45 and 36 -40 years (Figure 7).
Figure 7.
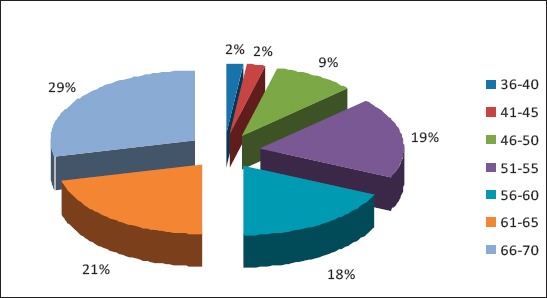
Age distribution of the respondents
4.3. The results of ultrasound morphological characteristics of the liver
The results of ultrasound morphological characteristics of the liver in experimental group Awhich used XY curcumin
In the subgroup AA1, patient with METS and PD, from the experimental group A using curcumin, the mean value of the ultrasound morphological liver appearance was numerically expressed at the beginning of the study as 1.60. Described by the ultrasound characteristics, this finding is similar to the mid-point between “initial” and “moderate steatosis”. At the end of the study, this numerical value was 1.04, which is described by ultrasound characteristics as “initial steatosis”. In this casep=0.000 (with the remark that the result obtained is rounded to three decimal places, which means that the real probability is <0.001), indicating that there is a significant difference in the results of ultrasound morphological characteristics of the liver obtained at the beginning and at the end of the study in the experimental AA1 subgroup. The average reduction is 0.560, and the 95% confidence interval ranges from the lower of 0.351 to the upper 0.769 (Table 3).
Table 3.
Ultrasound morphological characteristics of liver in respondents with METS. Subgroups: AA1 (METS & PD); AA2 (METS & DM type 2); BA1 (METS & PD); BA2 (METS &DM type 2).

In the subgroup AA2, patients with METS and DM type 2, which also belong to experimental group A, there was a statistically significant difference in ultrasound morphological liver characteristics measured at two different moments. The ultrasound morphological liver appearance at the beginning of the study was numerically expressed by mean of 2.20, which by ultrasound characteristics means the existence of “moderate steatosis”. At the end of the study, the numerical value decreased to the mean of 1.36, which would be described as “initial steatosis”. Student’s t-test for the paired samples evaluated the effect of curcumin on liver characteristics in experimental subgroup AA2withp=0.000. The mean decrease in values was 0.840, while the 95% confidence interval ranged from 0.686 to 0.994 (Table 3).
Results of the ultrasound morphological characteristics of the liver in control group B which didnotuse curcumin
In the control subgroup BA1 or respondents with METS and PD characteristics, from the control group B which did not usecurcumin, ultrasound morphological liver appearance, expressed by the meanofvalues at the beginning of the study was 1.44, which would characterize ultrasound as “initial steatosis”. At the end of the study, the mean numerical value was 1.60, which also means “initial steatosis” but with a tendency of deterioration compared to the beginning. In this case, given that p=0.103, it is concluded that there is no significant difference in ultrasound morphological characteristics of the liver at the beginning and end of the study in the control subgroup BA1. During one-year period, average morbidity of the liver measured by ultrasound was 1.44 at the beginning of the study, to 1.60 in the end (Table 3). In the control subgroup BA2 of patients with METS and DM type 2 characteristics, of control group B without the use of curcumin, the mean value of ultrasound morphological liver appearance was 2.00 at the beginning and end of the study. This means that ultrasound morphological appearance of the liver in this subgroup remained with the same characteristics of “moderate steatosis”. Significance p=1000 in this group suggests that there is no significant difference in the morphological characteristics of the liver at the beginning and end of the study (Table 3).
5. DISCUSSION
All respondents in our study meet diagnostic criteria for METS. Both in the experimental (A) and control (B) group, there were 25 subjects fulfilling METS and PD or METS and DM type 2 diagnostic criteria. Patients in both groups, experimental and control, were treated with nonpharmacological and pharmacological measures, and patients from experimental group also received tablet of XY curcumin at a dose of 400mg once a day for a year, as long as the study lasted. Non-pharmacological measures implied that all respondents were educated about changes in nutrition, smoking habits, and the importance of regular physical activity. Pharmacological measures implied the use of drugs to achieve target metabolic parameters in METS.
All subjects underwentultrasound liver examination which characterized the morphological appearance of the liver in the sense of the presence of non-alcoholic steatosis at the beginning and at the end of the study. The study aimed to determine the effect of XY curcumin as an intervention agent on ultrasound morphological characteristics of the liver in subjects with METS in experimental group A.
The role of primary health care is irreplaceable in early detection and the creation of better control of individual parameters of METS. In order to limit the number of new cases, the lifestyle of the population with the PD must be altered. This proved to be a big challenge. One of the alternative approaches to the prevention of DM type 2 development is to intervene within METS before the disease develops into fully developed form of DM type 2. In Europe, theBotnia research (16) found 10% prevalence of METS in persons with normal glucose tolerance (NGT), 50% in stage of pre-diabetes, and 80% DM patients. According to the results of NHANES III (17) using the NCEP ATP III (2001) METS prevalence rate in the United States, adjusted for age, was 24% in adults. The prevalence increases with age and in the age group 20-29 was about 7%, while in the age group 60-69 years was the largest at 44%. In our study, respondents with diagnostic characteristics of METS and PD, aged 61-70, were represented by 34%.
In recent years, several effective interventional regimens have been developed for the treatment of METS, with encouraging results (18). However, these regimes are not always economically feasible (18). Today’s focus is on identifying new effective therapeutic agents, with relatively low cost and relatively low toxicity, which can be used regularly to control the DM Type 2 advancement in METS. Here, curcumin has its own area in which it can be used. There is evidence of beneficial effects of curcumin on human health even in the Ayurvedic and Chinese traditional medicine for the past thousand years. There is little known about the benefits of daily and continuous use of curcumin in our environment, although evidence of the beneficial effects of this natural preparation exists (19).
Curcumin attracted scientific attention as a therapeutic agent in experimental diabetes and the treatment of complications, primarily because it is an effective, relatively inexpensive and safe mean of reducing glycaemia and hyperlipidemia in the rat (20). It is widespreadusedand there is opinion that it has a positive effect on human health. Curcumin has been shown to possess anti-inflammatory and anti-diabetic properties (21, 22, 23, 24), may delay the development of DM type 2, improve function and prevent the death of pancreatic beta cells, and reduce IR in experimental animals (21, 22, 24).
People with diabetes often have NAFLD and other liver diseases (25). Glucose abnormalities are the fundamental component of METS. With excessive accumulation of fatty tissue, atherogenic dyslipidemia, elevated BP, IR, disturbed fibrinolysis and inflammation, and NAFLD together multiply toxicity. Fat liver infiltration and consequent fibrosis have become a major health problem. Up to 25% of adults with NASH may have cirrhosis. Metabolic steatosis may coexist with hepatitis C virus infection, regardless of genotype, which can lead to the occurrence of hepatocellular carcinoma.
Fortunately, there are healthy strategies that can help and reduce the amount of fat in the liver, namely: nutrition, physical activity, and maintaining healthy body weight. Changing the lifestyle, in this manner, can help reduce and eventually eliminate the steatosity. The research team led by Professor Michael Trauner of the Medical University of Graz (2010) analyzed tissue and blood samples of chronic liver inflammation in mice before and after adding curcumin to their diet after four or eight weeks. This team found that mice on the curcuminic diet had significantly less obstruction of the bile ducts, significantly less damage to liver and cells scarring. Researchers have concluded that the positive effects of curcumin, which have caused the disruption of the chemical signal pathways responsible for inflammation. Study of Fu et al. (26) has demonstrated that curcumin significantly protects liver from damage caused by the AST, ALT, and alkaline phosphatase activity, and improves the histological liver architecture. In addition, curcumin reduces oxidative stress by increasing the content of liver glutathione, leading to a reduction in LDL-cholesterol levels.
Curcumin reduces inflammation by decreasing levels of inflammatory cytokines, including interferon-γ, TNF-α and IL-6. Furthermore, curcumin suppresses insulin-induced HSC activation by interrupting the insulin signal pathway and decreasing oxidative stress, thereby decreasing the abundance of platelet-derived growth factors, transforming growth factor-β, their receptors, and collagen type I collagen. Thanks to these findings, curcumin may be a therapeutic antifibrous drug for the treatment of liver fibrosis.
In our research, it has been shown that continuous education on healthy habits, with continued use of 400mg of curcumin during one year, significantly improves the morphological characteristics of the liver in both experimental subgroups–both in subgroup AA1 with METS and PD characteristics, as well as in subgroup AA2 with the characteristics of METS and DM type 2, with p<0.001. The use of curcumin at a dose of 400mg improved the morphological characteristics of the liver in the METS patients.
6. CONCLUSION
In this study, there were 65% of women, 86% of respondents were aged 51-70 years and there was no statistically significant difference in the age of respondents among the analyzed groups. The use of curcumin at a dose of 400mg per day during one year has statistically significantly improved ultrasound morphological characteristics of liver in subjects with METS. Changes in morphological liver appearance were more pronounced in respondents with METS and DM type 2 than others.
Footnotes
• Conflict of interest: none declared.
• Authors contribution: All authors have equally contributed to this paper in terms of concept and design, drafting and gave their final approval.
REFERENCES
- 1.Zimmet P, Alberti G. The IDF definition why we need a global consesus. Diabetes Voice. 2006;51:11–14. [Google Scholar]
- 2.Saely CH, Koch L, Schmid F, Marte T, Aczel S, Langner P, et al. Adult Treatment Panel III 2001 but not International Diabetes Federation 2005 Criteria of the Metabolic Syndrome Predict Clinical Cardiovascular Events in Subjects who Underwent Coronary Angiography. Diabete Care. 2006;29:901–7. doi: 10.2337/diacare.29.04.06.dc05-2011. [DOI] [PubMed] [Google Scholar]
- 3.International Diabetes Federation: The IDF consensus worldwide definition of the metabolic syndrome 2005. Available from http://www.idf.org/webdata/docs/Metabolic _syndrome_definition.pdf .
- 4.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WPT, Loria CM, Smith SC. Harmonizing the Metabolic Syndrome. Circulation. 2009;120:1640–45. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 5.Medina J, Fernandez-Salazar LI, Garcia-Buey L, Moreno-Otero R. Approach to the pathogenesis and treatment of nonalcoholic steatohepatitis. Diab Care. 2004;27:2057–66. doi: 10.2337/diacare.27.8.2057. [DOI] [PubMed] [Google Scholar]
- 6.Beneš-Mirić S. Atlas ultrazvučne dijagnostike abdomena: Difuzne promjene jetre. 1. izd. Tuzla: Printcom; 2002. pp. 38–54. [Google Scholar]
- 7.Ammon HP, Wahl MA. Pharmacology of Curcuma longa. Planta Med. 1991;57:1–7. doi: 10.1055/s-2006-960004. [DOI] [PubMed] [Google Scholar]
- 8.Lampe V, Milobedzka J. No title available. Ber Dtsch Chem Ges. 1913;46:2235. [Google Scholar]
- 9.Sharma OP. Antioxidant activity of curcumin and related compounds. Biochem Pharmacol. 1976;25:1811–12. doi: 10.1016/0006-2952(76)90421-4. [DOI] [PubMed] [Google Scholar]
- 10.Negi PS, Jayaprakasha GK, Jagan Mohan Rao L, Sakariah KK. Antibacterial activity of turmeric oil: a byproduct from curcumin manufacture. J Agric FoodChem. 1999;47:4297–4300. doi: 10.1021/jf990308d. [DOI] [PubMed] [Google Scholar]
- 11.Jurenka JS. Anti-inflammatory Properties of Curcumin, a Major Constituent of Curcuma longa: A Review of Preclinical and Clinical Research. Altern Med Rev. 2009;14(2):141–153. [PubMed] [Google Scholar]
- 12.Garcea G, Berry DP, Jones DJ, et al. Consumption of the putative chemopreventive agent curcumin by cancer patients: assessment of curcumin levels in the colorectum and their pharmacodynamic consequences. Cancer Epidemiol Biomarkers Prev. 2005;14:120–5. [PubMed] [Google Scholar]
- 13.Camilleri M. Dyspepsia, irritable bowel syndrome, and constipation: review and what’s new. Rev Gastroenterol Disord. 2001;1:2–17. [PubMed] [Google Scholar]
- 14.Barbara G, De Giorgio R, Stanghellini V, et al. A role for inflammation in irritable bowel syndrome? Gut. 2002;5:41–4. doi: 10.1136/gut.51.suppl_1.i41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gukovsky I, Reyes CN, Vaquero EC, et al. Curcumin ameliorates ethanol and nonethanol experimentalpancreatitis. Am J Physiol Gastrointest Liver Physiol. 2003;284:G85–G95. doi: 10.1152/ajpgi.00138.2002. [DOI] [PubMed] [Google Scholar]
- 16.Isomaa B, Almgrem P, Tuomi T, et al. Cardiovascular morbiditi and mortality asociated with the metabolic syndrome. Diabetes Care. 2001;24:683–9. doi: 10.2337/diacare.24.4.683. [DOI] [PubMed] [Google Scholar]
- 17.Ford ES, Giles WH, Dietz WH. Prevalence metabolic syndrome amnog US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287:356–9. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 18.Hanley AJ, Karter AJ, Festa A. i sar. Factor analysis of metabolic syndrome using directly measured insulin sensitivity: The Insulin Resistance Atherosclerosis Study. Diabetes. 2002;51:2642–7. doi: 10.2337/diabetes.51.8.2642. [DOI] [PubMed] [Google Scholar]
- 19.Zang DW, Fu M, Gao SH, Liu JL. Curcumin and Diabetes: A Systematic Review. Evidence-Based Complementary and Alternative Medicine. 2013:16. doi: 10.1155/2013/636053. Article ID 636053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chuengsamarn S, Rattanamongkolgul S, Luechapudiporn R, Phisalaphong C, Jirawatnotai S. Curcumin Extract for Prevention of Type 2 Diabetes. Diabetes Care. 2012;35(11):2121–7. doi: 10.2337/dc12-0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kuroda M, Mimaki Y, Nishiyama T, et al. Hypoglycemic effects of turmeric (Curcuma longa L. rhizomes) on genetically diabetic KK-Ay mice. Biological and Pharmaceutical Bulletin. 2005;28(5):937–9. doi: 10.1248/bpb.28.937. [DOI] [PubMed] [Google Scholar]
- 22.Nishiyama T, Mae T, Kishida H, et al. Curcuminoids and sesquiterpenoids in turmeric (Curcuma longa L.) Suppress an increase in blood glucose level in type 2 diabetic KK-Aγmice. Journal of Agricultural and Food Chemistry. 2005;53(4):959–63. doi: 10.1021/jf0483873. [DOI] [PubMed] [Google Scholar]
- 23.Aggarwal BB, Sethi G, Baladandayuthapani V, Krishnan S, Shishodia S. Targeting cell signaling pathways for drug discovery: an old lock needs a new key. J Cell Biochem. 2007;102:580–92. doi: 10.1002/jcb.21500. [DOI] [PubMed] [Google Scholar]
- 24.Weisberg SP, Leibel R, Tortoriello TV. Dietary curcumin significantly improves obesity-associated inflammation and diabetes in mouse models of diabesity. Endocrinology. 2008;149(7):3549–58. doi: 10.1210/en.2008-0262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prentki M, Madiraju SRM. Glycerolipid metabolism and signaling in health and disease. Endocrine Reviews. 2008;29(6):647–76. doi: 10.1210/er.2008-0007. [DOI] [PubMed] [Google Scholar]
- 26.Fu Y, Zheng S, Lin J, Ryerse J, Chen A. Mol Pharmacol. 2008;73(2):399–409. doi: 10.1124/mol.107.039818. [DOI] [PubMed] [Google Scholar]
- 27.Genuth S, Alberti KG, Bennett P, Buse J, Defronzo R, Kahn R, Kitzmiller J. and all. Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2003 Nov;26(11):3160–7. doi: 10.2337/diacare.26.11.3160. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organisation: Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia -Report of a WHO/IDF consultation. Geneva: 2006. [Google Scholar]


