Abstract
The importance of high blood pressure (BP) and the effect of BP lowering in older adults remain controversial due to the mixed evidence in this population. Frailty status may resolve the apparently conflicting findings and identify subpopulations who share common risk. Emerging evidence demonstrates that low BP is associated with poor outcomes in older frail adults or those with poor functional status. In contrast, in non-frail older adults, low BP appears beneficial. Frail older adults may be at increased risk of hypotension, serious fall injuries, and polypharmacy. Additionally, peripheral BP may not be the best prognostic measure in this population. The majority of clinical practice guidelines give little recommendation for frail older adults, which is likely due to their systematic underrepresentation in randomized controlled trials. Future studies need to consider modifications to safely include frail older adults, and guidelines should consider inclusion of evidence beyond randomized controlled trials.
Keywords: Aged, frailty, physical function, cognitive function, antihypertensive medications, falls
INTRODUCTION
Over 70% of U.S. adults aged 65 years and older have high blood pressure (BP), and the prevalence increases with age.[1] High BP is associated with increased risk of stroke, coronary heart disease, peripheral arterial disease, kidney disease, and many other adverse outcomes.[2] Despite its high prevalence and high morbidity, the importance of high BP and the effect of BP lowering in older adults remain controversial.[3] One of the primary factors driving this controversy is the inconsistent evidence for an association of high BP with adverse outcomes in older adults. A major challenge of research in older adults is that heterogeneity is one of the hallmarks of this population. In any age group, older adults are a mix of those who are thriving, and those who are frail and potentially nearing death.[4] This heterogeneity makes the study of risk in older adults challenging, as population-level effects may be eclipsed by the variability within populations. Apparently conflicting results of prior studies may be due to the fact that older adults are not one population, but, rather several populations where the association between BP and outcomes differs between the subgroups. Frailty status may be one measure to identify these subpopulations and identify those who share common risk.
In this review, we summarize the recent evidence on frailty as it relates to high BP and outcomes in older adults. We focused on articles published in the last three years, with exception made for seminal works or those that provide important context. We aim to highlight novel advances in the field and illuminate areas of uncertainty for future study.
LOW BP AND ADVERSE OUTCOMES IN OLDER ADULTS
Over 25 years ago, Matilla et al. reported that, among adults living in Finland aged ≥ 85 years, those with systolic BP ≥ 160 mmHg had over twofold lower rates of death compared to persons with levels of 120-140 mmHg. [5] Contemporary studies continue to confirm an association between low BP and adverse outcomes in some older populations. Recently in the Leiden 85-plus Study, a cohort study of 271 Swedish men and women aged 85 years at baseline, investigators found that falling and low systolic BP < 150 mmHg were associated with increased risk of mortality.[6] The association of falling BP and mortality was stronger in institutionalized participants, suggestive of an exaggerated risk in frail older adults. Other studies have reported null or harmful effects of low BP at younger ages and for a variety of hard cardiovascular outcomes. In the Secondary Manifestations of Arterial Disease Study, a cohort of 5,788 participants with symptomatic vascular disease, there was no association between higher systolic or diastolic BP and vascular events (stroke, myocardial infarction or vascular death) or all-cause mortality in adults older than 65 years.[7] The MOnica, Risk, Genetics, Archiving, and Monograph (MORGAM) Project included 68,551 participants aged 19-78 years from 34 European cohorts with baseline between 1982 and 1997. In a 2012 paper, the authors reported lower diastolic BP below 71 mmHg was associated with an increased risk of stroke among participants aged 50 and older.[8]
Low BP has also been associated with poor function and low quality of life. Also in the Leiden 85, Sabayan et al. reported that higher systolic BP was associated with lower level of disability on the activities of daily living (ADL) and reduced probability of worsening disability. Higher systolic and diastolic BP were associated with higher cognitive function, and slower declines in Mini-Mental State Examination (MMSE) scores.[9] A recent study of memory clinic patients found an association between low daytime systolic BP (≤128 mmHg) and worse change in MMSE among those treated with antihypertensive therapy.[10] Finally, a recent study of dialysis patients, a population with high prevalence of frailty and functional impairment, demonstrated that those with predialysis systolic BP of 130 mmHg or higher had better physical performance compared with those with lower BP.[11] These findings suggest that excessive BP lowering may be detrimental in older adults with poor physical or cognitive function.
Despite a multitude of studies that have demonstrated an association between low BP and poor outcomes, two large meta-analyses have reported a linear association between BP and cardiovascular outcomes, across the age spectrum. The Prospective Studies Collaboration, a meta-analysis of individual data for one million adults, included participants in 61 cohort studies aged 40-89 years.[12] The investigators reported that the association of higher BP and vascular mortality was linear down to a BP of 115/75 mmHg, across all ages. More recently, the CArdiovascular research using LInked Bespoke studies and Electronic health Records program analyzed data from 1.25 million patient records.[13] In this study, the authors reported a linear association between blood pressure and nearly all of 12 cardiovascular outcomes, across all ages. Although both meta-analyses examined these associations across the age spectrum, they did not examine whether they were robust across functional status. The discordance with literature demonstrating a non-linear between BP and outcomes may be due to the pooling of data across heterogeneous subgroups of older adults. As a whole, the association may appear linear, although when broken into subgroups, differential patterns of association may exist.
OBSERVATIONAL EVIDENCE ON BP, FRAILTY, AND OUTCOMES
Frailty is an aging-related clinical syndrome described as a lack of resiliency and functional reserve, as well as a decreased ability to maintain physiological homeostasis under the onslaught of external stressors. Fried, et al., presented a frailty phenotype based on five criteria: unintentional weight loss, exhaustion, weakness, low physical activity, and slow gait speed.[14] Frail individuals are at increased risk for adverse health outcomes, including increased morbidity, mortality, falls, and hospitalization.[14, 15]
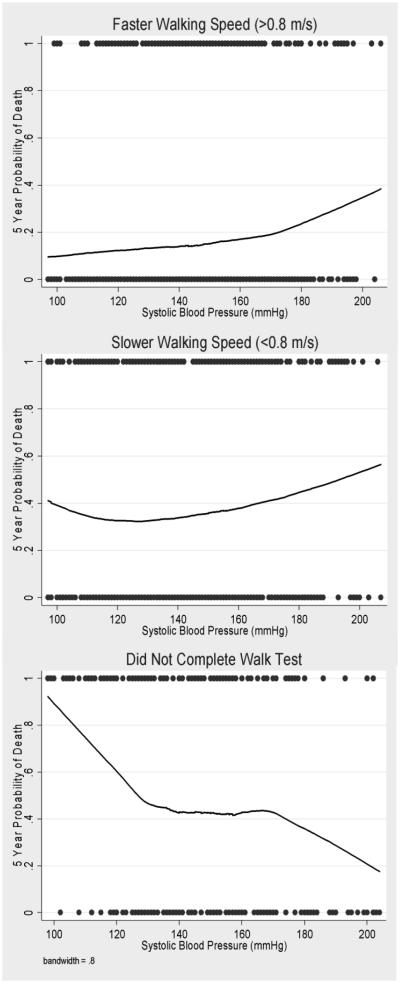
Recently, a preponderance of evidence has emerged that has illustrated that the association of BP and events is attenuated or inverted among frail older adults or those with poor functional status. In the National Health and Nutrition Examination Survey, we examined the association between BP and all-cause and cardiovascular mortality in persons aged 65 years and older.[16] Based on usual walking speed in a 20-ft corridor, we categorized participants into three groups: faster walkers (gait speed ≥0.8 m/s), slower walkers (<0.8 m/s), and those who did not complete the walk. We found that the association between BP and mortality varied significantly by walking speed, and three distinct patterns emerged. (Figure) Among fast walkers, persons with high systolic BP had a 35% (95% confidence interval [CI]: 3 - 77%) higher risk of death compared with those with BP <140 mmHg. In contrast, there was no association between systolic BP and mortality among the slow walkers. Interestingly, among persons who did not complete the test, higher systolic BP was associated with a 62% (95% CI: 38-77%) lower risk of death. Persons who did not complete the test also had the highest prevalence of comorbidities. These findings remained robust after multivariable adjustment, and across several sensitivity analyses including the exclusion of deaths in the first year of follow-up. We have published similar findings using self-reported walking speed in elderly Latinos participating in the Sacramento Area Latino Study on Aging (SALSA).[17] In this population, there was a significant interaction between systolic BP and walking speed for the outcome of all-cause mortality. These findings suggest that these patterns of associations are present across diverse populations.
Figure.
The association of systolic blood pressure and mortality, stratified by gait speed, in NHANES (1999-2002). Lines were derived by locally weighted regression.
Peralta et al. was the first to extend this hypothesis to include cardiovascular events.[18] In the Cardiovascular Health Study (CHS), a cohort study of adults aged 65 and older, the association of diastolic BP with incident cardiovascular events varied by the presence of ADL limitation (p for interaction 0.05). Among persons with ≥ 1 ADL limitation, a lower diastolic BP was associated with higher risk for incident CV events. Compared to persons with diastolic BP ≤ 65 mmHg, the HR for incident CV events was 0.65 (95% CI: 0.44, 0.96) for diastolic BP 66-80 mmHg and 0.49 (95% CI: 0.25, 0.94) for diastolic BP > 80 mmHg. In contrast, among persons without ADL limitation, the association of DBP > 80 mmHg and incident CV events was in the harmful direction (HR = 1.04 (95% CI: 0.79, 1.37)) compared to diastolic BP ≤ 65 mmHg.
Researchers from the Leiden 85 Study have reported parallel findings for risk of stroke.[19] In this cohort of 513 participants aged 85 years old, cognitive function was measured by the MMSE and investigators also assessed ADL. Among subjects with impaired ADL, higher systolic BP (HR, 0.74 [95% CI, 0.59–0.92]), mean arterial pressure (HR: 0.68 [95% CI, 0.47–0.97]), and pulse pressure (HR, 0.71 [95% CI, 0.55–0.93]) were associated with lower risk of stroke. Similarly, among participants with impaired cognitive functioning, higher systolic BP was associated with reduced risk of stroke (HR, 0.80 [95% CI, 0.65–0.98]). In contrast, in those subjects with preserved cognitive functioning, higher diastolic BP (HR: 1.98 [95% CI, 1.21–3.22]) and mean arterial pressure (HR, 1.70 [95% CI, 1.08–2.68]) were associated with higher risk of stroke. The patterns were similar in those without ADL impairment although the effect size did not reach statistical significance. Also in this cohort, investigators reported the association between higher SBP and slower annual decline in MMSE scores was strongest in persons with high ADL disability.
A limitation of prior studies is that none have examined the explicit role of BP treatment in frail populations, However, two of the studies stratified by antihypertensive medication use and found a slightly stronger inverted association between BP and outcomes in those participants on treatment, although the stratified samples were small. [16, 18] Whether treatment to lower BP is associated with benefit or an excess of harm remains to be answered. A recent study in elderly residents of nursing homes may shed some light on this topic. In the Predictive Values of Blood Pressure and Arterial Stiffness in Institutionalized Very Aged Populations (PARTAGE) study, investigators found that a low systolic BP (<130 mmHg) was associated with mortality only among persons who were receiving two or more medications.[20] There was no association of low systolic BP and mortality among participants receiving no or one medication. This interesting observational study suggests that in nursing home residents, who are likely to be frail, the combination of multiple medications and lower BP may be associated with harm.
THE ROLE OF RANDOMIZED CONTROLLED TRIALS
The obvious question remains, why not look at the effect of antihypertensives in frail older adults in randomized controlled trials? Yet the problem is that frail older adults are systematically underrepresented in clinical trials, which remain the mainstay of evidence for the development of clinical practice guidelines. Sardar and colleagues reported that the mean patients’ age was 75 years and older in only 2% of the 653 trials included in the American College of Cardiology/American Heart Association guidelines for atrial fibrillation, heart failure, and acute coronary syndrome.[21] A recent comparative study of participants in an observational study and those in a clinical trial found that older participants differed from age-norms of activity, suggesting that older study participants are less representative compared with younger participants.[22] Additionally, the vast majority of randomized controlled trials exclude institutionalized individuals and those with a life-threatening chronic health condition. While these criteria may be in place to ensure the safety of the participant, as well as to improve the feasibility of completion of the trial, they result in systematic underrepresentation of frail older adults and those with complex comorbid health conditions.
The Hypertension in the Very Elderly Trial (HYVET) demonstrated a strong protective effect of antihypertensive therapy to a target of 150/90 mmHg on stroke, heart failure, and cardiovascular and all-cause mortality in adults aged 80 years and older.[23] Yet even with the high BP required as inclusion criteria for HYVET, participants had one-half to one-quarter the prevalence of chronic health conditions associated with hypertension compared with participants aged 80 years and older in NHANES.[24] Additionally, a recent meta-analysis of treatment of hypertension in adults 80 years and older found significant heterogeneity between HYVET and other trials.[25] Despite the strong protective effect observed in HYVET, the overall estimate for the effect of treatment of hypertension on all-cause mortality in this meta-analysis was null (HR = 1.06, 95% CI: 0.89, 1.25).
Although no trial has been designed to evaluate the effectiveness of BP lowering across frailty status, the Systolic Blood Pressure Intervention Trial (SPRINT) may help gain some clarity.[26] The study population included oversampling for blacks, aged 75 years and older, and chronic kidney disease, all of which are associated with a disproportionately high burden of frailty. In addition, the SPRINT protocol included extensive physical and cognitive measures which will enable for the evaluation of the functional health of the population. It remains to be determined whether there will be sufficient sample size for a post-hoc analysis of treatment effects by frailty status.
MECHANISMS
Substantial literature has debated the mechanism mediating the association of low BP and poor outcomes in older adults.[3, 27-32] Some have proposed that older or frail adults are more likely to have chronic health conditions that lead to low BP, such as heart or renal failure, and these chronic health conditions also increase the risk of morbidity and mortality. In other words, there is the presence of confounding by poor health. While this relationship certainly explains some of the association of low BP and poor outcomes, there is substantial evidence that indicates there are other contributing factors.
Alterations in vascular structure and function accompany the aging process in most adults. Increased vascular stiffness may result from atherosclerosis, arterial calcification, endothelial dysfunction, and smooth muscle cell fibrosis.[33] Because stiffening of the arteries can lead to faster pulse wave velocity, the reflection of the waveform can result in an augmented systolic pressure peak and increase in pulsatile flow. This wave augmentation disproportionately affects systolic BP compared with diastolic BP, leading to a higher prevalence of isolated systolic hypertension and higher pulse pressure amplification in older age. Additionally, the increase pulsatile flow can become turbulent, and shear stress patterns can exacerbate endothelial dysfunction and inflammation.
One explanation for the association of low BP and poor outcomes is that peripheral BP is not the optimal measure for determining cardiovascular risk in older frail adults. Changes in vascular characteristics may make it difficult to determine whether or not peripheral pressure (typically taken in brachial area) can accurately reflect central pressure, which is the pressure observed by the vital organs. There is growing interest in understanding whether non-invasive measurement of central pressure parameters can improve risk stratification in older adults. Emerging research has aimed at identification of whether alternative BP parameters may have stronger prognostic value in frail older adults. The PARTAGE study is one of the first large-scale studies to examine the role of BP and pulse pressure amplification, defined as the percentage increase in pulse pressure in the brachial artery relative to central, and cardiovascular events in nursing home residences. Benetos et al. have reported that the ratio of pulse pressure amplification has a stronger prognostic value compared to standard BP measurements.[34]
More accurate and reliable methods to evaluate central BP are of key importance in older adults because low central BP has been proposed as one causal mechanism by which low measured BP could lead to poor outcomes. It has been hypothesized that low BP could lead to inadequate perfusion of the central organs, most importantly the heart, which is perfused during diastole. Potential adverse effects may be exacerbated in persons with already limited coronary perfusion. Several studies have demonstrated evidence of a J-shaped association between diastolic BP and coronary outcomes,[35] but this remains an issue of active debate.
Another physiologic change that accompanies aging is a decrease in autonomic function and baroreflex sensitivity, leading to a loss of ability to adapt to changing BP. Orthostatic hypotension has been suggested to be a marker of frailty. In 1,347 participants in the Canadian Study of Health and Aging, Rockwood et al. found that orthostatic hypotension was associated with mortality, but this was no longer significant after adjustment for frailty.[36] The authors suggested that frailty may be a preferred measure of vascular system dysregulation compared with orthostatic hypotension due to the transient nature and challenges of accurately measuring orthostatic hypotension. Whether these changes are associated with increased susceptibility to medication-associated adverse effects is uncertain.
There is a preponderance of literature that has examined a link between BP and falls and fall injuries; this could be another mechanism mediating the association between low BP and poor outcomes. In an Austrian study of 3,544 community-dwelling men and women, researchers found that higher systolic and diastolic BP was associated with a lower risk of falls [37] Tinetti et al. reported an elevated risk of serious fall injury among older adults on antihypertensive medication use. The risks were exacerbated among persons with previous fall injury.[38] Others have examined a transitory increase in risk. In a large administrative health care database in Canada, investigators reported a 43% increased risk of hip fracture in the first 45 days following antihypertensive treatment initiation.[39] Another study found an increased risk of hip fracture during the first 7 days after a loop diuretic initiation.[40] In addition to being a severe adverse event, a serious fall injury resulting in hospitalization could initiate a cascade of poor health in frail older adults that could result in additional morbidity or even death.
CONCLUSIONS AND RECOMMENDATIONS
The evidence overwhelmingly suggests that pharmacologic BP lowering may have limited benefit in older adults who are frail, and it may have unintended consequences including increased risk of adverse outcomes and serious fall-related injuries. Adverse effects may be exacerbated in a frail population who are physiologically vulnerable and have low resilience to stressors. Furthermore, older adults’ willingness to take medication for cardiovascular prevention is extremely sensitive to the probability of adverse effects.[41] Additionally, approximately 40% of adults aged 65 years and older are on 5 or more medications, so the potential for polypharmacy is increased with the treatment of hypertension, which often requires two or more antihypertensive agents to reach goal levels.[42] More data are needed to better understand the relative balance of benefits and harms of pharmacologic BP lowering in frail older adults.
Several major professional groups have highlighted the lack of evidence guiding therapeutic management of hypertension, especially in frail older adults or those with multiple chronic health conditions.[43-45] The 2013 European Society of Hypertension and European Society of Cardiology (ESH/ECC) guideline suggests that treatment decisions in frail older adults should be made by the treating physician and “based on monitoring of the clinical effects of the treatment.”[46] While it is a strength that the guideline recognizes that frail older adults may have differing needs, this vague recommendation leaves ample room for confusion and variable practice patterns. One group has published a consensus guideline specifically targeting frail older adults.[47] The members of the Dalhousie Academic Detailing Service (DADS) and the Palliative and Therapeutic Harmonization (PATH) program give recommendations for both initiating and stopping antihypertensive therapy in older frail adults. (Box 1) Although these recommendations are made on the best available evidence, the list of questions regarding the optimal BP in older frail adults remains much longer than the list of answers. In a recent review article focusing on the oldest old, Muller et al. summarizes several research questions regarding the treatment of hypertension in individuals aged 80 years and older.[33] (Box 2)
Box 1. Summary of recommendations for treating hypertension in the frail elderly from a Canadian professional group [47].
Stop or decrease antihypertensive medications if systolic BP is below 140 mmHg and the medication is not indicated for another condition.
Initiate or increase treatment if systolic BP is 160 mmHg or higher
Treat to a target systolic BP of 140 to 160 mm Hg
In the very frail with a short life expectancy, a target systolic BP of 160 to 190 mmHg is reasonable
In general, use no more than two medications
Box 2. Selected Research Questions on Treatment of Hypertensive Individuals Aged >80 Years from Muller et al. [33].
Is a target reduction in systolic BP (eg, 10–20 mm Hg) more beneficial than a target level of systolic BP (eg, 140–150 mm Hg) and diastolic BP (eg, 70–75 mm Hg)?
Is the use of >2 antihypertensives safe and effective in fit individuals?
What are the preferred first and second line antihypertensive treatments?
Do surrogate end points exist that accurately predict beneficial effects of antihypertensive treatment?
What factor(s) related to frailty or biological age can most precisely predict the lack of clinical benefit of antihypertensive treatment?
What are the characteristics of those oldest old in whom higher BP levels are beneficial?
Is a severely reduced estimated GFR an argument in favor (to decrease the risk of end-stage renal disease) or against (to avoid adverse effects) drug treatment?
Why is antihypertensive treatment not beneficial in the frail?
Is reduction or withdrawal of antihypertensives beneficial in frail older patients, in patients exposed to polypharmacy, or in patients with diastolic BP <70 mm Hg or orthostatic hypotension?
Is reduction or withdrawal of antihypertensives beneficial when renal function worsens during such treatment (eg, a fall in estimated GFR >10%–20%)?
What parameter(s) of orthostatic hypotension is (are) most strongly related to clinically important outcomes?
Is either short-term BP variability as derived from 24-hour recordings or longer term variability such as expressed in visit-to-visit variability of blood pressure a risk factor in the oldest old?
Based this review of the literature, we have identified eight priority questions regarding the treatment of high BP in frail older adults.
What is the optimal range for BP in frail older adults for prevention of myocardial infarction, stroke, heart failure, and mortality?
What is the optimal range for BP in frail older adults for preservation of physical and cognitive health?
Should there be a lower threshold for diastolic BP, at which BP treatment should be de-intensified?
Does change in BP (both natural and pharmacologic) affect risk of events?
What are the risks of orthostatic hypotension, hypotension-related symptoms, falls, and fall-related injuries in frail older adults on antihypertensives?
Do risks increased linearly with the number of antihypertensive agents or is there a threshold effect at which risk is increased (i.e. ≥ 2 medications)?
What is the best marker or markers to identify the older population who will benefit from BP lowering?
Should comorbidities such as diabetes or chronic kidney disease be considered in frail adults when deciding on BP targets?
Aside from the DADS/PATH guideline, clear recommendations for how to treat BP in older frail adults are lacking. One of the unintended side effects of “raising the bar” for the quality of evidence included in evidence-based practice guidelines is that frail older adults are systematically underrepresented.[48] High-quality evidence, which is considered to only come from randomized controlled trials with hard outcomes, has not included frail older adults, for a mix of ethical, scientific, and logistical considerations. A classic randomized controlled trial with a washout period prior to randomization may subject this vulnerable population to potentially harmful fluctuations in BP and the possible risk of falls that accompany antihypertensive initiation. Additionally, frail older adults may not safely be able to complete the study protocol or there may be concerns about informed consent in persons with cognitive impairment. Finally, the presence of multiple chronic health conditions and competing risks may increase heterogeneity and limit the power to identify beneficial treatment effects, as well as increasing the potential harms. Although some of these concerns can be attenuated with thoughtful modifications, we have not yet been able to bridge the gap to include a truly representative sample of older adults in randomized clinical trials. This review demonstrates the trouble with this lack of representativeness because the benefit of BP lowering and the potential harms of treatment appear to vary by frailty and functional status.
Evidence-based clinical practice guidelines will need to be adapted to incorporate evidence beyond traditional randomized controlled trials for frail older adults. We propose that study designs that evaluate the above research questions and others in frail populations will need to be sensitive to the unique needs of this population. A treatment de-intensification trial may prove to be more appropriate compared with a classic randomized controlled trial for many research questions. In this design, patients could be randomized to less medication or a less intensive target, and carefully monitored for cardiovascular outcomes as well as functional status and quality of life outcomes. Additionally, in areas of uncertain evidence, patient preferences have increased weight, and also need to be taken into account. This means that pragmatic trials, or observational evidence may need to be used to answer some research questions. This is especially true for subpopulations of frail older adults, or those with multiple chronic health conditions. Creative scientific approaches need to be applied to most effectively address the question of treatment of hypertension in this complex population, along with multi-disciplinary teams to address the myriad of clinical, ethical, methodologic, and logistical issues that will be faced in this complex population. Only then will we be able to bridge the gap in guidelines for the treatment of this growing and vulnerable population.
ACKNOWLEDGMENTS
Support for this research was provided by the National Institute on Aging (K01AG039387, R01AG46206).
REFERENCES
- 1.McDonald M, Hertz RP, Unger AN, et al. Prevalence, awareness, and management of hypertension, dyslipidemia, and diabetes among United States adults aged 65 and older. J Gerontol A Biol Sci Med Sci. 2009;64(2):256–63. doi: 10.1093/gerona/gln016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 3.Goodwin JS. Embracing complexity: A consideration of hypertension in the very old. J Gerontol A Biol Sci Med Sci. 2003;58(7):653–8. doi: 10.1093/gerona/58.7.m653. [DOI] [PubMed] [Google Scholar]
- 4.Diehr P, Williamson J, Burke GL, et al. The aging and dying processes and the health of older adults. J Clin Epidemiol. 2002;55(3):269–78. doi: 10.1016/s0895-4356(01)00462-0. [DOI] [PubMed] [Google Scholar]
- 5.Mattila K, Haavisto M, Rajala S, et al. Blood pressure and five year survival in the very old. Br Med J. 1988;296(6626):887–9. doi: 10.1136/bmj.296.6626.887. (Clin Res Ed) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Poortvliet RK, de Ruijter W, de Craen AJ, et al. Blood pressure trends and mortality: the Leiden 85-plus Study. J Hypertens. 2013;31(1):63–70. doi: 10.1097/HJH.0b013e32835aa351. [DOI] [PubMed] [Google Scholar]
- 7.Dorresteijn JA, van der Graaf Y, Spiering W, et al. Relation between blood pressure and vascular events and mortality in patients with manifest vascular disease: J-curve revisited. Hypertension. 2012;59(1):14–21. doi: 10.1161/HYPERTENSIONAHA.111.179143. [DOI] [PubMed] [Google Scholar]
- 8.Vishram JK, Borglykke A, Andreasen AH, et al. Impact of age on the importance of systolic and diastolic blood pressures for stroke risk: the MOnica, Risk, Genetics, Archiving, and Monograph (MORGAM) Project. Hypertension. 2012;60(5):1117–23. doi: 10.1161/HYPERTENSIONAHA.112.201400. [DOI] [PubMed] [Google Scholar]
- 9.Sabayan B, Oleksik AM, Maier AB, et al. High blood pressure and resilience to physical and cognitive decline in the oldest old: the Leiden 85-plus Study. J Am Geriatr Soc. 2012;60(11):2014–9. doi: 10.1111/j.1532-5415.2012.04203.x. [DOI] [PubMed] [Google Scholar]
- 10.Mossello E, Pieraccioli M, Nesti N, et al. Effects of low blood pressure in cognitively impaired elderly patients treated with antihypertensive drugs. JAMA Intern Med. 2015;175(4):578–85. doi: 10.1001/jamainternmed.2014.8164. [DOI] [PubMed] [Google Scholar]
- 11.Abreo AP, Glidden D, Painter P, et al. Association of physical function with predialysis blood pressure in patients on hemodialysis. BMC Nephrol. 2014;15:177. doi: 10.1186/1471-2369-15-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–13. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 13.Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet. 2014;383(9932):1899–911. doi: 10.1016/S0140-6736(14)60685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–56. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 15.Rockwood K, Stadnyk K, MacKnight C, et al. A brief clinical instrument to classify frailty in elderly people. Lancet. 1999;353(9148):205–6. doi: 10.1016/S0140-6736(98)04402-X. [DOI] [PubMed] [Google Scholar]
- 16.Odden MC, Peralta CA, Haan MN, et al. Rethinking the association of high blood pressure with mortality in elderly adults: the impact of frailty. Arch Intern Med. 2012;172(15):1162–8. doi: 10.1001/archinternmed.2012.2555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Odden MC, Covinsky KE, Neuhaus JM, et al. The association of blood pressure and mortality differs by self-reported walking speed in older Latinos. J Gerontol A Biol Sci Med Sci. 2012;67(9):977–83. doi: 10.1093/gerona/glr245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peralta CA, Katz R, Newman AB, et al. Systolic and diastolic blood pressure, incident cardiovascular events, and death in elderly persons: the role of functional limitation in the cardiovascular health study. Hypertension. 2014;64(3):472–80. doi: 10.1161/HYPERTENSIONAHA.114.03831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sabayan B, van Vliet P, de Ruijter W, et al. High blood pressure, physical and cognitive function, and risk of stroke in the oldest old: the Leiden 85-plus Study. Stroke. 2013;44(1):15–20. doi: 10.1161/STROKEAHA.112.663062. [DOI] [PubMed] [Google Scholar]
- 20.Benetos A, Labat C, Rossignol P, et al. Treatment With Multiple Blood Pressure Medications, Achieved Blood Pressure, and Mortality in Older Nursing Home Residents: The PARTAGE Study. JAMA Intern Med. 2015 doi: 10.1001/jamainternmed.2014.8012. [DOI] [PubMed] [Google Scholar]
- 21.Sardar MR, Badri M, Prince CT, et al. Underrepresentation of women, elderly patients, and racial minorities in the randomized trials used for cardiovascular guidelines. JAMA Intern Med. 2014;174(11):1868–70. doi: 10.1001/jamainternmed.2014.4758. [DOI] [PubMed] [Google Scholar]
- 22.Golomb BA, Chan VT, Evans MA, et al. The older the better: are elderly study participants more non-representative? A cross-sectional analysis of clinical trial and observational study samples. BMJ Open. 2012;2(6) doi: 10.1136/bmjopen-2012-000833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887–98. doi: 10.1056/NEJMoa0801369. [DOI] [PubMed] [Google Scholar]
- 24.Odden MC, Peralta CA, Covinsky KE. Walking speed is a useful marker of frailty in older persons--reply. JAMA Intern Med. 2013;173(4):325–6. doi: 10.1001/jamainternmed.2013.2542. [DOI] [PubMed] [Google Scholar]
- 25.Bejan-Angoulvant T, Saadatian-Elahi M, Wright JM, et al. Treatment of hypertension in patients 80 years and older: the lower the better? A meta-analysis of randomized controlled trials. J Hypertens. 2010;28(7):1366–72. doi: 10.1097/HJH.0b013e328339f9c5. [DOI] [PubMed] [Google Scholar]
- 26.Ambrosius WT, Sink KM, Foy CG, et al. The design and rationale of a multicenter clinical trial comparing two strategies for control of systolic blood pressure: the Systolic Blood Pressure Intervention Trial (SPRINT) Clin Trials. 2014;11(5):532–46. doi: 10.1177/1740774514537404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hajjar I. Commentary on Goodwin's "Embracing complexity: a consideration of hypertension in the very old". J Gerontol A Biol Sci Med Sci. 2003;58(12):M1146–8. doi: 10.1093/gerona/58.12.m1146-a. [DOI] [PubMed] [Google Scholar]
- 28.Newman AB. Commentary on "Embracing complexity: A consideration of hypertension in the very old". J Gerontol A Biol Sci Med Sci. 2003;58(7):666–7. doi: 10.1093/gerona/58.7.m666. discussion 669-70. [DOI] [PubMed] [Google Scholar]
- 29.Michel JP, Grab B, Perrenoud JJ. Commentary on "Embracing complexity: A consideration of hypertension in the very old". J Gerontol A Biol Sci Med Sci. 2003;58(7):665–6. doi: 10.1093/gerona/58.7.m665. discussion 669-70. [DOI] [PubMed] [Google Scholar]
- 30.Lowenthal DT. Commentary on "Embracing complexity: A consideration of hypertension in the very old". J Gerontol A Biol Sci Med Sci. 2003;58(7):664–5. doi: 10.1093/gerona/58.7.m664. discussion 669-70. [DOI] [PubMed] [Google Scholar]
- 31.Hajjar RR. Commentary on "Embracing complexity: A consideration of hypertension in the very old". J Gerontol A Biol Sci Med Sci. 2003;58(7):661–2. discussion 669-70. [PubMed] [Google Scholar]
- 32.Aronow WS. Commentary on "Embracing complexity: A consideration of hypertension in the very old". J Gerontol A Biol Sci Med Sci. 2003;58(7):659–60. doi: 10.1093/gerona/58.7.m659. discussion 669-70. [DOI] [PubMed] [Google Scholar]
- 33.Muller M, Smulders YM, de Leeuw PW, et al. Treatment of hypertension in the oldest old: a critical role for frailty? Hypertension. 2014;63(3):433–41. doi: 10.1161/HYPERTENSIONAHA.113.00911. [DOI] [PubMed] [Google Scholar]
- 34.Benetos A, Gautier S, Labat C, et al. Mortality and cardiovascular events are best predicted by low central/peripheral pulse pressure amplification but not by high blood pressure levels in elderly nursing home subjects: the PARTAGE (Predictive Values of Blood Pressure and Arterial Stiffness in Institutionalized Very Aged Population) study. J Am Coll Cardiol. 2012;60(16):1503–11. doi: 10.1016/j.jacc.2012.04.055. [DOI] [PubMed] [Google Scholar]
- 35.Banach M, Aronow WS. Blood pressure j-curve: current concepts. Curr Hypertens Rep. 2012;14(6):556–66. doi: 10.1007/s11906-012-0314-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rockwood MR, Howlett SE, Rockwood K. Orthostatic hypotension (OH) and mortality in relation to age, blood pressure and frailty. Arch Gerontol Geriatr. 2012;54(3):e255–60. doi: 10.1016/j.archger.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 37.Klein D, Nagel G, Kleiner A, et al. Blood pressure and falls in community-dwelling people aged 60 years and older in the VHM&PP cohort. BMC Geriatr. 2013;13:50. doi: 10.1186/1471-2318-13-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tinetti ME, Han L, Lee DS, et al. Antihypertensive medications and serious fall injuries in a nationally representative sample of older adults. JAMA Intern Med. 2014;174(4):588–95. doi: 10.1001/jamainternmed.2013.14764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Butt DA, Mamdani M, Austin PC, et al. The risk of hip fracture after initiating antihypertensive drugs in the elderly. Arch Intern Med. 2012;172(22):1739–44. doi: 10.1001/2013.jamainternmed.469. [DOI] [PubMed] [Google Scholar]
- 40.Berry SD, Zhu Y, Choi H, et al. Diuretic initiation and the acute risk of hip fracture. Osteoporos Int. 2013;24(2):689–95. doi: 10.1007/s00198-012-2053-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fried TR, Tinetti ME, Towle V, et al. Effects of benefits and harms on older persons' willingness to take medication for primary cardiovascular prevention. Arch Intern Med. 2011;171(10):923–8. doi: 10.1001/archinternmed.2011.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Charlesworth CJ, Smit E, Lee DS, et al. Polypharmacy Among Adults Aged 65 Years and Older in the United States: 1988-2010. J Gerontol A Biol Sci Med Sci. 2015 doi: 10.1093/gerona/glv013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. Circulation. 2011;123(21):2434–506. doi: 10.1161/CIR.0b013e31821daaf6. [DOI] [PubMed] [Google Scholar]
- 44.Gomez-Huelgas R, Giner-Galvan V, Mostaza JM, et al. Unanswered clinical questions in the management of cardiometabolic risk in the elderly: a statement of the Spanish society of internal medicine. BMC Cardiovasc Disord. 2014;14:193. doi: 10.1186/1471-2261-14-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311(5):507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 46.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013;34(28):2159–219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 47.Mallery LH, Allen M, Fleming I, et al. Promoting higher blood pressure targets for frail older adults: a consensus guideline from Canada. Cleve Clin J Med. 2014;81(7):427–37. doi: 10.3949/ccjm.81a.13110. [DOI] [PubMed] [Google Scholar]
- 48.Institute of Medicine (U.S.) Committee on Standards for Developing Trustworthy Clinical Practice Guidelines. In: Graham R, editor. Clinical practice guidelines we can trust. National Academies Press; Washington, DC: 2011. [PubMed] [Google Scholar]