Abstract
Background:
Intra-articular physeal fractures of the distal femur are an uncommon injury pattern, with only a few small case series reported in the literature.
Purpose:
To pool patients from 3 high-volume pediatric centers to better understand this injury pattern, to determine outcomes of surgical treatment, and to assess risk factors for complications.
Study Design:
Case series; Level of evidence, 4.
Methods:
A multicenter retrospective review of all patients presenting with an intra-articular physeal fracture between 2006 and 2016 was performed. Patient demographic and injury data, surgical data, and postoperative outcomes were documented. Radiographs were evaluated for fracture classification (Salter-Harris), location, and displacement. Differences between patients with and without complications were compared by use of analysis of variance or chi-square tests.
Results:
A total of 49 patients, with a mean age of 13.5 years (range, 7-17 years), met the inclusion criteria. The majority of fractures were Salter-Harris type III fractures (84%) involving the medial femoral condyle (88%). Football was responsible for 50% of the injuries. The initial diagnosis was missed in 39% of cases, and advanced imaging showed greater mean displacement (6 mm) compared with radiographs (3 mm). All patients underwent surgery and returned to sport with “good to excellent” results after 2 years. Complications were more common in patients with wide-open growth plates, patients with fractures involving the lateral femoral condyle, and patients who were casted (P < .05).
Conclusion:
Clinicians evaluating skeletally immature athletes (particularly football players) with acute knee injuries should maintain a high index of suspicion for an intra-articular physeal fracture. These fractures are frequently missed, and advanced imaging may be required to establish the diagnosis. Leg-length discrepancies and angular deformities are not uncommon, and patients should be monitored closely. Surgical outcomes are good when fractures are identified, with high rates of return to sport.
Keywords: adolescent knee injury, intra-articular physeal fracture, Salter-Harris type III and IV fractures
Injuries of the knee are common in pediatric and adolescent patients, particularly athletes.2 Although much attention has been focused on soft tissue injuries pertaining to the anterior cruciate ligament (ACL), the medial patellofemoral ligament, and the menisci, bony injuries can also be observed but are relatively rare. In particular, physeal fractures of the distal femur represent less than 1% of physeal injuries.6,12 In 1963, Robert Salter and Robert Harris16 classified physeal fractures using the distal femur and basing the description on the involvement and orientation of the fracture line through the growth plate.
Several unique features of the distal femoral physis create clinical concerns when this structure is injured. The distal femoral physis is the fastest growing physis in the body and is responsible for 35% of longitudinal growth of the lower extremity.13 During peak growth velocity, the distal femoral physis grows approximately 10 to 12 mm per year.2 Additionally, the undulating course of the physis when fractured leads to a complex shearing injury of the growth plate cartilage, which predisposes toward bony bar formation.9 For these reasons, fractures pose significant risk of premature physeal closure, with a subsequent angular deformity and leg-length discrepancy. When a physeal fracture extends into the joint (Salter-Harris type III and IV fractures), several additional complications can occur, placing the patient at increased risk for arthrofibrosis, nonunion, and posttraumatic arthritis.
To date, the literature contains few reports of intra-articular distal femur fractures in the skeletally immature patient, and all of the reports available are relatively small case reports. Anecdotally, we have noticed an increasing frequency of these fractures in our clinics. The purpose of this study was to combine data from 3 high-volume pediatric hospitals to identify common injury patterns, treatment approaches, outcomes, and complications of the management of Salter-Harris type III and IV intra-articular distal femur fractures.
Methods
After internal review board approval was obtained, a retrospective review was performed regarding all intra-articular distal femur fractures presenting to 1 of 3 tertiary care pediatric hospitals. Inclusion criteria included patients younger than 18 years with open physes who had sustained a Salter-Harris type III or IV fracture of the distal femur. Patients with diaphyseal extension of the fracture were excluded.
Patient charts were reviewed, and the following data were documented: age, sex, height, weight, body mass index, extremity side, mechanism of injury, sport of injury, time from injury to diagnosis and treatment, and whether the fracture was initially missed by the original treating practitioner (whether the patient’s primary care physician, an emergency department provider, or the initial orthopaedic surgeon). All radiographic studies were evaluated; fracture displacement, both the intra-articular step-off and gap, was assessed on each radiographic view, which included the anteroposterior (AP), lateral, tunnel, and Merchant views if obtained. Maximal displacement, both gap and step-off, was measured using any advanced imaging (computed tomography [CT] and/or magnetic resonance imaging [MRI]) that was obtained, including the axial, sagittal, and coronal sequences. Associated injuries were documented, including ligamentous injuries, meniscal injuries, and injuries with neurovascular compromise. Patient treatment was recorded; in this series, every patient was treated surgically. The surgical approach was documented including the use of an open arthrotomy, an arthroscopically assisted approach, or a percutaneous technique. The type of fixation and screw configuration was also recorded. We documented the postoperative protocol, including whether the patient was kept nonweightbearing and whether a cast or brace was used. Additionally, the duration of weightbearing restriction and immobilization was documented. Variation existed as to the assessment of limb deformity, with some institutions favoring hip-to-ankle long-leg alignment films on all patients and other institutions favoring a clinical examination and reserving the additional radiographic imaging for patients with a clinically evident leg-length discrepancy or angular deformity.
Outcome measures included achievement of union, return to sport, range of motion restrictions, physical therapy requirement, and the need for additional procedures, including implant removal, subsequent soft tissue procedures, or any deformity correction that was necessary. A good outcome was achieved if fracture union was achieved, the patient had returned to sport, and no functional deficit was present. Differences between patients with and without complications that required further surgical treatment (other than implant removal) or potentially caused long-term issues were compared by analysis of variance (ANOVA) or chi-square test as appropriate. All continuous data were checked for normality and homogeneity of variances prior to use of parametric ANOVA technique. Alpha was set at P < .05 to declare significance, and analyses were performed with SPSS version 24 (IBM Corp).
Results
Between 2006 and 2016, 49 intra-articular distal femur fractures that met our inclusion criteria were identified. Table 1 shows the patient demographic and injury data. The majority of fractures (84%) occurred during adolescence, between the ages of 12 and 16 years, and males predominated (88%). The vast majority were Salter-Harris type III fractures (84%) and involved the medial femoral condyle (88%). A tackle during football was the most common mechanism of injury, responsible for 50% of the fractures. The time from injury to consultation with the orthopaedic team averaged 3.3 days, but 10% of patients were not referred within the first 2 weeks. A large number (39%) of fractures were missed by the initial evaluating physician. Fractures that were nondisplaced or minimally displaced (≤2 mm) were missed in 50% of cases, whereas those displaced more than 2 mm were missed in 31% of cases; however, this was not statistically significant (P < .42). The mean radiographic fracture displacement that was typically best seen on the AP radiograph was 3 mm, but advanced imaging showed greater mean displacement of 6 mm (P = .007). All patients presented with a large knee effusion and a normal neurovascular examination. Concomitant ligament and meniscus injuries were present in 12% of patients.
TABLE 1.
Demographic, Injury, and Treatment Data for the 49 Patientsa
| Age, y | 13.5 ± 2.0 |
| Male sex | 43 (88) |
| Right extremity involvement | 28 (57) |
| Height, cm | 170 ± 11 |
| Weight, kg | 74 ± 24 |
| Body mass index | 25.1 ± 6.2 |
| High energy/contact mechanism | 38 (78) |
| Fracture location | |
| Medial femoral condyle | 43 (88) |
| Lateral femoral condyle | 6 (12) |
| Salter-Harris type | |
| Salter-Harris III | 41 (84) |
| Salter-Harris IV | 8 (16) |
| Time from injury to diagnosis, d | 3.3 ± 5.3 |
| Missed diagnosis | 16 (39) |
| Concomitant injuries | |
| Anterior cruciate ligament | 4 (8) |
| Meniscus | 2 (4) |
| Other fractures | 4 (8) |
| Advanced imaging | 26 (53) |
| Treatment approach | |
| Arthroscopically assisted | 6 (12) |
| Percutaneous | 14 (29) |
| Arthrotomy | 29 (59) |
aData presented as mean ± SD or n (%).
All 49 patients were treated surgically, with 92% receiving a screw-only construct, 4% receiving a plate and screw construct, and 4% receiving a screw and cross-pin Kirschner wire construct. A percutaneous technique was used in 29% of cases, an arthroscopically assisted technique in 12%, and an open arthrotomy in 59%. Variability existed with respect to postoperative protocols, but all patients were kept nonweightbearing for a period of 4 to 8 weeks and a cast was used postoperatively in 41% of patients, whereas a brace was used in the rest of the patients.
At a mean follow-up of 24 months, outcomes were almost uniformly good. Complete radiographic healing was observed in 100% of patients, and all of the athletes returned to full activities. Range of motion was symmetric in 80% of patients. For the remaining 20% of patients who lost range of motion, this tended to be a loss of flexion less than 20°. One patient with significant arthrofibrosis required an arthroscopic lysis of adhesions and manipulation under anesthesia. One year postoperatively, he had range of motion from 0° to 125° and had returned to full sports with no deficits. At final follow-up, a limb-length discrepancy was identified in 14% of patients and averaged 17 mm (range, 7-40 mm) in these patients. An angular deformity was identified in 4 patients (8%), with 2 being varus deformities and 2 being valgus deformities. Second procedures were necessary in 6 patients (12%) for their resultant leg-length discrepancy or angular deformity. Four of these procedures in patients aged 12 to 14 years were contralateral epiphysiodeses. One younger patient who was 8 years of age at the time of injury underwent a limb-lengthening procedure for a nearly 5-cm leg-length discrepancy, and the final patient who was 6.5 years of age at the time of injury underwent a successful bar excision. A concomitant soft tissue injury was identified in 12% of cases, with the majority involving the ACL. Three of the 4 ACL injuries (75%) were partial tears that were treated nonsurgically and had no residual instability after their fractures had healed. One patient with a complete ACL tear underwent a staged reconstruction once the fracture had healed and he had regained motion. In 22% of cases, the patients elected to have their symptomatic implants removed. Complications were more common in patients with open growth plates compared with “closing” growth plates, patients with fractures involving the lateral femoral condyle, and patients who were casted (P < .05) (Table 2).
TABLE 2.
Comparison of Patients With and Without Complicationsa
| With Complication (n = 11) | Without Complication (n = 38) | P Valueb | |
|---|---|---|---|
| Age, y | 12.7 ± 3.0 | 13.8 ± 1.7 | .13 |
| Sex, % male | 73 | 92 | .12 |
| Body mass index | 17.6 ± 4.9 | 26.6 ± 5.4 | .002 |
| Physis open, % | 78 | 22 | .02 |
| Salter-Harris type, % | .06 | ||
| Salter-Harris III | 17 | 83 | |
| Salter-Harris IV | 50 | 50 | |
| Fracture location, % | .03 | ||
| Medial femoral condyle | 13 | 87 | |
| Lateral femoral condyle, % | 50 | 50 | |
| High-energy mechanism, % | 36 | 18 | .24 |
| Initial fracture missed, % | 38 | 24 | .13 |
| Treatment approach, % | .79 | ||
| Arthroscopically assisted | 17 | 83 | |
| Percutaneous | 29 | 71 | |
| Arthrotomy | 21 | 79 | |
| Postoperative casting, % | 40 | 10 | .03 |
aComplication defined as a condition that required further surgical treatment other than implant removal or that potentially caused long-term problems. Data for age and body mass index presented as mean ± SD.
bBoldface values indicate P < .05.
Discussion
Intra-articular fracture of the distal femur is a relatively rare injury pattern in skeletally immature patients, with around 100 cases having been reported in the literature (Table 3).ǁ The current series reporting an additional 49 fractures enables broader conclusions to be reached and statistical analysis to be performed. In general, this fracture is unique to adolescence and occurs when the distal femoral physis is narrowing and starting to close. If this fracture is recognized early, surgical outcomes are good with low complication rates, but patients need to be monitored for premature physeal closure and residual knee laxity. Additionally, when a premature physeal closure is identified early, a guided growth procedure can often eliminate the need for an osteotomy.
TABLE 3.
Summary of Published Studies Regarding Pediatric Intra-articular Distal Femur Fractures
| Salter-Harris Type III | Salter-Harris Type IV | All Fractures | |
|---|---|---|---|
| Rogers et al15 | 7 | 0 | 7 |
| Torg et al19 | 6 | 0 | 6 |
| McKissick et al11 | 3 | 0 | 3 |
| Lippert et al8 | 14 | 0 | 14 |
| Eid and Hafez7 | 19 | 22 | 41 |
| Edmunds and Nade6 | 5 | 2 | 7 |
| Lombardo and Harvey10 | 5 | 3 | 8 |
| Thomson et al18 | 2 | 4 | 6 |
| Riseborough et al14 | 7 | 6 | 13 |
| Czitrom et al5 | 2 | 11 | 13 |
| Bertin and Goble4 | 5 | 1 | 6 |
| Arkader et al2 | 4 | 7 | 11 |
| Current study | 41 | 8 | 49 |
| All studies | 120 | 64 | 184 |
Although several mechanisms of injury were responsible for the various fracture patterns that were observed in our cohort, the vast majority of the Salter-Harris type III fractures involving the medial femoral condyle were the result of a contact injury with a valgus force. This is seen frequently in football players when either the shoulder or helmet of an opposing player impacts the lateral aspect of the knee. Given this common mechanism, this injury has previously been coined a football “clipping injury.”15 This unique fracture pattern shares several key characteristics with a Tillaux fracture, which is an avulsion injury of the anterior inferior tibiofibular ligament resulting in a Salter-Harris type III fracture of the anterolateral distal tibia. Similar to closure of the distal tibia, closure of the distal femoral physis starts centrally and progresses peripherally toward the perichondral ring.17 This asymmetric physeal closure likely explains the age distribution of these fractures, which occur almost exclusively during adolescence. Similar to the anterior inferior tibiofibular ligament in the ankle, the medial collateral ligament and possibly the medial patellofemoral ligament, which attach to the medial epiphysis, are likely responsible for the bony avulsion of the medial femoral condyle, whereas the fibular collateral ligament and the popliteus are likely responsible for the lateral-sided fracture equivalent (Figure 1).
Figure 1.
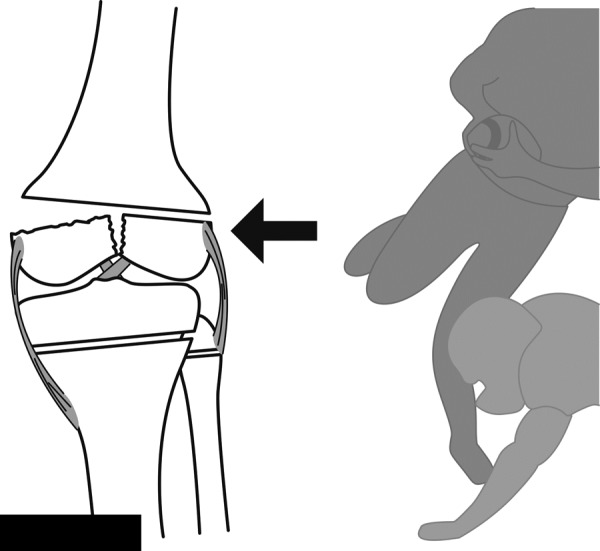
Schematic diagram showing the typical mechanism associated with a Salter-Harris type III fracture. The mechanism includes an avulsion of the medial femoral condyle from the pull of the intact medial structures, including the superficial medial collateral ligament, deep medial collateral ligament, posterior oblique ligament, and medial patellofemoral ligament. Image courtesy of SD PedsOrtho.
Previous studies have shown that intra-articular physeal fractures may be difficult to accurately diagnose and characterize on plain radiographs.15,19 In our series, these fractures were frequently missed by the initial clinician, especially if the fracture was nondisplaced or minimally displaced. Some key steps may improve the physician’s ability to adequately detect these fractures. First, obtaining a knee series with a Merchant and tunnel view is imperative. Many radiographic knee series performed in the emergency department were incomplete and did not include Merchant or tunnel views. For many of the fractures in this series, these views were the only projections that allowed visualization of the fracture. Second, if an adolescent patient presents with a large posttraumatic effusion but no obvious fracture, advanced imaging should be obtained (Figure 2). The results of the current study showed that not only was the advanced imaging more useful for quantifying the degree of fracture displacement, but MRI in particular was helpful in detecting additional soft tissue injuries such as ACL tears. Furthermore, a recent study has shown that the vast majority (approximately 80%) of adolescents presenting with a traumatic effusion will have significant knee abnormalities, including ACL tears, meniscal tears, and patellar dislocations.1 This information, combined with our data, suggests that clinicians should have a low threshold for obtaining an MRI when evaluating a patient with a traumatic knee effusion with no obvious fracture on plain radiographs.
Figure 2.
(A, B) Anteroposterior and lateral radiographs of an adolescent male football player with no obvious fracture visualized on plain radiographs but large effusion best seen in the suprapatellar pouch on the lateral view. (C, D) Coronal and axial computed tomography images confirming the intra-articular fracture and demonstrating how marked displacement can be underrecognized on plain films. Image courtesy of SD PedsOrtho.
In the literature, several studies have shown an association between an intra-articular distal femur fracture and other injuries about the knee.4,7,19 It has therefore been suggested that treating physicians must maintain a high index of suspicion for these combined injuries. In our series, 8% had a concomitant cruciate ligament tear, but only 2% were clinically significant. At our institutions, we treat the cruciate ligament injuries in a delayed fashion. Interestingly, 75% of these ACL injuries did not require additional ligament surgery once the fracture was stabilized and had healed. For the remaining patient with residual instability, a staged reconstruction was performed once the fracture had healed and joint motion had been restored. An important consideration in these cases is the placement of the lag screws relative to the joint and the physis. Screws should be placed anterior to the Blumensaat line to avoid inadvertent screw penetration into the notch and iatrogenic damage to either the ACL or posterior cruciate ligament (Figure 3), but the screws should not be angulated too anteriorly, to avoid penetration into the joint through the sulcus of the trochlea. Additionally, this screw placement will facilitate future femoral tunnel placement in ACL reconstruction and avoid tunnel-screw convergence.
Figure 3.
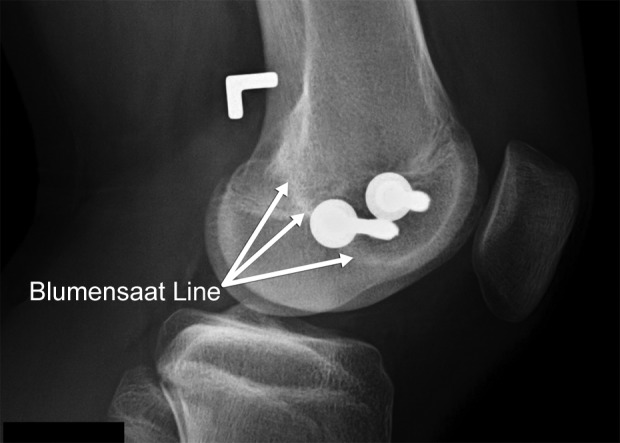
Lateral radiograph depicting proper lag screw placement anterior to the Blumensaat line, avoiding inadvertent notch penetration. Image courtesy of SD PedsOrtho.
Although reported in the literature,3,7,14 late fracture displacement was not observed in this series, likely due to the aggressive surgical treatment at our institutions. From our data, it is not clear what percentage of the nondisplaced or minimally displaced fractures would have healed with a period of immobilization and observation. Nonetheless, we favor surgery because it is technically easy; it can be performed percutaneously or arthroscopically when the fracture is minimally displaced; it enables early mobilization, helping to avoid arthrofibrosis; and it leads to predictable healing. Perhaps most important, surgical stabilization of these fractures prevents the possibility of late fracture displacement and malunion. Because these distal femur fractures represent physeal injuries, premature physeal closure may occur; an angular deformity was observed in 8% of cases, a leg-length discrepancy was identified in 14% of cases, and 12% of patients ultimately required an additional procedure to address these deformities. Fortunately, as discussed earlier, these “transitional fractures” often occur later in adolescence when the physis is starting to close, so many patients do not develop a clinically significant angular deformity or leg-length discrepancy. This is in contradistinction to Salter-Harris type II fractures of the distal femur, which tend to occur in younger patients, with as many as 40% requiring additional treatment for their premature physeal closure.2,6,7 For patients with open growth plates, we recommend routine clinical and radiographic follow-up for a minimum of 12 months or until both the distal femoral physes have symmetrically closed.
In our study, although limited by small numbers, lateral femoral condyle fractures appeared to be at a greater risk for complications compared with medial femoral condyle fractures (50% vs 13%; P < .03). Premature physeal closures associated with the lateral-sided fractures were also more likely to require a subsequent surgery (50% vs 7%). The reason for the poorer prognosis with the lateral femoral condyle fractures is unclear but possibly represents a higher energy mechanism of injury. Regardless, patients and their families need to be counseled and monitored accordingly.
Arthrofibrosis following significant knee trauma and surgery is not uncommon. In the current series, 20% of patients were noted to have mild loss of motion in their knee, particularly flexion. One patient developed significant arthrofibrosis requiring surgical lysis of adhesions and manipulation under anesthesia. Another observation of the current study was that the braced patients had lower rates of complication than the casted patients. Given these findings, we recommend early mobilization whenever possible assuming sufficient fixation has been achieved intraoperatively. Eid and Hafez7 also found a high rate of stiffness in their cohort of distal femur physeal fractures treated with a cast, with nearly 30% of patients losing 10° to 40° of flexion or 5° to 20° of extension.
The current study has several limitations that primarily relate to its retrospective design. Additionally, we focused our analysis on radiographic and surgeon-reported outcomes as opposed to patient-reported outcomes. Although a future prospective study with patient-derived outcomes would be beneficial, given the relative rarity of this injury pattern, it would take a multicenter group years to accumulate a large series of patients, making this study prohibitive and unlikely. Another limitation is that our relatively short-term follow-up limited our ability to make conclusions about the risk of future posttraumatic arthritis of these intra-articular fractures. Finally, our study had no nonoperative comparison group, limiting our ability to determine which fractures may have had acceptable outcomes without surgical intervention.
In conclusion, intra-articular physeal fractures (Salter-Harris type III and IV) of the distal femur represent a “transitional fracture” most commonly observed during adolescence when the physis is beginning to close. These injuries will frequently occur in football players as a result of a valgus force being applied to the lateral aspect of the knee. These injuries are often initially missed on radiographs (upward of 40%); when treating athletes in this age group who present with a large knee effusion, clinicians must keep a high index of suspicion and must have a low threshold for obtaining MRI or CT imaging. Surgical fixation results in reliable fracture healing with high rates of return to sport, but premature physeal closure may occur in approximately 10% of fractures involving the medial femoral condyle and potentially as high as 50% of fractures involving the lateral femoral condyle. Patients (especially patients with substantial growth remaining) should be observed for a minimum of 12 months or until both growth plates have symmetrically closed.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: H.B.E. is a paid consultant for Smith & Nephew and receives funding for the ROCK (Research in Osteochondritis of the Knee) Study Group.
Ethical approval for this study was obtained from the University of California, San Diego, Human Research Protections Program (project No. 151449X).
References
- 1. Abbasi D, May MM, Wall EJ, Chan G, Parikh SN. MRI findings in adolescent patients with acute traumatic knee hemarthrosis. J Pediatr Orthop. 2012;32(8):760–764. [DOI] [PubMed] [Google Scholar]
- 2. Arkader A, Warner WC, Jr, Horn BD, et al. Predicting the outcome of physeal fractures of the distal femur. J Pediatr Orthop. 2007;27:703–708. [DOI] [PubMed] [Google Scholar]
- 3. Bassett FH III, Goldner JL. Fractures involving the distal femoral epiphyseal growth line. South Med J. 1962;55:545–557. [DOI] [PubMed] [Google Scholar]
- 4. Bertin KC, Goble EM. Ligament injuries associated with physeal fractures about the knee. Clin Orthop Relat Res. 1983;177:188–195. [PubMed] [Google Scholar]
- 5. Czitrom AA, Salter RB, Willis RB. Fractures involving the distal epiphyseal plate of the femur. Int Orthop. 1981;4:269–277. [DOI] [PubMed] [Google Scholar]
- 6. Edmunds I, Nade S. Injuries of the distal femoral growth plate and epiphysis: should open reduction be performed? Aust N Z J Surg. 1993;63:195–199. [DOI] [PubMed] [Google Scholar]
- 7. Eid AM, Hafez MA. Traumatic injuries of the distal femoral physis: retrospective study on 151 cases. Injury. 2002;33:251–255. [DOI] [PubMed] [Google Scholar]
- 8. Lippert WC, Owens RF, Wall EJ. Salter-Harris type III fractures of the distal femur: plain radiographs can be deceptive. J Pediatr Orthop. 2010;30(6):598–605. [DOI] [PubMed] [Google Scholar]
- 9. Liu RW, Armstrong DG, Levine AD, Gilmore A, Thompson GH, Cooperman DR. An anatomic study of the distal femoral epiphysis. J Pediatr Orthop. 2013;33(7):743–749. [DOI] [PubMed] [Google Scholar]
- 10. Lombardo SJ, Harvey JP., Jr Fractures of the distal femoral epiphyses: factors influencing prognosis: a review of thirty-four cases. J Bone Joint Surg Am. 1977;59:742–751. [PubMed] [Google Scholar]
- 11. McKissick RC, Gilley JS, DeLee JC. Salter-Harris type III fractures of the medial distal femoral physis—a fracture pattern related to the closure of the growth plate: report of 3 cases and discussion of pathogenesis. Am J Sports Med. 2008;36(3):572–576. [DOI] [PubMed] [Google Scholar]
- 12. Peterson HA, Madhok R, Benson JT, Ilstrup DM, Melton LJ., 3rd Physeal fractures, part 1: epidemiology in Olmsted County, Minnesota, 1979-1988. J Pediatr Orthop. 1994;14(4):423–430. [DOI] [PubMed] [Google Scholar]
- 13. Pritchett JW. Longitudinal growth and growth-plate activity in the lower extremity. Clin Orthop Relat Res. 1992;275:274–279. [PubMed] [Google Scholar]
- 14. Riseborough EJ, Barrett IR, Shapiro F. Growth disturbances following distal femoral physeal fracture-separations. J Bone Joint Surg Am. 1983;65:885–893. [PubMed] [Google Scholar]
- 15. Rogers LF, Jones S, Davis AR, Dietz G. “Clipping injury” fracture of the epiphysis in the adolescent football player: an occult lesion of the knee. Am J Roentgenol Radium Ther Nucl Med. 1974;121(1):69–78. [DOI] [PubMed] [Google Scholar]
- 16. Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Joint Surg. 1963;45A:587–622. [Google Scholar]
- 17. Sasaki T, Ishibashi Y, Okamura Y, Toh S, Sasaki T. MRI evaluation of growth plate closure rate and pattern in the normal knee joint. J Knee Surg. 2002;15(2):72–76. [PubMed] [Google Scholar]
- 18. Thomson JD, Stricker SJ, Williams MM. Fractures of the distal femoral epiphyseal plate. J Pediatr Orthop. 1995;15:474–478. [DOI] [PubMed] [Google Scholar]
- 19. Torg JS, Pavlov H, Morris VB. Salter-Harris type-III fracture of the medial femoral condyle occurring in the adolescent athlete. J Bone Joint Surg Am. 1981;63:586–591. [PubMed] [Google Scholar]



