Abstract
Background:
Medicare insures the largest population of patients at risk for rotator cuff tears in the United States.
Purpose:
To evaluate the trends in incidence, concomitant procedures, and complications with open and arthroscopic rotator cuff repairs in Medicare patients.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
All Medicare patients who had undergone open or arthroscopic rotator cuff repair from 2005 through 2011 were identified with a claims database. Annual incidence, concomitant procedures, and postoperative complications were compared between these 2 groups.
Results:
In total, 372,109 rotator cuff repairs were analyzed. The incidence of open repairs decreased (from 6.0 to 4.3 per 10,000 patients, P < .001) while the incidence of arthroscopic repairs increased (from 4.5 to 7.8 per 10,000 patients, P < .001) during the study period. Patients in the arthroscopic group were more likely to have undergone concomitant subacromial decompression than those in the open group (87% vs 35%, P < .001), and the annual incidence of concomitant biceps tenodesis increased for both groups (from 3.8% to 11% for open and 2.2% to 16% for arthroscopic, P < .001). While postoperative complications were infrequent, patients in the open group were more likely to be diagnosed with infection within 6 months (0.86% vs 0.37%, P < .001) but no more likely to undergo operative debridement (0.43% vs 0.26%, P = .08). Additionally, patients in the open group were more likely to undergo intervention for shoulder stiffness within 1 year (1.4% vs 1.1%, P = .01).
Conclusion:
In the Medicare population, arthroscopic rotator cuff repairs have increased in incidence and now represent the majority of rotator cuff repair surgery. Among concomitant procedures, subacromial decompression was most commonly performed despite evidence suggesting a lack of efficacy. Infections and stiffness were rare complications that were slightly but significantly more frequent in open rotator cuff repairs.
Keywords: rotator cuff, arthroscopy, open, Medicare, shoulder
Rotator cuff tears are one of the most commonly encountered musculoskeletal pathologies for older patients, with an estimated 10% of patients >60 years old affected.25 While the majority of rotator cuff tears are treated nonoperatively,13 rotator cuff repair surgery is nonetheless one of the most commonly performed surgeries in orthopaedics.8 Rotator cuff repairs were historically performed via an open approach, but in recent times the arthroscopic approach has become increasingly common and widely accepted.7,10,24
Many studies compared the benefits of arthroscopic rotator cuff repairs with open and mini-open rotator cuff repairs.26,27,30,34 Although each surgical approach possesses specific advantages and disadvantages,7 they have thus far been shown to have comparable clinical outcomes and complication rates.12,15,28 Some studies found higher costs associated with arthroscopic rotator cuff repairs,2,6 whereas others found no cost difference between them.16
Known complications following rotator cuff repair surgery include postoperative infections, shoulder stiffness, and tendon reruptures.21 The reported rates of these complications vary by source. Although 1 study of Veterans Affairs (VA) patients demonstrated higher rates of some complications in its open rotator cuff repair group, including wound infections within the first 30 postoperative days, it is unknown if this difference is true for a nationally representative cohort.19,21,27
Medicare provides health insurance in the United States to >45 million patients, the majority of whom are >65 years old.23 With the average age of patients undergoing rotator cuff repair being 63 years old,11 it would be logical that the Medicare population would be an appropriate and nationally representative patient population to evaluate with regard to rotator cuff repair outcomes.
The purpose of this study was to assess trends in the surgical management of rotator cuff tears in the Medicare population. Specifically, we evaluated the change in incidence of open and arthroscopic rotator cuff repairs and the incidence of postoperative complications in this population. We also assessed trends in concomitant procedures associated with rotator cuff repair surgery in Medicare patients, as 1 study suggested that the rates of these procedures have been increasing31 despite there currently being a lack of evidence supporting their use.1,17,22,29,33
On the basis of previous studies, we hypothesized that the incidence of arthroscopic but not open rotator cuff repairs had increased, that concomitant procedure incidence had increased in both surgical groups, and that the incidence of postoperative shoulder infection and stiffness was higher in the open group than the arthroscopic group.
Methods
Data Query and Analysis
The PearlDiver patient record database (PearlDiver Inc; www.pearldiverinc.com) is a publically available database of >4 billion insurance billing records. It contains the records of patients who have had an orthopaedic code—International Classification of Diseases, Ninth Revision (ICD-9) or Current Procedural Terminology (CPT)—assigned to their billing record from private insurance and Medicare. The PearlDiver database was chosen because it contained the records of all Medicare patients with an orthopaedic ICD-9 or CPT code from 2005 through 2011.
This database was queried for Medicare patients who had undergone any open rotator cuff repair (CPT 23410, 23412, or 23420) and for those who had undergone arthroscopic rotator cuff repair (CPT 29827) from 2005 through 2011. We did include CPT 23420, which can be used for either an open repair or a reconstruction of a large rotator cuff tear, in the open rotator cuff repair group. Despite the fact that this code does include open reconstructions, we used it to be inclusive of all Medicare open rotator cuff repairs and because the only CPT code for arthroscopic rotator cuff repairs, 29827, also includes arthroscopic rotator cuff reconstructions. CPT 23420 accounted for 28.6% of all open rotator cuff repairs, indicating that it was not solely used for the relatively rare open rotator cuff reconstruction procedure. The database does not differentiate between open and mini-open rotator cuff repairs. Demographic data and the annual incidence of open and arthroscopic rotator cuff repairs per 10,000 patient-years and per 100 rotator cuff tear diagnoses were determined.
These 2 patient populations, the open group and the arthroscopic group, were subsequently queried to evaluate the rates of concomitant procedures and postoperative complications, including infections and shoulder stiffness, within each group. We did not evaluate revision surgery because operative laterality is not defined within CPT coding data.
To evaluate the incidence of concomitant procedures, the open and arthroscopic rotator cuff repair populations were each queried for subacromial decompression (CPT 23130 or 29826), distal clavicle resection (CPT 23120 or 29824), and biceps tenodesis (CPT 23430 or 29828) performed on the same day as the rotator cuff repair. We were unable to evaluate the incidence of concomitant biceps tenotomies because no specific CPT code exists for this procedure. The percentage of rotator cuff repairs in each group with these concomitant procedures was then calculated and compared. Additionally, the change in incidence of these concomitant procedures over time was evaluated as well as the percentage of open and arthroscopic concomitant procedures for each surgical group.
To evaluate postoperative shoulder infections, the open and arthroscopic rotator cuff repair populations were each queried for postoperative infection diagnoses (ICD-9-D-998.5, 998.51, or 998.59) entered within 6 months following the index rotator cuff repair. Each of these postoperative infection populations was then further queried for surgical debridement interventions (CPT 10060, 10061, 10140, 10180, 11040, 11041, 11042, 11043, 11044, 20000, 20005, 23030, 23031, or 23035) within 6 months following the index procedure. The mean percentage of patients with a diagnosis of postoperative shoulder infection and the mean percentage of patients who subsequently underwent surgical management of their postoperative infection were then compared between the open and arthroscopic groups.
Last, to evaluate postoperative shoulder stiffness, the 2 groups were each queried for shoulder manipulation under anesthesia without subsequent surgical intervention (CPT 23700, excluding CPT 29825 and 23020), arthroscopic lysis of adhesions (CPT 29825), and open capsular contracture release (CPT 23020) within 1 year following the index procedure. The mean number of manipulations under anesthesia, arthroscopic lysis of adhesions, open capsular contracture releases, and any intervention were then calculated and compared between the open and arthroscopic groups.
Statistical Analysis
A 2-tailed Student t test was used to determine the statistical significance of differences between mean values in the open and arthroscopic rotator cuff repair groups, with equality of variance determined via the F test. The χ2 test was used to evaluate the significance of differences in open and arthroscopic concomitant procedure percentages, and the χ2 test for trend was used to evaluate significance of trends in rotator cuff repairs and concomitant procedures. Statistical significance for all analyses was set at P <.05.
Results
Trends in Rotator Cuff Repairs
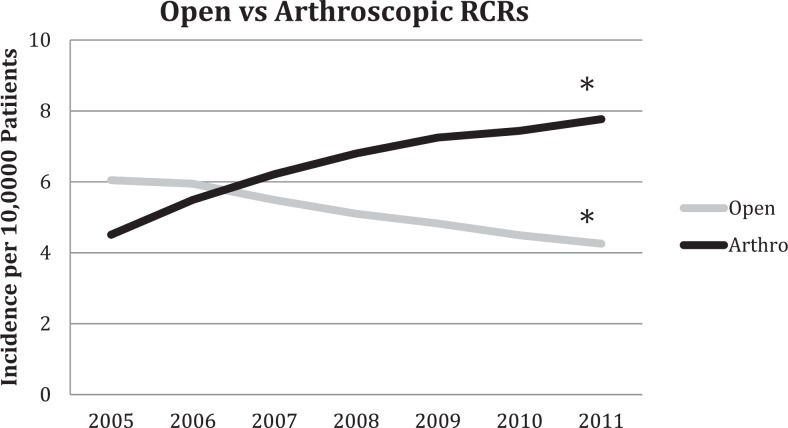
There were 372,109 rotator cuff repair surgical procedures (157,135 open and 199,823 arthroscopic) performed on Medicare patients between 2005 and 2011 (Table 1). On average, there were 45.5 million Medicare enrollees, 189,244 rotator cuff tear diagnoses, and 53,158 rotator cuff repairs performed each year. The overall incidence of rotator cuff repair during this time was 9.63 per 10,000 patients per year (4.24 open vs 5.39 arthroscopic repairs; P = .02). The incidence of open rotator cuff repairs decreased (from 6.04 to 4.25 per 10,000; P < .001) while the incidence of arthroscopic rotator cuff repairs increased (from 4.51 to 7.77 per 10,000; P < .001) during the study period (Figure 1).
TABLE 1.
Rotator Cuff Tears and Repairs in the Medicare Population, 2005-2011a
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | |
|---|---|---|---|---|---|---|---|
| Patientsb | 42,499,593 | 43,338,571 | 44,263,111 | 45,411,883 | 46,520,716 | 47,664,048 | 48,849,404 |
| RCTsb | 169,828 | 179,079 | 183,753 | 188,120 | 193,037 | 198,382 | 212,510 |
| RCRsc | 44,864 (26.4) | 49,575 (27.7) | 51,802 (28.2) | 54,063 (28.7) | 56,181 (29.1) | 56,889 (28.7) | 58,735 (27.6) |
| Male, %d | |||||||
| RCT | 44.1 | 44.3 | 44.7 | 41.1 | 45.3 | 45.3 | 45.4 |
| RCR | 49.0 | 49.0 | 49.5 | 44.0 | 49.7 | 50.0 | 49.6 |
aRCRs, rotator cuff repairs; RCTs, rotator cuff tears.
bValues represent the total number of patients.
cValues represent the number (percentages) of patients diagnosed with an RCT who underwent an RCR.
dValues represent the percentages of patients in the RCT and RCR groups who were male.
Figure 1.
Annual incidence of open and arthroscopic rotator cuff repairs (RCRs) per 10,000 Medicare patients. *Statistically significant trend, P < .001.
Concomitant Procedures
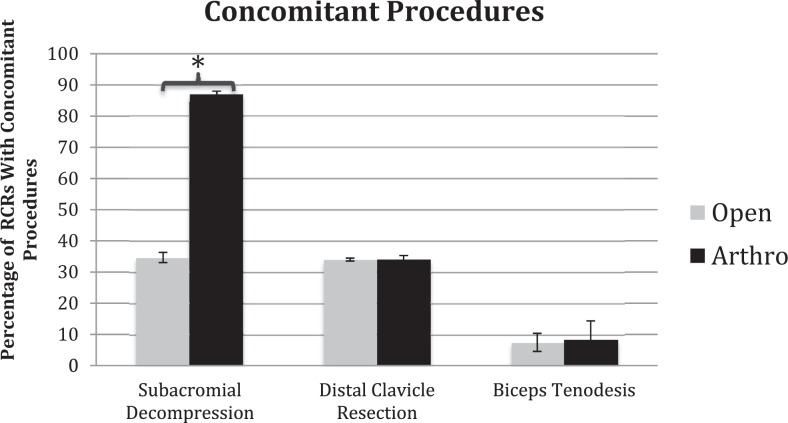
Patients who had undergone arthroscopic rotator cuff repair were 2.49 times more likely to additionally undergo subacromial decompression than those who had undergone open rotator cuff repair (Figure 2). There was no difference, however, in rates of distal clavicle resection and biceps tenodesis between the open and arthroscopic groups. Patients in the arthroscopic group were more likely than patients in the open group to undergo arthroscopic, as opposed to open, subacromial decompressions, distal clavicle resections, and biceps tenodeses (Table 2).
Figure 2.
Incidence of concomitant procedures per index rotator cuff repair (RCR), open vs arthroscopic, in Medicare patients from 2005 to 2011. *P < .001. Error bars indicate ±1 SD.
TABLE 2.
Open and Arthroscopic Concomitant Proceduresa
| RCRb: Concomitant Procedure | Percentage | P Value |
|---|---|---|
| Open | <.001 | |
| Open SAD | 17.3 | |
| Arthroscopic SAD | 82.7 | |
| Arthroscopic | ||
| Open SAD | 0.3 | |
| Arthroscopic SAD | 99.7 | |
| Open | <.001 | |
| Open DCR | 64.0 | |
| Arthroscopic DCR | 36.0 | |
| Arthroscopic | ||
| Open DCR | 4.1 | |
| Arthroscopic DCR | 95.9 | |
| Open | <.001 | |
| Open BT | 85.6 | |
| Arthroscopic BT | 14.4 | |
| Arthroscopic | ||
| Open BT | 20.0 | |
| Arthroscopic BT | 80.0 |
aValues represent the percentage of patients in each surgical group, having undergone a given concomitant procedure, who underwent an open or arthroscopic concomitant procedure. BT, biceps tenodesis; DCR, distal clavicle resection; RCR, rotator cuff repair; SAD, subacromial decompression.
bPrimary procedure.
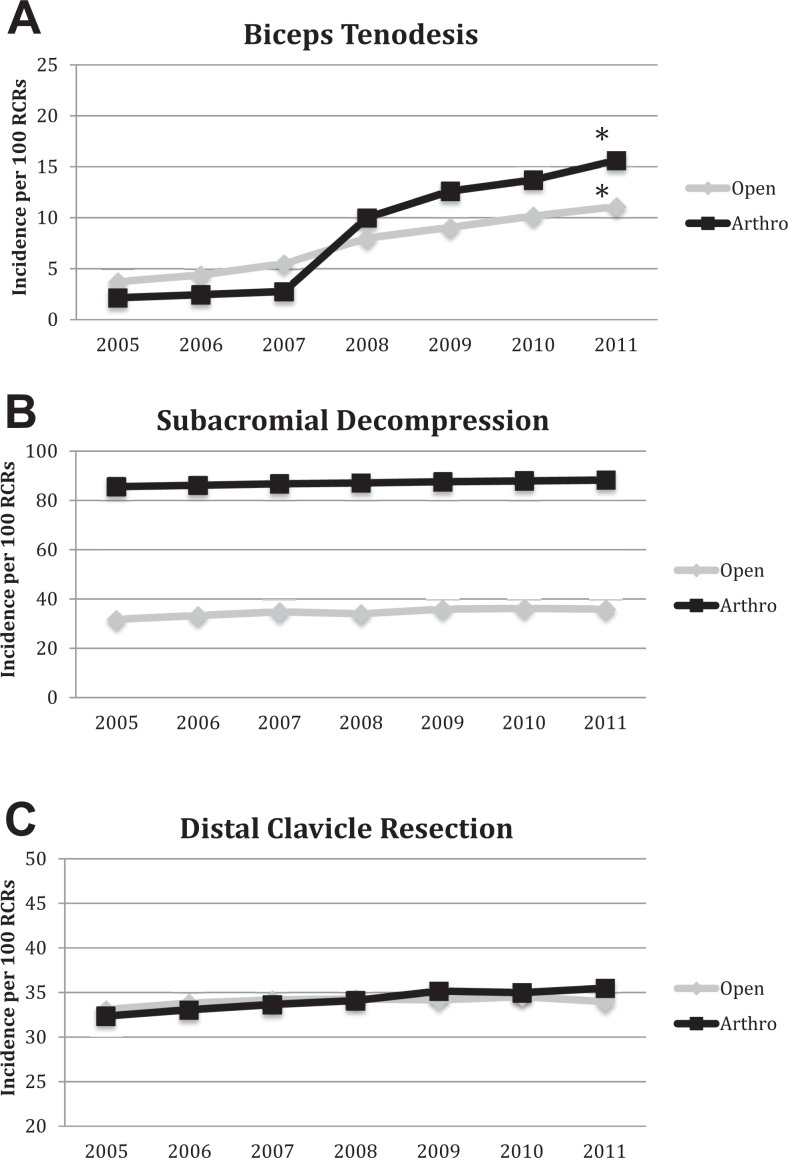
The annual rate of concomitant biceps tenodesis increased significantly from 2005 through 2011 in the open and arthroscopic groups (Figure 3A). The annual rate of concomitant subacromial decompression (Figure 3B) and distal clavicle resection (Figure 3C), however, did not change significantly in either the open or the arthroscopic group.
Figure 3.
The annual incidence of concomitant (A) biceps tenodeses, (B) subacromial decompressions, and (C) distal clavicle resections per 100 rotator cuff repairs (RCRs) in the open and arthroscopic RCR groups. *Statistically significant change in incidence over time, P < .001.
Postoperative Complications
Patients in the open rotator cuff repair group were 2.32 times more likely than patients in the arthroscopic group to be diagnosed with a postoperative shoulder infection within 6 months of their rotator cuff repair. There was, however, no statistically significant difference in the percentage of patients who subsequently required surgical debridement for their postoperative infection between the 2 groups (Table 3).
TABLE 3.
Postoperative Complications
| Complication | Opena | Arthroscopica | P Value |
|---|---|---|---|
| Infection diagnosis | 0.86 | 0.37 | <.001 |
| Surgical debridement | 0.43 | 0.26 | .08 |
| Manipulation under anesthesia | 1.1 | 0.68 | <.001 |
| Arthroscopic lysis of adhesions | 0.27 | 0.42 | .02 |
| Any stiffness intervention | 1.4 | 1.1 | .01 |
aValues expressed are the incidence of postoperative complications per 100 rotator cuff repairs.
More patients in the open group than in the arthroscopic group required an intervention for postoperative shoulder stiffness within 1 year of rotator cuff repair. Patients in the open rotator cuff repair group were more likely to undergo shoulder manipulation under anesthesia than patients in the arthroscopic group, while those in the arthroscopic rotator cuff repair group were more likely to undergo arthroscopic lysis of adhesions (Table 3). Few patients from either group underwent open treatment for postoperative stiffness (0.02% in the open group, 0.00% in the arthroscopic group; P = .15).
Discussion
Our study evaluated rotator cuff repair surgery in the Medicare population because it represents the largest cohort of patients with rotator cuff tears in the United States. Accordingly, this study evaluated the largest number of rotator cuff repair surgeries to date. We hypothesized that the incidence of arthroscopic, but not open, rotator cuff repairs had increased, that the rates of concomitant procedures had increased in both surgical groups, and that the incidence of postoperative complications was higher in the open group than the arthroscopic group based on results from previous studies.
Our study found that the incidence of arthroscopic rotator cuff repairs has indeed increased while the incidence of open rotator cuff repairs has decreased. These findings confirm previous studies of other patient cohorts that also reported this paradigm shift from predominantly open to predominantly arthroscopic rotator cuff repairs.7,19,35 This shift has occurred despite a lack of evidence supporting one procedure over another.12,18,28 This cultural shift may be due to young surgeons’ preferences and familiarity with arthroscopic procedures, patients’ preferences for minimally invasive procedures, or even industry marketing forces.
Interestingly, when Medicare patients are compared with other patient populations, this transition from predominantly open to predominantly arthroscopic rotator cuff repairs occurred later than in the private health insurance population but earlier than in the VA population.19,35 The first year in which >50% of rotator cuff repairs were performed arthroscopically was in 2007 for the Medicare patient population, compared with 2005 for a private insurance group,35 while this threshold had not yet been met as of 2009 in the VA patient population.19 This difference in arthroscopic rotator cuff repair adoption rate in the Medicare population versus other patient populations may indicate that younger patients with private insurance have sought out newer technology earlier than Medicare and VA patients. Alternatively, the adoption rates may reflect differences in resource utilization among the patient populations, given the possible higher costs associated with the arthroscopic approach2,6; for example, it was demonstrated that patients with private health insurance are twice as likely as Medicare patients to undergo physical therapy after rotator cuff repair surgery.3
While concomitant procedures currently have an unclear effect on the outcome of rotator cuff repairs,1,5,17,22,29,33 these procedures are often performed with rotator cuff repairs to address additional aspects of shoulder pathology. We found that the incidence of subacromial decompression was high for both groups but greater in the arthroscopic rotator cuff repair group than in the open group (see Figure 2). This is despite evidence from studies suggesting that acromioplasty provides no benefit to the outcome of rotator cuff repair.1,5 Interestingly, countries such as Finland have experienced a decrease in the incidence of acromioplasties since 2007,20 while this has not been the case for Medicare patients. This difference may reflect a continued belief in the effectiveness of subacromial decompression or differences in training, or it may be related to reimbursement influences.
Additionally, we found that the incidence of concomitant biceps tenodesis increased significantly for open and arthroscopic repairs over time (see Figure 3). Biceps tenodesis has become an increasingly common procedure in recent years, and the increase in concomitant biceps tenodesis with rotator cuff repair in our study period may reflect the overall popularization of this procedure. Many studies have demonstrated good surgical outcomes following biceps tenotomy or tenodesis, likely influencing this increasing incidence.10,14,33 A database review of private health insurance and Medicare patients demonstrated that the annual number of open biceps tenodeses increased by 57.3% from 2008 to 2011, while the annual number of arthroscopic biceps tenodeses increased by 83.4% from 2008 to 2011.31 This overall increase in biceps tenodeses likely explains the similar increase in concomitant biceps tenodeses with rotator cuff repairs and may reflect an increased awareness of biceps tendon pathology as a potential cause of shoulder pathology.10,14,33
The difference in concomitant subacromial decompression rates is interesting because of the current lack of evidence supporting the use of concomitant procedures in conjunction with rotator cuff repairs.1,5,29 The greater incidence of subacromial decompression in the arthroscopic group may be due to the facility in which it is performed during the arthroscopic approach. Alternatively, it may partially be due to a difference in subacromial decompression billing code utilization between the arthroscopic and open groups, as CPT 23420 can signify an open rotator cuff repair performed with or without acromioplasty. On average, CPT 23420 accounted for 28.6% of the annual open rotator cuff repairs. If one were to assume that all of these codes represented open rotator cuff repairs with subacromial decompressions, this estimate would increase the mean number of concomitant subacromial decompressions from 0.35 to 0.63 per index procedure for the open group. This adjusted incidence, however, remains significantly lower than the 0.87 subacromial decompressions per index procedure in the arthroscopic group (P < .001), indicating that the difference in concomitant subacromial decompression rate is not solely due to coding differences between the open and arthroscopic groups.
Unsurprisingly, patients who had had arthroscopic rotator cuff repair were relatively more likely to undergo arthroscopic concomitant procedures as compared with patients in the open rotator cuff repair group (Table 2). The percentage of patients in the open group who underwent arthroscopic subacromial decompression may indicate the percentage of patients in the open group who underwent mini-open, instead of traditional open, rotator cuff repair, as this procedure would be performed only for the former.
Complications following rotator cuff repair surgery, regardless of surgical approach, include superficial and deep infection, shoulder stiffness, and tendon retear.21 We found that the incidences of postoperative infection diagnosis and surgical debridement were generally low for both groups (Table 3) but that the incidence of postoperative infection diagnosis in the open group was 2.32 times greater than in the arthroscopic group. The increased diagnoses, but not debridement procedures, likely represent an increased incidence of superficial, but not deep, infections in the open rotator cuff repair group. This difference, while statistically significant, may not be clinically relevant. Although the VA patient population has unique characteristics that limits its external validity (eg, >80% rate of diabetes), a retrospective review of nearly 10,000 VA patients also revealed higher rates of postoperative superficial, but not deep, infections in the open group versus the arthroscopic rotator cuff repair group.19
Compared with other studies of patients undergoing shoulder arthroscopy, our 2 patient populations had similar rates of postoperative infection debridement procedures. A retrospective review of a private health insurance database from 2004 through 2009 demonstrated that only 0.27% of arthroscopic shoulder procedures required surgical management of a postoperative infection within 30 days.32 Specific risk factors included age >50 years and rotator cuff repair,32 both of which are applicable to our cohort. In contrast to authors of earlier studies, we captured infection data for up to 6 months after surgery to include indolent infections such as Propionibacterium acnes, which account for 51% to 86% of postoperative infections following shoulder arthroscopy.21
Previously published rates of postoperative shoulder stiffness following open and arthroscopic rotator cuff repairs ranged between 0.5% and 4.8% and between 2.6% and 8.7%, respectively.21,24 These large ranges reflect the fact that postoperative shoulder stiffness lacks specific diagnostic criteria. Because of this lack of specific diagnostic criteria, we chose instead to evaluate the rates of intervention for shoulder stiffness (manipulation under anesthesia or surgery) as a more specific and reliable marker for this complication. We found that both surgical groups had low rates of postoperative shoulder stiffness severe enough to necessitate an intervention but that a greater percentage of patients in the open group than in the arthroscopic group required an intervention.
Other studies found no significant difference in the rates of postoperative shoulder stiffness between open and arthroscopic rotator cuff repairs,27,28 but these studies analyzed far fewer patients and were assessing stiffness diagnoses, not interventions. We believe that these 2 factors resulted in our study’s demonstrating a distinction in shoulder stiffness rates between the 2 surgical groups. Of patients who did require intervention for postoperative stiffness, patients in the open repair group were more likely to undergo manipulation under anesthesia than those in the arthroscopic group, while those in the arthroscopic group were more likely to undergo arthroscopic lysis of adhesions than those in the open group (see Table 3). This difference in treatment choice likely reflects providers’ relative comfort with shoulder arthroscopy and the patients’ comorbidities that influenced the initial choice of open versus arthroscopic surgery.
Limitations
Limitations of this study include its retrospective nature and its reliance on billing data, which lack ideal granularity.23 Since the study was retrospective, we were unable to adjust for differences in comorbidity rates between the 2 groups or rotator cuff tear complexity factors, such as tear size and Goutallier grade, which may account for some of the differences in postoperative complications or may have influenced the surgeons’ choice of open over arthroscopic approach. The inclusion of CPT 23420 in the open group, while necessary to include all open rotator cuff repairs in the analysis, may have biased the open group to more difficult massive repairs and reconstructions. Certain complications, such as tendon retears, deep vein thrombosis, and anesthetic complications, were unable to be assessed from the data set, as were cost and patient outcomes. Tendon retear rates in particular would have been a valuable comparison given that retears are often the most clinically significant complications. There is some evidence to suggest that arthroscopic rotator cuff repairs have a higher incidence of retears following repair of tears >3 cm,4 which may influence surgeons to choose the open approach for larger and more complicated tears. We were unable to assess the rates of revision operations because laterality is not included in CPT codes, which makes revision surgery and contralateral primary surgery indistinguishable in this data set. Last, we were unable to specifically evaluate mini-open rotator cuff repairs owing to the lack of a CPT code for this procedure. The rate of arthroscopic concomitant subacromial decompression in the open rotator cuff repair group may indicate the incidence of mini-open rotator cuff repairs (see Table 2), as this concomitant procedure would be performed arthroscopically in only a mini-open approach, but we cannot confirm this hypothesis.
Conclusion
This study demonstrates that the overall incidence of rotator cuff tears and the percentage undergoing surgery did not change in the Medicare population from 2005 to 2011. The incidence of arthroscopic rotator cuff repairs during this time increased, while that of open rotator cuff repairs decreased, despite a lack of clear evidence showing improved outcomes with arthroscopic surgery in the literature. Subacromial decompression remained the most common concomitant procedure despite studies demonstrating no benefit.1,5,9 The incidence of concomitant biceps tenodesis has increased significantly in open and arthroscopic rotator cuff repairs. While infections were rare following rotator cuff repairs, there was an increased incidence of superficial, but not deep, infections in open repairs. These findings from a large and nationally representative patient cohort contribute to the body of literature identifying the differences between open and arthroscopic rotator cuff repair. Given these findings and other contributing factors, such as retear rates, cost-effectiveness, and patient outcomes, future prospective studies are required to fully elucidate the benefits of the 2 approaches.
Acknowledgment
The authors thank Dr Brett Owens for kindly providing supplementary data from his manuscript.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This research project was supported in part by the H&H Lee Surgical Scholars Research Program.
Ethical approval was not sought for this study.
References
- 1. Abrams GD, Gupta AK, Hussey KE, et al. Arthroscopic repair of full-thickness rotator cuff tears with and without acromioplasty: randomized prospective trial with 2-year follow-up. Am J Sports Med. 2014;42(6):1296–1303. [DOI] [PubMed] [Google Scholar]
- 2. Adla DN, Rowsell M, Pandey R. Cost-effectiveness of open versus arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2010;19(2):258–261. [DOI] [PubMed] [Google Scholar]
- 3. Arshi A, Kabir N, Cohen JR, et al. Utilization and costs of postoperative physical therapy after rotator cuff repair: a comparison of privately insured and Medicare patients [published online July 29, 2015]. Arthroscopy. doi:10.1016/j.arthro.2015.06.018. [DOI] [PubMed] [Google Scholar]
- 4. Bishop J, Klepps S, Lo IK, Bird J, Gladstone JN, Flatow EL. Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Shoulder Elbow Surg. 2006;15(3):290–299. [DOI] [PubMed] [Google Scholar]
- 5. Chahal J, Mall N, MacDonald PB, et al. The role of subacromial decompression in patients undergoing arthroscopic repair of full-thickness tears of the rotator cuff: a systematic review and meta-analysis. Arthroscopy. 2012;28(5):720–727. [DOI] [PubMed] [Google Scholar]
- 6. Churchill RS, Ghorai JK. Total cost and operating room time comparison of rotator cuff repair techniques at low, intermediate, and high volume centers: mini-open versus all-arthroscopic. J Shoulder Elbow Surg. 2010;19(5):716–721. [DOI] [PubMed] [Google Scholar]
- 7. Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL. National trends in rotator cuff repair. J Bone Joint Surg. 2012;94(3):227–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eljabu W, Klinger HM, von Knoch M. The natural history of rotator cuff tears: a systematic review. Arch Orthop Trauma Surg. 2015;135(8):1055–1061. [DOI] [PubMed] [Google Scholar]
- 9. Frank JM, Chahal J, Frank RM, Cole BJ, Verma NN, Romeo AA. The role of acromioplasty for rotator cuff problems. Orthop Clin North Am. 2014;45(2):219–224. [DOI] [PubMed] [Google Scholar]
- 10. Gombera MM, Kahlenberg CA, Nair R, Saltzman MD, Terry MA. All-arthroscopic suprapectoral versus open subpectoral tenodesis of the long head of the biceps brachii. Am J Sports Med. 2015;43(5):1077–1083. [DOI] [PubMed] [Google Scholar]
- 11. Henry P, Wasserstein D, Park S, et al. Arthroscopic repair for chronic massive rotator cuff tears: a systematic review [published online September 10, 2015]. Arthroscopy. doi:10.1016/j.arthro.2015.06.038. [DOI] [PubMed] [Google Scholar]
- 12. Ji X, Bi C, Wang F, Wang Q. Arthroscopic versus mini-open rotator cuff repair: an up-to-date meta-analysis of randomized controlled trials. Arthroscopy. 2015;31(1):118–124. [DOI] [PubMed] [Google Scholar]
- 13. Kuhn JE. Nonoperative treatment of rotator cuff tears. Am J Orthop. 2016;45(2):66–67. [PubMed] [Google Scholar]
- 14. Meeks BD, Meeks NM, Froehle AW, Wareing E, Bonner KF. Patient satisfaction after biceps tenotomy. Orthop J Sports Med. 2017;5(5):23259 6711770773-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Morse K, Davis AD, Afra R, Kaye EK, Schepsis A, Voloshin I. Arthroscopic versus mini-open rotator cuff repair: a comprehensive review and meta-analysis. Am J Sports Med. 2008;36(9):1824–1828. [DOI] [PubMed] [Google Scholar]
- 16. Murphy J, Gray A, Cooper C, Cooper D, Ramsay C, Carr A. Costs, quality of life and cost-effectiveness of arthroscopic and open repair for rotator cuff tears: an economic evaluation alongside the UKUFF trial. Bone Joint J. 2016;98B(12):1648–1655. [DOI] [PubMed] [Google Scholar]
- 17. Oh JH, Kim JY, Choi JH, Park S-M. Is arthroscopic distal clavicle resection necessary for patients with radiological acromioclavicular joint arthritis and rotator cuff tears? A prospective randomized comparative study. Am J Sports Med. 2014;42(11):2567–2573. [DOI] [PubMed] [Google Scholar]
- 18. Osti L, Papalia R, Paganelli M, Denaro E, Maffulli N. Arthroscopic vs mini-open rotator cuff repair: a quality of life impairment study. Int Orthop. 2010;34(3):389–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Owens BD, Williams AE, Wolf JM. Risk factors for surgical complications in rotator cuff repair in a veteran population [published online July 8, 2015]. J Shoulder Elbow Surg. doi:10.1016/j.jse.2015.04.020. [DOI] [PubMed] [Google Scholar]
- 20. Paloneva J, Lepola V, Karppinen J, Ylinen J, Äärimaa V, Mattila VM. Declining incidence of acromioplasty in Finland. Acta Orthop. 2015;86(2):220–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Parada SA, Dilisio MF, Kennedy CD. Management of complications after rotator cuff surgery. Curr Rev Musculoskelet Med. 2015;8(1):40–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Park YB, Koh KH, Shon MS, Park YE, Yoo JC. Arthroscopic distal clavicle resection in symptomatic acromioclavicular joint arthritis combined with rotator cuff tear: a prospective randomized trial. Am J Sports Med. 2015;43(4):985–990. [DOI] [PubMed] [Google Scholar]
- 23. Pugely AJ, Martin CT, Harwood J, Ong KL, Bozic KJ, Callaghan JJ. Database and registry research in orthopaedic surgery: part I. Claims-based data. J Bone Joint Surg Am. 2015;97(15):1278–1287. [DOI] [PubMed] [Google Scholar]
- 24. Randelli P, Spennacchio P, Ragone V, Arrigoni P, Casella A, Cabitza P. Complications associated with arthroscopic rotator cuff repair: a literature review. Musculoskelet Surg. 2012;96(1):9–16. [DOI] [PubMed] [Google Scholar]
- 25. Reilly P, Macleod I, Macfarlane R, Windley J, Emery RJH. Dead men and radiologists don’t lie: a review of cadaveric and radiological studies of rotator cuff tear prevalence. Ann R Coll Surg Engl. 2006;88(2):116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sauerbrey AM, Getz CL, Piancastelli M, Iannotti JP, Ramsey ML, Williams GR. Arthroscopic versus mini-open rotator cuff repair: a comparison of clinical outcome. Arthroscopy. 2005;21(12):1415–1420. [DOI] [PubMed] [Google Scholar]
- 27. Severud EL, Ruotolo C, Abbott DD, Nottage WM. All-arthroscopic versus mini-open rotator cuff repair: a long-term retrospective outcome comparison. Arthroscopy. 2003;19(3):234–238. [DOI] [PubMed] [Google Scholar]
- 28. Shan L, Fu D, Chen K, Cai Z, Li G. All-arthroscopic versus mini-open repair of small to large sized rotator cuff tears: a meta-analysis of clinical outcomes. PLoS ONE. 2014;9(4):e94421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Shin S-J, Oh JH, Chung SW, Song MH. The efficacy of acromioplasty in the arthroscopic repair of small- to medium-sized rotator cuff tears without acromial spur: prospective comparative study. Arthroscopy. 2012;28(5):628–635. [DOI] [PubMed] [Google Scholar]
- 30. Verma NN, Dunn W, Adler RS, et al. All-arthroscopic versus mini-open rotator cuff repair: a retrospective review with minimum 2-year follow-up. Arthroscopy. 2006;22(6):587–594. [DOI] [PubMed] [Google Scholar]
- 31. Werner BC, Brockmeier SF, Gwathmey FW. Trends in long head biceps tenodesis. Am J Sports Med. 2015;43(3):570–578. [DOI] [PubMed] [Google Scholar]
- 32. Yeranosian MG, Arshi A, Terrell RD, Wang JC, McAllister DR, Petrigliano FA. Incidence of acute postoperative infections requiring reoperation after arthroscopic shoulder surgery. Am J Sports Med. 2014;42(2):437–441. [DOI] [PubMed] [Google Scholar]
- 33. Yi Y, Lee J-M, Kwon SH, Kim J-W. Arthroscopic proximal versus open subpectoral biceps tenodesis with arthroscopic repair of small- or medium-sized rotator cuff tears [published online June 4, 2015]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3641-5. [DOI] [PubMed] [Google Scholar]
- 34. Youm T, Murray DH, Kubiak EN, Rokito AS, Zuckerman JD. Arthroscopic versus mini-open rotator cuff repair: a comparison of clinical outcomes and patient satisfaction. J Shoulder Elbow Surg. 2005;14(5):455–459. [DOI] [PubMed] [Google Scholar]
- 35. Zhang AL, Montgomery SR, Ngo SS, Hame SL, Wang JC, Gamradt SC. Analysis of rotator cuff repair trends in a large private insurance population. Arthroscopy. 2013;29(4):623–629. [DOI] [PubMed] [Google Scholar]