Abstract
Objectives
To provide a detailed and current characterisation of funding of a representative sample clinical trials. We also aimed to develop guidance for standardised reporting of funding information.
Methods
We addressed the extent to which clinical trials published in 2015 in any of the 119 Core Clinical Journals included a statement on the funding source (eg, whether a not-for-profit organisation was supported by a private-for-profit organisation), type of funding, amount and role of funder. We used a stepwise approach to develop a guidance and an instrument for standardised reporting of funding information.
Results
Of 200 trials, 178 (89%) included a funding statement, of which 171 (96%) reported being funded. Funding statements in the 171 funded trials indicated the source in 100%, amount in 1% and roles of funders in 50%. The most frequent sources were governmental (58%) and private-for-profit (40%). Of 54 funding statements in which the source was a not-for-profit organisation, we found evidence of undisclosed support of those from private-for-profit organisation(s) in 26 (48%). The most frequently reported roles of funders in the 171 funded trials related to study design (42%) and data analysis, interpretation or management (41%). Of 139 randomised controlled trials (RCTs) addressing pharmacological or surgical interventions, 29 (21%) reported information on the supplier of the medication or device. The proposed guidance addresses both the funding information that RCTs should report and the reporting process. Attached to the guidance is a fillable PDF document for use as an instrument for standardised reporting of funding information.
Conclusion
Although the majority of RCTs report funding, there is considerable variability in the reporting of funding source, amount and roles of funders. A standardised approach to reporting of funding information would address these limitations. Future research should explore the implications of funding by not-for-profit organisations that are supported by for-profit organisations.
Keywords: funding, role of funder, randomised controlled trial
Strengths and limitations of this study.
First cross-sectional survey of a large and representative sample of clinical randomised controlled trials (RCTs) to describe the characteristics of the funding statements in detail.
Provides a proposed guidance and instrument for standardised reporting of funding information.
Use of systematic and transparent methods, for example, duplicate and independent processes in screening and data collection.
Includes trials limited to the clinical field and so our findings may not apply similarly to other fields such as public health research.
Background
Funding sources may influence the reporting of research findings and the interpretation of results.1–6 One study found that 86% of trial protocols documented an industry partner’s right to disapprove or review proposed manuscripts.7 This might also apply to other types of funders, for example, government. Reporting of funding in trials may appropriately influence how physicians interpret and use trial findings in clinical practice.8 9 The Consolidated Standards of Reporting Trials (CONSORT) checklist recognises this issue by including a section on reporting of funding.10 11
Reports in the lay media have documented how for-profit organisations support research through not-for-profit organisations.12 13 In one example, The Independent recently highlighted a systematic review suggesting that the consumption of low-energy sweeteners in place of sugar reduces energy intake and body weight.14 The review authors list the International Life Sciences Institute as the study funder. While the Institute describes itself as ‘a non-profit, worldwide organisation whose mission is to provide science that improves human health’, it receives funding primarily from companies such as the Coca-Cola Company, PepsiCo and Nestlé.15 Other examples of not-for-profit organisations funded by industry and supporting research are the Sugar Association16 17 and the now defunct Global Energy Balance Network.18
We conducted a comprehensive review of the literature and found 22 studies that assessed reporting of funding in clinical trials (see online supplementary appendix 1).5 19–39 The main gap we identified in this literature is a detailed and current characterisation of funding of a representative sample of trials. Indeed, all of the identified studies focused on trials published in specific clinical areas or journals. Most (14, 64%) reported only on funded trials or did not differentiate between non-funded trials and those that do not report on funding. Seventeen studies (77%) did not always distinguish trials with no funding from those funded by the government or by not-for-profit sources. Moreover, these studies seldom assessed reporting on the role of funder (n=4), provision of supplies (n=2) and the amount of funding (n=0). None of the studies explored the relationship between not-for-profit organisations funding trials and for-profit organisations.
bmjopen-2017-015997supp001.pdf (279.8KB, pdf)
Therefore, the main objective of this study was to provide a detailed and current characterisation of funding of a representative sample of clinical trials. We also aimed to develop guidance for standardised reporting of funding information.
Methods
Design overview and definitions
We followed systematic methodology to conduct a cross-sectional survey of published randomised controlled trials (RCTs). We define funding as any support (eg, monetary support, provision of supplies, assistance in manuscript writing). We considered as funding statement any text in the trial report providing any information regarding the funding of the trial, including a statement of no funding. A funding statement could indicate more than one funding contribution.
Eligibility criteria
We included reports of studies described as RCTs comparing at least two therapeutic interventions of any type in humans and published in English. We included RCTs with cross-over designs and secondary reports of trials (ie, follow-up study, post hoc analysis, interim analysis, prespecified analysis or secondary outcomes or substudy of a trial). We excluded non-randomised trials, trials addressing basic sciences topics and non-clinical interventions, and research letters.
Search strategy
We searched Ovid Medline in September 2015 and limited our search to the year 2015 and the 119 Core Clinical Journals (Abridged Index Medicus).40 We applied the search filter obtained from the Cochrane handbook to identify RCTs. See online supplementary appendix 2 for the detailed search strategy.
Selection process
We used an online sequence generator (www.random.org/sequences) to randomise the citations captured by the search. We followed the order of the randomisation list to screen citations until we obtained 200 eligible RCTs. Our sample size allows for a narrow 95% CI (±5%) around proportions of studies reporting sources of funding.
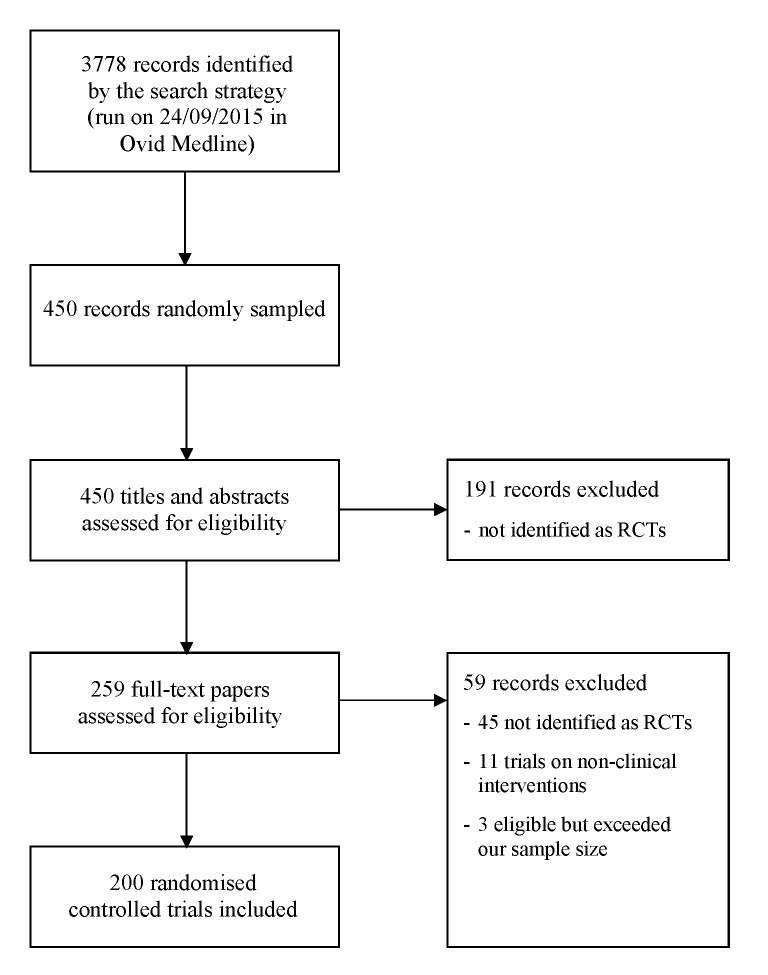
Following calibration exercises, three reviewers (MBH, NJ, MK) worked in teams of two (MBH was the reviewer on both) to screen titles and abstracts in duplicate and independently, using EndNote X7.5 software (Thomson Reuters, Philadelphia, Pennsylvania, USA). We obtained the full texts of citations judged as potentially eligible by either reviewer. The two teams of reviewers screened full texts in duplicate and independently. They resolved disagreements by discussion, or with the help of a third reviewer (EAA) as needed. A Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) study flow diagram41 presents the results of the selection process (figure 1).
Figure 1.
Study flow diagram. RCTs, randomised controlled trials.
Data extraction process
We developed a standardised data extraction form along with specific instructions. After pilot testing the form, we embedded it electronically into Research Electronic Data Capture (REDCap), a secure web-based application designed to support data capture for research studies.42 After completing calibration exercises, nine authors divided into teams of two extracted data in duplicate and independently (MBH was a reviewer on each of the eight teams). Each team compared results and resolved disagreements through discussion, or with the help of a third reviewer (EAA) as needed.
Data extracted
We extracted the following characteristics of the RCTs:
number of trial authors;
whether it is the first full-text report of the trial findings;
classification of the income level of the country in which the first author’s institution is located (as high, upper-middle, lower-middle or low-income country according to the July 2015 World Bank list of economies);
type of intervention and type of control;
number of trial sites;
number of randomised participants;
level of risk of bias associated with allocation concealment, a methodological feature as an indicator of risk of bias (based on the Cochrane Collaboration’s tool for assessing risk of bias);43
whether authors reported conflicts of interest;
whether the report included a funding statement.
We then focused on trials that included funding information. We extracted the following funding characteristics reported in the paper:
whether it reported funding versus no funding;
the type of source(s) of funding (see online supplementary appendix 3). These included internal funding (when it is an academic or hospital affiliation) and external funding, categorised into government, private-for-profit, private not-for-profit with evidence of support by private-for-profit that is a health industry, private not-for-profit with evidence of support by private-for-profit that is not a health industry and private not-for-profit with no evidence of support by private-for-profit. As needed, we performed an online search to accurately assign the type of the funding source. When a funding source was identified as a not-for-profit organisation, we searched the organisation’s website for any information on partnership with or support from a for-profit organisation (see online supplementary appendix 4 for details);
amount of funding;
whether the paper reported to be sponsored by a source different than the source of funding/support;
whether information was reported (across the paper) on supplies in trials on pharmacological or surgical interventions (ie, drugs, devices, equipment, samples or placebos) and whether the supplier is a funding source. We looked for that information in the funding statements, acknowledgement statements and the methods section.
Finally, and in trials that reported being funded, we assessed whether the role of funder was explicitly reported for any funder as involved or not involved in the process of the research study.
Data analysis
We assessed agreement between reviewers of each team for inclusion of RCTs at the full-text screening stage using chance-corrected agreement (kappa statistic). We conducted descriptive analyses of the general characteristics of the RCT, as well as the characteristics of the funding statement. We present summary data for categorical variables as frequencies and percentages and for continuous variables as median and IQR. All calculations used SPSS, V. 21.0 for Windows (SPSS, Chicago, Illinois, USA).
Candidate independent variables for multivariable logistic regression analyses to assess the predictors of reported funding and the role of funder included characteristics of the RCT and variables related to Journal policy for reporting funding (ie, journal requirement for reporting of funding, journal requirement for reporting on the role of funder). For variables related to journal policy for reporting funding information, we used unpublished data we had collected in mid-2014 for another cross-sectional survey.44
Development of the guidance
We used the following approach for developing the proposed guidance for standardised reporting of funding information. First, our classification of funding sources was based on one we had used in a previous study (governmental, private not-for-profit and private-for-profit)45 that we modified after a review of relevant literature5 22 27 and of journals’ policies on reporting of funding information (unpublished data from another cross-sectional survey).44 Second, we refined the classification through an iterative process of discussion and revisions based on funding statements reported in this sample of RCTs, as well as in a sample of systematic reviews.46 Finally, we used Adobe Acrobat XI software to develop a fillable PDF document for use as an instrument for standardised reporting of funding information.
The process included both in-person and email discussions among the authors of this article and feedback from external experts. The individuals involved have the following profiles: author EAA is a clinical epidemiologist and was an associate journal editor for Health and Quality of Life Outcomes journal; author GG is a clinical epidemiologist and has been a member of editorial boards of eight journals. The external experts we consulted include Dr Elie Al-Chaer (health researcher with a law degree and editor-in-chief of International Journal of Women’s Health and Dove Press), Dr Joerg Meerpohl (associate editor of Health and Quality of Life Outcomes journal) and Dr Peter Tugwell (co-editor of the Journal of Clinical Epidemiology).
Results
Figure 1 presents the study flow diagram. Agreement proved substantial (kappa=0.78) and near perfect (kappa=0.86) respectively for each of the two teams at the full-text screening stage.
Characteristics of the RCT
The first authors of most trials (90%) had affiliations in high-income countries and almost half (49%) assessed pharmacological interventions (table 1). About half the trials (54%) were multicentre, and had two as the median number of sites. Most trials (94%) reported on conflicts of interest and 54% disclosed presence of conflicts of interest. Almost all (178, 89%) included a funding statement.
Table 1.
General characteristics of the included randomised controlled trials (n=200)
| Overall | |
| n (%)* | |
| Number of trial authors; median (IQR) | 9 (6–14)† |
| Paper is the first full-text report of the trial findings | 171 (86%) |
| Classification of the income level of the country in which the first author’s institution is located: | |
| High income | 179 (90%) |
| Upper middle income | 15 (8%) |
| Lower middle income | 4 (2%) |
| Low income | 2 (1%) |
| Type of intervention | |
| Pharmacological | 97 (49%) |
| Surgical/invasive procedure | 42 (21%) |
| Non-invasive procedure | 11 (6%) |
| Lifestyle intervention | 15 (8%) |
| Screening/diagnostic intervention | 9 (5%) |
| Psycho-therapeutic intervention | 4 (2%) |
| Rehabilitation | 6 (3%) |
| Other | 16 (8%) |
| Type of control | |
| Active control (as opposed to non-active) | 82 (41%) |
| Number of trial sites; median (IQR) | 2 (1–17) |
| Number of randomised participants; median (IQR) | 160 (60–485) |
| Level of risk of bias associated with allocation concealment | |
| High risk | 4 (2%) |
| Low risk | 59 (30%) |
| Unclear | 137 (69%) |
| Reporting of conflicts of interest | |
| Not reported | 12 (6%) |
| Reported with no conflicts of interest disclosed | 80 (40%) |
| Reported with conflicts of interest disclosed | 108 (54%) |
| Inclusion of a funding statement | |
| Included (as opposed to not included) | 178 (89%) |
*For continuous variables, numbers refer to median (IQR), indicated in the relevant row.
†The number of trial authors per trial ranged between 1 and 91.
Characteristics of the reported funding
Table 2 presents the characteristics of the reported funding of the 178 trials with a funding statement, of which 171 (96%) reported being funded. The median number (IQR) of funding sources for each funded trial was 1 (1–3), with a range of 1 to 12 sources per trial. The top most frequent sources of funding were governmental (58%) and private-for-profit (40%). Of the 54 funding contribution statements in which the source was identified as being a not-for-profit organisation, we found evidence of support of those organisations from private-for-profit entity(ies) in 29 (54%), of which 26 (48%) did not disclose this support in the study report. Twenty-one trials (12%) reported funding from private-for-profit in addition to another source. Two trials reported the amount of funding received. Of the 139 RCTs assessing pharmacological or surgical interventions, 29 (21%) reported information on the supplier of the medication or device.
Table 2.
Characteristics of the funding statements included in the randomised controlled trials (n=178 trials)
| Overall | |
| n (%) | |
| Funding statement reported being: | |
| Funded (as opposed to not funded) | 171 (96) |
| Source(s) of funding (when reported as funded, n=171)* | |
| Internally funded | 26 (15) |
| Externally funded by: | |
| Government | 99 (58) |
| Private-for-profit | 68 (40) |
| Private not-for-profit with evidence of support by private-for-profit that is a health industry | 14 (8) |
| Private not-for-profit with evidence of support by private-for-profit that is not a health industry | 15 (9) |
| Private not-for-profit with no evidence of support by private-for-profit | 25 (15) |
| Statement included amount of funding received | 2 (1) |
| Paper reported to be sponsored by a source different than the source of funding/support | 2 (1) |
| Paper reported information on supplies (ie, drugs, devices, equipment, samples or placebos)† | |
| Yes, supplied by manufacturer same as funder | 12 (9) |
| Yes, supplied by manufacturer different than funder | 17 (12) |
| Not reported | 110 (79) |
*More than one type could apply for trials reporting more than one source of funding.
†Calculated using the number of trials on pharmacological interventions and surgical/invasive procedures (n=139).
The reported roles of funders
Table 3 presents the reported roles of funders in the 171 trials that reported being funded. Eighty-five trials (50%) indicated the role of funders and provided descriptions of 22 different roles. The most frequent roles indicated in these 85 trials were participation in the design of the study (42%), data collection (27%), data analysis, interpretation or management (41%), manuscript preparation (32%), decision to submit the manuscript (15%) and conduct of the study (15%).
Table 3.
Reporting on the roles of funders in the randomised controlled trials that reported being funded (n=171)
| Reported role as: | Did not report role | ||
| Not involved | Involved | ||
| n (%) | n (%) | n (%) | |
| Any role of the below | 41 (24) | 44 (26) | 86 (50) |
| Protocol/design of the study | 41 (24) | 30 (18) | 100 (58) |
| Data collection | 31 (18) | 16 (9) | 124 (73) |
| Verifying data accuracy/fact checking | 0 (0) | 3 (2) | 168 (98) |
| Outcome adjudication | 0 (0) | 1 (1) | 170 (99) |
| Data analysis/interpretation/management | 40 (23) | 31 (19) | 100 (58) |
| Funded a medical writer | 1 (1) | 19 (11) | 151 (88) |
| Preparation of the manuscript | 34 (20) | 20 (12) | 117 (68) |
| Review of the manuscript | 17 (10) | 7 (4) | 147 (86) |
| Approval of the manuscript | 17 (10) | 8 (5) | 146 (85) |
| Decision to submit the manuscript | 18 (10) | 6 (4) | 147 (86) |
| Appointed an independent data and safety monitoring board | 0 (0) | 1 (1) | 170 (99) |
| Auditing of study conduct | 0 (0) | 3 (2) | 168 (98) |
| Management | 0 (0) | 3 (2) | 168 (98) |
| Team assembly | 0 (0) | 2 (1) | 169 (99) |
| Conduct of study | 13 (8) | 12 (7) | 146 (85) |
| Generated randomisation list | 0 (0) | 3 (2) | 168 (98) |
| Enrolment of participants | 0 (0) | 1 (1) | 170 (99) |
| Logistical support | 0 (0) | 3 (2) | 168 (98) |
| Holding study data | 0 (0) | 1 (1) | 170 (99) |
| Study oversight | 0 (0) | 2 (1) | 169 (99) |
| Steering committee | 0 (0) | 1 (1) | 170 (99) |
| Measurement of study variable | 0 (0) | 5 (3) | 166 (97) |
Results of the regression analyses
Online supplementary appendix 5 presents the details of the multivariable logistic regression analyses. Reporting being funded was positively associated with two variables (table 4), based on data from all included trials (n=200). Explicit reporting on the role of funder was positively associated with three variables (table 4), based on data from trials reporting being funded (n=171).
Table 4.
Results of the multivariable regression analysis
| Dependent variables | Independent variables | Adjusted OR (95% CI) |
p Value |
| ‘Reporting being funded’ model (n=200) | Journal impact factor | 1.44 (1.09 to 1.90) |
0.011 |
| Affiliation with an institution from a high-income country (reference category being middle or low-income countries) | 0.09 (0.02 to 0.37) |
0.001 | |
| ‘Explicit reporting on the role of funder’ model (n=171) | Journal impact factor | 1.07 (1.04 to 1.10) |
<0.0001 |
| Journal requirement for reporting on the role of funder | 3.76 (1.64 to 8.62) |
0.002 | |
| Funding from private-for-profit source(s) (reference category being all other types of funding sources) | 5.7 (2.37 to 13.85) |
<0.0001 |
Proposed guidance
The proposed guidance provides suggestions for both funding information and the reporting process. Box 1 lists the funding information that relates to the phases of the research study for which the funding was received, the funding sources and the involvement of the funders in the process of the research study.
Box 1. Suggestions for what funding information to report.
Funding sources (and grant ID if applicable)
-
All types of funding sources, including the following with specifications:
Internal funding (specifying institution)
Government(s) (specifying granting agency, level of government)
Intergovernment (two or more government agencies such as the European Union)
Private-for-profit (listing companies/entities)
Private not-for-profit (listing organisations/philanthropies)
Research phases for which funding was received: planning, conduct and/or reporting of the research study under consideration. When funding relates to provision of supplies, the appropriate answer is ‘conduct’.
Type of funding received including monetary support, provision of supplies, and so on.
Value of monetary support and value of other supports.
Whether the funding provided by any of the funding sources is supported by an entity other than/external to the funding source.
Involvement (role) of funding sources
-
Involvement (role) of each funder in the process of the research study, including:
Study planning and conduct: design and protocol drafting, study management, participant recruitment, data collection, data management, data analysis, quality control.
Study reporting (manuscript): preparation, review, approval, decision to submit.
Authorship: authors employed by the funder.
As for the process of reporting funding information, we suggest that the corresponding author plays the role of the guarantor of this information (given his/her primary responsibility of communicating with both the journal and the readers) and take responsibility for
Collecting funding information and filling a standardised form
Sending the form to all coauthors for approval and verification of accuracy and completeness of the information
Submitting the up-to-date form at the time of submission of the manuscript for consideration for publication
Updating and re-submitting the form at the time of acceptance of the manuscript for final publication
Online supplementary appendix 6 provides a fillable PDF document for use as an instrument for standardised reporting of funding information.
bmjopen-2017-015997supp002.pdf (6.8MB, pdf)
Discussion
Summary of findings
The objective of this study was to describe the characteristics of the funding statements in reports of clinical trials. About nine in ten trial reports included a funding statement and 96% of those statements indicated that funding existed. The latter statements specified the source, amount and role of funders in 100%, 1% and 50% of cases, respectively. The most commonly reported sources of funding were government and private-for-profit sources. Of all funding contribution statements in which the source was identified as being a not-for-profit organisation, about half related to not-for-profit organisations for which we found evidence of support by private-for-profit entity(ies). Only three of those statements disclosed the support by the private-for-profit entities. For trials of pharmacological or surgical interventions, only a fifth reported information on the supplier of the medication or device. We identified descriptions of a total of 22 different roles for the funders. Trials most frequently reported on roles related to the design of the study, data collection, data analysis and manuscript preparation. We also propose a guidance and instrument for standardised reporting of funding information.
Reporting of funding
The high percentage of trials that reported being funded may be explained by the fact that conducting an RCT typically requires a large number of resources.47–49 Also, we found a positive association between reporting being funded and affiliation with an institution from a high-income country. This may reflect better opportunities for, and higher ability of, institutions from high-income countries to obtain funding.
Explicit reporting on the role of funder was associated with journal requirement for reporting on the role of funder. This might explain the relatively low percentage of trials that reported on the roles of funders given that only 31% of clinical journals require authors to state the role of funder (unpublished data from another cross-sectional survey44). Explicit reporting on the role of funder was positively associated with trial funding from private-for-profit sources. This may be due to the adherence of the industry to higher standards of reporting. Indeed, several studies found that industry-funded trials had higher quality scores as compared with trials funded by other sources.24 50–53
Both reporting being funded and explicit reporting on the role of funder were associated with higher journal impact factor. This is consistent with our previous findings that better reporting of authors’ conflicts of interest is associated with higher journal impact factor for both systematic reviews and trials published in Core Clinical Journals.46 54
We found that half of not-for-profit organisations included in funding contribution statements were supported by private-for-profit entity(ies). This is probably an underestimate due to lack of reporting of such support by authors. This also suggests that these types of relationships are prevalent. Indeed, one recent study found that 96 national health organisations accepted money from the Coca-Cola Company, PepsiCo or both,55 with a number of these organisations known to fund research (eg, Juvenile Diabetes Research Foundation). This is very concerning given that the appearance of support by a not-for-profit may portray confidence in the study findings, in spite of the fact that the indirect for-profit support may have biased those findings. Indeed, while we explored whether private not-for-profit organisations were supported by private-for-profit entity(ies), this may also apply to other types of funding sources.
Strengths and limitations
This is the first cross-sectional survey of a large and representative sample of clinical RCTs to describe the characteristics of the funding statements in detail. Our proposed guidance and instrument for standardised reporting of funding information may serve researchers from different fields of health. Moreover, they may be used for other types of research studies and manuscripts and not only trials (eg, systematic reviews). In addition, we used systematic and transparent methods for screening and data collection.
As our study focused on clinical trials, our findings may not apply similarly to other fields, for example, health policy and systems research. While we did not conduct a formal and extensive validation of the guidance (and instrument), we believe that it has both face and content validity given that we based it on a thorough review of the related literature, on the cross-sectional survey of trials, and we revised it based on feedback from journal editors and a lawyer.
Comparison to similar studies
We identified 22 studies on the reporting of funding information in clinical trials (see online supplementary appendix 1).5 19–39 While all 22 studies focused on trials published in specific clinical areas or journals, our study assessed a wide sample of clinical trials published in any of the Core Clinical Journals. None of the 22 studies looked at whether the amount of funding was reported. In fact, we found that two trials in our sample reported amount. Two out of the 22 studies assessed reporting of provision of supplies in trials published between 1987 and 1994.34 39 To our knowledge, our study is the first one to survey a recent sample of trials for reporting of amount of funding and information on supplies.
Only 4 out of the 22 studies assessed reporting on the roles of funders.20 22 28 36 Whereas these studies assessed this in industry-funded or partially industry-funded trials, we assessed this across all types of funders. For example, we found that 44% of trials funded solely by governmental sources reported on the role of funder. Example statements from those that reported involvement of the government as a funder include ‘appointed an independent data and safety monitoring board’, ‘had input into the study design and data interpretation’ and ‘reviewed and approved the report’.
Our previous study on clinical systematic reviews found that a third of systematic reviews did not report on funding or reported no funding in comparison to 15% of trials in this study.46 When the included systematic reviews reported being funded, the most commonly reported sources of funding were internal funding and government (52% and 67%, respectively). While only 2% of clinical systematic reviews reported funding from private-for-profit sources, we found that 40% of clinical trials reported such funding. Moreover, trials were twice more likely than systematic reviews to report on not-for-profit as their funding source (32% and 16%, respectively). While half of funded trials reported on the role of the funder, a quarter of funded systematic reviews did so.
In comparison to the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT)56 57 and the CONSORT checklist sections on funding,10 11 our guidance provides more detailed and specific recommendations for the reporting of funding information and includes detailed definitions and examples of types of funders. It also includes a clear classification of roles in which funders may be involved in the process of the trial. Whereas the International Committee of Medical Journal Editors conflict of interest disclosure form includes a section for the reporting of ‘financial support’, the questions and options that follow imply types of financial conflicts of interest for each individual author rather than the study’s funding.58
Implications for practice
Our proposed guidance may help with clearer and more detailed reporting of the characteristics of funding in trials. This may in turn help readers and systematic reviewers better assess the significance of the funding and how it might affect the credibility of findings.8 59 Specifically, we recommend that trial authors explicitly report more details on the funders, whether they are supported by for-profit organisations, the provision of drugs and equipment,11 and on the role of funders.20 22 28 36 We suggest that authors do not to report funding information (ie, grants received for the conduct of the study) in both the funding section and the conflict of interest section of the manuscript, but only in the former one. Also, our findings have implications for reporting statements (such as SPIRIT and CONSORT) for improving the reporting of funding information.
Implications for future research
Future research should further explore the issue of funding of not-for profit organisations by for-profit organisations and the role of the latter in the planning, conduct and reporting of research studies. Future research could also assess for the accuracy and completeness of reporting of trial funding and roles of funders. Moreover, it would be interesting to explore reporting of funding in primary studies of other research fields (eg, health policy and systems), especially that roles of funders may vary from those described in clinical trials. Finally, our proposed guidance and instrument for the standardised reporting of funding information would benefit from formal and extensive validation.
Supplementary Material
Acknowledgments
We thank Dr Elie Al-Chaer, Dr Joerg Meerpohl and Dr Peter Tugwell for their expert opinion and constructive feedback on the proposed guidance and instrument for standardised reporting of funding information. We also thank the reviewers whose suggestions helped improve this manuscript.
Footnotes
Contributors: MBH, GG and EAA conceived and designed the study. MBH coordinated the study throughout. EAA had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. MBH, NJ and MK screened papers for inclusion. MBH, NJ, EAA-J, DJH, EAA-J, LCL, MZH, MA-G and SA extracted the data. MBH and EAA analysed and interpreted the data. MBH wrote the first draft of the manuscript with EAA. MBH and EAA developed the first draft of the fillable PDF document. All authors critically revised the manuscript and approved the final version.
Funding: This project was funded by the American University of Beirut Faculty of Medicine’s Medical Practice Plan (MPP) funds. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication. The authors and their contributions to the manuscript are independent from the funder.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data available upon request.
References
- 1. Amiri AR, Kanesalingam K, Cro S, et al. Does source of funding and conflict of interest influence the outcome and quality of spinal research? Spine J 2014;14:308–14. 10.1016/j.spinee.2013.10.047 [DOI] [PubMed] [Google Scholar]
- 2. Bartels RH, Delye H, Boogaarts J. Financial disclosures of authors involved in spine research: an underestimated source of bias. Eur Spine J 2012;21:1229–33. 10.1007/s00586-011-2086-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Crocetti MT, Amin DD, Scherer R. Assessment of risk of bias among pediatric randomized controlled trials. Pediatrics 2010;126:298–305. 10.1542/peds.2009-3121 [DOI] [PubMed] [Google Scholar]
- 4. Lundh A, Lexchin J, Mintzes B, et al. Industry sponsorship and research outcome. Cochrane Database Syst Rev 2017;2:MR000033 10.1002/14651858.MR000033.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mugambi MN, Musekiwa A, Lombard M, et al. Association between funding source, methodological quality and research outcomes in randomized controlled trials of synbiotics, probiotics and prebiotics added to infant formula: a systematic review. BMC Med Res Methodol 2013;13:137 10.1186/1471-2288-13-137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Riaz H, Raza S, Khan MS, et al. Impact of funding source on clinical trial results including cardiovascular outcome trials. Am J Cardiol 2015;116:1944–7. 10.1016/j.amjcard.2015.09.034 [DOI] [PubMed] [Google Scholar]
- 7. Kasenda B, von Elm E, You JJ, et al. Agreements between industry and academia on publication rights: a retrospective study of protocols and publications of randomized clinical trials. PLoS Med 2016;13:e1002046 10.1371/journal.pmed.1002046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kesselheim AS, Robertson CT, Myers JA, et al. A randomized study of how physicians interpret research funding disclosures. N Engl J Med 2012;367:1119–27. 10.1056/NEJMsa1202397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Coultas D. Ethical considerations in the interpretation and communication of clinical trial results. Proc Am Thorac Soc 2007;4:194–9. discussion 198-9 10.1513/pats.200701-007GC [DOI] [PubMed] [Google Scholar]
- 10. Schulz KF, Altman DG, Moher D, et al. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol 2010;63:834–40. 10.1016/j.jclinepi.2010.02.005 [DOI] [PubMed] [Google Scholar]
- 11. Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 Explanation and Elaboration: Updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol 2010;63:e1–e37. 10.1016/j.jclinepi.2010.03.004 [DOI] [PubMed] [Google Scholar]
- 12. The Independent. A recent study that said Diet Coke can help you lose weight was quietly funded by Coca-Cola, Sunday 17 January 2016. http://www.independent.co.uk/news/science/study-that-said-diet-fizzy-drunks-can-help-weight-loss-was-quietly-funded-by-coca-cola-and-pepsi-a6817686.html
- 13. The New York Times. Coca-Cola funds scientists who shift blame for obesity away from bad diets, august 9, 2015. http://well.blogs.nytimes.com/2015/08/09/coca-cola-funds-scientists-who-shift-blame-for-obesity-away-from-bad-diets/?_r=0
- 14. Rogers PJ, Hogenkamp PS, de Graaf C, et al. Does low-energy sweetener consumption affect energy intake and body weight? A systematic review, including meta-analyses, of the evidence from human and animal studies. Int J Obes 2016;40:381–94. 10.1038/ijo.2015.177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. International Life Sciences Institute. Mission & operating principles. 2016. http://ilsi.org/about/mission/
- 16. The Sugar Association, I. Research. https://www.sugar.org/research/ (accessed on 15 Nov 2016).
- 17. Kearns CE, Schmidt LA, Glantz SA. Sugar industry and coronary heart disease research: a historical analysis of internal industry documents. JAMA Intern Med 2016;176:1680–5. 10.1001/jamainternmed.2016.5394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kmietowicz Z. Coca-Cola funded group set up to promote ‘energy balance’ is disbanded. BMJ 2015;351:h6590 10.1136/bmj.h6590 [DOI] [PubMed] [Google Scholar]
- 19. Als-Nielsen B, Chen W, Gluud C, et al. Association of funding and conclusions in randomized drug trials: a reflection of treatment effect or adverse events? JAMA 2003;290:921–8. 10.1001/jama.290.7.921 [DOI] [PubMed] [Google Scholar]
- 20. Bero L, Oostvogel F, Bacchetti P, et al. Factors associated with findings of published trials of drug-drug comparisons: why some statins appear more efficacious than others. PLoS Med 2007;4:e184 10.1371/journal.pmed.0040184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bhandari M, Busse JW, Jackowski D, et al. Association between industry funding and statistically significant pro-industry findings in medical and surgical randomized trials. CMAJ 2004;170:477–80. [PMC free article] [PubMed] [Google Scholar]
- 22. Bridoux V, Moutel G, Schwarz L, et al. Disclosure of funding sources and conflicts of interest in phase III surgical trials: survey of ten general surgery journals. World J Surg 2014;38:2487–93. 10.1007/s00268-014-2580-5 [DOI] [PubMed] [Google Scholar]
- 23. Clifford TJ, Barrowman NJ, Moher D. Funding source, trial outcome and reporting quality: are they related? Results of a pilot study. BMC Health Serv Res 2002;2:18 10.1186/1472-6963-2-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Djulbegovic B, Lacevic M, Cantor A, et al. The uncertainty principle and industry-sponsored research. Lancet 2000;356:635–8. 10.1016/S0140-6736(00)02605-2 [DOI] [PubMed] [Google Scholar]
- 25. Etter JF, Burri M, Stapleton J. The impact of pharmaceutical company funding on results of randomized trials of nicotine replacement therapy for smoking cessation: a meta-analysis. Addiction 2007;102:815–22. 10.1111/j.1360-0443.2007.01822.x [DOI] [PubMed] [Google Scholar]
- 26. Hodgson R, Allen R, Broderick E, et al. Funding source and the quality of reports of chronic wounds trials: 2004 to 2011. Trials 2014;15:19 10.1186/1745-6215-15-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Khan NA, Lombeida JI, Singh M, et al. Association of industry funding with the outcome and quality of randomized controlled trials of drug therapy for rheumatoid arthritis. Arthritis Rheum 2012;64:2059–67. 10.1002/art.34393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lundh A, Krogsbøll LT, Gøtzsche PC. Sponsors' participation in conduct and reporting of industry trials: a descriptive study. Trials 2012;13:146 10.1186/1745-6215-13-146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Momeni A, Becker A, Bannasch H, et al. Association between research sponsorship and study outcome in plastic surgery literature. Ann Plast Surg 2009;63:661–4. 10.1097/SAP.0b013e3181951917 [DOI] [PubMed] [Google Scholar]
- 30. Montgomery JH, Byerly M, Carmody T, et al. An analysis of the effect of funding source in randomized clinical trials of second generation antipsychotics for the treatment of schizophrenia. Control Clin Trials 2004;25:598–612. 10.1016/j.cct.2004.09.002 [DOI] [PubMed] [Google Scholar]
- 31. Peppercorn J, Blood E, Winer E, et al. Association between pharmaceutical involvement and outcomes in breast cancer clinical trials. Cancer 2007;109:1239–46. 10.1002/cncr.22528 [DOI] [PubMed] [Google Scholar]
- 32. Perlis CS, Harwood M, Perlis RH. Extent and impact of industry sponsorship conflicts of interest in dermatology research. J Am Acad Dermatol 2005;52:967–71. 10.1016/j.jaad.2005.01.020 [DOI] [PubMed] [Google Scholar]
- 33. Ridker PM, Torres J. Reported outcomes in major cardiovascular clinical trials funded by for-profit and not-for-profit organizations: 2000-2005. JAMA 2006;295:2270–4. 10.1001/jama.295.19.2270 [DOI] [PubMed] [Google Scholar]
- 34. Rochon PA, Gurwitz JH, Simms RW, et al. A study of manufacturer-supported trials of nonsteroidal anti-inflammatory drugs in the treatment of arthritis. Arch Intern Med 1994;154:157–63. 10.1001/archinte.1994.00420020059007 [DOI] [PubMed] [Google Scholar]
- 35. Shah RV, Albert TJ, Bruegel-Sanchez V, et al. Industry support and correlation to study outcome for papers published in Spine. Spine 2005;30:1099–104. discussion 1105 10.1097/01.brs.0000161004.15308.b4 [DOI] [PubMed] [Google Scholar]
- 36. Tuech JJ, Moutel G, Pessaux P, et al. Disclosure of competing financial interests and role of sponsors in phase III cancer trials. Eur J Cancer 2005;41:2237–40. 10.1016/j.ejca.2004.12.036 [DOI] [PubMed] [Google Scholar]
- 37. Tungaraza T, Poole R. Influence of drug company authorship and sponsorship on drug trial outcomes. Br J Psychiatry 2007;191:82–3. 10.1192/bjp.bp.106.024547 [DOI] [PubMed] [Google Scholar]
- 38. Voineskos SH, Coroneos CJ, Ziolkowski NI, et al. A systematic review of surgical randomized controlled trials: part 2. Funding source, conflict of interest, and sample size in plastic surgery. Plast Reconstr Surg 2016;137:453e–61. 10.1097/01.prs.0000475767.61031.d1 [DOI] [PubMed] [Google Scholar]
- 39. Yaphe J, Edman R, Knishkowy B, et al. The association between funding by commercial interests and study outcome in randomized controlled drug trials. Fam Pract 2001;18:565–8. 10.1093/fampra/18.6.565 [DOI] [PubMed] [Google Scholar]
- 40. U.S. National Library of Medicine. Abridged Index Medicus (AIM or ‘Core Clinical’) Journal Titles. 2016. https://www.nlm.nih.gov/bsd/aim.html (accessed on 2 May 2017).
- 41. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Med 2009;3:e123–30. [PMC free article] [PubMed] [Google Scholar]
- 42. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Table 8.5.d: Criteria for judging risk of bias in the ‘Risk of bias’ assessment tool. The Cochrane Collaboration, 2011. http://handbook.cochrane.org [Google Scholar]
- 44. Shawwa K, Kallas R, Koujanian S, et al. Requirements of clinical journals for authors’ disclosure of financial and non-financial conflicts of interest: a cross sectional study. PLoS One 2016;11:e0152301 10.1371/journal.pone.0152301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Akl EA, Carrasco-Labra A, Brignardello-Petersen R, et al. Reporting, handling and assessing the risk of bias associated with missing participant data in systematic reviews: a methodological survey. BMJ Open 2015;5:e009368 10.1136/bmjopen-2015-009368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hakoum MB, Anouti S, Al-Gibbawi M, et al. Reporting of financial and non-financial conflicts of interest by authors of systematic reviews: a methodological survey. BMJ Open 2016;6:e011997 10.1136/bmjopen-2016-011997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Glass HE, Hollander K. Managing clinical grant costs. Contemp Clin Trials 2009;30:221–6. 10.1016/j.cct.2009.02.001 [DOI] [PubMed] [Google Scholar]
- 48. Idoko OT, Kochhar S, Agbenyega TE, et al. Impact, challenges, and future projections of vaccine trials in Africa. Am J Trop Med Hyg 2013;88:414–9. 10.4269/ajtmh.12-0576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ravinetto R, De Nys K, Boelaert M, et al. Sponsorship in non-commercial clinical trials: definitions, challenges and the role of Good Clinical Practices guidelines. BMC Int Health Hum Rights 2015;15:34 10.1186/s12914-015-0073-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Pengel LH, Barcena L, Morris PJ. The quality of reporting of randomized controlled trials in solid organ transplantation. Transpl Int 2009;22:377–84. 10.1111/j.1432-2277.2008.00789.x [DOI] [PubMed] [Google Scholar]
- 51. Rios LP, Odueyungbo A, Moitri MO, et al. Quality of reporting of randomized controlled trials in general endocrinology literature. J Clin Endocrinol Metab 2008;93:3810–6. 10.1210/jc.2008-0817 [DOI] [PubMed] [Google Scholar]
- 52. Yuen SY, Pope JE. Learning from past mistakes: assessing trial quality, power and eligibility in non-renal systemic lupus erythematosus randomized controlled trials. Rheumatology 2008;47:1367–72. 10.1093/rheumatology/ken230 [DOI] [PubMed] [Google Scholar]
- 53. Lexchin J, Bero LA, Djulbegovic B, et al. Pharmaceutical industry sponsorship and research outcome and quality: systematic review. BMJ 2003;326:1167–70. 10.1136/bmj.326.7400.1167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Hakoum MB, Jouni N, Abou-Jaoude EA, et al. Authors of clinical trials reported individual and financial conflicts of interest more frequently than institutional and nonfinancial ones: a methodological survey. J Clin Epidemiol 2017. 10.1016/j.jclinepi.2017.04.002 [DOI] [PubMed] [Google Scholar]
- 55. Aaron DG, Siegel MB. Sponsorship of National Health Organizations by two major Soda companies. Am J Prev Med 2017;52:20–30. 10.1016/j.amepre.2016.08.010 [DOI] [PubMed] [Google Scholar]
- 56. Chan AW, Tetzlaff JM, Altman DG, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med 2013;158:200–7. 10.7326/0003-4819-158-3-201302050-00583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Chan AW, Tetzlaff JM, Gøtzsche PC, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. International Committee of Medical Journal Editors. Conflict of Interest Disclosure Forms. http://www.icmje.org/about-icmje/faqs/conflict-of-interest-disclosure-forms/ (accessed on 3 May 2017).
- 59. Elia N, von Elm E, Chatagner A, et al. How do authors of systematic reviews deal with research malpractice and misconduct in original studies? A cross-sectional analysis of systematic reviews and survey of their authors. BMJ Open 2016;6:e010442 10.1136/bmjopen-2015-010442 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-015997supp001.pdf (279.8KB, pdf)
bmjopen-2017-015997supp002.pdf (6.8MB, pdf)