Abstract
Objectives:
To review the characteristics of and to identify the reasons for severe maternal admissions to the ICU.
Design:
This was an analytical, observational, open, and retrospective study.
Setting:
In our ICU.
Patients:
A total of 487 severe maternal cases were reviewed during the 8-year study period of January 2009 to December 2016.
Intervention:
None.
Measurements and Main Results:
A total of 487 severe maternal cases (12.6%) among the 3,867 patients admitted to ICU were reviewed. Of these, 361 patients were admitted for obstetric reasons, mainly pregnancy-induced hypertension (58.7%) and postpartum hemorrhage (36.8%). The remaining 126 patients were admitted for nonobstetric reasons, including cardiac-related disease (31.0%), immune-related disease (24.6%), and sepsis (20.6%). A total of 249 patients experienced combined comorbidities: the most common was a scarred uterus (100 patients; 40.2%), followed by endocrine-related disease (25.3%), immune-related disease (21.3%), and cardiac-related disease (18.1%). Central venous insertion (90.6%) was the most common intervention, followed by arterial catheter insertion (33.7%), mechanical ventilation (11.7%), blood purification (5.7%), and invasive hemodynamic monitoring (3.7%). Nine patients died during the study period, of which the death of four could have been avoided.
Conclusions:
The number of severe maternal cases has increased annually in our ICU. Although obstetric causes remained the most common reason for admission, the nonobstetric causes and basic complications were too complex, dangerous, and beyond the reach of the obstetrician with regard to monitoring and treatment. We call for a multidisciplinary team mainly composed of ICU staff to improve severe maternal outcomes.
Keywords: intensive care unit, multidisciplinary team, severe maternal
Maternal mortality is an important quality assurance indicator of basic healthcare and an indicator of the level of development of a country. China has made substantial progress in reducing maternal mortality over recent decades: the maternal mortality rate (MMR) has reduced from 80.0 per 100,000 live births in 1991 to 24.5 per 100,000 in 2012 (1). However, the absolute number of maternal deaths remains high because of China’s big population base. In addition, it is very difficult to reduce the MMR because of disparate regional economic conditions.
In recent years, an increasing number of severe maternal (SM) patients have been admitted to our unit mainly for two reasons. First, the progress made in intensive medicine, reproductive medicine, and other related clinical specialties has led to many women with comorbidities such as heart disease, diabetes, hypertension, lupus erythematosus, and kidney dysfunction being squeezed into the crowd of high-risk pregnancy groups; this has led to an increase in the number of cases and severity of SM. In addition, the spectrum of SM has changed, and the challenges of the disease are now beyond the scope of the skills of obstetric specialists. Second, the changing population policy in China has made the situation of SM rescue worse. Since the early 1970s, the Chinese government has implemented a family planning policy beginning with only one child per couple; it was not until 2014 that two children for partial couples were permitted, and it was not until 2016 that two children were permitted. There were too many women 35 years old or older who were eager to have a second baby, and many of these had a history of abuse of cesarean delivery. This means that severe complications, both obstetric and nonobstetric, have increased.
The ICU is becoming a main battlefield for SM rescue in China. Therefore, we performed a retrospective analysis on SM in the last 8 years (from January 2009 to December 2016) in our unit. The results led us to call for a multidisciplinary team (MDT) mainly composed of ICU staff to reduce the MMR.
MATERIALS AND METHODS
This is a descriptive study of consecutive obstetric patients admitted to the ICU of The Second Clinical Hospital of Fujian Medical University of China from January 2009 to December 2016. Our ICU was a 10-bed closed unit in 2009, and 18 beds were added from 2012; it admits ~500 patients annually. We bear the regional rescue work of SM and account for above 10 million inhabitants.
A total of 487 women in our ICU at any time of pregnancy or within 42 days of termination of pregnancy were analyzed, regardless of the reason for hospitalization. All the patients remained in the ICU for at least 24 hours, and their baseline data were collected by the Medical Records Department. The admission books of the ICU were also used to obtain more detailed information. All data of patients were checked by three doctors to reduce mistakes.
The following data were recorded: demographic characteristics; medical history; pregnancy-related situations; mode of delivery; entry status and time; Acute Physiology and Chronic Health Evaluation (APACHE) II score (2); length of ICU stay; and the number of hysterectomies, stillbirths, and maternal deaths. The main obstetric reasons for ICU admission included postpartum hemorrhage, pregnancy-induced hypertension (PIH), amniotic fluid embolism, ruptured ectopic pregnancy, antepartum hemorrhage, and puerperal infection. The main nonobstetric reasons for admission were sepsis, cardiac-related disease, endocrine-related disease, immune-related disease, asthma, trauma, renal-related disease, pancreatitis, and cerebrovascular accident. Obstetric disorders were defined as specific pregnancy-related conditions that occurred during pregnancy or in the first 42 days of the postpartum period. Nonobstetric conditions were defined as all other conditions that were not specifically pregnancy related. Any comorbidities (viral hepatitis type B carriers were not included) that led to ICU admission and main operations such as cardiopulmonary resuscitation (CPR), central venous catheter insertion, arterial catheter insertion, mechanical ventilation, blood purification, and invasive hemodynamic monitoring, as well as maternal deaths, were recorded and analyzed.
The following rules were used in collecting data: good health in the past means no basic disease before pregnancy, including no scarred uterus. The main reason for ICU admission was considered according to the following rules when several diseases coexisted: the priority sequence was eclampsia, postpartum hemorrhage, severe preeclampsia, and basic diseases. With regard to data regarding comorbidities for ICU admission, 18 women had two or more comorbidities, and all these complications were recorded at the same time.
The present study was approved by the ethics committee, and all information obtained was used only to describe the patient population and for data analysis. The results were expressed as numbers and percentages or means ± sds.
RESULTS
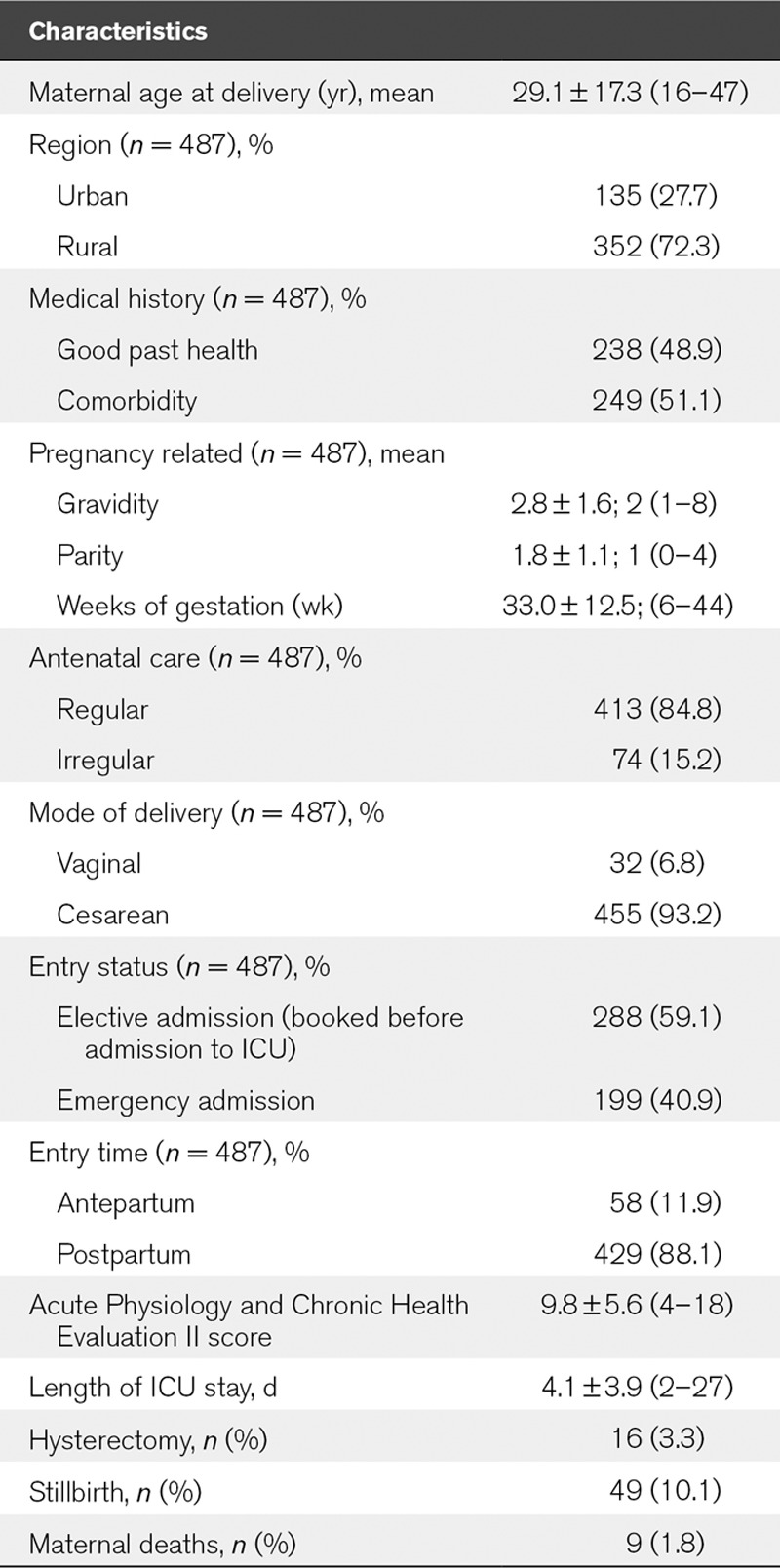
A total of 487 obstetric patients were admitted to the ICU during the study period, which represented 12.6% of the total ICU admissions and 1.6% of the total maternal in our hospital. The basic characteristics of the 487 patients are shown in Table 1. Most came from rural areas (72.3%; 352/487) and received regular antenatal care before admission (84.8%; 413/487). A total of 238 patients enjoyed good past health (48.9%; 238/487), and 199 patients were admitted to the ICU under emergency conditions (40.9%; 199/487). The entry time was mainly in the postpartum period (88.1%; 429/487), and the most common mode of delivery was cesarean (93.2%; 455/487). Sixteen patients (3.3%; 16/487) underwent a hysterectomy; there were 49 stillbirths (10.1%; 49/487), and nine patients (1.8%; 9/487) died.
TABLE 1.
Patient Characteristics From 2009 to 2016
Most patients were admitted for obstetric reasons (74.1%; 361/487), of which PIH was the most common (58.7%; 212/361), followed by postpartum hemorrhage (36.8%; 133/361) that was caused by uterine atony (38.3%; 51/133), placenta accrete (24.1%; 32/133), placenta previa (14.3%; 19/133), coagulation disorders (6.8%; 9/133), and other reasons (16.5%; 22/133) such as birth canal injury and uterine rupture. One hundred twenty-six patients (25.9%; 126/487) were admitted for nonobstetric reasons, most of which were cardiac-related disease (31.0%; 39/126), followed by immune-related disease (24.6%; 31/126) and sepsis (20.6%; 26/126) (Table 2).
TABLE 2.
Main Reason for ICU Admission From 2009 to 2016
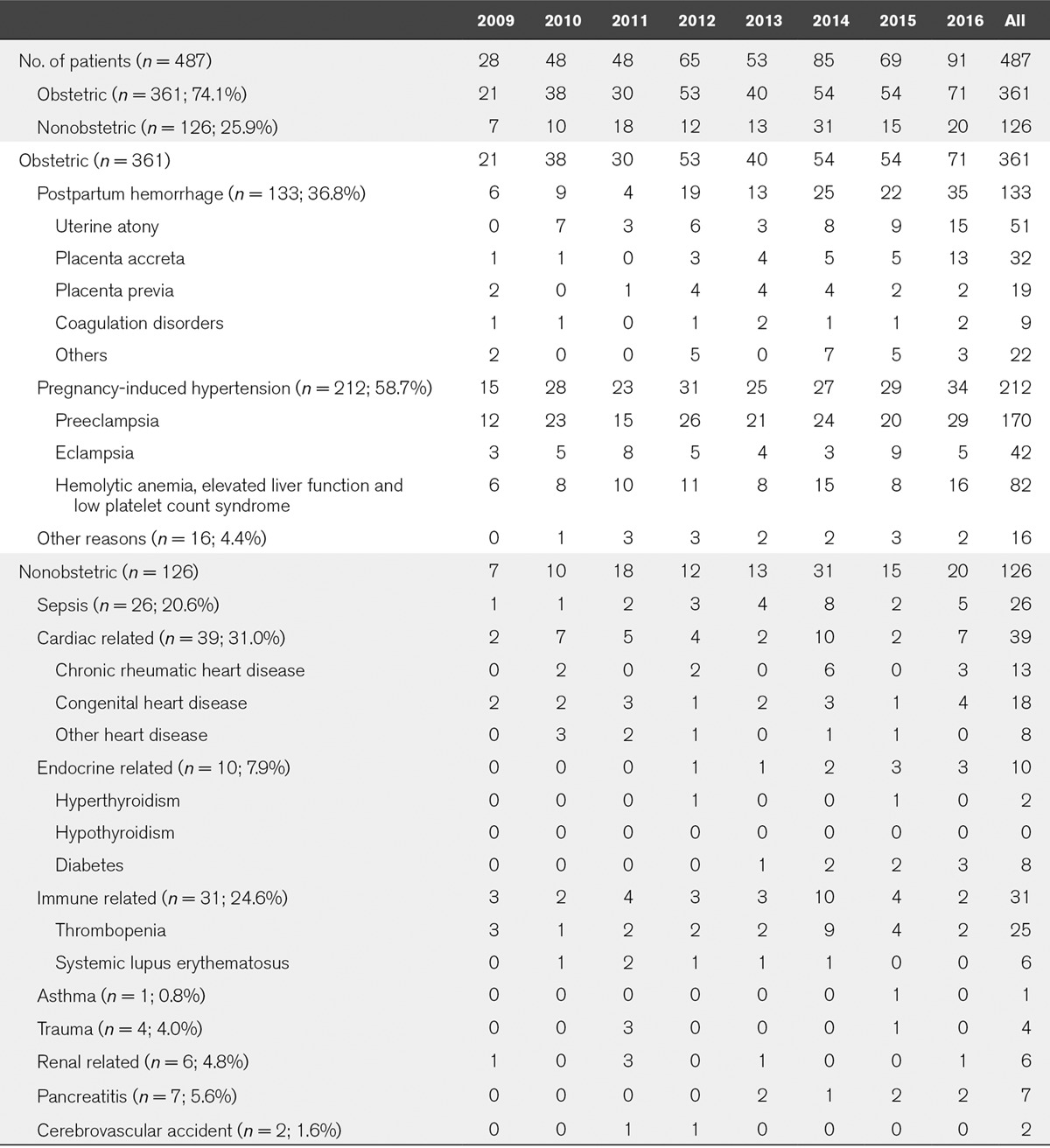
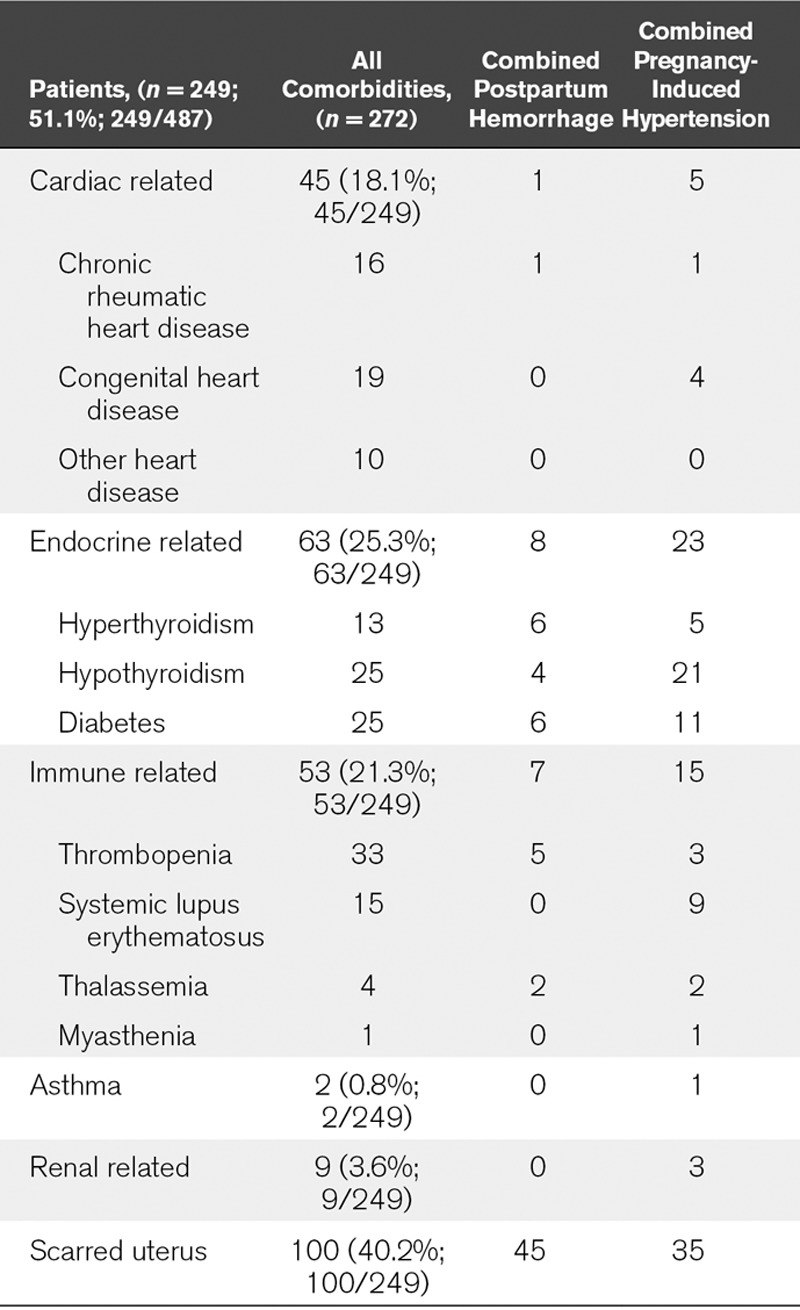
Table 3 shows the basic comorbidities at ICU admission from 2009 to 2016. Among the 249 patients with combined comorbidities, 100 (40.2%; 100/249) had a scarred uterus; the next most common comorbidities were endocrine-related disease (25.3%; 63/249), immune-related disease (21.3%; 53/249), and cardiac-related disease (18.1%; 45/249). All 249 patients with postpartum hemorrhage and PIH are listed in Table 3.
TABLE 3.
Basic Comorbidities for ICU Admission From 2009 to 2016
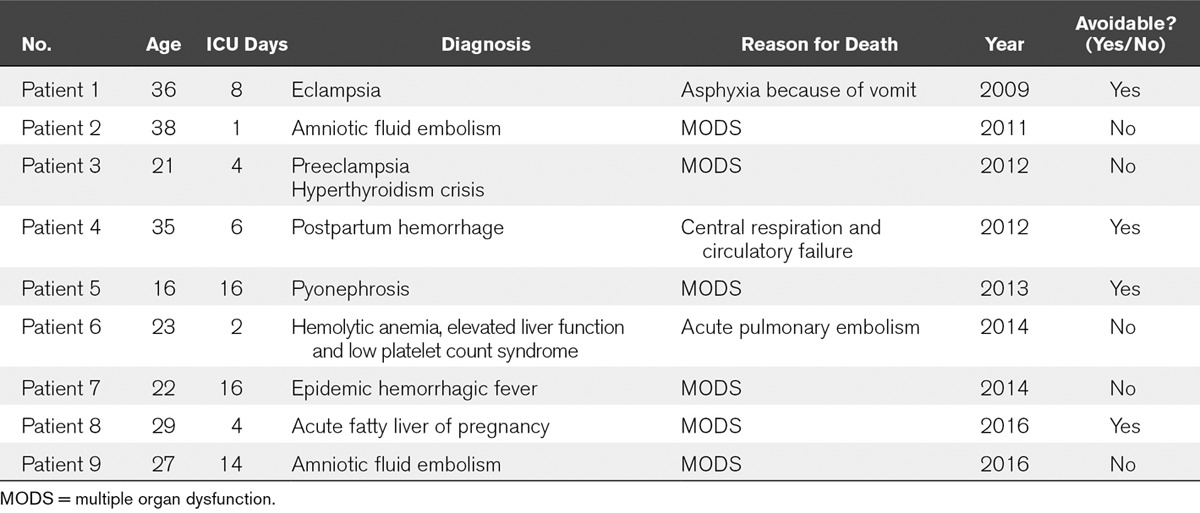
Central venous insertion (90.6%; 441/487) was the most common intervention in all patients, followed by arterial catheter insertion (33.7%; 164/487), mechanical ventilation (11.7%; 57/487), blood purification (5.7%; 28/487), and invasive hemodynamic monitoring (3.7%; 18/487). Four patients required CPR, of which one survived, two died, and one was in a vegetative state (Table 4). Nine mothers died during the study period; their basic data are listed in Table 5.
TABLE 4.
Main Operations Performed in the ICU From 2009 to 2016
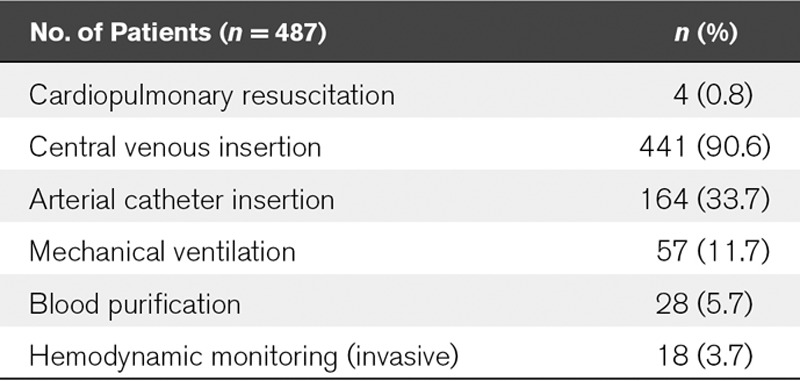
TABLE 5.
The Reasons for Maternal Death From 2009 to 2016
DISCUSSION
Although this is a single-center study, we were still able to observe the clinical characteristics of SM. This group was derived from a higher percentage of rural patients, some of whom failed to attend regular antenatal examinations and often came to the hospital in an emergency situation in a very dangerous state. Therefore, the government should adopt more effective interventions to improve patient prenatal management in rural areas.
The APACHE II score of this group of patients was not high, but this does not mean that their illness was not serious. Patient age, electrolyte disorders, and the infection index tended to be lower in SM patients. However, liver enzymes and the platelet index are not included in the APACHE II scoring system; therefore, we think that the routine use of the APACHE II score in the ICU does not reflect the severity of SM. Obstetric patients are a particularly unique cohort for physicians. These patients are young and otherwise healthy; their management is challenged by concerns for fetal viability, altered maternal physiology, and diseases specific to pregnancy (3). Young physicians are easily misled by a low APACHE II score and can underestimate the severity of the illness. As such, there is a need for another scoring system that is suited for a SM condition.
A cross-sectional study performed by the World Health Organization from May 1, 2010, to December 31, 2011, showed that 7.3% women had potentially life-threatening disorders and 1.0% developed a SM outcome (SMO; i.e., maternal death or maternal near miss). In addition, 26.7% of the women with an SMO had postpartum hemorrhage and 25.9% had preeclampsia or eclampsia; the cardiovascular, respiratory, and blood coagulation systems were the most frequent organ dysfunctions in women with an SMO (4). In the current study, PIH accounted for 43.5% (212/487) of the overall cases of SM, and postpartum hemorrhage accounted for 27.3% (133/487). It is worth noting that there was an increasing annual trend in placenta accreta, especially after the introduction of the population policy of two children for partial couples in 2014. We hypothesize that this is closely related to the abuse of cesarean section in over 40 years of the one-child policy in China.
Although nonobstetric disease was the second reason for admission to the ICU, it was too complex so that it needed more advanced means of monitoring and treatment. The patients with nonobstetric disease should be treated using an MDT mainly composed of ICU staff rather than obstetricians because of the limited experience of obstetricians. We also noticed that patients being admitted to the ICU because of diabetes and pancreatitis has increased in the last 4 years. In addition, most of the pancreatitis cases in this group were caused by hyperlipidemia, including women combined with both stillbirth and life-threatening ketoacidosis (5). Nutrition equilibrium and blood glucose monitoring during pregnancy should be considered.
There were 100 scar uterus cases in this group, of which 45 patients also experienced postpartum hemorrhage and some required a hysterectomy. We believe that the occurrence of scar uterus will increase after the 2016 policy of two children in China, which will increase the proportion of postpartum hemorrhage caused by placenta accreta and placenta previa. Although endocrine diseases were the fourth main reason for ICU admission among nonobstetric diseases, they were the leading cause of basic complications after scar uterus and led to a high risk of obstetric complications, especially in patients with hypothyroidism. Women with underlying indirect causes had a significantly increased risk of obstetric complications and SMO (6).
Nine patients died during the study period, of which we believe that the death of four patients could have been avoided. The first fatality was caused by PIH, when eclampsia occurred and a large amount of vomitus was drawn into the lung. The patient required CPR and died after 1 week. We think that the patient’s death could have been avoided if we had given her gastrointestinal decompression earlier. The fourth patient who died suffered a postpartum hemorrhage because of birth canal injury and subsequent cardiac arrest during transfer to the hospital. We think that her death was due to the obstetrician’s grassroots surgical technique and lack of experience in emergency hemorrhage rescue. The fifth fatality was a 16-year-old patient with pyonephrosis; she had sepsis shock and multiple organ dysfunction (MODS) because the surgeon did not remove the source of infection in a timely manner. The eighth fatality was acute fatty liver combined with MODS. Her family refused further treatment and insisted that she leave the hospital; she died after 2 days. To a certain extent, patients 5 and 8 died due to poor economic conditions. A systematic analysis of the global burden of disease in 2013 (7) showed that the accelerated decreases in maternal mortality coincided with the increased availability of assistance for the mother. It is important that the relief policies for SM are more widely and effectively disseminated and implemented.
Our unit carried out the clinical pathway on PIH since 2010, which improved medical quality (8). In our ICU, the number of SM cases has tended to increase annually. We think that the most important reason for this, in addition to the development of related disciplines and the change in population policy, it that ICU doctors gave obstetricians more cooperation and confidence for transferring SM cases to the ICU. Therefore, We call for an MDT mainly composed of ICU staff to reduce MMR.
ACKNOWLEDGMENT
We thank LetPub (www.letpub.com) for its linguistic assistance during the preparation of this article.
Footnotes
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Xi B, Zhou C, Zhang M, et al. Maternal and child mortality in China. Lancet 2014; 383:953–954. [DOI] [PubMed] [Google Scholar]
- 2.Knaus WA, Draper EA, Wagner DP, et al. APACHE II: A severity of disease classification system. Crit Care Med 1985; 13:818–829. [PubMed] [Google Scholar]
- 3.Ashraf N, Mishra SK, Kundra P, et al. Obstetric patients requiring intensive care: A one year retrospective study in a tertiary care institute in India. Anesthesiol Res Pract 2014; 2014:789450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Souza JP, Gulmezoglu AM, Vogel H, et al. Moving beyond essential interventions for reduction of maternal mortality (the WHO Multicountry Survey on Maternal and Newborn Health): A cross-sectional study. Lancet 2014; 381:1747–1755. [DOI] [PubMed] [Google Scholar]
- 5.Liu Y, Hong S, Xu H. Maternal acute necrotizing pancreatitis and fetal death associated with diabetic ketoacidosis. Pancreas 2016; 45:e9–e10. [DOI] [PubMed] [Google Scholar]
- 6.Lumbiganon P, Laopaiboon M, Intarut N, et al. ; WHO Multicountry Survey on Maternal and Newborn Health Research Network: Indirect causes of severe adverse maternal outcomes: A secondary analysis of the WHO Multicountry Survey on Maternal and Newborn Health. BJOG 2014; 121(Suppl 1):32–39. [DOI] [PubMed] [Google Scholar]
- 7.Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, et al. Global, regional, and national levels and causes of maternal mortality during 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014; 384:980–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu Y, Sun X, Hong S, et al. The application of perioperative clinical pathway for severe preeclampsia patients in ICU. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 2011; 23:313–315. [PubMed] [Google Scholar]


