Abstract
Objectives
Patients with asthma–chronic obstructive pulmonary disease (COPD) overlap syndrome (ACOS) and cardiovascular diseases (CVDs) share common risk factors. However, the association between ACOS and the incidence of CVDs has not been reported. This study investigated the relationship between CVDs and ACOS in the general population.
Setting
Data were obtained from Taiwan’s National Health Insurance Research Database for the period 2000 to 2010.
Participants
The ACOS cohort comprised patients (n=5814) who had received a diagnosis of asthma and COPD. The non-ACOS cohort comprised patients who had not received a diagnosis of asthma or COPD and were matched to the ACOS cohort (2:1) by age, sex and index date (n=11 625).
Primary and secondary outcome measures
The cumulative incidence of CVDs—coronary artery disease (CAD), cardiac dysrhythmia (CD) and heart failure (HF)—was calculated. Cox proportional regression analysis was employed to examine the relationship between ACOS and CVDs.
Results
After adjustment for multiple confounding factors—age, sex, comorbidities and medications—patients with ACOS were associated with a significantly higher risk of CVDs; the adjusted HRs (aHRs; 95% CI) for CAD, CD and HF were 1.62 (1.50 to 1.76), 1.44 (1.30 to 1.61) and 1.94 (1.73 to 2.19), respectively, whereas those of beta-blockers treatment for CAD, CD and HF were 1.19 (0.92 to 1.53), 0.90 (0.56 to 1.45) and 0.82 (0.49 to 1.38). The aHR of atenolol treatment for CD was 1.72 (1.01 to 2.93). The aHRs (95% CIs) of ACOS without acute exacerbation of COPD (AE-COPD) for CAD, CD and HF were 1.85 (1.70 to 2.01), 1.57 (1.40 to 1.77) and 2.07 (1.82 to 2.35), respectively.
Conclusion
ACOS was associated with higher CVD risk, even without the presence of previous comorbidities or AE-COPD. No significant differences in CVD events were observed in the ACOS cohort using beta-blockers, except for those using atenolol for treating CD.
Keywords: chronic obstructive pulmonary disease, asthma–chronic obstructive pulmonary disease overlap syndrome, cardiovascular diseases, cohort study
Strengths and limitations of this study.
The strength of this study is its use of population-based data to perform a longitudinal assessment of the risk of cardiovascular diseases in patients with asthma–chronic obstructive pulmonary disease overlap syndrome (ACOS).
The data are highly representative of the general population and minimised the likelihood of selection bias.
To avoid bias, only patients with a medication possession ratio of ≥80 were included in this analysis.
The causal relationships could not be established owing to the retrospective cohort study design.
Currently, there is no universally accepted definition of ACOS, which makes it difficult to clarify its epidemiology and pathophysiology.
Introduction
Asthma–chronic obstructive pulmonary disease (COPD) overlap syndrome (ACOS)1 2 is a newly recognised, systemic inflammatory disease3 4 that shares the characteristics of asthma and COPD.5 6 ACOS is a form of airway and pulmonary vessel disease7 8 that is associated with a disproportionate number of exacerbations and a higher overall healthcare burden9 than either asthma or COPD alone.
Cardiovascular diseases (CVDs), includes coronary artery disease (CAD), cardiac dysrhythmia (CD) and heart failure (HF). Respiratory failure in an acute exacerbation of COPD (AE-COPD) may contribute to hypoxaemia and hypercapnia.10 These complications are associated with atherosclerosis11 and CVDs.12 Therefore, the incidence of HF increases with an increase in the incidence of CD. In addition, the use of a bronchodilator is associated with CAD and HF.13 CD and CAD are predisposing factors of sudden death. Previous studies suggest a beneficial effect of beta-blockers on AE in mild to moderate COPD.14 15 However, benefits are less obvious in severe COPD and coexistent CVDs.15 The role of beta-blockers14 (eg, β1-adrenoceptor blockers) in AE-COPD with CAD, CD and HF, such as in elderly with severe cases,15 is still being debated.16 17
Patients with ACOS have higher frequency of hospital admission and bronchodilator use18; therefore, ACOS may also be associated with5 CVDs.19 However, the relationship between ACOS and the risk of CVDs in the general population has not been reported in detail.
Beta-blockers (eg, β1-adrenoceptor blockers) may have an anti-inflammatory effect in patients with COPD and protect16 their cardiovascular system.20 Additionally, beta-blockers may play a role in patients with ACOS and coexistent CVDs.5 14 Therefore, we conducted this nationwide population-based cohort study to investigate the relationship between ACOS and CVDs including CAD, CD and HF. In addition, we evaluated the role of beta-blockers in the relationship of patients with ACOS which has not been examined in any previous study.
Materials and methods
Data source
This retrospective study used data from the Longitudinal Health Insurance Database 2000 (LHID2000), a subset of the National Health Insurance Research Database (NHIRD). The LHID2000 includes the data of 1 000 000 patients randomly sampled from all the enrollees of the National Health Insurance (NHI) programme in Taiwan from 1996 to 2000, with follow-up data collected until 2011.21 Studies have detailed the specifications of the NHI programme and the LHID2000.22 Diseases were defined according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes.
Ethics statement
The NHIRD encrypts patients’ personal information to protect their privacy and provides researchers with anonymous identification numbers associated with relevant claims information, including sex, date of birth, medical services received and prescriptions. Therefore, patient consent is not required to access the NHIRD.
Sampled participants
The ACOS cohort included patients aged ≥40 years who had received a diagnosis of COPD (ICD-9-CM codes 491, 492 and 496) between 1 January 2000 and 31 December 2010. The index date was defined as the date when asthma23 was first diagnosed.7 24 We excluded patients who had a history of CAD (ICD-9-CM codes 410–414), CD (ICD-9-CM code 427) and HF (ICD-9-CM code 428) before the index date or were younger than 40 years. For each patient in the ACOS cohort, two patients without ACOS were randomly selected for the same period (2000–2010) by using the same exclusion criteria as those applied to the ACOS cohort. This non-ACOS cohort was matched (2:1) to the ACOS cohort by sex, age (every 5-year span) and index year. Diagnosis of COPD is based on clinical symptoms or signs and pulmonary function test (PFT) results according to the strict policy of bronchodilator use2 in Taiwan. If a physician (eg, a local medical doctor) does not record clinical symptoms or signs and performed a PFT, the physician does not receive the application fee. In the study by Cheng et al, patients with COPD underwent chest X-ray (84.7%), PFT (58.4%) and CT (39.4%) in a hospital; the results of those examinations support the diagnosis of COPD in the NHIRD.25 The non-ACOS26 cohort included patients without either asthma or COPD.27
Outcomes and relevant variables
The major outcomes were a new diagnosis of CAD (ICD-9-CM codes 410–414), CD (ICD-9-CM code 427) or HF (ICD-9-CM code 428). All study patients were followed until they received a diagnosis of a major outcome, they withdrew from the NHI programme or 31 December 2011, whichever occurred first. Comorbidities potentially related to the major outcomes include diabetes (ICD-9-CM code 250), hypertension (ICD-9-CM codes 401–405), hyperlipidaemia (ICD-9-CM code 272), hyperuricaemia (ICD-9-CM code 790.6), end-stage renal disease (ICD-9-CM code 585), bone fracture (ICD-9-CM codes 800–829), pneumonia (ICD-9-CM codes 480–486), mental disorders (ICD-9-CM codes 290–319), stroke (ICD-9-CM codes 430–438) and tobacco dependency (ICD-9-CM code 305.1). Medications possibly associated with the major outcomes were also evaluated, including bisoprolol, atenolol, metoprolol and beta-blockers (only patients with a medication possession ratio (MPR) of ≥80 were included in this analysis). Severe COPD with acute exacerbation was defined as AE-COPD (ICD-9-CM codes 491.21, 491.22, 492.8, 518.81, 518.82 and 518.84).
Statistical analysis
The demographic factors, comorbidities and medications of the ACOS and non-ACOS cohorts were compared using the χ2 test for categorical variables and Student’s t-test for continuous variables. To estimate the risk of the major outcomes, incidence density rates were calculated for both cohorts as the number of major outcome events divided by the sum of the whole follow-up period in years (per 1000 person-years). The cumulative incidence curves of the major outcomes were assessed using the Kaplan-Meier method, and the differences in tested curves were analysed using the log-rank test. Univariate and multivariate Cox proportional hazard regression models were used to examine the effect of the ACOS cohort in the risks of the major outcomes, which were reported as HRs with 95% CIs. Variables with significant differences in the univariate Cox model were included in the multivariate model. The significance level was set at p<0.05. Data analysis was performed using SAS software, V.9.4 (SAS Institute).
Results
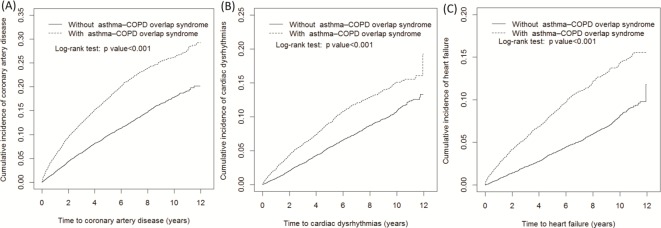
We enrolled 5814 and 11 625 patients in the ACOS and non-ACOS cohorts, respectively. In the ACOS cohort, 58.5% and 46.8% of patients were men and were aged ≥65 years, respectively (table 1). The mean age was 63.8±12.2 and 63.3±12.2 years in the ACOS and non-ACOS cohorts, respectively. Compared with the non-ACOS cohort, the ACOS cohort tended to have hypertension, hyperlipidaemia, hyperuricaemia, bone fracture, pneumonia, mental disorders, stroke and tobacco dependency. In addition, fewer patients in the ACOS cohort used atenolol than in the non-ACOS cohort (0.84% vs 1.18%). The cumulative incidence rates of CAD, CD and HF were higher in the ACOS cohort than in the non-ACOS cohort (figure 1). The overall incidence density rate of CAD was 35.2 and 20.0 per 1000 person-years in the ACOS and non-ACOS cohorts, respectively (table 2). The corresponding adjusted HR (aHR) of CAD was 1.62 (95% CI 1.50 to 1.76) after adjustment for age; sex; comorbidities, namely diabetes, hypertension, hyperlipidaemia, pneumonia, mental disorders and stroke and the use of bisoprolol, atenolol, metoprolol or beta-blockers. The sex-specific ACOS-to-non-ACOS cohort relative risk of CAD was significant in both women (aHR=1.51; 95% CI 1.32 to 1.73) and men (aHR=1.68; 95% CI 1.52 to 1.86). The age-specific ACOS-to-non-ACOS cohort relative risk of CAD was higher for those aged 40–49 years (aHR=1.58; 95% CI 1.17 to 2.13), those aged 50–64 years (aHR=1.67; 95% CI 1.45 to 1.92) and those aged ≥65 years (aHR=1.57; 95% CI 1.42 to 1.75). Patients without comorbidities in the ACOS cohort were associated with a significantly higher risk of CAD (aHR=1.82; 95% CI 1.52 to 2.18), CD (aHR=1.80; 95% CI 1.45 to 2.23) and HF (aHR=2.31; 95% CI 1.77 to 3.02) than those in the non-ACOS cohort. We compared the risk of CAD, CD and HF in the two cohorts with regard to the variables of sex, age and the presence of comorbidities. The risk of CAD, CD and HF was higher in the ACOS cohort than in the non-ACOS cohort, except for those aged 40–49 years, who were not associated with a significantly higher risk of CD.
Table 1.
Demographics and comorbidities of the ACOS and non-ACOS cohorts
| Variable | ACOS | p Value | |||
| No (n=11 625) | Yes (n=5814) | ||||
| n | % | n | % | ||
| Sex | 0.99 | ||||
| Female | 4828 | 41.5 | 2414 | 41.5 | |
| Male | 6797 | 58.5 | 3400 | 58.5 | |
| Age, years | 0.99 | ||||
| 40–49 | 1950 | 16.8 | 975 | 16.8 | |
| 50–64 | 4242 | 36.5 | 2121 | 36.5 | |
| ≥65 | 5433 | 46.7 | 2718 | 46.8 | |
| Mean (SD)* | 63.3 | 12.2 | 63.8 | 12.2 | 0.55 |
| Comorbidity | |||||
| Diabetes | 1449 | 12.5 | 774 | 13.3 | 0.11 |
| Hypertension | 4221 | 36.3 | 2799 | 48.1 | <0.001 |
| Hyperlipidaemia | 2169 | 18.7 | 1418 | 24.4 | <0.001 |
| Hyperuricaemia | 176 | 1.51 | 140 | 2.41 | <0.001 |
| End-stage renal disease | 25 | 0.22 | 6. | 0.10 | 0.10 |
| Bone fractures | 1243 | 10.7 | 794 | 13.7 | <0.001 |
| Pneumonia | 494 | 4.25 | 1045 | 18.0 | <0.001 |
| Mental disorders | 2960 | 25.5 | 2435 | 41.9 | <0.001 |
| Stroke | 476 | 4.09 | 362 | 6.23 | <0.001 |
| Tobacco dependency | 54 | 0.46 | 76 | 1.31 | <0.001 |
| Medicine | |||||
| Bisoprolol | 44 | 0.38 | 26 | 0.45 | 0.50 |
| Atenolol | 137 | 1.18 | 49 | 0.84 | 0.04 |
| Metoprolol | 7 | 0.06 | 3 | 0.05 | 0.82 |
| Beta-blockers | 217 | 1.87 | 89 | 1.53 | 0.11 |
χ2 test.
*Student’s t-test.
ACOS, asthma–chronic obstructive pulmonary disease overlap syndrome.
Figure 1.
Cumulative incidence of coronary artery disease (A), cardiac dysrhythmia (B) and heart failure (C) of patients with and without critical illness, as determined using propensity score matching. COPD, chronic obstructive pulmonary disease.
Table 2.
Incidence rates and adjusted HRs of coronary artery disease, cardiac dysrhythmia and heart failure in the ACOS and non-ACOS cohorts after stratification by sex, age, comorbidities (no/yes) and medications (no/yes)
| Variables | ACOS | Compared with non-ACOS cohort | ||||||
| No | Yes | |||||||
| Event | PY | Rate | Event | PY | Rate | Crude HR (95% CI) | Adjusted HR†(95% CI) | |
| Coronary artery disease | ||||||||
| Overall | 1450 | 72 458 | 20.0 | 1147 | 32 580 | 35.2 | 1.74 (1.61 to 1.88)*** |
1.62 (1.50 to 1.76)*** |
| Sex | ||||||||
| Female | 519 | 31 337 | 16.6 | 416 | 14 337 | 29.0 | 1.73 (1.52 to 1.97)*** | 1.51 (1.32 to 1.73)*** |
| Male | 931 | 41 122 | 22.6 | 731 | 18 243 | 40.1 | 1.76 (1.59 to 1.94)*** | 1.68 (1.52 to 1.86)*** |
| Age, years | ||||||||
| 40–49 | 98 | 13 957 | 7.02 | 97 | 6720 | 14.4 | 2.05 (1.55 to 2.71)*** | 1.58 (1.17 to 2.13)** |
| 50–64 | 461 | 27 863 | 16.6 | 405 | 12 667 | 32.0 | 1.92 (1.68 to 2.19)*** | 1.67 (1.45 to 1.92)*** |
| ≥65 | 891 | 30 639 | 29.1 | 645 | 13 192 | 48.9 | 1.66 (1.50 to 1.84)*** | 1.57 (1.42 to 1.75)*** |
| Comorbidity‡ | ||||||||
| No | 382 | 32 438 | 11.8 | 166 | 7923 | 21.0 | 1.78 (1.48 to 2.14)*** | 1.82 (1.52 to 2.18)*** |
| Yes | 1068 | 40 021 | 26.7 | 981 | 24 656 | 39.8 | 1.48 (1.36 to 1.62)*** | 1.56 (1.43 to 1.70)*** |
| Cardiac dysrhythmia | ||||||||
| Overall | 862 | 75 887 | 11.4 | 622 | 35 785 | 17.4 | 1.53 (1.38 to 1.69)*** | 1.44 (1.30 to 1.61)*** |
| Sex | ||||||||
| Female | 313 | 32 716 | 9.57 | 221 | 15 643 | 14.1 | 1.48 (1.24 to 1.75)*** | 1.42 (1.19 to 1.71)*** |
| Male | 549 | 43 171 | 12.7 | 401 | 20 141 | 19.9 | 1.56 (1.37 to 1.78)*** | 1.46 (1.28 to 1.67)*** |
| Age, years | ||||||||
| 40–49 | 62 | 14 149 | 4.38 | 47 | 7001 | 6.71 | 1.54 (1.05 to 2.24)* |
1.32 (0.88 to 1.98) |
| 50–64 | 218 | 29 249 | 7.45 | 164 | 14 117 | 11.6 | 1.56 (1.27 to 1.91)*** | 1.33 (1.07 to 1.65)** |
| ≥65 | 582 | 32 489 | 17.9 | 411 | 14 667 | 28.0 | 1.56 (1.38 to 1.77)*** | 1.46 (1.28 to 1.67)*** |
| Comorbidity‡ | ||||||||
| No | 274 | 33 057 | 8.29 | 117 | 8255 | 14.2 | 1.71 (1.38 to 2.13)*** | 1.80 (1.45 to 2.23)*** |
| Yes | 588 | 42 830 | 13.7 | 505 | 27 530 | 18.3 | 1.33 (1.19 to 1.50)*** | 1.44 (1.28 to 1.63)*** |
| Heart failure | ||||||||
| Overall | 616 | 77 072 | 7.99 | 588 | 36 054 | 16.3 | 2.04 (1.82 to 2.28)*** | 1.94 (1.73 to 2.19)*** |
| Sex | ||||||||
| Female | 251 | 33 058 | 7.59 | 217 | 15 708 | 13.8 | 1.81 (1.51 to 2.17)*** | 1.60 (1.32 to 1.94)*** |
| Male | 365 | 44 014 | 8.29 | 371 | 20 345 | 18.2 | 2.20 (1.90 to 2.54)*** | 2.17 (1.87 to 2.52)*** |
| Age, years | ||||||||
| 40–49 | 19 | 14 379 | 1.32 | 24 | 7110 | 3.38 | 2.56 (1.41 to 4.68)** | 2.17 (1.15 to 4.11)* |
| 50–64 | 136 | 29 493 | 4.61 | 148 | 14 255 | 10.4 | 2.24 (1.78 to 2.83)*** | 1.92 (1.50 to 2.45)*** |
| ≥65 | 461 | 33 200 | 13.9 | 416 | 14 688 | 28.3 | 2.04 (1.79 to 2.33)*** | 1.86 (1.62 to 2.13)*** |
| Comorbidity‡ | ||||||||
| No | 154 | 33 673 | 4.57 | 83 | 8430 | 9.85 | 2.16 (1.66 to 2.82)*** | 2.31 (1.77 to 3.02)*** |
| Yes | 462 | 43 399 | 10.7 | 505 | 27 623 | 18.3 | 1.71 (1.51 to 1.94)*** | 1.91 (1.69 to 2.17)*** |
Rate denotes incidence rate (per 1000 person-years) and Crude HR denotes relative HR.
*p<0.05, **p<0.01, ***p<0.001.
†Covariables found to be significantly associated with coronary artery disease, cardiac dysrhythmia and heart failure in the univariate Cox proportional regression model were further analysed using a multivariate Cox proportional regression model.
‡Individuals with diabetes, hypertension, hyperlipidaemia, hyperuricaemia, end-stage renal disease, bone fracture, pneumonia, mental disorders, stroke and tobacco dependency were classified in the comorbidity group.
ACOS, asthma–chronic obstructive pulmonary disease overlap syndrome; PY, person-years.
The results of the univariate and multivariate Cox proportional hazards regression models used to analyse the contribution of age, sex, comorbidities and medications to the three outcome events are listed in table 3. The risk of CAD, CD and HF increased with age, and men had a higher risk of CAD and CD than did women. Diabetes was associated with a higher risk of CAD and HF, and hypertension was associated with a higher risk of CAD, CD and HF. Patients with hyperlipidaemia had a higher risk of CAD. Pneumonia was associated with a higher risk of CD and HF, whereas patients with mental disorders had a higher risk of CAD. Patients with stroke had a higher risk of HF. In the ACOS cohort, patients who received atenolol treatment were associated with a higher risk of CD (aHR=1.72; 95% CI 1.01 to 2.93). The aHRs (95% CIs) of beta-blocker treatment for CAD, CD and HF were 1.19 (0.92 to 1.53), 0.90 (0.56 to 1.45) and 0.82 (0.49 to 1.38), respectively.
Table 3.
Crude and adjusted HRs of coronary artery disease, cardiac dysrhythmia and heart failure in association with ACOS cohort, sex, age, comorbidities and medications in Cox regression models
| Variable | Coronary artery disease | Cardiac dysrhythmia | Heart failure | |||
| Crude HR (95% CI) | Adjusted HR† (95% CI) | Crude HR (95% CI) | Adjusted HR† (95% CI) | Crude HR (95% CI) | Adjusted HR† (95% CI) | |
| ACOS | 1.74 (1.61 to 1.88)*** | 1.62 (1.50 to 1.76)*** | 1.53 (1.38 to 1.69)*** | 1.44 (1.30 to 1.61)*** | 2.04 (1.82 to 2.28)*** | 1.94 (1.73 to 2.19)*** |
| Age, years (per year increase) | 1.03 (1.03 to 1.04)*** | 1.03 (1.02 to 1.03)*** | 1.05 (1.05 to 1.06)*** | 1.05 (1.04 to 1.05)*** | 1.07 (1.07 to 1.08)*** | 1.07 (1.06 to 1.07)*** |
| Sex (women vs men) | 1.36 (1.25 to 1.47)*** | 1.31 (1.21 to 1.42)*** | 1.36 (1.22 to 1.51)*** | 1.20 (1.08 to 1.34)** | 1.19 (1.06 to 1.34)** | 1.00 (0.89 to 1.12) |
| Comorbidity | ||||||
| Diabetes | 1.69 (1.53 to 1.86)*** | 1.23 (1.10 to 1.37)*** | 1.08 (0.92 to 1.25) | – | 1.73 (1.50 to 2.01)*** | 1.24 (1.07 to 1.44)** |
| Hypertension | 2.40 (2.22 to 2.59)*** | 1.77 (1.63 to 1.93)*** | 1.82 (1.65 to 2.02)*** | 1.26 (1.13 to 1.41)*** | 2.68 (2.39 to 3.01)*** | 1.59 (1.40 to 1. 80)*** |
| Hyperlipidaemia | 1.49 (1.37 to 1.63)*** | 1.15 (1.05 to 1.26)** | 1.06 (0.93 to 1.20) | – | 1.08 (0.94 to 1.24) | – |
| Hyperuricaemia | 1.40 (1.07 to 1.83)* | 0.93 (0.71 to 1.22) | 1.00 (0.66 to 1.51) | – | 1.62 (1.12 to 2.34)* | 0.99 (0.68 to 1.44) |
| End-stage renal disease | 1.56 (1.65 to 3.73) | – | 2.33 (0.88 to 6.20) | – | 0.70 (0.10 to 4.97) | – |
| Bone fractures | 1.13 (1.00 to 1.27) | – | 1.32 (1.14 to 1.54)*** | 1.09 (0.94 to 1.28) | 1.43 (1.21 to 1.68)*** | 1.07 (0.90 to 1. 26) |
| Pneumonia | 1.44 (1.26 to 1.64)*** | 0.99 (0.87 to 1.14) | 1.90 (1.63 to 2.23)*** | 1.34 (1.13 to 1.57)*** | 2.19 (1.85 to 2.58)*** | 1.28 (1.07 to 1.52)** |
| Mental disorders | 1.39 (1.28 to 1.50)*** | 1.14 (1.05 to 1.24)** | 1.25 (1.13 to 1.40)*** | 1.09 (0.97 to 1.21) | 1.27 (1.12 to 1.42)*** | 0.95 (0.84 to 1.08) |
| Stroke | 1.59 (1.35 to 1.89)*** | 0.93 (0.79 to 1.11) | 1.65 (1.32 to 2.05)*** | 1.00 (0.80 to 1.26) | 2.52 (2.05 to 3.09)*** | 1.26 (1.02 to 1.56)* |
| Tobacco dependency | 0.87 (0.48 to 1.57) | – | 0.74 (0.31 to 1.79) | – | 0.96 (0.40 to 2.31) | – |
| Medicine | ||||||
| Bisoprolol | 1.77 (1.00 to 3.12)* | 0.99 (0.54 to 1.79) | 1.25 (0.52 to 3.00) | – | 1.62 (0.67 to 3.91) | – |
| Atenolol | 1.21 (0.17 to 8.61) | – | 1.86 (1.27 to 2.73)** | 1.72 (1.01 to 2.93)* | 2.02 (1.35 to 3.03)*** | 1.73 (0.97 to 3.08) |
| Metoprolol | 1.21 (0.17 to 8.61) | – | 4.13 (1.03 to 16.5)* | 3.01 (0.70 to 13.0) | 2.31 (0.33 to 16.4) | – |
| Beta-blockers | 1.94 (1.45 to 2.59)*** | 1.19 (0.92 to 1.53) | 1.53 (1.10 to 2.13)* | 0.90 (0.56 to 1.45) | 1.58 (1.10 to 2.28)* | 0.82 (0.49 to 1.38) |
Crude HR denotes relative HR.
*p<0.05, **p<0.01, ***p<0.001.
†Covariables found to be significantly associated with coronary artery disease, cardiac dysrhythmia and heart failure in the univariate Cox proportional regression model were further analysed using the multivariate Cox proportional regression model.
ACOS, asthma–chronic obstructive pulmonary disease overlap syndrome.
In the ACOS cohort, the aHRs (95% CIs) of patients without AE-COPD for CAD, CD and HF were 1.85 (1.70 to 2.01), 1.57 (1.40 to 1.77) and 2.07 (1.82 to 2.35), respectively (table 4). In the ACOS cohort, patients without AE-COPD were associated with a higher risk of CVDs. Meanwhile, the aHR (95% CI) of patients with AE-COPD for HF was 1.64 (1.36 to 1.97) in the ACOS cohort. The patients with AE-COPD were associated with a higher risk of HF in the ACOS cohort.
Table 4.
Incidences and HRs of coronary artery disease, cardiac dysrhythmia and heart failure in the ACOS cohort stratified by AE-COPD
| Variable | N | Event | PY | Rate | Crude HR (95% CI) |
Adjusted HR† (95% CI) |
| Coronary artery disease | ||||||
| Non-ACOS | 11 625 | 1450 | 72 458 | 20.0 | 1 (reference) | 1 (reference) |
| All ACOS | ||||||
| Without AE-COPD | 4373 | 934 | 24 507 | 38.1 | 1.89 (1.74 to 2.05)*** | 1.85 (1.70 to 2.01)*** |
| With AE-COPD | 1441 | 213 | 8073 | 26.4 | 1.31 (1.13 to 1.51)*** | 1.05 (0.90 to 1.21) |
| Cardiac dysrhythmia | ||||||
| Non-ACOS | 11 625 | 862 | 75 887 | 11.4 | 1 (reference) | 1 (reference) |
| All ACOS | ||||||
| Without AE-COPD | 4373 | 482 | 27 336 | 17.6 | 1.55 (1.39 to 1.73)*** | 1.57 (1.40 to 1.77)*** |
| With AE-COPD | 1441 | 140 | 8448 | 16.6 | 1.45 (1.22 to 1.74)*** | 1.11 (0.93 to 1.34) |
| Heart failure | ||||||
| Non-ACOS | 11 625 | 616 | 77 072 | 7.99 | 1 (reference) | 1 (reference) |
| All ACOS | ||||||
| Without AE-COPD | 4373 | 438 | 27 636 | 15.9 | 1.98 (1.75 to 2.24)*** | 2.07 (1.82 to 2.35)*** |
| With AE-COPD | 1441 | 150 | 8418 | 17.8 | 2.22 (1.86 to 2.65)*** | 1.64 (1.36 to 1.97)*** |
Rate denotes incidence rate (per 1000 person-years) and Crude HR denotes relative HR.
*p<0.05, **p<0.01, ***p<0.001.
†Covariables found to be significantly associated with coronary artery disease, cardiac dysrhythmia and heart failure in the univariate Cox proportional regression model were further analysed using a multivariate Cox proportional regression model.
ACOS, asthma–chronic obstructive pulmonary disease overlap syndrome; AE-COPD, acute exacerbation of chronic obstructive pulmonary disease; PY, person-years.
Discussion
In this study, the ACOS cohort had more comorbidities and a higher risk of CVDs than did the non-ACOS cohort (aHRs for CAD, CD and HF=1.62, 1.44 and 1.94, respectively; all p<0.001). These findings are consistent with those of a retrospective cohort study conducted by van Boven et al, who reported a strong association of CVDs with hospitalisation for ACOS,28 and those of a study conducted by Hekking et al, who discovered that prescriptions for CVDs were the most prevalent in patients with ACOS.29 We also found that even patients without comorbidities in the ACOS cohort were associated with a significantly higher risk of CVDs during the follow-up period (aHRs for CAD, CD and HF=1.82, 1.80 and 2.31, respectively; all p<0.001).
Inflammation is systemic in COPD, and this contributes to the development of various crucial comorbidities.30 Strong associative evidence3–5 11 31–33 confirmed that inflammatory cells or mediators in COPD are relevant to the development of CVDs. The exact mechanism underlying the association between ACOS and CVDs is unclear; however, it may be partially explained by systemic inflammation in both patients with ACOS and those with CVDs. Gao et al26 reported that the levels of inflammatory markers in the sputum and serum were higher in patients with ACOS than in healthy controls, those with only asthma and those with only COPD.3 From a biological viewpoint, several studies have reported an association between increased levels of inflammatory markers (eg, cytokine) and an increased risk of CVDs, including CAD,31 CD32 and HF.33 Taken together, these findings may support the association with CVDs34 of systemic pulmonary vessel35 (eg, the pulmonary artery7) and airway inflammation3 accompanied by hypoxaemia36 and atherosclerosis12 of the vessel11 in ACOS,7 as observed in younger adults in the present study (age ≥40 to <65 years; p<0.05 for CAD, CD and HF, except for CD (age 40–49 years, p>0.05)). Meanwhile, patients without AE-COPD who were in the ACOS cohort (aHRs for CAD, CD and HF=1.85, 1.57 and 2.07, respectively; all p<0.05) were still associated with the risk of CVDs; this result is consistent with that of a previous study.37
Comorbidities, such as atherosclerosis-related diseases12 (eg, diabetes, hypertension and hyperlipidaemia; all p<0.05) and hypoxaemia-related diseases27 (eg, pneumonia; p<0.05), were associated with the risk of CVDs (eg, CAD7) in the current study; this finding is also consistent with those of previous studies.7 11 12
Beta-blockers (eg, selective β1-adrenoceptor blockers) have nearly the same anti-inflammatory effect on inflammatory processes.17 Beta-blockers have antioxidant properties,38 and they are used to treat CAD,39 HF40 and CD. Atenolol,41 metoprolol42 and bisoprolol43 treatments have been reported to exert a cardioprotective effect in patients with CVDs. No significant differences were observed in CVD events in patients who received β1-adrenoceptor blockers between the ACOS and non-ACOS cohorts (bisoprolol for CAD, aHR=0.99; metoprolol for CD, aHR=3.01; atenolol for HF, aHR=1.73; all p>0.05), which is different from the cardioprotective effect of COPD observed in a previous study.39 This result may be attributable to higher systemic,3 26 airway8 34 and pulmonary vessel inflammation3 34 in the ACOS cohort than in the COPD cohort and a higher frequency of AE-COPD,7 27 44 which aggravates these inflammatory conditions. The higher incidence of HF (aHR=1.64; p<0.05) identified in the ACOS cohort with AE-COPD supports this speculation. This may explain the reason for no significant differences in CVD events in patients who received beta-blockers between the ACOS and non-ACOS cohorts (aHRs for CAD, CD and HF=1.19, 0.90 and 0.82, respectively; all p>0.05). In the ACOS cohort, patients who used selective β1-adrenoceptor blockers (eg, atenolol) still had a higher risk of CD (aHR=1.72; p<0.05) than the non-ACOS cohort. These results warrant more studies to elucidate the exact mechanisms underlying the associations among beta-blocker use, ACOS and CVDs.
The frequency of AE-COPD in the ACOS cohort compared with that in the non-ACOS cohort (eg, patients with only COPD, patients with only asthma and patients without asthma or COPD) that was determined in our study is different from those reported in previous studies.1 2 24 In our previous study,7 the frequency of AE-COPD was higher in the ACOS cohort than in the non-ACOS cohort (patients without asthma or COPD). The results of this study revealed that the frequency of CAD and CD events did not differ between the ACOS cohort with a higher frequency of AE-COPD and the non-ACOS cohort (aHRs for CAD and CD=1.05 and 1.11, respectively; all p>0.05). One possible explanation is that the ACOS cohort with AE-COPD had a higher frequency of hospitalisation and intensive care (oxygen provision, chest care and increased dosage of bronchodilators/inhaler corticosteroids or oral corticosteroids and use of antibiotics),24 45 46 which may have reduced the number of hypoxaemia or hypercapnia events. This strategy may have counterbalanced2 the risk of CAD and CD in the ACOS cohort with AE-COPD.1 Studies conducted in Korea1 and Japan47 have reported that the lung function of patients with ACOS may be recovered by medication. Meanwhile, the ACOS cohort appeared to be more responsive to bronchodilators34 and inhaled corticosteroids48 compared with the COPD-only cohort; this finding supports the results of our study. However, the risk of HF in the ACOS cohort with AE-COPD was still higher (aHR=1.64; p<0.05)49 than that in the non-ACOS cohort. In Chung et al’s study,44 the frequency of AE-COPD in the ACOS cohort (aHR=2.58; p<0.05) was higher than that in the COPD-only cohort. The risk of HF (aHR=1.26; p<0.05) was higher in the ACOS cohort than in the COPD cohort. These findings are consistent with those of the current study. Additional randomised controlled trials should be conducted to confirm different findings in different cohorts (eg, ACOS- and COPD-only cohorts) and our speculations.
The results of this study imply that ACOS itself is associated with the risk of CVDs, even without the presence of previous comorbidities or AE-COPD. In addition, beta-blockers may play a role in CVD development. The results of this study indicate that physicians should be alert to detect ACOS early in adults aged ≥40 years. Thus, quitting smoking, chest care and regular follow-ups under a multidisciplinary team may be beneficial for preventing the complications of ACOS.
The strength of this study was its use of population-based data to perform a longitudinal assessment of the risk of CVDs in patients with ACOS. The data used is highly representative of the general population and minimised the likelihood of selection bias. The Global Initiative for Asthma and the Global Initiative for Chronic Obstructive Lung Disease Committees jointly created the term ACOS to acknowledge the daily reality of patients who have features of both asthma and COPD. In the present study, we defined patients with ACOS as those with concurrent, physician-diagnosed COPD and asthma. This definition is similar to the diagnostic criteria used in other recent studies.11 13 23 24 27 In addition, we also considered lifestyle (eg, tobacco dependency) and the effects of medications (eg, beta-blockers). To avoid bias, only patients with an MPR of ≥80 were included in this analysis. Furthermore, the ACOS cohort was derived from patients with COPD who had received a PFT. Owing to the diagnosis of the COPD, we monitored the benefits of the inhaler and prescribed the long-term inhaler largely based on the PFT in Taiwan.27 50 For example, grading of severity of airflow limitation in COPD based on postbronchodilator forced expiratory volume in 1 s.28–30 Tobacco dependency and COPD-related diseases24 27 (diabetes, hypertension, hyperlipidaemia, hyperuricaemia, end-stage renal disease, bone fracture, pneumonia, mental disorders and stroke) were included in the analysis. The programme of continuity of care for patients with COPD in Taiwan is well-established, and the related medical policy may have avoided confounding factors in this study.
Limitations
No universally accepted definition of ACOS currently exists, which makes it difficult to clarify its epidemiology and pathophysiology. The definition and factors for classifying a patient as having ACOS differ between studies. In this study, we defined ACOS according to the presence of both asthma and COPD based on ICD-9-CM codes. This was probably the most substantial limitation of this study. However, the ACOS cohort was derived from COPD groups23 aged ≥40 years, as it was in studies conducted in Japan2 and Korea,1 9 and was based on ICD-9-CM codes used in a study recently conducted in the USA.24 The Non-Interventional Study of COPD Patients with Asthma Overlap Syndrome in Vietnam and Taiwan (ClinicalTrials.gov identifier: NCT02878252) may address this point in the near future. Finally, data on cytokines were not available in this study. Bias resulting from unknown confounders may have affected our results.
Conclusion
ACOS was associated with the risk of CVDs, even without the previous presence of comorbidities or AE-COPD. No significant differences in CVD events were observed in patients who used beta-blockers in the ACOS cohort, except for those who used atenolol to treat CD.
Supplementary Material
Footnotes
J-JY and W-HH contributed equally.
Contributors: Conceptualisation: J-JY and W-HH. Methodology: C-LL, W-HH and J-JY. Software: C-LL and W-HH. Validation: J-JY, Y-FW, C-LL and W-HH. Formal analysis: J-JY, Y-FW, C-LL and W-HH. Investigation: J-JY and W-HH. Resources: J-JY and W-HH. Data curation: J-JY, Y-FW, C-LL and W-HH. Writing (original draft preparation): J-JY, Y-FW, C-LL and W-HH. Writing (review and editing): J-JY, Y-FW, C-LL and W-HH. Visualisation: J-JY, Y-FW, C-LL and W-HH. Supervision: W-HH and J-JY. Project administration: W-HH and J-JY. Funding acquisition: W-HH.
Funding: This study is supported in part by Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW106-TDU-B-212-113004), China Medical University Hospital, Academia Sinica Taiwan Biobank Stroke Biosignature Project (BM10601010036), Taiwan Clinical Trial Consortium for Stroke (MOST 106-2321-B-039-005), Tseng-Lien Lin Foundation, Taichung, Taiwan, Taiwan Brain Disease Foundation, Taipei, Taiwan and Katsuzo and Kiyo Aoshima Memorial Funds, Japan. No additional external funding was received for this study.
Disclaimer: The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Competing interests: None declared.
Ethics approval: This study was approved as fulfilling the exemption condition by the Institutional Review Board (IRB) of China Medical University Hospital. The IRB number is CMUH104-REC2-115-CR2. The IRB also specifically waived the consent requirement.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The dataset used in this study is held by the Taiwan Ministry of Health and Welfare. All relevant data are provided in the paper.
References
- 1.Park HJ, Byun MK, Kim HJ, et al. . Asthma-COPD overlap shows favorable clinical outcomes compared to pure COPD in a Korean COPD cohort. Allergy Asthma Immunol Res 2017;9:431–7. 10.4168/aair.2017.9.5.431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tochino Y, Asai K, Shuto T, et al. . Asthma-COPD overlap syndrome—coexistence of chronic obstructive pulmonary disease and asthma in elderly patients and parameters for their differentiation. J Gen Fam Med 2017;18:5–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iwamoto H, Gao J, Koskela J, et al. . Differences in plasma and sputum biomarkers between COPD and COPD-asthma overlap. Eur Respir J 2014;43:421–9. 10.1183/09031936.00024313 [DOI] [PubMed] [Google Scholar]
- 4.Fu JJ, McDonald VM, Gibson PG, et al. . Systemic inflammation in older adults with asthma-COPD overlap syndrome. Allergy Asthma Immunol Res 2014;6:316–24. 10.4168/aair.2014.6.4.316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Magnussen H, Watz H. Systemic inflammation in chronic obstructive pulmonary disease and asthma: relation with comorbidities. Proc Am Thorac Soc 2009;6:648–51. 10.1513/pats.200906-053DP [DOI] [PubMed] [Google Scholar]
- 6.Ding B, Enstone A. Asthma and chronic obstructive pulmonary disease overlap syndrome (ACOS): structured literature review and physician insights. Expert Rev Respir Med 2016;10:363–71. 10.1586/17476348.2016.1144476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yeh JJ, Wang YC, Kao CH. Asthma-chronic obstructive pulmonary disease overlap syndrome associated with risk of pulmonary embolism. PLoS One 2016;11:e0162483 10.1371/journal.pone.0162483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Takayanagi S, Kawata N, Tada Y, et al. . Longitudinal changes in structural abnormalities using MDCT in COPD: do the CT measurements of airway wall thickness and small pulmonary vessels change in parallel with emphysematous progression? Int J Chron Obstruct Pulmon Dis 2017;12:551–60. 10.2147/COPD.S121405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim J, Kim YS, Kim K, et al. . Socioeconomic impact of asthma, chronic obstructive pulmonary disease and asthma-COPD overlap syndrome. J Thorac Dis 2017;9:1547–56. 10.21037/jtd.2017.05.07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Einvik G, Bhatnagar R, Holmedahl NH, et al. . Hypercapnea is associated with cardiac arrhythmias in COPD. Eur Respir J 2015;46:PA3007. [Google Scholar]
- 11.Vukic Dugac A, Ruzic A, Samarzija M, et al. . Persistent endothelial dysfunction turns the frequent exacerbator COPD from respiratory disorder into a progressive pulmonary and systemic vascular disease. Med Hypotheses 2015;84:155–8. 10.1016/j.mehy.2014.11.017 [DOI] [PubMed] [Google Scholar]
- 12.Yeh JJ, Wang YC, Chen JH, et al. . Effect of systemic lupus erythematosus on the risk of incident respiratory failure: a national cohort study. PLoS One 2016;11:e0163382 10.1371/journal.pone.0163382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rusinowicz T, Zielonka TM, Zycinska K. Cardiac Arrhythmias in patients with exacerbation of COPD. Springer: Boston, MA, 2017. [DOI] [PubMed] [Google Scholar]
- 14.Oda N, Miyahara N, Ichikawa H, et al. . Long-term effects of beta-blocker use on lung function in Japanese patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 2017;12:1119–24. 10.2147/COPD.S133071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Puente-Maestu L, Álvarez-Sala LA, de Miguel-Díez J. Beta-blockers in patients with chronic obstructive disease and coexistent cardiac illnesses. COPD Research and Practice 2015;1:11 10.1186/s40749-015-0013-y [DOI] [Google Scholar]
- 16.Stefan MS, Rothberg MB, Priya A, et al. . Association between β-blocker therapy and outcomes in patients hospitalised with acute exacerbations of chronic obstructive lung disease with underlying ischaemic heart disease, heart failure or hypertension. Thorax 2012;67:977–84. 10.1136/thoraxjnl-2012-201945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Coppola S, Froio S, Chiumello D. β-Blockers in critically ill patients: from physiology to clinical evidence. Crit Care 2015;19:119 10.1186/s13054-015-0803-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Joo H, Han D, Lee JH, et al. . Heterogeneity of asthma-COPD overlap syndrome. Int J Chron Obstruct Pulmon Dis 2017;12:697–703. 10.2147/COPD.S130943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van der Molen T. Co-morbidities of COPD in primary care: frequency, relation to COPD, and treatment consequences. Prim Care Respir J 2010;19:326–34. 10.4104/pcrj.2010.00053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rutten FH, Zuithoff NP, Hak E, et al. . Beta-blockers may reduce mortality and risk of exacerbations in patients with chronic obstructive pulmonary disease. Arch Intern Med 2010;170:880–7. 10.1001/archinternmed.2010.112 [DOI] [PubMed] [Google Scholar]
- 21.Database NHIR. Taiwan: http://nhird.nhri.org.tw/en/index.html (cited in 2015). [Google Scholar]
- 22.Hu WS, Lin CL, Huang CY, et al. . Cataract increases the risk of peripheral artery occlusive disease: a nationwide population-based cohort study with propensity score. Int J Cardiol 2016;220:768–71. 10.1016/j.ijcard.2016.06.084 [DOI] [PubMed] [Google Scholar]
- 23.Baarnes CB, Kjeldgaard P, Nielsen M, et al. . Identifying possible asthma-COPD overlap syndrome in patients with a new diagnosis of COPD in primary care. NPJ Prim Care Respir Med 2017;27:16084 10.1038/npjpcrm.2016.84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wurst KE, St Laurent S, Hinds D, et al. . Disease burden of patients with asthma/COPD overlap in a US claims database: impact of ICD-9 coding-based definitions. COPD 2017;14:200–9. 10.1080/15412555.2016.1257598 [DOI] [PubMed] [Google Scholar]
- 25.Cheng SL, Chan MC, Wang CC, et al. . COPD in Taiwan: a national epidemiology survey. Int J Chron Obstruct Pulmon Dis 2015;10:2459–67. 10.2147/COPD.S89672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gao J, Iwamoto H, Koskela J, et al. . Characterization of sputum biomarkers for asthma-COPD overlap syndrome. Int J Chron Obstruct Pulmon Dis 2016;11:2457–65. 10.2147/COPD.S113484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yeh JJ, Wang YC, Kao CH. Asthma-chronic obstructive pulmonary diseases overlap syndrome increases the risk of incident tuberculosis: a national cohort study. PLoS One 2016;11:e0159012 10.1371/journal.pone.0159012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Boven JF, Román-Rodríguez M, Palmer JF, et al. . Comorbidome, pattern, and impact of asthma-COPD overlap syndrome in real life. Chest 2016;149:1011–20. 10.1016/j.chest.2015.12.002 [DOI] [PubMed] [Google Scholar]
- 29.Hekking PP, Amelink M, Wener RR, et al. . Prevalence of co-morbidities in severe asthma, COPD and overlap syndrome. Eur Respir J 2015;46:PA1045. [Google Scholar]
- 30.Divo MJ, Casanova C, Marin JM, et al. . COPD comorbidities network. Eur Respir J 2015;46:640–50. 10.1183/09031936.00171614 [DOI] [PubMed] [Google Scholar]
- 31.Swerdlow DI, Holmes MV, Kuchenbaecker KB, et al. . The interleukin-6 receptor as a target for prevention of coronary heart disease: a mendelian randomisation analysis. Lancet 2012;379:1214–24. 10.1016/S0140-6736(12)60110-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lim GB. Arrhythmias: IL-6 and risk of atrial fibrillation in chronic kidney disease. Nat Rev Cardiol 2016;13:183 10.1038/nrcardio.2016.23 [DOI] [PubMed] [Google Scholar]
- 33.Mabuchi N, Tsutamoto T, Wada A, et al. . Relationship between interleukin-6 production in the lungs and pulmonary vascular resistance in patients with congestive heart failure. Chest 2002;121:1195–202. 10.1378/chest.121.4.1195 [DOI] [PubMed] [Google Scholar]
- 34.Koehler U, Hildebrandt O, Krönig J, et al. . [Chronic hypoxia and cardiovascular risk : Clinical significance of different forms of hypoxia]. Herz 2017. (Epub ahead of print). 10.1007/s00059-017-4570-5 [DOI] [PubMed] [Google Scholar]
- 35.Suzuki T, Tada Y, Kawata N, et al. . Clinical, physiological, and radiological features of asthma-chronic obstructive pulmonary disease overlap syndrome. Int J Chron Obstruct Pulmon Dis 2015;10:947–54. 10.2147/COPD.S80022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Costanzo L, Pedone C, Battistoni F, et al. . Relationship between FEV1 and arterial stiffness in elderly people with chronic obstructive pulmonary disease. Aging Clin Exp Res 2017;29:157–64. 10.1007/s40520-016-0560-3 [DOI] [PubMed] [Google Scholar]
- 37.Zhang XL, Chi YH, Wang leF, et al. . Systemic inflammation in patients with chronic obstructive pulmonary disease undergoing percutaneous coronary intervention. Respirology 2014;19:723–9. 10.1111/resp.12295 [DOI] [PubMed] [Google Scholar]
- 38.Ayashi S, Assareh AR, Jalali MT, et al. . Role of antioxidant property of carvedilol in mild to moderate hypertensive patients: a prospective open-label study. Indian J Pharmacol 2016;48:372–6. 10.4103/0253-7613.186206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Su VY, Chang YS, Hu YW, et al. . Carvedilol, bisoprolol, and metoprolol use in patients with coexistent heart failure and chronic obstructive pulmonary disease. Medicine 2016;95:e2427 10.1097/MD.0000000000002427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kubota Y, Asai K, Furuse E, et al. . Impact of β-blocker selectivity on long-term outcomes in congestive heart failure patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 2015;10:515–23. 10.2147/COPD.S79942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Calzavacca P, Lankadeva YR, Bailey SR, et al. . Effects of selective β1-adrenoceptor blockade on cardiovascular and renal function and circulating cytokines in ovine hyperdynamic sepsis. Crit Care 2014;18:610 10.1186/s13054-014-0610-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Serg M, Kampus P, Kals J, et al. . Nebivolol and metoprolol: long-term effects on inflammation and oxidative stress in essential hypertension. Scand J Clin Lab Invest 2012;72:427–32. 10.3109/00365513.2012.691991 [DOI] [PubMed] [Google Scholar]
- 43.Ohtsuka T, Hamada M, Hiasa G, et al. . Effect of beta-blockers on circulating levels of inflammatory and anti-inflammatory cytokines in patients with dilated cardiomyopathy. J Am Coll Cardiol 2001;37:412–7. 10.1016/S0735-1097(00)01121-9 [DOI] [PubMed] [Google Scholar]
- 44.Chung WS, Lin CL, Kao CH. Comparison of acute respiratory events between asthma-COPD overlap syndrome and COPD patients: a population-based cohort study. Medicine 2015;94:e755 10.1097/MD.0000000000000755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Barnes PJ. Therapeutic approaches to asthma-chronic obstructive pulmonary disease overlap syndromes. J Allergy Clin Immunol 2015;136:531–45. 10.1016/j.jaci.2015.05.052 [DOI] [PubMed] [Google Scholar]
- 46.Yamauchi Y, Yasunaga H, Matsui H, et al. . Comparison of in-hospital mortality in patients with COPD, asthma and asthma-COPD overlap exacerbations. Respirology 2015;20:940–6. 10.1111/resp.12556 [DOI] [PubMed] [Google Scholar]
- 47.Kitaguchi Y, Yasuo M, Hanaoka M. Comparison of pulmonary function in patients with COPD, asthma-COPD overlap syndrome, and asthma with airflow limitation. Int J Chron Obstruct Pulmon Dis 2016;11:991–7. 10.2147/COPD.S105988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Feng JX, Lin Y, Lin J, et al. . Relationship between fractional exhaled nitric oxide level and efficacy of inhaled corticosteroid in asthma-COPD overlap syndrome patients with different disease severity. J Korean Med Sci 2017;32:439–47. 10.3346/jkms.2017.32.3.439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee HY, Baek SH. Optimal use of beta-blockers for congestive heart failure. Circ J 2016;80:565–71. 10.1253/circj.CJ-16-0101 [DOI] [PubMed] [Google Scholar]
- 50.Donohue JF, Ohar JA. Effects of corticosteroids on lung function in asthma and chronic obstructive pulmonary disease. Proc Am Thorac Soc 2004;1:152–60. 10.1513/pats.200402-003MS [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.