Abstract
Objectives
In a randomised controlled trial, we found that informing women about overdetection changed their breast screening decisions. We now present a mediation analysis exploring the psychological pathways through which study participants who received the intervention processed information about overdetection and how this influenced their decision-making. We examined a series of potential mediators in the causal chain between exposure to overdetection information and women’s subsequently reported breast screening intentions.
Design
Serial multiple mediation analysis within a randomised controlled trial.
Setting
New South Wales, Australia.
Participants
811 women aged 48–50 years with no personal history of breast cancer.
Interventions
Two versions of a decision aid giving women information about breast cancer deaths averted and false positives from mammography screening, either with (intervention) or without (control) information on overdetection.
Main outcome
Intentions to undergo breast cancer screening in the next 2–3 years.
Mediators
Knowledge about overdetection, worry about breast cancer, attitudes towards breast screening and anticipated regret.
Results
The effect of information about overdetection on women’s breast screening intentions was mediated through multiple cognitive and affective processes. In particular, the information led to substantial improvements in women’s understanding of overdetection, and it influenced—both directly and indirectly via its effect on knowledge—their attitudes towards having screening. Mediation analysis showed that the mechanisms involving knowledge and attitudes were particularly important in determining women’s intentions about screening participation.
Conclusions
Even in this emotive context, new information influenced women’s decision-making by changing their understanding of possible consequences of screening and their attitudes towards undergoing it. These findings emphasise the need to provide good-quality information on screening outcomes and to communicate this information effectively, so that women can make well-informed decisions.
Trial registration number
This study was prospectively registered with the Australian New Zealand Clinical Trials Registry (ACTRN12613001035718) on 17 September 2013.
Keywords: breast imaging, overdiagnosis, decision aid, informed decision making, cancer screening, mediation
Strengths and limitations of this study.
Random allocation between two decision aids, differing only in the presence or absence of information about overdetection, enabled a rigorous test of the specific effects of this information when described in the context of other screening outcomes.
Participants were women entering the target age range for breast screening, who were sampled randomly from the general community and were facing real decisions.
Our serial mediation model controlled for a comprehensive set of baseline variables and examined plausible, theory-driven cause–effect relationships between exposure to the intervention and subsequently measured variables.
Nonetheless, given the cross-sectional nature of the outcome and mediator data, we cannot definitively establish the causal sequence of these variables.
Introduction
Breast cancer screening is a complex and emotionally charged issue,1 a topic surrounded by what has been described as a perfect storm of politics and science.2 While screening can reduce deaths from breast cancer, it can also cause harm through the counterintuitive phenomenon of overdetection or overdiagnosis. The term overdetection is increasingly accepted in the specific context of screening to distinguish it from overdiagnosis that occurs via other mechanisms, such as broadening disease definitions. An overdetected breast cancer is one found by screening, and consequently treated, that would not have caused any health problems had it been left undetected and untreated.3 Without screening, such a cancer would never have been diagnosed. Overdetected cancers are ‘real’ cancers in the sense that they meet current pathological criteria for cancer diagnosis, but finding and treating them does not improve health outcomes. Such a diagnosis and the resulting treatment can cause serious lifelong harm, and overdetection is, therefore, considered the major downside to breast screening.
Mounting evidence of the extent of overdetection (estimated as 19% of breast cancers diagnosed in women invited to screen from age 50 to 69 years4 and 30% for those who attend screening5) has led to recognition that the benefits and harms of breast screening are finely balanced for women at population-level risk of breast cancer. The risk of overdetection and its consequences must be weighed against the benefit of reducing breast cancer mortality (relative risk reduction estimated as 20% for women invited to screen from age 50 to 694 and 30% for those screened5). Experts familiar with the evidence now acknowledge that individual women may perceive the harm-benefit trade-off differently depending on their personal context and preferences—some will opt for screening while others decline, and either choice may be appropriate if it represents an informed decision.6–8 Throughout the history of breast screening, however, women invited to participate have not been given all the relevant information.9–11 Consensus is growing that information on screening benefits and harms, including overdetection, must be communicated clearly and transparently to women offered screening so that they can make informed decisions about whether to be screened.4 12 13 This is all the more important because of evidence that women hold misconceptions about breast screening and its effects.14 15
Against the background of this recommended shift in communication, the issue of how information about overdetection affects women and their screening decisions is critical. In a randomised trial, we addressed this question in women approaching the recommended age for starting mammography screening (age 50, when women are invited for screening in many countries including Australia).16 We sent women one of two versions of a decision aid (evidence-based information booklet) giving information about breast cancer deaths averted and false positives from screening (abnormal mammograms in women without cancer), either with or without information on overdetection.17 The intervention produced several significant effects on decision-making.16 The additional overdetection information improved knowledge, increased the number of women making an informed choice about screening (primary outcome of the trial), and also reduced positive attitudes to screening and the number of women intending to be screened.16
From our study design— chosen to identify the specific impact of information about overdetection—it appears that communicating this information influenced women’s assessment of the value of screening to them, leading to lower intentions to be screened within the intervention group. This finding has never been observed before and raises important questions. To facilitate the translation of intervention research findings into other contexts, it is recommended to test hypothesised causal mechanisms.18 However, causal processes leading from the use of decision aids to the decisions subsequently made are not well understood, as few studies have addressed questions about how these interventions achieve their effects.19 Only recently have decision aid developers started to critically examine in detail how behavioural, cognitive and social theories of decision-making could inform the design and evaluation of decision support interventions.20 In this paper, we explore the psychological pathways through which study participants processed overdetection information and integrated it into their decision-making. We provide an explanatory account incorporating cognitive and affective pathways, using psychological theories21 and mediation analysis.22
Methods
We did a parallel-group randomised controlled trial with women aged 48–50 years, recruited from the general community in New South Wales, Australia. The trial is described in detail elsewhere.16 23 Trained interviewers from an independent non-profit company recruited participants via telephone. Women were eligible if they had not undergone mammography in the past 2 years and did not have a personal or strong family history of breast cancer. Participants knew that they would receive one of two versions of a breast screening information booklet but did not know how these differed or which was the intervention.
We collected sociodemographics and baseline data on women’s stage of decision-making (how far along they were with their decision about breast screening), basic conceptual knowledge, attitudes and intentions (table 1).16 23 We then randomly assigned 879 women to the intervention (n=440) or control group (n=439) and sent their allocated decision aid by post. A programmer who had no contact with participants generated the randomisation sequence, which was inaccessible until after recruitment, ensuring allocation concealment.
Table 1.
Baseline sample characteristics (N=811)
| Variable | Intervention group (n=406) |
Control group (n=405) |
| Sociodemographics | n (%) | n (%) |
| Family history of breast cancer | ||
| No close blood relative ever diagnosed | 389 (96) | 386 (95) |
| One close blood relative diagnosed aged ≥50 years | 17 (4) | 19 (5) |
| Country of birth | ||
| Australia or New Zealand | 327 (81) | 335 (83) |
| Other | 79 (19) | 70 (17) |
| Main language spoken at home | ||
| English | 390 (96) | 396 (98) |
| Other | 16 (4) | 9 (2) |
| Education | ||
| School only or trade certificate | 226 (56) | 225 (56) |
| Diploma or university degree or higher | 180 (44) | 180 (44) |
| Marital status | ||
| Married or living with a partner | 317 (78) | 333 (82) |
| Not currently living with a partner | 89 (22) | 72 (18) |
| Parent status | ||
| Has one or more children | 361 (89) | 363 (90) |
| No children | 45 (11) | 42 (10) |
| Work status | ||
| Working full time or part time | 333 (82) | 341 (84) |
| No paid job currently | 73 (18) | 64 (16) |
| Age | ||
| 48–49 years | 289 (71) | 294 (73) |
| 50 years | 117 (29) | 111 (27) |
| Preintervention measures | Mean (SD) | Mean (SD) |
| Stage of decision-making about screening | 3.4 (1.0) | 3.4 (0.9) |
| Knowledge (basic concepts of screening) | 4.4 (0.8) | 4.4 (0.8) |
| Baseline attitudes to breast screening | 26.5 (3.6) | 26.8 (3.6) |
| Baseline intentions about screening | 4.5 (0.8) | 4.6 (0.8) |
All baseline variables appearing above were included as covariates in the mediation analysis (sociodemographic factors were dichotomised as shown). Possible ranges: stage of decision-making 1 (not yet thought about the options) to 4 (already made a choice), knowledge 0 (none correct) to 5 (all correct), attitudes 6 (least positive) to 30 (most positive), intentions 1 (definitely not) to 5 (definitely).
The intervention decision aid contained evidence-based explanatory and quantitative information about important outcomes of undergoing screening biennially from age 50 to 69 years (breast cancer mortality reduction, overdetection and false positives) compared with not screening over this period. The control decision aid omitted all overdetection content but was otherwise identical to the intervention. The decision aids were short booklets combining text and visual formats and are published.16 17
Our purpose in the analysis reported here was to explore causal pathways between exposure to information about overdetection in a decision aid (intervention) and subsequent breast screening intentions (outcome). We examined a series of potential mediators of this relationship: knowledge about overdetection, worry about breast cancer, attitudes towards breast screening and anticipated regret. We collected follow-up data for these variables using standardised questions in a structured postintervention telephone interview, 1–4 weeks after randomisation. The participant’s group assignment was unknown to the interviewer until the end of the interview.
Our postintervention knowledge scale assessed conceptual understanding of three key screening outcomes (breast cancer mortality reduction, overdetection and false positives) and awareness of the approximate numbers affected.16 For the mediation analysis, we used the overdetection knowledge subscale (scored 0–10, including conceptual and numeric components) because conveying this new information was the main aim of the intervention. We assessed attitudes to breast screening via a widely used 6-item instrument (possible range: 6–30), intentions to undergo screening in the next 2–3 years (1 item, 5-point response scale from definitely to definitely not) and worry about developing breast cancer (1 item, 4-point scale).16 23 24 Higher scores on these measures reflect better knowledge, more positive attitudes and intentions, and greater worry, respectively. We collected women’s anticipated regret both for screening (anticipating that if she undergoes screening (action) she may later wish she had not) and not screening (anticipating that if she does not undergo screening (inaction) she may later wish she had).25 We then calculated a differential anticipated regret score26 by subtracting the action from the inaction score. Higher scores on the resulting measure (possible range: –4 to 4) reflect greater anticipated regret for not screening, adjusted for the woman’s anticipated regret for screening. See the (online supplementary appendix 1)for further details about these measures.
bmjopen-2017-016246supp001.pdf (125.4KB, pdf)
We tested whether these variables functioned in a chain with a specified direction of causal flow (serial mediation).22 Based on health psychology theories (eg, theory of planned behaviour27 28) we tested the following causal chain: intervention (group allocation) → overdetection knowledge → worry → attitudes → anticipated regret → intentions. One could hypothesise, for example, that exposure to information (if communicated effectively) should increase knowledge about overdetection. Understanding that some breast cancers would not cause harm even if untreated might reduce worry about breast cancer, which may affect attitudes towards screening. Anticipation of feeling regret if one does not (vs does) undergo screening might depend on attitudes and in turn influence intentions.
Mediation models were tested using model 6 in the PROCESS macro (V.2.16) for SPSS (V.24).22 This procedure applies an ordinary least squares path analytic framework to estimate both direct and indirect effects (IEs) of the intervention on screening intentions. To derive these effects, PROCESS fits a series of linear regression models with each variable treated as the outcome in turn. The regression coefficients estimate how each variable affects other variables later in the sequence. Baseline variables in table 1 (all measured preintervention, including baseline screening intentions) were statistically controlled by including them as covariates during mediation analyses. Outcome and mediator variables were standardised (expressed in units of SD from the sample mean) for the mediation analysis. We used a bootstrapping procedure in order to conduct inference tests for the IEs. This involved repeatedly drawing samples (with replacement) of size n (where n equals the original sample size) from the existing data, and then estimating the IE in each re-sampled dataset. By repeating this process thousands of times, PROCESS generated an empirical approximation of the underlying sampling distribution of the IE which was then used to construct a CI for the effect. In this study, 50 000 bootstrap samples were used to create 95% bias-corrected CIs (95% CIs) for the IEs, which we considered significant if the CI did not include zero.
Results
Of 879 participants randomised, 838 completed the follow-up interview. Among these, 27 did not answer all relevant questions and were excluded from the mediation analysis. Sociodemographic characteristics were similar for randomised participants who were and were not included in the mediation analysis. Table 1 shows baseline characteristics of the 811 included participants, which were well balanced between the intervention and control groups.
Table 2 presents mean postintervention scores for intervention and control groups on the variables included in the mediation model. Compared with controls, the intervention group showed greater knowledge about overdetection, lower worry about breast cancer, less positive attitudes towards breast screening, lower anticipated regret for not screening (vs for screening) and lower intentions to undergo screening. Correlations between these variables were significant (p<0.001) as shown in the (online supplementary appendix).
Table 2.
Means and SDs for study groups on screening intentions and mediator variables
| Variable | Intervention group (n=406) |
Control group (n=405) |
|
| Mean (SD) | Mean (SD) | p Value | |
| Overdetection knowledge | 6.2 (2.2) | 4.0 (1.6) | <0.001 |
| Breast cancer worry | 1.7 (0.7) | 1.8 (0.7) | <0.001 |
| Screening attitudes | 24.5 (4.4) | 26.1 (4.1) | <0.001 |
| Anticipated regret | 1.9 (1.7) | 2.5 (1.6) | <0.001 |
| Screening intentions | 4.1 (1.1) | 4.5 (0.9) | <0.001 |
Possible score ranges were as follows: overdetection knowledge 0–10, breast cancer worry 1–4, attitudes 6–30, anticipated regret −4 to 4, intentions 1–5. See (online supplementary appendix 1) for further details on measures. Groups were compared here using t-tests.
Serial mediation analysis found that the total IE of the intervention on intentions was statistically significant, indicating that the intervention influenced intentions indirectly through its effects on the combined set of mediators. Reading the intervention rather than the control decision aid was associated with a decrease in screening intentions as a result of all specific indirect causal sequences in the model (table 3). As the direct effect was not significant, there was no evidence that the intervention affected intentions independently of its influence on the mediators modelled.
Table 3.
Direct and indirect effects (IEs) of the intervention on intentions via four sequential mediators
| Path | Effect | SE | 95% CI | |
| Total effect | −0.2768 | 0.0540 | −0.3828 | −0.1708 |
| Direct effect | −0.0192 | 0.0501 | −0.1175 | 0.0791 |
| Total IE | −0.2576 | 0.0449 | −0.3488 | −0.1734 |
| Specific IEs | ||||
| 1. Knowledge | −0.0731 | 0.0267 | −0.1281 | −0.0230 |
| 2. Knowledge, worry | −0.0010 | 0.0017 | −0.0073 | 0.0007 |
| 3. Knowledge, attitudes | −0.0700 | 0.0171 | −0.1071 | −0.0396 |
| 4. Knowledge, anticipated regret | −0.0201 | 0.0072 | −0.0375 | −0.0088 |
| 5. Knowledge, worry, attitudes | −0.0001 | 0.0007 | −0.0023 | 0.0011 |
| 6. Knowledge, worry, anticipated regret | −0.0004 | 0.0005 | −0.0021 | 0.0002 |
| 7. Knowledge, attitudes, anticipated regret | −0.0121 | 0.0040 | −0.0220 | −0.0059 |
| 8. Knowledge, worry, attitudes, anticipated regret | −0.0000 | 0.0001 | −0.0004 | 0.0021 |
| 9. Worry | −0.0047 | 0.0050 | −0.0191 | 0.0021 |
| 10. Worry, attitudes | −0.0003 | 0.0027 | −0.0063 | 0.0046 |
| 11. Worry, anticipated regret | −0.0020 | 0.0014 | −0.0063 | −0.0003 |
| 12. Worry, attitudes, anticipated regret | −0.0001 | 0.0005 | −0.0012 | 0.0008 |
| 13. Attitudes | −0.0618 | 0.0285 | −0.1178 | −0.0065 |
| 14. Attitudes, anticipated regret | −0.0106 | 0.0056 | −0.0241 | −0.0016 |
| 15. Anticipated regret | −0.0012 | 0.0104 | −0.0216 | 0.0200 |
N=811; 50 000 bootstrap samples; bias-corrected CIs. The sequential mediators are: overdetection knowledge, breast cancer worry, attitudes, anticipated regret. Bold effects are significant (p<0.05).
The specific path coefficients are shown in figure 1. The figure illustrates, for example, that participants who received the intervention decision aid demonstrated greater knowledge than controls, participants with greater knowledge expressed less positive attitudes and participants with less positive attitudes also had less positive intentions.
Figure 1.
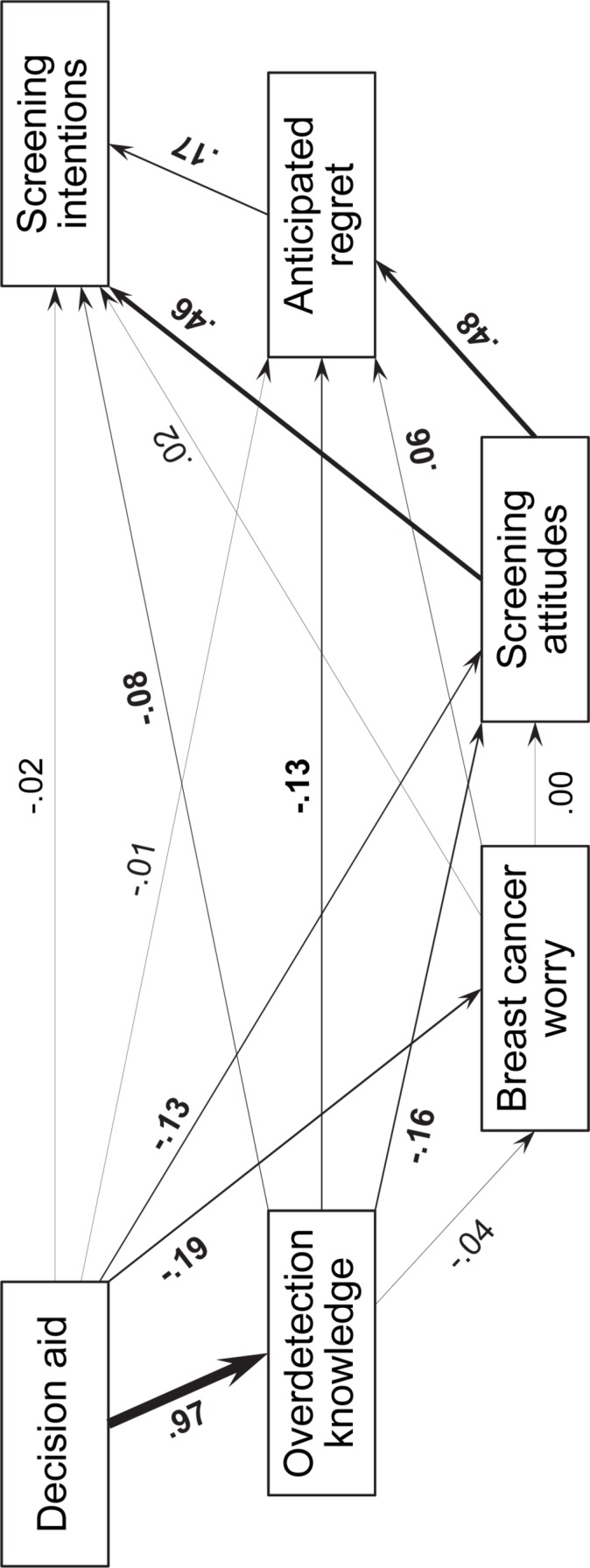
Graphic representation of the serial multiple mediation model of decision aid effects on breast screening intentions via four sequential mediators (overdetection knowledge, breast cancer worry, screening attitudes and anticipated regret). The intervention was hypothesised to exert an effect on screening intentions through the four mediators in sequence. Outcome and mediator variables were standardised prior to analysis. Bold coefficients are significant (p<0.05). Analyses controlled for baseline measures including screening intentions and attitudes, basic screening knowledge, stage of decision-making, breast cancer family history, birthplace, main language spoken, education, marital status, parent status, work status and age.
Table 3 presents effect estimates and 95% CIs for the 15 specific IEs representing causal pathways through the various mediator sequences. The main significant IEs of the intervention on intentions were those involving knowledge and attitudes as mediators, both separately (IE1, IE13 in table 3) and together in sequence (IE3). The first specific IE (IE1) tested whether overdetection knowledge mediated the relationship between the decision aid received and subsequent breast screening intentions; this effect was significant. Relative to those assigned to the control decision aid, participants receiving the intervention demonstrated better knowledge about overdetection and consequently expressed lower intentions to have screening. Another significant effect, IE13 showed that the intervention resulted in less positive attitudes, which also led to lower screening intentions. IE3 tested the causal chain: intervention → knowledge → attitudes → intentions. This was also significant and demonstrated that participants exposed to the intervention gained better overdetection knowledge, those with better knowledge had less positive attitudes, and these attitudes were in turn associated with reduced intentions to screen. Pairwise contrasts revealed that the three largest specific IEs (IE1, IE3 and IE13) did not significantly differ in size.
The anticipated regret variable was also involved in several significant mediation pathways, influenced by knowledge and attitudes separately (IE4, IE14) and together (IE7). The most complex of the significant IEs was IE7 leading from the intervention → overdetection knowledge → screening attitude → anticipated regret → screening intention. Compared with the control group, women receiving the intervention had greater overdetection knowledge, which led to less positive attitudes (as above); these were in turn associated with lower anticipated regret for not screening (vs screening), which translated into reduced intentions to screen.
The specific IE for the pathway through the complete causal chain involving all four mediators in sequence (IE8)—that is, adding breast cancer worry to the mediators discussed above—was not significant. Worry was part of only one significant IE (IE11). The intervention reduced breast cancer worry; women with lower worry had lower anticipated regret for not screening, which again reduced screening intentions.
Discussion
This study showed that the relationship between exposure to information on overdetection and women’s subsequent breast screening intentions was mediated by multiple cognitive and affective pathways. The intervention decision aid substantially improved understanding of overdetection, and it influenced—both directly and indirectly via its effect on knowledge—women’s attitudes towards having screening. The mediation analysis revealed that these mechanisms involving knowledge and attitudes were particularly important in determining intentions about screening participation. Anticipated regret played a role in several additional pathways linking knowledge, attitudes and intentions. As women became more knowledgeable about overdetection and their screening attitudes became less positive, this lessened their expectation that not screening would cause regret and increased the realisation that screening might cause regret, which in turn influenced intentions. The non-significance of the direct effect (ie, relationship between study group and intentions after adjusting for all mediators) confirms that our model captured the key relevant constructs, suggesting little of the observed total effect was due to other differences between the intervention and control decision aids (eg, length, newness of information and time spent reading).
The randomised controlled trial design is a key strength of this study. Random allocation between two decision aids, differing only in the presence or absence of information about overdetection, enabled a rigorous test of the specific effects of this information when described in the context of other screening outcomes. Our serial mediation model controlled for a comprehensive set of baseline variables and examined plausible, theory-driven cause–effect relationships between exposure to the intervention and subsequently measured variables. Nonetheless, a limitation is that given the cross-sectional nature of the outcome and mediator data, we cannot definitively establish the causal sequence of these variables. While some of the group differences shown in table 2 are small, our purpose in this article was not to establish the clinical significance of such differences (see elsewhere for more detailed analysis16) but rather to explore possible causal mechanisms involved. Whether the outcome variables in the serial mediation model are normally distributed or not, the inferences are likely to remain valid due to the large sample size of the study.22 29 Participants had not been screened in the 2 years prior to the study and were close to the age (50 years) at which women are invited into the Australian national breast screening programme. Intervention effects could vary in other populations depending on age and cultural context. For example, providing information about overdetection to women who already have more personal experience with screening (eg, women in their 60s) might produce less of an effect on attitudes and intentions, as suggested by our previous qualitative research.30
Although previous literature has reported on screening decisions aided by decision support techniques,31 32 little work to date has examined mechanisms for how information provided in such resources translates into decisions. Our mediation findings are in line with the explanatory account of health decisions offered by the theory of planned behaviour.27 28 Under this theory, attitudes towards a behaviour are determined by salient beliefs about its consequences (in this case, the understanding conveyed by the decision aid that overdetection is a possible consequence of screening); these attitudes in turn determine intentions. Our observed mediation effects involving anticipated regret accord with other empirical evidence supporting its usefulness as an extension to the theory of planned behaviour.33 Worry about the threat of breast cancer, though emphasised by other health psychology theories, did not appear to play a major role in determining screening intentions among our study participants. While the power of emotion has been cited as a challenge for communicating harms of mammography,34 our findings reinforce the vital role of good educational materials by demonstrating how evidence-based information influenced women’s cognitions about screening and showing that cognitions, rather than emotions, were instrumental in decision-making. Using a theoretical basis in behavioural psychology or decision-making theory is often overlooked but may strengthen the design and evaluation of decision support materials, although operationalising such theories can be challenging.20 There is a need to develop and employ comprehensive theoretical frameworks that help us better understand the role of comprehension of benefits and harms in shaping informed screening decisions, as well as how external factors—such as conflicting information from different sources—may influence both information processing and decision-making in this sometimes controversial area.2 35–37
Conclusions
We have previously shown that giving women evidence-based written information about overdetection in breast screening can change women’s screening intentions. Importantly, for the first time we now provide evidence, using mediation analysis, of how this cognitive and affective process works: the decision aid intervention achieved substantial knowledge gains, and thereby influenced attitudes and intentions towards screening. Our findings underline the importance of providing good-quality information to women when they are invited to consider screening, using materials with the capacity to successfully impart new and relevant knowledge. Effective communication tools and decision support resources are especially needed against a background of widely documented unrealistic public expectations of screening which may be driven by psychological factors in combination with sometimes misleading messages about benefits and lack of attention to harms.38 39 Our findings are a reminder that information can be a powerful intervention, and that the development of information resources must be done properly with rigour and care.
Supplementary Material
Acknowledgments
We thank Hazel Thornton for her contribution to the research project over many years and for helpful comments on an earlier draft of this manuscript.
Footnotes
Twitter: @jolynhersch @wiserhealthcare
Contributors: All authors contributed to study design. KMC, AB, JJ, NH, HD and KMG obtained funding. JH, KMC and JJ led development of the intervention and implementation of the trial. KMG advised on the statistical analysis. JH performed the statistical analysis, produced the tables and figure and drafted the manuscript. All authors contributed to data interpretation and critically reviewed the manuscript.
Funding: This work was supported by the National Health and Medical Research Council of Australia through project grant number 1062389.
Competing interests: None declared.
Ethics approval: This study was approved by the University of Sydney Human Research Ethics Committee (2012/1429). Participants gave informed consent to take part in the study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
- 1. Harvey SC. The charge and the challenges of breast cancer screening. J Womens Health 2014;23(Suppl 1):S1–2. 10.1089/jwh.2014.1509 [DOI] [PubMed] [Google Scholar]
- 2. Elmore JG. Breast cancer screening: balancing evidence with culture, politics, money, and media : Houssami N, Miglioretti D, Breast cancer screening: an examination of scientific evidence. Amsterdam: Elsevier, 2016:1–27. [Google Scholar]
- 3. Welch HG, Black WC. Overdiagnosis in cancer. J Natl Cancer Inst 2010;102:605–13. 10.1093/jnci/djq099 [DOI] [PubMed] [Google Scholar]
- 4. Independent UK Panel on Breast Cancer Screening. The benefits and harms of breast cancer screening: an independent review. Lancet 2012;380:1778–86. 10.1016/S0140-6736(12)61611-0 [DOI] [PubMed] [Google Scholar]
- 5. Jacklyn G, Glasziou P, Macaskill P, et al. Meta-analysis of breast cancer mortality benefit and overdiagnosis adjusted for adherence: improving information on the effects of attending screening mammography. Br J Cancer 2016;114:1269–76. 10.1038/bjc.2016.90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Heath I. It is not wrong to say no. BMJ 2009;338:b2529 10.1136/bmj.b2529 [DOI] [PubMed] [Google Scholar]
- 7. Kirwan CC. Breast cancer screening: what does the future hold? BMJ 2013;346:f87 10.1136/bmj.f87 [DOI] [PubMed] [Google Scholar]
- 8. Stefanek ME. Uninformed compliance or informed choice? A needed shift in our approach to cancer screening. J Natl Cancer Inst 2011;103:1821–6. 10.1093/jnci/djr474 [DOI] [PubMed] [Google Scholar]
- 9. Gummersbach E, Piccoliori G, Zerbe CO, et al. Are women getting relevant information about mammography screening for an informed consent: a critical appraisal of information brochures used for screening invitation in Germany, Italy, Spain and France. Eur J Public Health 2010;20:409–14. 10.1093/eurpub/ckp174 [DOI] [PubMed] [Google Scholar]
- 10. Jørgensen KJ, Gøtzsche PC. Content of invitations for publicly funded screening mammography. BMJ 2006;332:538–41. 10.1136/bmj.332.7540.538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zapka JG, Geller BM, Bulliard JL, et al. Print information to inform decisions about mammography screening participation in 16 countries with population-based programs. Patient Educ Couns 2006;63:126–37. 10.1016/j.pec.2005.09.012 [DOI] [PubMed] [Google Scholar]
- 12. Welch HG, Passow HJ. Quantifying the benefits and harms of screening mammography. JAMA Intern Med 2014;174:448–54. 10.1001/jamainternmed.2013.13635 [DOI] [PubMed] [Google Scholar]
- 13. Løberg M, Lousdal ML, Bretthauer M, et al. Benefits and harms of mammography screening. Breast Cancer Res 2015;17:63 10.1186/s13058-015-0525-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Biller-Andorno N, Jüni P. Abolishing mammography screening programs? A view from the Swiss Medical Board. N Engl J Med 2014;370:1965–7. 10.1056/NEJMp1401875 [DOI] [PubMed] [Google Scholar]
- 15. Schwartz LM, Woloshin S, Sox HC, et al. US women’s attitudes to false positive mammography results and detection of ductal carcinoma in situ: cross sectional survey. BMJ 2000;320:1635–40. 10.1136/bmj.320.7250.1635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hersch J, Barratt A, Jansen J, et al. Use of a decision aid including information on overdetection to support informed choice about breast cancer screening: a randomised controlled trial. Lancet 2015;385:1642–52. 10.1016/S0140-6736(15)60123-4 [DOI] [PubMed] [Google Scholar]
- 17. Hersch J, Jansen J, Barratt A, et al. Overdetection in breast cancer screening: development and preliminary evaluation of a decision aid. BMJ Open 2014;4:e006016 10.1136/bmjopen-2014-006016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Riddle M. Science of Behavior Change Working Group. News from the NIH: using an experimental medicine approach to facilitate translational research. Transl Behav Med 2015;5:486–8. 10.1007/s13142-015-0333-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Krones T, Keller H, Becker A, et al. The theory of planned behaviour in a randomized trial of a decision aid on cardiovascular risk prevention. Patient Educ Couns 2010;78:169–76. 10.1016/j.pec.2009.06.010 [DOI] [PubMed] [Google Scholar]
- 20. Elwyn G, Stiel M, Durand MA, et al. The design of patient decision support interventions: addressing the theory-practice gap. J Eval Clin Pract 2011;17:565–74. 10.1111/j.1365-2753.2010.01517.x [DOI] [PubMed] [Google Scholar]
- 21. Armitage CJ, Conner M. Social cognition models and health behaviour: a structured review. Psychol Health 2000;15:173–89. 10.1080/08870440008400299 [DOI] [Google Scholar]
- 22. Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York: Guilford, 2013. [Google Scholar]
- 23. Hersch J, Barratt A, Jansen J, et al. The effect of information about overdetection of breast cancer on women’s decision-making about mammography screening: study protocol for a randomised controlled trial. BMJ Open 2014;4:e004990 10.1136/bmjopen-2014-004990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dormandy E, Michie S, Hooper R, et al. Informed choice in antenatal Down syndrome screening: a cluster-randomised trial of combined versus separate visit testing. Patient Educ Couns 2006;61:56–64. 10.1016/j.pec.2005.02.006 [DOI] [PubMed] [Google Scholar]
- 25. Sandberg T, Hutter R, Richetin J, et al. Testing the role of action and inaction anticipated regret on intentions and behaviour. Br J Soc Psychol 2016;55:407–25. 10.1111/bjso.12141 [DOI] [PubMed] [Google Scholar]
- 26. Sivell S, Elwyn G, Edwards A, et al. Factors influencing the surgery intentions and choices of women with early breast cancer: the predictive utility of an extended theory of planned behaviour. BMC Med Inform Decis Mak 2013;13:92 10.1186/1472-6947-13-92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991;50:179–211. 10.1016/0749-5978(91)90020-T [DOI] [Google Scholar]
- 28. Ajzen I. Martin Fishbein’s legacy: the reasoned action approach. Ann Am Acad Pol Soc Sci 2012;640:11–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lumley T, Diehr P, Emerson S, et al. The importance of the normality assumption in large public health data sets. Annu Rev Public Health 2002;23:151–69. 10.1146/annurev.publhealth.23.100901.140546 [DOI] [PubMed] [Google Scholar]
- 30. Hersch J, Jansen J, Barratt A, et al. Women’s views on overdiagnosis in breast cancer screening: a qualitative study. BMJ 2013;346:f158 10.1136/bmj.f158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Biesecker BB, Schwartz MD, Marteau TM. Enhancing informed choice to undergo health screening: a systematic review. Am J Health Behav 2013;37:351–9. 10.5993/AJHB.37.3.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. van Agt HM, Korfage IJ, Essink-Bot ML. Interventions to enhance informed choices among invitees of screening programmes-a systematic review. Eur J Public Health 2014;24:789–801. 10.1093/eurpub/ckt205 [DOI] [PubMed] [Google Scholar]
- 33. Sandberg T, Conner M. Anticipated regret as an additional predictor in the theory of planned behaviour: a meta-analysis. Br J Soc Psychol 2008;47:589–606. 10.1348/014466607X258704 [DOI] [PubMed] [Google Scholar]
- 34. Rosenbaum L. Invisible risks, emotional choices–mammography and medical decision making. N Engl J Med 2014;371:1549–52. 10.1056/NEJMms1409003 [DOI] [PubMed] [Google Scholar]
- 35. Steckelberg A, Kasper J, Mühlhauser I. Selective information seeking: can consumers' avoidance of evidence-based information on colorectal cancer screening be explained by the theory of cognitive dissonance? Ger Med Sci 2007;5:Doc05. [PMC free article] [PubMed] [Google Scholar]
- 36. Baena-Cañada JM, Rosado-Varela P, Expósito-Álvarez I, et al. Using an informed consent in mammography screening: a randomized trial. Cancer Med 2015;4:1923–32. 10.1002/cam4.525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Petrova D, Garcia-Retamero R, Catena A, et al. To screen or not to screen: What factors influence complex screening decisions? J Exp Psychol Appl 2016;22:247–60. 10.1037/xap0000086 [DOI] [PubMed] [Google Scholar]
- 38. Hoffmann TC, Del Mar C. Patients' expectations of the benefits and harms of treatments, screening, and tests: a systematic review. JAMA Intern Med 2015;175:274–86. 10.1001/jamainternmed.2014.6016 [DOI] [PubMed] [Google Scholar]
- 39. Hersch JK, Nickel BL, Ghanouni A, et al. Improving communication about cancer screening: moving towards informed decision making. Public Health Res Pract 2017;27:e2731728 10.17061/phrp2731728 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-016246supp001.pdf (125.4KB, pdf)


