Abstract
Introduction
Allied health professionals (AHPs) report positive attitudes to using research evidence in clinical practice, yet often lack time, confidence and skills to use, participate in and conduct research. A range of multifaceted strategies including education, mentoring and guidance have been implemented to increase AHPs’ use of and participation in research. Emerging evidence suggests that knowledge brokering activities have the potential to support research engagement, but it is not clear which knowledge brokering strategies are most effective and in what contexts they work best to support and maintain clinicians’ research engagement.
Methods and analysis
This protocol describes an exploratory concurrent mixed methods study that is designed to understand how allied health research fellows use knowledge brokering strategies within tailored evidence-based interventions, to facilitate research engagement by allied health clinicians. Simultaneously, a realist approach will guide a systematic process evaluation of the research fellows’ pattern of use of knowledge brokering strategies within each case study to build a programme theory explaining which knowledge brokering strategies work best, in what contexts and why. Learning and behavioural theories will inform this critical explanation.
Ethics and dissemination
An explanation of how locally tailored evidence-based interventions improve AHPs use of, participation in and leadership of research projects will be summarised and shared with all participating clinicians and within each case study. It is expected that local recommendations will be developed and shared with medical and nursing professionals in and beyond the health service, to facilitate building research capacity in a systematic and effective way.
Keywords: Knowledge Brokering, Research Capacity Building, Knowledge Translation
Strengths and limitations of this study.
This protocol uses an innovative mixed methods design to explore and understand effective research capacity building from the perspective of allied health clinicians.
This protocol will monitor and evaluate the development and implementation of evidence-based interventions with allied health clinicians to build use of, participation in and leadership of research.
This protocol includes a realist evaluation of the context and mechanisms underlying successful knowledge brokering activities, incorporating a critical evaluation of learning and behavioural theories.
Limitations include the focus on locally funded case studies within one geographical area, that may not be able to be replicated in other settings.
Introduction
Clinician engagement in research has the potential to improve healthcare processes and performance.1 2 Specifically, patient care and service delivery benefits can be enhanced when research is led by the professionals who will use it.3 As clinicians identify key clinical needs and gaps, and collaborate with researchers to answer their questions, the resultant research has the potential to improve clinical practice.4 Further, evidence suggests that research engagement can enhance job satisfaction, professional confidence and contribute to enhanced attitudes towards research.5 6 Given these benefits, building research capacity and supporting research engagement are key strategic goals for many healthcare providers.7 However, there is significant diversity in the circumstances and mechanisms that translate clinicians’ research engagement into improved healthcare performance.1
In particular, allied healthcare professionals (AHPs) tend to be less engaged in research when compared with medical professionals. Allied health, the second largest clinical workforce in Australia, including physiotherapists, occupational therapists, speech pathologists, psychologists, dieticians, social workers and podiatrists, reports positive attitudes about the use of research evidence in clinical practice and many are interested in participating in research. A recent systematic review confirmed that allied health professionals are motivated to conduct research to increase their research skills and job satisfaction and enhance their careers.8 However, AHPs often describe barriers such as lacking time and confidence to conduct and use research.9–11 There is also considerable variation in the quality and quantity of research evidence to support clinical practice across the diverse range of professions described as allied health.11
Within complex healthcare settings, differing levels of clinician research engagement exist. While research engagement refers to clinicians participating in and leading specific research projects, the evidence-based practice movement has argued that all clinicians need to be able to read, critically appraise and apply appropriate research to improve their own clinical practice and provide individualised care to patients.12 Indeed, supporting AHPs to use research to inform their practice has been a key focus for this professional group.13–15 The ability to use and apply research is often seen as the precursor for clinicians to design and participate in research projects. Glasziou’s triangle supports this expectation and suggests that most clinicians will be users of research, some will participate and few will lead research projects.16 Despite the expectation that most clinicians should be using research to inform their clinical practice, many indicate that they do not have the time, resources, skills and support to do so.6
Recent evidence suggests that due to the complex nature of research engagement several processes are required to extend clinicians’ engagement in research from users to participants and leaders.17 There is limited evidence to support traditional approaches of didactic education, including conference attendance in building research engagement, and yet this tends to be an orthodox approach taken in healthcare to support clinician research engagement.18 Rather multifaceted and integrated approaches including printed educational materials, local opinion leaders, small group work, training, mentoring, supervision, partnership development, protected time, audit and feedback have been evaluated to be effective in building research capacity.17 19 20 More recently, models of collaborative and clinician-led research are proposed as more practical.21 Complementary strategies have also been recommended, including the provision of grant funding, bursaries, training, support networks and formal partnerships.22 Further, research leadership and conjoint positions are recommended strategies.8
As well as requiring a multifaceted approach to supporting research engagement, a key finding identified is that programmes need to be tailored to suit individual learners’ needs and, in allied health, this is often facilitated by research fellows.23–25 A recent systematic review suggested that embedding allied health research facilitators within healthcare settings contributed to increased research activity by boosting individual-based and team-based research skills and participation.26 These findings were confirmed by an Australian qualitative exploration of funded allied health research fellow positions, in that research fellows enhanced research skills, improved team work and fostered a research culture.6 However, it is not certain which research facilitator-led activities most influence clinicians’ research engagement. Further, there is evidence to suggest that a team-based approach to research capacity building can improve both individuals’ skills and the organisations’ capacity to support research.27 Thus, no one best model for improving clinicians’ research engagement and research capacity exists.28 29 Instead effective projects often create a suite of interventions and tailor these to the local context and individual needs.17 This makes it difficult to monitor and evaluate outcomes and the relationship between factors facilitating and supporting clinician research engagement remains unclear.1
Given these considerations, parallels exist between processes of individualised support and those used by knowledge brokers. Knowledge brokers were introduced in Canada to facilitate interactions between clinicians and researchers, to encourage the judicious use of research evidence in clinical decision making and practice, with varying levels of success.30 In the UK, knowledge brokers were embedded in service delivery teams to understand how research knowledge was used to inform clinical practice.31–33
To assist with explaining the processes required to support research engagement of AHPs, a deeper investigation of the work of knowledge brokers may be helpful.31–33 The exchange of knowledge can be considered as a dynamic social and political process, which is influenced by the surrounding context.34 Three major groups of knowledge brokering activities were delineated as effective in promoting the awareness and use of research evidence in multiple health-related settings, in a recent systematic review.35 Being a ‘knowledge manager’ involved identifying and organising relevant information for use. Being a ‘linkage agent’ included identifying, engaging and connecting key stakeholders to facilitate networks and collaboration between clinical practice and academic settings to bridge the gap between research knowledge and clinical practice. Finally, being a ‘capacity builder’ included developing clinicians’ capacity to access, analyse, interpret and apply knowledge, in order to participate in and lead research. While knowledge brokering activities have the potential to support researcher development, it is not clear from the published literature, which knowledge brokering strategies are most effective and in what contexts they work best.
Low levels of allied health research activity and capacity were documented in a Queensland health service following an audit in 2014.36 Since then, there has been significant infrastructural investment with the recruitment of a professorial and three research fellow positions during 2015. These positions were introduced to build a research culture and to facilitate clinician engagement in research, consistent with recommendations in a recent systematic review.8 This study proposes the development of exploratory case studies within a realist framework to investigate how specific knowledge brokering activities influence allied health clinicians’ research engagement in one local health service. Allied health research fellows will develop evidence-based interventions to facilitate research use, participation and leadership by allied health clinicians, and they will be guided to identify which knowledge brokering strategies are most beneficial, within specific clinical contexts.
Methods and analysis
Objectives
This research study seeks to understand how allied health research fellows use knowledge brokering strategies within tailored evidence-based interventions, to facilitate research engagement by allied health clinicians. The term research engagement encompasses clinicians using research evidence to inform their clinical practice, participating in research projects and leading research projects.
Specifically, the project has two objectives:
to document the patterns and outcomes of research engagement (use, participation in and leadership of research) for specific individuals and within clinical teams;
to document and explain the use of specific knowledge brokering strategies used to influence research engagement, in order to build a programme theory about which strategies work best, in what contexts and why.
Design
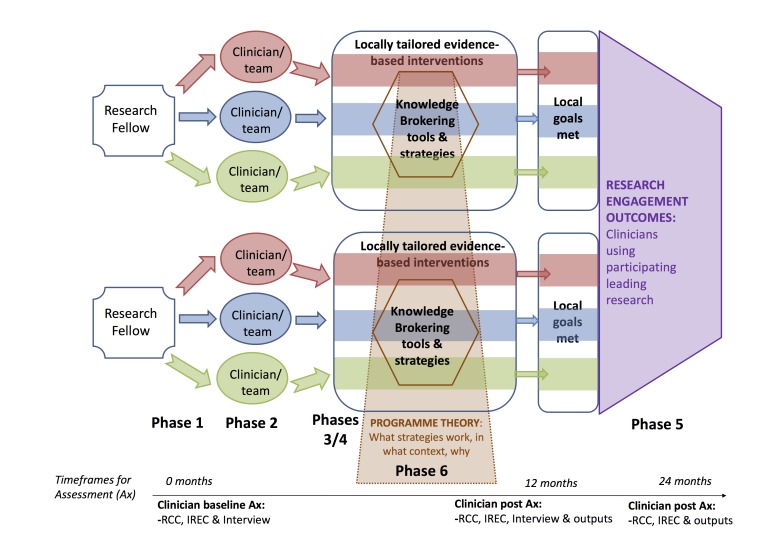
An exploratory concurrent mixed methods approach will be used to understand how allied health research fellows can design, implement and evaluate individual-based and team-based case studies of tailored evidence-based interventions, to facilitate engagement in research by allied health clinicians (see figure 1).
Figure 1.
Pragmatic model.
Simultaneously, a realist approach will guide a systematic process of monitoring the research fellows’ use of knowledge brokering strategies within each case study.37 Through examining each case study deeply and investigating commonalities between case studies, a programme theory will be postulated to explain which knowledge brokering strategies work best, in what contexts and why.
Study setting
This study will occur in one health service. All research fellows are recurrently funded within part time positions, to enhance research capability. All allied health clinicians have allocated time for professional development and are encouraged to use research to ensure their clinical practice is evidence based. Therefore, this research intervention will be a component of routine practice that will be formally monitored and evaluated.
The health service includes two hospitals and over 15 community centres and services. The smaller hospital is less than 15 years old and is located near a private university offering medical and some postgraduate allied health courses. The large tertiary hospital was rebuilt in 2013 beside a publicly funded university providing comprehensive undergraduate and postgraduate medical, nursing and allied health programmes.
Eligibility criteria
Clinician participants
We will recruit a convenience sample of allied health clinicians employed within the health service, who have line manager approval to participate. Participants will volunteer to engage in research, to support planning, delivery or evaluation of their own services.
Roger’s theory of diffusion of innovation will be used to identify motivated teams and individuals.38 Diffusion of innovation theory suggests that it is most efficient to work in an exploratory study with motivated teams and individuals. Therefore, ‘early adopter’ individuals and teams will be defined as those volunteering to work with the research fellows as part of this study.
Research fellow participants
The researchers described in this protocol are employed by the health service as research fellows. Research fellows are required to have completed their PhD and have both clinical and research experience. An additional independent researcher will lead the process evaluation for the realist evaluation, where all three research fellows and the principle investigator will participate in building the programme theory.
Intervention
Research fellows will design an evidence-based intervention for each participating individual or team of allied health clinicians. It will be designed to achieve an agreed research engagement goal that requires clinicians to use research evidence to inform their clinical practice, participate in research projects and/or lead a research project. Research fellows will facilitate each case study team or individual clinician, for up to 12 months, while using their choice of knowledge brokering strategies.
Within each case study, research fellows will be guided by the knowledge-to-action framework, to describe a knowledge–practice gap and to develop an intervention to enhance the understanding and use of research in clinical practice.39 Together with clinicians, they will identify a clinical challenge where the research evidence is not supported by clinical practice.
The Theoretical Domains Framework (TDF) will be used to identify, analyse and organise barriers and facilitators for change, for individuals within each case study.40 41 With an understanding of their participants’ abilities, and the local barriers and facilitators, research fellows will collaboratively set a realistic research engagement goal with the clinicians within each case study.
The identified barriers and facilitators will inform the intervention design and guide implementation strategies.39 Research fellows will synthesise and organise data from individual and focus group assessment to select and tailor evidence-based interventions to support clinicians’ research engagement. Where appropriate, research fellows will facilitate clinicians to implement a tailored local intervention and monitor it for future sustainability.
The behaviour change wheel will inform the intervention design.42 Together individuals’ capability, motivation and capacity for behaviour change will provide a deeper level of analysis and understanding of their research engagement. Workplace learning theory will also be considered when designing, implementing and explaining this study’s research capacity building interventions.43 It is acknowledged that learning occurs through practice and that clinical environments can be modified to augment learning. To include learning as a core component of building research engagement, we will focus on three key considerations: practice curriculum, pedagogic practices and personal epistemological practices.44 Consideration will also be given to how participant clinicians and research fellows identify, sequence and engage in learning experiences, and how the allied health clinicians construct knowledge from these experiences.
Research fellows will also choose appropriate and complementary knowledge brokering strategies to implement their evidence-based intervention, in each case study. It is expected that they will use a range of knowledge management, linkage and capacity building strategies to meet their team’s collaborative research engagement goal.35 The number and combination of knowledge brokering strategies will be chosen by each research fellow, dependent on team goals and individual learning needs.
Outcomes
There will be two set of different outcomes, to reflect the two study objectives. The first outcome will be the documentation by clinicians of their engagement in research over a 12-month intervention, within each case study. Clinicians will complete two self-reported questionnaires before and after their tailored intervention. Individual quantitative changes will be interpreted by comparison with qualitative interview and focus group data. It will be important to note how clinicians described achieving their research engagement goal and whether they identified learning new skills or changing their behaviour to use research to inform their clinical practice. It will also be vital to identify ways in which clinicians participated in and led research activities in their workplace.
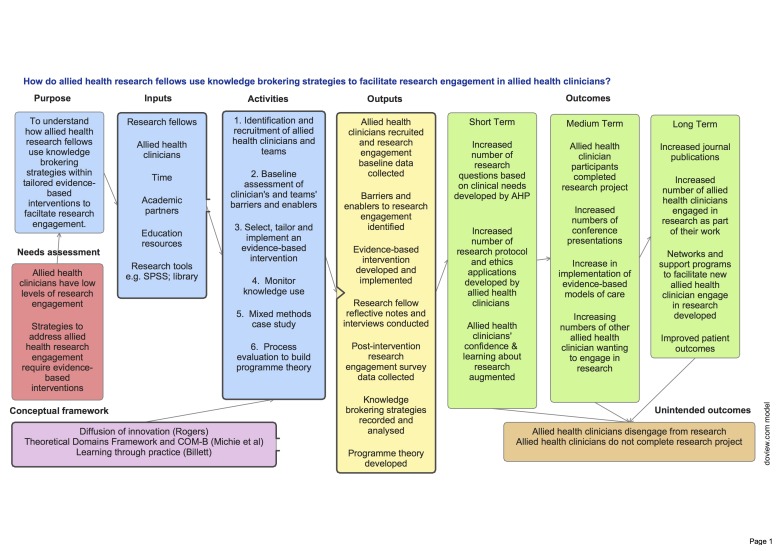
Specific examples of short-term, medium-term and long-term outcomes have been documented in the logic model (figure 2). We will look for increased numbers of research projects, research protocols, ethical applications, conference presentations, journal publications, grant applications and postgraduate study enrolments by allied health clinicians. We will also look for examples where clinicians have become more confident in understanding and using research evidence to inform clinical practice. We will be looking for changes in clinical practice, including models of care and patient outcomes, which are based on relevant research evidence. Initially, we will be documenting change by clinicians who participated in the evidence-based interventions facilitated by the research fellows, but we may be able to see similar changes in other clinicians who have been working alongside them. We will also look to document additional and unexpected changes.
Figure 2.
Logic model. AHP, allied health professional.
The second major outcome is the development of a programme theory about what knowledge brokering strategies are successful in building clinicians’ research engagement, in what contexts and for what reasons. A realist approach will be used to facilitate the research fellows to articulate and test behavioural and learning theories between different contexts and in response to their use of different knowledge brokering strategies.37
An independent researcher will facilitate research fellows to make comparisons within and between their own case studies about the usage of different knowledge brokering strategies. Research fellows will be encouraged to critically review their own context and identify key components of knowledge brokering strategies that facilitate successful research engagement and explain changes using learning and behavioural theories. All research fellows will build a programme theory about which knowledge brokering strategies facilitate clinicians’ research engagement, in which contexts and for which theoretical reasons.37 It will be important to consider the role and contribution of learning to behaviour change through addressing the interplay between individual learning needs, different behavioural interventions as clinicians engage in the use of research, and they participate in and lead research projects.
This protocol, coproduced by the researchers through active and critical contribution, enables each research fellow to work creatively to implement their own case studies.45 A logic model was simultaneously developed to document the resources, activities and outputs of this project, together with short-term, medium-term and long-term outcomes (see figure 2).
Participant timeline
The entire study procedure is summarised in the logic model across six phases (see figure 2). The approximate time for each phase is described:
identification and recruitment of allied health clinicians and teams (month −1 to start)
baseline assessment of clinicians and teams (month 1)
select, tailor and implement evidence-based intervention (from months 1 to 12)
mixed methods case study evaluation (at month 12)
monitor knowledge use (at months 3, 6, 9 and 12)
process evaluation to build programme theory (from months 4 to 14).
Phases 1–4 describe the intervention for each case study, embedded within a preassessment and postassessment for every participating clinician. Phases 5 and 6 will occur concurrently for the research fellows, as they document and monitor the use of specific knowledge brokering strategies used to facilitate clinicians’ research engagement.
A follow-up evaluation is planned for all clinicians after 24 months.
Sample size
A convenience sample of allied health clinicians was identified, for which all three research fellows could support in the time allocated for these positions. All research fellows were employed at half time to facilitate clinicians’ engagement in research. They were employed full time within the health service, in complementary roles of a senior clinician, an educator and a researcher.
Recruitment
An expression of interest was distributed by email to all allied health clinicians across the health service. Maximum variation sampling was used to ensure diverse representation across allied health professions.46 Clinicians were invited to demonstrate an interest in increasing their research engagement. They were required to have an interest in undertaking research, to want to learn more about using research in clinical practice and/or to identify support they required from a research fellow. They were also required to have formal support from their line manager to participate.
From the expressions of interest received, clinicians were matched with a research fellow who had complementary content and/or research skills. Potential conflicts of line management were avoided.
Data collection methods
Clinician participants
Within each case study, patterns of research engagement for individual clinicians will be documented using two self-report questionnaires. Clinicians were provided with paper and electronic versions of both questionnaires after they had completed and returned the participation information and consent form. All clinician participants were asked to provide a baseline measurement of their perceived engagement in research by completing the following two self-reported baseline assessments:
Research Capacity and Culture (RCC) tool,47
Individual Research Engagement Continuum (IREC) (available as online supplementary file).
bmjopen-2016-014876supp001.pdf (365.3KB, pdf)
The RCC tool is a validated questionnaire which measures confidence in engaging in research across individual, team and organisation domains.47 It includes statements that clinicians rate on a scale of 1–10 in terms of their team’s perceived success or skill level. The RCC tool also asks clinicians to identify whether (or not) they had experienced specific motivators and barriers to undertaking research as an individual or within a team.
The IREC tool has been developed specifically for this project for participants to indicate their practical level of research engagement, from non-user through to user and participant to leaders. Clinicians will be asked to indicate and describe their engagement in identifiable research behaviours and skills.
At baseline, all participant clinicians will be invited to a face-to-face interview and/or focus group. Where clinicians are working in a team-based case study, a focus group will be conducted and individual interviews will be used for clinicians working individually within a case study. The purpose is to identify and prioritise local barriers and facilitators at individual, team and organisational levels, within each case study, in order to inform the development of evidence-based interventions. An interview schedule has been informed by the 14 domains of the TDF40 41 to better understand the individual and team barriers and facilitators to AHP research engagement. Clinicians will have the opportunity to member check the transcripts and be involved in the decisions taken by research fellows in collaboratively setting a research engagement goal for the 12-month intervention.
After the 12-month-tailored intervention, participating clinicians within each case study will be invited to participate in an interview or focus group to reflect on their achievement of their research engagement goal. An interview schedule will guide a semistructured discussion about clinicians’ experiences of participating in a tailored evidence-based intervention. Participants will be asked to describe and explain any changes in their learning and their behaviour at work, and they will be asked about how these changes have influenced their engagement in research. This focus group/interview will be facilitated by a research fellow not involved in providing the intervention to that team. Documentation of specific outcomes will be undertaken at 12 and 24 months guided by suggestions highlighted in the logic model.
Research fellow participants
Research fellows will maintain reflective field notes for every interaction they have with clinician participants. They will document the knowledge brokering strategies used within each case study using a purpose-designed Knowledge Brokering Taxonomy tool based on a recent systematic review.35 This tool has been developed with prompting questions to describe key decisions taken, behaviours observed, changes and issues noted. Research fellows will be encouraged to justify their reasons for using specific knowledge brokering strategies and begin to explain how the particular strategy may have influenced any observable changes in clinicians’ learning and behaviour.
Short interviews will be conducted with each research fellow every 3 months by an independent researcher. Research fellows will be facilitated to review their own patterns of use of knowledge brokering strategies before each interview. Using their reflective notes and the Knowledge Brokering Taxonomy tool, each research fellow will be asked about the numbers and comparative frequency of knowledge brokering strategies they have used. For a commonly used knowledge brokering strategy, they will be asked to describe their justification for its use and the impact it has in facilitating clinicians’ research engagement. Interviews will be transcribed and thematically analysed by the independent researcher. They will look for patterns between the clinical context, the use of specific knowledge brokering strategies and observable behaviour change. This is consistent with a realist approach.37 After each series of interviews, a feedback discussion will be held with all research fellows to discuss common themes. Comparisons will be made within and across the different case studies in relation to the use and justification of specific knowledge brokering strategies.
Data management
All clinician and research fellow data will be stored electronically on a secure shared drive. Paper documents will be stored in a locked cabinet.
Data analysis
Clinician participants
Quantitative methods will be used to document patterns of research engagement by individuals. Individual scores from the RCC and IREC tools will be evaluated within each case study and across all participating clinicians in the project to determine changes before and after the intervention. Demographic variables will be presented in numbers and percentages. Median and IQRs will be calculated for each skill in each domain of the RCC at preintervention and postintervention timeframes and compared using a Wilcoxon signed-rank test to determine the effect of the intervention. For comparing pre, post and follow-up data, we will use a Friedman test. Chi-squared tests will be used to test relationships between dichotomous demographic, research activity, barrier and motivator variables. For categorical data, numbers and proportions will be used to display the data at preintervention and postintervention timeframes. Mann-Whitney U tests will be used to test differences between individual, team and organisation research capacity variables. An alpha level of 0.05 will be used and 95% CIs will be calculated.
Qualitative data analyses will be used for all focus group and individual interviews. Interviews will be transcribed verbatim and clinicians will be invited to member check their transcripts. Transcripts will be coded into descriptive categories and subcategories, for theoretically informed thematic analysis.46
At baseline and for each case study, individual RCC and IREC scores were considered together with the themes identified from interviews and focus groups to collaboratively develop the research engagement goal and the evidence-based intervention. After the intervention is complete, changes in individual questionnaire scores will be interpreted by comparison to the themes from interviews and focus groups. It is expected that quantitative changes (or the lack thereof) will be explained through clinicians’ experiences of learning about and engaging in research activities.
Research fellows
For the realist evaluation, there are likely to be several iterations of analysis performed to deepen understanding of how specific knowledge brokering interventions influenced clinicians’ research engagement. Research fellows will be facilitated to reflect and use theories of diffusion of innovations,38 behaviour change42 and workplace learning43 44 to discuss and explain how specific knowledge brokering strategies worked within specific clinical teams to increase clinicians’ engagement with research. There will be a forward analysis from context, to investigate the mechanisms that supported effective research engagement. At the same time, there will also be a backward analysis, where the goals achieved within each case study will be interrogated for the mechanisms that supported them, in specific contexts.37
Ethics and dissemination
Ethical approval has been received from Gold Coast Health (HREC/16/QGC/96) on 1 April 2016 and site specific and management approval (SSA/16/QGC/96) on 22 July 2016.
The feasibility and effectiveness of locally tailored evidence-based interventions will be summarised and shared with all participating clinicians and within each case study. Case studies will be individually described. A programme theory will be developed to explain which knowledge brokering strategies work best to enhance clinician’s research engagement. Where possible, the specific context and mechanisms will be linked to effective outcomes, with reference to learning and behavioural theories.
Lessons learnt will be shared with the wider allied health management and leadership groups through local presentations and feedback to clinical and management. Where appropriate, recommendations for enhancing clinicians’ engagement in research will be shared with nursing and medical staff in the same health service. Presentations will also be designed for state, national and international conferences. It is expected that presentations and publications will be sourced from individual or groups of case studies and from the research project as a whole.
It is expected that further work will be required to develop the programme theory and test a more specific range of knowledge brokering strategies in more consistent and rigorous research methodologies. It will also be important to investigate outcomes for medical and nursing staff, ideally within clinical teams.
Supplementary Material
Acknowledgments
with thanks to all participating allied health clinicians and managers
Footnotes
Contributors: SM developed the initial research question, and led the protocol development with CN, RW and KW. CN prepared the first draft of this manuscript. SM, RW and KW developed and refined the study protocol. AB is the independent researcher working with researchfellows to develop the programme theory. All authors provided critical evaluation and revision of the manuscript and have given final approval of the manuscript accepting responsibility for all aspects.
Funding: confirmed as accurate
Disclaimer: none required
Competing interests: None declared.
Patient consent: not required
Ethics approval: Gold Coast Health Ethics Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Hanney S, et al. Engagement in research: an innovative three-stage review of the benefits for health-care performance. Health Services and Delivery Research. 1, 2013. [PubMed] [Google Scholar]
- 2. Harding K, et al. Organisational benefits of a strong research culture in a health service: a systematic review. Australian Health Review, 2016. [DOI] [PubMed] [Google Scholar]
- 3. Blevins D, Farmer MS, Edlund C, et al. Collaborative research between clinicians and researchers: a multiple case study of implementation. Implement Sci 2010;5:1–9. 10.1186/1748-5908-5-76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Misso ML, Ilic D, Haines TP, et al. Development, implementation and evaluation of a clinical research engagement and leadership capacity building program in a large Australian health care service. BMC Med Educ 2016;16:1–9. 10.1186/s12909-016-0525-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zallman L, Tendulkar S, Bhuyia N, et al. Provider's perspectives on building research and quality improvement capacity in primary care: a strategy to improve workforce satisfaction. Clin Transl Sci 2013;6:404–8. 10.1111/cts.12066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wenke RJ, Mickan S, Bisset L. A cross sectional observational study of research activity of allied health teams: is there a link with self-reported success, motivators and barriers to undertaking research? BMC Health Serv Res 2017;17:114 10.1186/s12913-017-1996-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McKeon S, et al. Strategic Review of Health and Medical Research. Commonwealth of Australia: Canberra, 2013. [Google Scholar]
- 8. Borkowski D, McKinstry C, Cotchett M, et al. Research culture in allied health: a systematic review. Aust J Prim Health 2016;22:294–303. 10.1071/PY15122 [DOI] [PubMed] [Google Scholar]
- 9. Heiwe S, Kajermo KN, Tyni-Lenné R, et al. Evidence-based practice: attitudes, knowledge and behaviour among allied health care professionals. Int J Qual Health Care 2011;23:198–209. 10.1093/intqhc/mzq083 [DOI] [PubMed] [Google Scholar]
- 10. Stephens D, Taylor NF, Taylor N, et al. Research experience and research interests of allied health professionals. J Allied Health 2009;38:e107–11. [PubMed] [Google Scholar]
- 11. Pickstone C, Nancarrow S, Cooke J, et al. Building research capacity in the allied health professions. Evidence & Policy: A Journal of Research, Debate and Practice 2008;4:53–68. 10.1332/174426408783477864 [DOI] [Google Scholar]
- 12. Sackett DL, Rosenberg WM, Gray JA, et al. Evidence based medicine: what it is and what it isn't. BMJ 1996;312:71–2. 10.1136/bmj.312.7023.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dizon JMR, Grimmer-Somers KA, Kumar S. Current evidence on evidence-based practice training in allied health: a systematic review of the literature. Int J Evid Based Healthc 2012;10:347–60. 10.1111/j.1744-1609.2012.00295.x [DOI] [PubMed] [Google Scholar]
- 14. Harding KE, Stephens D, Taylor NF, et al. Development and evaluation of an allied health research training scheme. J Allied Health 2010;39:e143–8. [PubMed] [Google Scholar]
- 15. Tilson JK, Mickan S, Howard R, et al. Promoting physical therapists' use of research evidence to inform clinical practice: part 3--long term feasibility assessment of the PEAK program. BMC Med Educ 2016;16:1–13. 10.1186/s12909-016-0654-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Del Mar C, Askew D. Building family/general practice research capacity. Ann Fam Med 2004;2:S35–S40. 10.1370/afm.146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mazmanian PE, Coe AB, Evans JA, et al. Are researcher development interventions, alone or in any combination, effective in improving researcher behavior? A systematic review. Eval Health Prof 2014;37:114–39. 10.1177/0163278713510375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Haines A, Kuruvilla S, Borchert M. Bridging the implementation gap between knowledge and action for health. Bull World Health Organ 2004;82:724–31. [PMC free article] [PubMed] [Google Scholar]
- 19. Grimshaw JM, Eccles MP, Lavis JN, et al. Knowledge translation of research findings. Implementation Science 2012;7:1–17. 10.1186/1748-5908-7-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cooke J, Nancarrow S, Dyas J, et al. An evaluation of the 'Designated Research Team' approach to building research capacity in primary care. BMC Fam Pract 2008;9:1–12. 10.1186/1471-2296-9-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Brauer SG, Haines TP, Bew PG. Fostering clinician-led research. Aust J Physiother 2007;53:143–4. 10.1016/S0004-9514(07)70020-X [DOI] [PubMed] [Google Scholar]
- 22. Hulcombe J, Sturgess J, Souvlis T, et al. An approach to building research capacity for health practitioners in a public health environment: an organisational perspective. Aust Health Rev 2014;38:252–8. 10.1071/AH13066 [DOI] [PubMed] [Google Scholar]
- 23. Gagliardi AR, Perrier L, Webster F, et al. Exploring mentorship as a strategy to build capacity for knowledge translation research and practice: protocol for a qualitative study. Implementation Science 2009;4:1–8. 10.1186/1748-5908-4-55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gagliardi AR, Webster F, Perrier L, et al. Exploring mentorship as a strategy to build capacity for knowledge translation research and practice: a scoping systematic review. Implementation Science 2014;9:1–10. 10.1186/s13012-014-0122-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cooke J. A framework to evaluate research capacity building in health care. BMC Fam Pract 2005;6:44 10.1186/1471-2296-6-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wenke R, Mickan S. The role and impact of research positions within health care settings in allied health: a systematic review. BMC Health Serv Res 2016;16:355 10.1186/s12913-016-1606-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Holden L, Pager S, Golenko X, et al. Evaluating a team-based approach to research capacity building using a matched-pairs study design. BMC Fam Pract 2012;13:1–10. 10.1186/1471-2296-13-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Huber J, Nepal S, Bauer D, et al. Tools and instruments for needs assessment, monitoring and evaluation of health research capacity development activities at the individual and organizational level: a systematic review. Health Res Policy Syst 2015;13:1–17. 10.1186/s12961-015-0070-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Marshall AP, Roberts S, Baker MJ, et al. Survey of research activity among multidisciplinary health professionals. Aust Health Rev 2016:667 10.1071/AH15156 [DOI] [PubMed] [Google Scholar]
- 30. Dobbins M, Robeson P, Ciliska D, et al. A description of a knowledge broker role implemented as part of a randomized controlled trial evaluating three knowledge translation strategies. Implement Sci 2009;4:23 10.1186/1748-5908-4-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ward V, House A, Hamer S. Knowledge Brokering: The missing link in the evidence to action chain? Evid Policy 2009;5:267–79. 10.1332/174426409X463811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ward VL, House AO, Hamer S. Knowledge brokering: exploring the process of transferring knowledge into action. BMC Health Serv Res 2009;9:12 10.1186/1472-6963-9-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ward V, House A, Hamer S. Developing a framework for transferring knowledge into action: a thematic analysis of the literature. J Health Serv Res Policy 2009;14:156–64. 10.1258/jhsrp.2009.008120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ward V, Smith S, House A, et al. Exploring knowledge exchange: a useful framework for practice and policy. Soc Sci Med 2012;74:297–304. 10.1016/j.socscimed.2011.09.021 [DOI] [PubMed] [Google Scholar]
- 35. Bornbaum CC, Kornas K, Peirson L, et al. Exploring the function and effectiveness of knowledge brokers as facilitators of knowledge translation in health-related settings: a systematic review and thematic analysis. Implement Sci 2015;10:162 10.1186/s13012-015-0351-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wenke R. Allied health, reseach activity and capacity. Gold Coast, Australia.: Gold Coast Health, 2014. [Google Scholar]
- 37. Pawson R. Evidence-based policy. a realist perspective. London: Sage Publications., 2006. [Google Scholar]
- 38. Rogers EM. Diffusion of innovations. 4th ed New York: Simon & Schuster., 1995. [Google Scholar]
- 39. Graham ID, Logan J, Harrison MB, et al. Lost in knowledge translation: time for a map? J Contin Educ Health Prof 2006;26:13–24. 10.1002/chp.47 [DOI] [PubMed] [Google Scholar]
- 40. Michie S, Johnston M, Abraham C, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care 2005;14:26–33. 10.1136/qshc.2004.011155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Phillips CJ, Marshall AP, Chaves NJ, et al. Experiences of using the Theoretical Domains Framework across diverse clinical environments: a qualitative study. J Multidiscip Healthc 2015;8:139–46. 10.2147/JMDH.S78458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6:42 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Billett S. Learning in the workplace: Strategies for effective practice. Crows Nest: Allen & Unwin., 2001. [Google Scholar]
- 44. Billett S. Learning through health care work: premises, contributions and practices. Med Educ 2016;50:124–31. 10.1111/medu.12848 [DOI] [PubMed] [Google Scholar]
- 45. Heaton J, Day J, Britten N. Collaborative research and the co-production of knowledge for practice: an illustrative case study. Implement Sci 2016;11:1–10. 10.1186/s13012-016-0383-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Patton MQ. Qualitative research & evaluation methods: integrating theory and practice. Vol. Fourthition. Thousand Oaks, California: SAGE Publications, Inc, 2015. [Google Scholar]
- 47. Holden L, Pager S, Golenko X, et al. Validation of the research capacity and culture (RCC) tool: measuring RCC at individual, team and organisation levels. Aust J Prim Health 2012;18:62–7. 10.1071/PY10081 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-014876supp001.pdf (365.3KB, pdf)