Abstract
OBJECTIVES
Medication errors involving chemotherapy are a serious source of avoidable medical harm that can result in chemotherapy-related adverse drug events. Efforts to reduce errors in the past decade have largely focused on chemotherapy errors at the prescriber level, using computerized or automated technology, but little has been done to ensure chemotherapy is administered accurately at the nursing level. The current study implemented a pharmacist-led, supplemental, institution-specific training program to nursing staff regarding the use of chemotherapy and to address knowledge deficits in newly hired nursing personnel.
METHODS
Inpatient pediatric oncology nurses were eligible to participate in a 3-session educational program regarding chemotherapy principles, adverse event management, and supportive care. Pre- and posttests were administered during the sessions to assess baseline and acquired knowledge. An attitudes survey was given to nurses prior to their first session and after the last session to assess the nurse's comfort with administration and management of chemotherapy.
RESULTS
Posttest scores following program implementation show a significant increase in baseline knowledge. Scores increased by 14.1% (p < 0.001) overall; they increased 6% (p = 0.266), 22% (p = <0.001), and 16.5% (p = <0.001) after sessions 1, 2, and 3, respectively. All respondents requested additional classes for orientation or continuing education.
CONCLUSIONS
A pharmacist-led, educational program significantly improves knowledge of chemotherapy administration and monitoring in pediatric oncology nurses and was well received by participants as an additional training opportunity.
Keywords: chemotherapy, education, nurse, oncology, pediatric, pharmacy
Background
In the wake of significant healthcare change, the media has reflected no shortage of concern for chemotherapy-related errors. Case reports of improper compounding, accidental administration by an improper route, and errors in equipment programming have led to tragic patient outcomes in patients receiving chemotherapy.1–3 A 2007 article stunned the lay media with its conclusion that “most chemotherapy errors reach the patient.” The study reported that 85% of United States Pharmacopoeia MEDMARX database errors affected the patient, the majority arising from improper administration. The authors characterized the potential causes primarily as performance deficits—41.3% of possible error causes—a stark contrast to previously reported data suggesting that errors primarily originate from prescribing.4,5
Efforts to reduce medication errors in the past decade have taken several approaches, beginning with the prescribing process. Computerized prescriber order entry gained immense popularity, with studies5–7 reporting rapid error reduction by 8% to 20%. However, its effect on overall error rates has not been consistently beneficial.8 Studies5,6 have also quantified the benefit of inpatient clinical pharmacy staff on error rates, particularly on the most harmful errors. In 2013, a retrospective audit from the Children's Oncology Group published a report9 indicating that only 0.6% of noted errors had resulted from prescribing, noting that these errors were most likely to be averted by the use of technology and clinical pharmacist services. Of these errors, none were noted to have reached the patient. The benefits of existing services notwithstanding, further error reduction strategies are needed. The authors9 emphasized institution-specific error recognition and intervention and an increased need for a paradigm shift for new error-reduction strategies that encompass a multidisciplinary approach.
It is not surprising that as the efforts to reduce errors in prescribing and dispensing succeed, the greatest source of failure and potential for patient harm remains in chemotherapy administration. Even with the addition of automated dispensing cabinets and barcode verification, there is still significant potential for human error.10 Inappropriate administration and management of medications places patients at risk for significant morbidity and mortality. Risks associated with increased hospital stay, escalation of care, or even death may result from the errors.11,12
In pediatric oncology, nurses remain the point of contact for all involved providers and are crucial in the administration of chemotherapy and in the monitoring of its effects. As the most abundant health professional in the practice area, they must be knowledgeable and clinically competent in their skill set. Because of the complexity of these medications and their adverse event rates, nurses have largely taken responsibility for educating their personnel and implementing safety measures to address issues with chemotherapy administration.13,14
In 2013, the most current consensus recommendations of the Chemotherapy Administration Safety Standards from the American Society of Clinical Oncology and Oncology Nursing Society (ASCO/ONS) were published. These recommendations expanded on the previous inpatient and outpatient standards to include oral chemotherapy, now with a total of 37 standards. The report15 addresses all processes of the medication use system, from prescribing to monitoring and education. However, unlike physician practice in pediatric oncology, which requires several years of recognized residency and fellowship training beyond schooling, and pharmacist practice, which highly encourages residency training and specialized certification, nurse training in pediatric oncology does not currently rely on national standards. Many institutions utilize the Association of Pediatric Hematology/Oncology Nursing (APHON) as a resource for training courses and certification. The chemotherapy certification courses for nurses comprise 2 full days of 12 core modules with associated tests to assess knowledge gained. Comprehensive modules contain large amounts of material, including detailed drug monographs, recall of which is difficult for participants to retain after the end of the course. These programs, though comprehensive in design, are unable to cover institution-specific guidelines and practices that are crucial for a clinical nurse. For nurses without prior experience, the transition to managing patients and their chemotherapy regimens on an oncology unit may be overwhelming.
In order to bridge the gap between an all-encompassing review and clinical competence that comes from experience in the field, this study implemented a multi-part, pharmacist-led educational program to determine its effect on nursing knowledge related to the practical administration and management of chemotherapy. The purpose of the program and study is to evaluate the utility of supplemental, institution-specific training to nursing staff regarding the use of chemotherapy and its supportive care and, additionally, to explore an objective for newly hired nurse orientation.
Methods
All materials, including participants' informed consent, were approved by the organization's institutional review board and office of research administration prior to study commencement. Nursing management and pharmacy personnel collaborated to develop content for the courses. The implementation of the course was conducted over 1 month and was completed by September 2014.
Inclusion into the study required participants to be inpatient pediatric oncology nurses at the host institution; the study population included advanced practice nurses, nursing management, and nurse educators. Nurses were highly encouraged, but not mandated, to attend the program sessions, and their consent to participate in the study portion was optional. Participants were excluded only if they did not meet the above criteria.
In order to provide an atmosphere of trust and security, a unique identification code coordinated with each participant. This code was created by the participant and was known only to the participant (available from the author upon request). This code was intended to accompany all questionnaires and tests, allowing for comparison between sessions, but removing personal identification from the information divulged through these measures.
Design of presentation materials began with a review of relevant educational literature. Objectives for each presentation were formatted to include the 2013 ASCO/ONS Chemotherapy Administration Safety Standards, particularly from the subheadings “Chemotherapy Administration” and “Monitoring and Assessment,” and to supplement information that was taught in the APHON certification course.
The program was implemented in 3 sessions: chemotherapy principles, chemotherapy management, and supportive care. In design, the educational programs addressed 2 primary learning objectives per session. Each of the programs was formatted to fit within a 30-minute window to allow for ease of cross coverage during shifts. The 3 sessions were offered on at least 4 different days and times weekly to accommodate different nursing staff rotations. In total, the program spanned 3 weeks, each week being dedicated to a different session of the program. The primary presenter was a study investigator.
Each session began with a 10-question test, commenced with a 30-minute lecture-based PowerPoint presentation of the materials, and ended with the same 10-question test material that had been used at the beginning of the session. Tests contained multiple-choice questions, including application-based questions. Participants who were new to the course were offered informed consent and a survey of professional demographics and personal attitudes toward activities of a pediatric oncology nurse. Nurses ranked their attitudes on a scale from 1 to 5 based on their level of confidence in the skill. Surveys from before and after each session are available from the author upon request. These activities mirrored the ASCO/ONS Chemotherapy Administration Safety Standards.
Data were analyzed utilizing primarily descriptive statistics. Test scores were expressed in terms of averages and standard deviations. Paired t-tests were used to compare test scores before and after each session.
Results
A total of 30 out of a possible 40 nurses participated in the program, 19 participants (48%) for Part 1, 19 participants (48%) for Part 2, and 12 participants (30%) for Part 3. Participation between the sessions is compared in the Figure; the majority of nurses attended at least 2 sessions. Fifty-five percent (55%) of nurses attended another presentation after the first session and 32% attended another after the second session.
Figure.
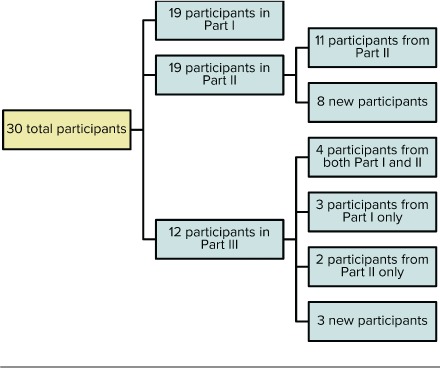
Study participation.
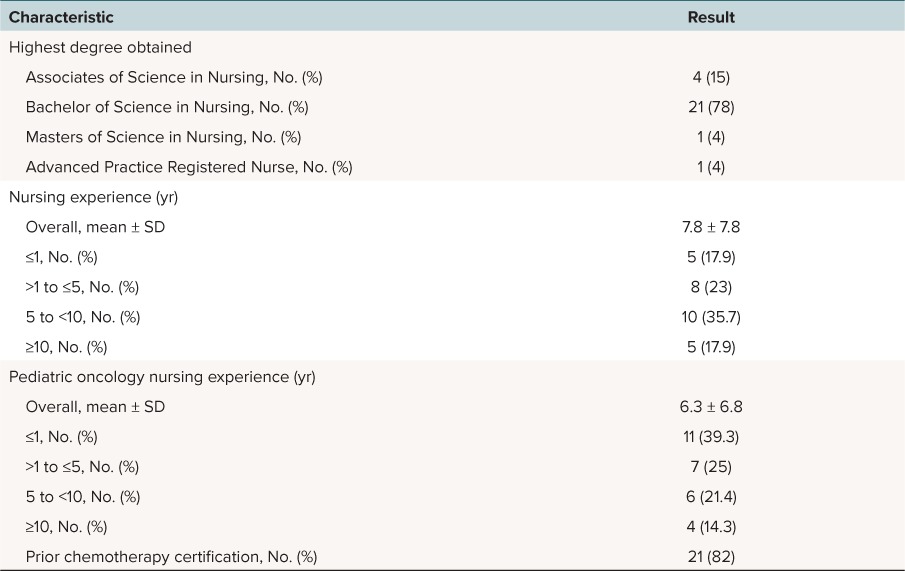
Table 1 summarizes the participant demographics. Seventy-eight percent of participating nurses had Bachelor of Science degrees in nursing training, and 53% had more than 5 years of experience in nursing. Twenty-one nurses reported receiving prior APHON certification, representing 82% of the sample population. However, 39% of participating nurses had less than 1 year of experience in pediatric oncology. Seventeen percent of nurses had less than 1 year of nursing experience in any setting.
Table 1.
Nursing participant demographics
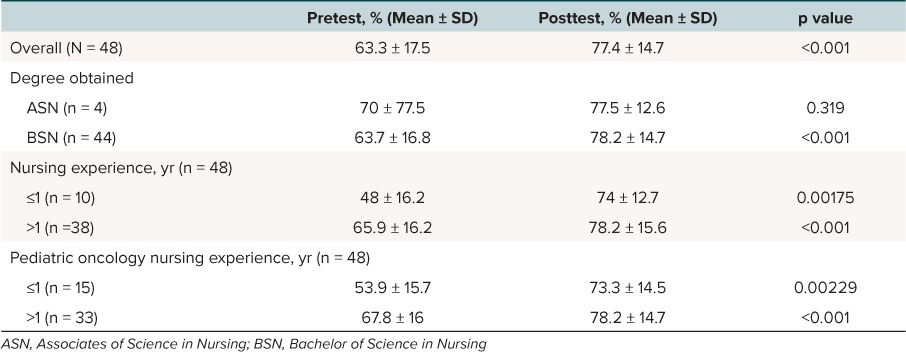
Average posttest scores increased by 14.1% (p < 0.001) overall. Scores from individual sessions increased by 6% (p = 0.266), 22% (p < 0.001), and 16.5% (p < 0.001) for Sessions 1, 2, and 3, respectively (Table 2). Table 3 describes the overall score results from the tests based on demographic differences. There was no apparent difference in posttest scores based on previous nursing experience, but those with previous experience in any setting had better average pretest scores compared to those who had less than 1 year of any nursing experience (48% ± 16.2% and 65.9 ± 16.2%, respectively). Nursing participants with less than 1 year of nursing experience had a greater increase in average test scores compared to those who had worked anywhere longer than 1 year (26% and 12.3%, respectively). Nurses who had not previously worked in pediatric oncology also had a greater increase in average test scores (19.4%) compared to the average (14.1%).
Table 2.
Comparison of individual session pre- and posttest scores
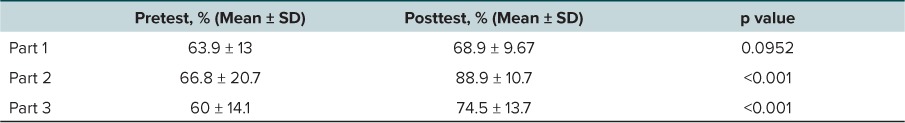
Table 3.
Summative demographic comparison of pre- and posttest scores
An average of 8 chemotherapy-related errors per month occurred in the 6 months leading up to creation and implementation of the educational program. During the implementation of the educational program, error rates decreased to 4 errors per month and remained steady at 4 errors per month in the 6 months following implementation.
Conclusions
As the acuity and complexity of care in pediatric oncology increase, the demand for adequately trained personnel becomes crucial. The present study implemented a pharmacist-led training program to instruct nurses on the management of chemotherapy. The most significant knowledge gap bridged by the program involved knowledge of adverse events associated with commonly used chemotherapy agents. Effects on principles of chemotherapy and supportive care measures were also statistically significant when comparing posttest score results. Overall, feedback provided from the nursing staff was positive and unanimous in terms of the request for additional and continued courses from pharmacy staff.
The first session of chemotherapy education highlighted the principles of oncologic diagnosis and staging, principles of chemotherapy agent use, and interpretation of treatment regimens or “roadmaps.” Nurses were expected to understand the ways in which a patient presented with oncologic disease and the laboratory markers and imaging techniques used to stage a patient's initial disease and response to chemotherapy. A portion of the presentation was also dedicated to family education resources. Nurses were asked 5 questions from a Children's Oncology Group treatment plan, and the majority of missed questions from the first test before and after the presentation were from this section. Several questions required careful reading of the supplied answers as well as the footnotes from the roadmap. When comparing, the relative time discussing roadmaps during the presentation was not equal to the amount of test material on roadmaps. However, the authors felt it was important to test for mastery of this crucial skill, assuming that most nurses would be competent, given their certifications and practice. Not only did this suggest poor baseline understanding of treatment regimens but it also indicated the importance of dedicating more time to this skill set in the future.
The second session expanded on the most commonly used chemotherapy, challenging nurses to recognize and manage the notable adverse effects. There were a total of 12 drugs discussed, each with a list of between 1 and 4 adverse events most commonly associated with it. Significant time was spent discussing the recognition, management, and monitoring for each adverse reaction. For example, methotrexate was described as causing nephrotoxicity, mitigated by the use of aggressive hydration and sodium bicarbonate–containing fluids to prevent damage to the kidneys. Test questions required nurses to match side effects with drugs and to initiate management plans for adverse reactions based on application-based questions. The strategy of presenting fewer drugs but more detailed side effect management was intended to give nurses a chance to make more meaningful connections with the material to prompt long-term memory storage.
The third session specifically highlighted supportive care measures and management of common adverse events associated with the general use of chemotherapy. It discussed management of common oncologic emergencies, extravasation guidelines, antiemetics, and prophylaxis for infections. Tests highlighted drug therapy for each of these areas, and nurses were expected to apply the information to questions with patient scenarios. In this session, the nurses were empowered to recognize the need for drugs such as allopurinol and the relative duration of its use in tumor lysis syndrome. Important institutional guidelines were also emphasized, including the appropriate recognition and initiation of antibiotic treatment of a fever in a patient with neutropenia.
A survey was also given to the nurses as a method of assessing skill level prior to and following the presentations. The nurses were asked to rank their ability to perform tasks similar to the competences listed in the ASCO/ONS guidelines on a scale from 1 to 5 (1 = rarely true, 5 = consistently true). Areas nurses identified as being least independent were identifying errors in patient's orders and answering questions from patients and their families. Overall, nurses' rankings of their abilities trended upward after attending the course.
Unfortunately, many nurses did not complete the survey, so analysis was not performed. All respondents requested additional classes for orientation or continuing education.
While measured knowledge was found to be statistically significant and error rate reduction was seen, the study had several limitations. First, it utilized a small study population and only measured knowledge acquired during each session. With low rates of attendance due to interference with patient care, the knowledge retained and applied from one session to another was not able to be assessed. As a result of time constraints, the longer-term knowledge retention, application of knowledge to nursing practice, and impact on patient safety were not assessed. Error rates were not categorized by prescriber ordering error, pharmacy preparation error, or nursing administration error; therefore, concluding that the educational program is the sole reason for error reduction is not feasible. Time was an unfortunate factor limiting completion of not only the sessions but also the tests. As such, some participants felt that not enough time was allotted for careful reading and selection of the answers. Future educational sessions may be recorded to allow for self-pacing of completion and at-home study.
Continuous quality assurance for program review will ensure that as the program continues it will be updated and will reflect the needs of both the nursing staff and the endpoint of patient safety and quality of care.
Several additional challenges contributing to the external applicability occurred during implementation of the study. The enrollment of nurses and information gathered relied on the ability of nurses to attend the individual sessions. Assistant nurse managers offered coverage for their clinical responsibilities to allow attendance in the programs, but nurses were not required to attend, and not all nurses who were available attended. Sessions at the end of a shift were convenient for the majority of nurses but were not always preferred, particularly for weekend or overnight shifts. Midafternoon sessions were planned during anticipated downtime but had high rates of variability, with patient responsibilities and ease of cross-coverage. The week of the third session in particular was characterized by significantly higher patient volume and acuity, which led to decreased session attendance. Future educational programs offered would be mandatory, scheduled orientation sessions to avoid competition with patient care.
While not the first study to examine the effects of pharmacists' teaching, this is the first known study of its kind to address the needs of pediatric oncology nursing training outside of national certifications. This pilot study demonstrates the ability of a pharmacist-led teaching program to address knowledge gaps that may be a source of potential errors and adverse events related to chemotherapy. Future research and study in this area should be aimed at determining the effects of specific educational techniques on study compliance, administration error avoidance, and management of adverse events.
Acknowledgments
We sincerely thank Elizabeth Reed and Darla York for their support of the education program. Appendices available from corresponding author upon request.
Abbreviations
- APHON
Association of Pediatric Hematology/Oncology Nursing
- ASCO/ONS
American Society of Clinical Oncology and Oncology Nursing Society
- ISMP
Institute for Safe Medication Practices
Footnotes
Disclosure The authors declare no conflicts or financial interest in any product or service mentioned in the manuscript, including grants, equipment, medications, employment, gifts, and honoraria. The authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Copyright Published by the Pediatric Pharmacy Advocacy Group. All rights reserved. For permissions, email: matthew.helms@ppag.org
REFERENCES
- 1. Fernandez CV, Esau R, Hamilton D, . et al. Intrathecal vincristine: an analysis of reasons for recurrent fatal chemotherapeutic error with recommendations for prevention. J Pediatr Hematol Oncol. 1998; 20 6: 587– 590. [DOI] [PubMed] [Google Scholar]
- 2. ISMP Canada. . Fluorouracil incident RCA: follow-up. ISMP Canada Saf Bull. 2007; 7 4: 1– 4. [Google Scholar]
- 3. ISMP. . Criminal prosecution of human error will likely have dangerous long-term consequences. ISMP Medication Safety Alert! 2007; 12 5: 1– 2. [Google Scholar]
- 4. Rinke ML, Shore AD, Kicks RW, Miller MR.. Characteristics of pediatric chemotherapy medication errors in a national error reporting database. Cancer. 2007; 110 1: 186– 195. [DOI] [PubMed] [Google Scholar]
- 5. Fortescue EB, Kaushal R, Landrigan CP, . et al. Prioritizing strategies for preventing medication errors and adverse drug events in pediatric inpatients. Pediatrics. 2003; 111 1: 722– 729. [DOI] [PubMed] [Google Scholar]
- 6. Wang JK, Herzog NS, Kaushal R, . et al. Prevention of pediatric medication errors by hospital pharmacists and the potential benefit of computerized physician order entry. Pediatrics. 2007; 119 1: e77– e85. [DOI] [PubMed] [Google Scholar]
- 7. Conroy S, Sweis D, Planner C, . et al. Interventions to reduce dosing errors in children: a systematic review of the literature. Drug Saf. 2007; 30 12: 1111– 1125. [DOI] [PubMed] [Google Scholar]
- 8. Walsh KE, Landrigan CP, Adams WG, . et al. Effect of computerized order entry on prevention of serious medication errors in hospitalized children. Pediatrics. 2008; 121 3: e421– e427. [DOI] [PubMed] [Google Scholar]
- 9. Watts RG, Parsons K.. Chemotherapy medication errors in a pediatric cancer treatment center: prospective characterization of error types and frequency and development of a quality improvement initiative to lower the error rate. Pediatr Blood Cancer. 2013; 60 8: 1320– 1324. [DOI] [PubMed] [Google Scholar]
- 10. Kuiper SA, McCreadie SR, Mitchell JF, . et al. Medication errors in inpatient pharmacy operations and technologies for improvement. Am J Health-Syst Pharm. 2007; 64 9: 955– 959. [DOI] [PubMed] [Google Scholar]
- 11. Holdsworth MT, Fichtl RE, Behta M, . et al. Incidence and impact of adverse drug events in pediatric inpatients. Arch Pediatr Adolesc Med. 2003; 157 1: 60– 65. [DOI] [PubMed] [Google Scholar]
- 12. Kaushal R, Bates DW, Landrigan C, . et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001; 285 16: 2114– 2120. [DOI] [PubMed] [Google Scholar]
- 13. Niemann D, Bertsche A, Meyrath D, . et al. A prospective three-step intervention study to prevent medication errors in drug handling in paediatric care. J Clin Nurs. 2015; 24 1–2: 101– 114. [DOI] [PubMed] [Google Scholar]
- 14. Fessele K, Yendro S, Mallory G.. Setting the bar: developing quality measures and education programs to define evidence-based, patient-centered, high-quality care. Clin J Oncol Nurs. 2014; 18 suppl: 7– 11. [DOI] [PubMed] [Google Scholar]
- 15. Neuss MN, Polovich M, McNuff K, . et al. 2013 Updated American Society of Clinical Oncology/Oncology Nursing Society chemotherapy administration safety standards including standards for the safe administration and management of oral chemotherapy. J Oncol Pract. 2013; 9 suppl 2: 5s– 13s. [DOI] [PMC free article] [PubMed] [Google Scholar]


