Abstract
Introduction: The number of HIV-infected children and adolescents requiring second-line antiretroviral treatment (ART) is increasing in low- and middle-income countries (LMIC). However, the effectiveness of paediatric second-line ART and potential risk factors for virologic failure are poorly characterized. We performed an aggregate analysis of second-line ART outcomes for children and assessed the need for paediatric third-line ART.
Methods: We performed a multicentre analysis by systematically reviewing the literature to identify cohorts of children and adolescents receiving second-line ART in LMIC, contacting the corresponding study groups and including patient-level data on virologic and clinical outcomes. Kaplan–Meier survival estimates and Cox proportional hazard models were used to describe cumulative rates and predictors of virologic failure. Virologic failure was defined as two consecutive viral load measurements >1000 copies/ml after at least six months of second-line treatment.
Results: We included 12 cohorts representing 928 children on second-line protease inhibitor (PI)-based ART in 14 countries in Asia and sub-Saharan Africa. After 24 months, 16.4% (95% confidence interval (CI): 13.9–19.4) of children experienced virologic failure. Adolescents (10–18 years) had failure rates of 14.5 (95% CI 11.9–17.6) per 100 person-years compared to 4.5 (95% CI 3.4–5.8) for younger children (3–9 years). Risk factors for virologic failure were adolescence (adjusted hazard ratio [aHR] 3.93, p < 0.001) and short duration of first-line ART before treatment switch (aHR 0.64 and 0.53, p = 0.008, for 24–48 months and >48 months, respectively, compared to <24 months).
Conclusions: In LMIC, paediatric PI-based second-line ART was associated with relatively low virologic failure rates. However, adolescents showed exceptionally poor virologic outcomes in LMIC, and optimizing their HIV care requires urgent attention. In addition, 16% of children and adolescents failed PI-based treatment and will require integrase inhibitors to construct salvage regimens. These drugs are currently not available in LMIC.
Keywords: antiretroviral treatment, children, adolescents, virologic failure, HIV-1, second-line treatment
Introduction
Worldwide, the number of HIV-infected children receiving antiretroviral treatment (ART) has more than doubled since 2010 to an estimated 823,000 in 2014 [1]. In low- and middle-income countries (LMIC), 97% of children on ART are on first-line treatment, and only 3% receives second-line ART [2]. However, with the increasing paediatric ART coverage in LMIC [1], the number of children failing first-line and requiring second-line options will rise.
Currently, the World Health Organization (WHO) recommends that HIV-infected children three years or older of age start non-nucleoside reverse-transcriptase inhibitor (NNRTI)-based ART as a first-line regimen and to switch to a protease inhibitor (PI)-based second-line regimen in case of treatment failure. Children younger than three years are advised to start PI-based first-line ART [3]. As PI-based treatment is costly and logistically challenging, local clinics might still prefer to start an NNRTI-based regimen as first-line ART in young children. Moreover, due to late diagnosis and linkage to care, perinatally HIV-infected children may only start ART after the age of three years [4–6]. As a consequence, 56% of children in LMIC still receive a nevirapine-based first-line regimen and switch to PI-based ART in case of failure [7]. Children have higher rates of first-line ART failure compared to adults [8–11]. The population of HIV-infected adolescents is growing as perinatally infected children now survive until adulthood, and HIV treatment in adolescents is especially challenging [12–14].
In order to ensure adequate long-term treatment for children and adolescents, evaluation of current second-line treatment outcomes is essential. Data, however, are scarce [15], and the available studies have small sample sizes, use different definitions of virologic failure and have different follow-up periods [16–19]. Therefore, it is hard to compare results across different cohorts. In adults, multicentre studies and meta-analyses of second-line ART have been conducted [15,20], but such analyses are missing for children. We performed a multicentre analysis of children and adolescents in LMIC to assess second-line treatment outcomes, describing the rate of virologic failure and identifying its predictors. In this way, we evaluated the effectiveness of second-line ART and estimated the need for third-line regimens.
Methods
We conducted a systematic review of the literature according to PRISMA guidelines [21] to identify cohorts of children receiving second-line ART in LMIC. We systematically searched the literature in Medline through PubMed, Embase, the Literatura Latino Americana de Ciencias de Salud and the African Index Medicus, as well as conference abstracts of the International AIDS Society, the Conference on Retroviruses and Opportunistic Infections and the HIV Pediatric Workshops of 2014 and 2015 to identify second-line cohorts whose results had not yet been published. The complete search strategy for published articles is provided in Supplementary Table S1. For conference abstracts, we used the search term “second-line” or “treatment-experienced”.
Study selection
We searched for cohort studies, cross-sectional studies and randomized controlled trials reporting second-line virologic treatment outcomes of children and adolescents living in LMIC (according to the World Bank 2016 definition [22]). Studies were eligible if they reported on at least five children on a PI-based second-line regimen. Within each eligible study, we further excluded: children aged <3 years or >18 years at switch to second-line ART; children who had received less than six months of first-line ART before switching; children who had received a first-line regimen not containing an NNRTI; children having either a first- or a second-line regimen consisting of dual therapy or monotherapy; and children without any viral load (VL) results during the first five years of second-line ART. In order to create a homogeneous group of participants, we selected only children on ritonavir-boosted lopinavir (LPV/r)-based ART, reflecting the 2013 WHO guidelines on paediatric second-line ART [23]. Because of the various changes in treatment guidelines for children younger than three years (from NNRTI-based first-line and PI-based second-line in 2010 to PI-based first-line and raltegravir-based second-line in 2016 [3,23,24]), we included only participants older than three years of age.
Studies were selected independently by two reviewers, and any disagreement was resolved by discussion between both. The authors of eligible articles were approached by email with a request to share the patient-level data of their cohort. If the study group agreed to share data, a data-sharing agreement was signed by both parties. Anonymized data sets were shared by email and were collected in one central database. If different study groups had included participants from the same study sites, we checked with the corresponding authors that none of the participants were included in our data set twice. Only the first author had direct access to all data in order to maintain confidentiality.
Data management
Data sets were provided by the corresponding authors in Stata®, SPSS® or Excel® format. The following variables were requested: sex; age at switch; calendar year at switch; country of residence; duration of first-line ART; drugs used in first-line regimen; reason for switching to second-line ART; drugs used in second-line regimen; VL, CD4 count/CD4 percentage and WHO/CDC (Centers for Disease Control and Prevention) HIV stage at switch; VL during follow-up and period between switch and VL measurement; status at moment of censoring (in care, dead, lost to follow-up, transferred out); and date of end of study. In order to compare CD4 count and CD4 percentages in different age groups, we constructed a variable, called CD4 status, defined as: normal - CD4 count >500 (for children five years or older) or CD4% >25 (for children younger than five years); diminished, CD4 count 100–500 (for children five years or older) or CD4% 10–25% (for children less than five years); and immunodeficient, CD4 count <100 (for children five years or older) or CD4% <10% (for children younger than five years).
Risk of bias assessment
To assess the potential risk of bias in each cohort, we developed a list of five criteria relevant for this analysis, based on existing checklists of the Newcastle Ottowa Scale [25], the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) [26] and the Cochrane Collaboration tool for assessing the risk of bias [27]. For each criterion, a study could score 1 if the criterion was met and 0 if the criterion was not met or not reported. Each cohort could obtain a maximum score of 5. Cohorts with a score of ≥4 were considered to have a lower risk of bias and below 4 a higher risk. Criteria and scores of each study are provided in Supplementary Table S2.
Data analysis
We defined young children as individuals aged nine years or younger and adolescents as individuals aged 10–18 years at switch. Baseline characteristics of young children and adolescents were described using counts and percentages or medians and interquartile ranges (IQRs). We did not use multiple imputation to adjust for missing data if these data were missing at the cohort level. For categorical variables, we added a “missing” category for individuals with missing data for that variable. Kaplan–Meier survival analysis was used to assess the cumulative incidence of virologic failure overall and separately for younger children and adolescents. Difference in virologic failure rates between groups was assessed using a log-rank test. In the primary analysis, we defined virologic failure according to the WHO definition of two consecutive VL measurements >1000 copies/ml after at least six months of second-line ART [3]. As not all studies used a second confirmatory VL measurement to define failure, we conducted a secondary analysis in which we defined failure as a single VL >1000 copies/ml after at least six months of second-line ART. Associations between virologic failure and age, sex, time spent on first-line ART, calendar year of switch and VL and CD4 count/percentage at switch were assessed using a Cox proportional hazard model, clustered by study cohort and by number of VL results per child (<5 results, 5–15 results and >15 results). Variables associated with failure at p < 0.10 in the univariable analysis and clinically relevant variables were added to the multivariable model. We checked for collinearity by calculating the variance inflation factor. The proportional hazard assumption was tested by calculating Schoenfeld residuals. To test for the robustness of our data, we conducted three sensitivity analyses in which we only included children in sub-Saharan Africa, only children with known VL and CD4 count/percentage results at switch to second-line ART or only studies with a perceived lower risk of bias. A two-sided p-value of ≤0.05 was considered significant. Data were analysed using Stata 12® (StataCorp LP, College Station, TX, USA).
Ethics
All included study cohorts obtained ethical clearance from their local ethical committee. All studies have been conducted in compliance with Good Clinical Practice guidelines and the principles of the Declaration of Helsinki. All participants in the included study cohorts provided informed consent to participate in the corresponding studies.
Results
Search
Our search strategy retrieved a total of 370 articles of which 340 articles were excluded. Of 371 retrieved conference abstracts, 367 abstracts were excluded. Main reasons for exclusion were not concerning second-line treatment, inclusion of adults rather than children or not reporting virologic treatment outcomes. Thirty articles and four abstracts were eligible for inclusion. The four abstracts all represented published articles, and these articles were already part of the 30 articles retrieved by our literature search. After full text screening of the remaining articles, 21 authors were contacted to participate which resulted in 12 contributing data sets (Figure 1).
Figure 1.
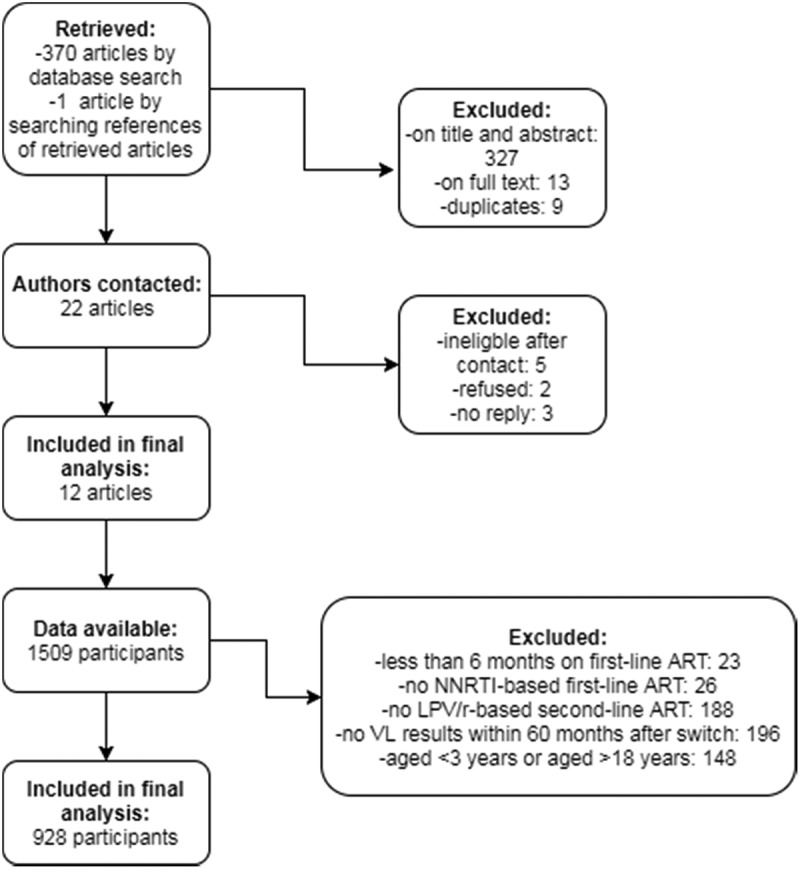
Flow chart of study and participant selection.
NNRTI: non-nucleoside reverse-transcriptase inhibitor; LPV/r: ritonavir-boosted lopinavir; VL: viral load.
Characteristics of included studies
The 12 remaining cohorts represent 928 children receiving LPV/r-based second-line ART in 14 countries in Asia and sub-Saharan Africa. Characteristics of children included are shown in Table 1, and study characteristics are described in Supplementary Table S3. Median age at switch was 9.0 years (IQR 6.1–12.0). Fifty-six children (6.0%) were enrolled in a randomized controlled trial, and all other children were included in observational cohort studies. Median time on first-line ART prior to switch was 36.0 months (IQR 21.6–51.6). The most common first-line regimen was zidovudine/lamivudine/nevirapine (AZT/3TC/NVP) in 235 children (25.8%), and the most common second-line regimen was AZT/3TC/LPV/r in 194 children (21.3%). A median of three VL results (IQR 2–6) per individual were reported during follow-up (for children: 3 (IQR 2–6), for adolescents: 4 (IQR 2–7)). At the time of censoring, 717 (77.3%) children were in care and on treatment, 20 (2.2%) were lost to follow-up, 24 (2.6%) had died, 72 (7.8%) had transferred out and for 95 (10.2%) children the status at end of follow-up was not recorded. Of all young children, 436/480 (90.8%) were still in care and on treatment at censoring compared to 281/353 (79.6%) of adolescents, p < 0.001 (χ2 test).
Table 1.
Characteristics of children and adolescents included in the multicentre analysis
| Children (3–9 years old) |
Adolescents (10–18 years old) |
Total |
|||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Total | 532 | 100 | 396 | 100 | 928 | 100 | |
| Region | Sub-Saharan Africa | 220 | 41.4 | 160 | 40.4 | 380 | 40.9 |
| Asia | 312 | 58.6 | 236 | 59.6 | 548 | 59.1 | |
| Calendar year of treatment switch | 2003–2007 | 52 | 9.8 | 18 | 4.5 | 70 | 7.5 |
| 2008–2010 | 369 | 69.4 | 278 | 70.2 | 647 | 69.7 | |
| 2011–2014 | 111 | 20.9 | 100 | 25.3 | 211 | 22.7 | |
| Gender | Boys | 307 | 57.7 | 185 | 46.7 | 492 | 53.0 |
| Girls | 225 | 42.3 | 211 | 53.3 | 436 | 47.0 | |
| Viral load at switch (copies/ml) | <1000 | 15 | 2.8 | 22 | 5.6 | 37 | 4.0 |
| 1000–10,000 | 74 | 13.9 | 52 | 13.1 | 126 | 13.6 | |
| 10,000–100,000 | 125 | 23.5 | 90 | 22.7 | 215 | 23.2 | |
| >100,000 | 121 | 22.7 | 58 | 14.6 | 179 | 19.3 | |
| Not available | 197 | 37.0 | 174 | 43.9 | 371 | 40.0 | |
| CD4 status at switcha | Normal | 129 | 24.2 | 51 | 12.9 | 180 | 19.4 |
| Diminished | 122 | 22.9 | 117 | 29.5 | 239 | 25.8 | |
| Immunodeficient | 44 | 8.3 | 52 | 13.1 | 96 | 10.3 | |
| Not available | 237 | 44.5 | 176 | 44.4 | 413 | 44.5 | |
| Duration of first-line antiretroviral treatment | <24 months | 190 | 35.7 | 75 | 18.9 | 265 | 28.6 |
| 24–48 months | 219 | 41.2 | 158 | 39.9 | 377 | 40.6 | |
| >48 months | 122 | 22.9 | 162 | 40.9 | 284 | 30.6 | |
| Not available | 1 | 0.2 | 1 | 0.3 | 2 | 0.2 | |
aNormal: CD4 count >500 or CD4% >25; diminished: CD4 count 100–500 or CD4% 10–25%; immunodeficient: CD4 count <100 or CD4% <10%. Status is based on CD4% for children younger than five years and on CD4 count for children five years or older.
Virologic failure
Of the 928 children on second-line PI-based ART, 722 (77.8%) children had at least two VL results during follow-up, were still in care and on treatment after six months of second-line ART and were included in the primary analysis (virologic failure defined as two consecutive VL >1000 copies/ml). Over a total follow-up time of 1882 person-years, 154 children experienced virologic failure, resulting in a failure rate of 8.2 (95% CI 7.0–9.6) per 100 person-years. After 12, 24 and 60 months, failure rates were 10.0% (95% CI 8.0–12.5), 16.4% (95% CI 13.9–19.4) and 25.3% (95% CI 21.7–29.2), respectively. In children, the failure rate was 4.5 (95% CI 3.4–5.8) and in adolescents 14.5 (95% CI 11.9–17.6) per 100 person-years. After 24 months, 9.1% (95% CI 6.6–12.4) of younger children and 26.3% (95% CI 21.7–31.8) of adolescents had experienced virologic failure, p < 0.001 (Figure 2(a)). For children from sub-Saharan Africa, the failure rate was 6.7 (95% CI 4.9–9.1) per 100 person-years and for children from Asia 8.9 (95% CI 7.4–10.6) per 100 persons-years.
Figure 2.
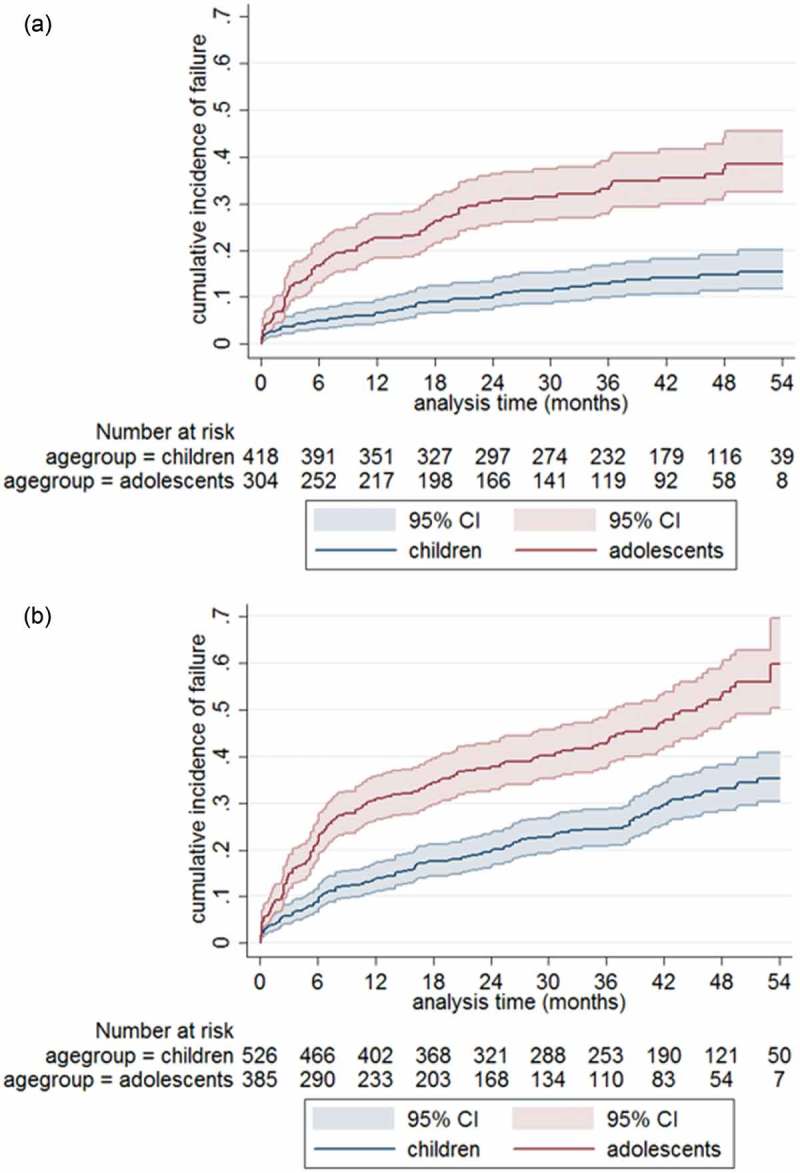
(a, b) Cumulative incidence of virologic failure among children and adolescents on second-line treatment. (a) Primary analysis and (b) secondary analysis.
Virologic failure in the primary analysis is defined as two consecutive VL results >1000 copies/ml after at least six months of second-line treatment (n = 722) and in the secondary analysis as a single VL >1000 copies/ml after at least six months of second-line treatment (n = 911). T0 is set at six months after treatment switch; total follow-up time is 60 months.
Out of 928 children, 911 (98.2%) children had at least one VL result, were still in care and on treatment after six months of second-line ART and were included in the secondary analysis (virologic failure defined as a single VL >1000 copies/ml). Over a total follow-up time of 2058 person-years, 307 children experienced virologic failure, resulting in a failure rate of 14.9 (95% CI 13.3–16.7) per 100 person-years. After 24 months, 17.5% (95% CI 14.4–21.2) of young children and 34.4% (95% CI 29.7–39.5) of adolescents failed, p < 0.001 (Figure 2(b)).
Predictors of virologic failure
In a multivariable analysis, adolescents had a higher risk of virologic failure compared to younger children (adjusted hazard ratio (aHR) 3.93 (95% CI 2.67–5.78), p < 0.001). Children who had spent more time on first-line ART had a lower risk: compared to <24 months of first-line ART, the aHR was 0.64 (95% CI 0.42–0.96), p = 0.032, for those on first-line ART for 24–48 months, and 0.53 (95% CI 0.33–0.85), p = 0.008, for those on first-line ART for >48 months. Sex, calendar year of switch, VL and CD4 status at switch were not associated with virologic failure (Table 2). Adolescence was the only factor associated with virologic failure in three sensitivity analyses, with an aHR of 3.08 (95% CI 1.35–7.02, p = 0.007) for children in sub-Saharan Africa only, an aHR of 5.11 (95% CI 2.66–9.82, p < 0.001) for children with a known VL and CD4 status at switch and an aHR of 4.32 (95% CI 1.69–11.04, p = 0.002) for children in studies with a perceived lower risk of bias (Supplementary Table S4).
Table 2.
Factors associated with second-line virologic failure
| Univariable model |
Multivariable model |
|||||
|---|---|---|---|---|---|---|
| Failure rate per 100 person-years (95% CI) | Hazard ratio | p | Adjusted hazard ratio | p | ||
| Age group | Children | 4.5 (3.4–5.8) | 1 | 1 | ||
| Adolescents | 14.5 (11.9–17.6) | 2.98 (2.10–4.22) | <0.001 | 3.93 (2.67–5.78) | <0.001 | |
| Gender | Boy | 7.5 (6.0–9.3) | 1 | 1 | ||
| Girl | 9.0 (7.2–11.3) | 1.18 (0.85–1.62) | 0.325 | 1.01 (0.72–1.41) | 0.949 | |
| Time on first-line ART | <24 months | 9.2 (6.9–12.5) | 1 | 1 | ||
| 24–48 months | 7.7 (6.0–9.8) | 0.75 (0.50–1.12) | 0.159 | 0.64 (0.42–0.96) | 0.032 | |
| >48 months | 8.2 (6.1–10.9) | 0.72 (0.46–1.11) | 0.136 | 0.53 (0.33–0.85) | 0.008 | |
| Calendar year (continuous) | 0.97 (0.87–1.08) | 0.607 | 0.99 (0.89–1.11) | 0.896 | ||
| Viral load at switch (copies/ml) | <1000 | 11.7 (4.9–28.2) | 1 | 1 | ||
| 1000–10,000 | 5.2 (2.9–9.4) | 0.52 (0.18–1.54) | 0.240 | 0.49 (0.16–1.47) | 0.203 | |
| 10,000–100,000 | 8.6 (6.1–12.1) | 0.81 (0.31–2.13) | 0.675 | 0.92 (0.34–2.51) | 0.877 | |
| >100.000 | 11.0 (7.8–15.5) | 0.94 (0.36–2.48) | 0.902 | 1.18 (0.42–3.33) | 0.757 | |
| Not available | 7.6 (6.1–9.6) | |||||
| CD4 status at switcha | Normal | 5.4 (3.4–8.6) | 1 | |||
| Diminished | 9.8 (7.2–13.3) | 1.52 (0.87–2.65) | 0.144 | 1.08 (0.60–1.97) | 0.791 | |
| Immunodeficient | 14.9 (10.0–22.2) | 2.19 (1.12–4.26) | 0.022 | 1.51 (0.72–3.18) | 0.280 | |
| Not available | 7.3 (5.8–9.2) |
Virologic failure is defined as two consecutive viral load results >1000 copies/ml after at least six months of second-line ART. Cox regression model is stratified by number of VL results per child and by study cohort. Age, calendar year, viral load and CD4 status are at moment of treatment switch.
aNormal: CD4 count >500 or CD4% >25; diminished: CD4 count 100–500 or CD4% 10–25%; immunodeficient: CD4 count <100 or CD4% <10%. Status is based on CD4% for children younger than five years and on CD4 count for children five years or older.
95% CI: 95% confidence interval; ART: antiretroviral treatment.
Discussion
The rate of virologic failure among children on second-line PI-based ART after failure of first-line NNRTI-based ART was 8.2 per 100 person-years, with 16.4% of children experiencing virologic failure within 24 months. Adolescents were almost four times more likely to experience virologic failure on second-line ART compared to younger children.
In the first two years of PI-based second-line ART, 16% of children experienced virologic failure. In a secondary analysis using a single VL measurement to define virologic failure, 25% failed. These outcomes are better than the pooled estimates of 60–75% of children achieving viral suppression in the first two years of first-line ART [11], which might reflect the higher potency and the higher “forgiveness of non-adherence” attributed to PIs compared to NNRTIs (mainly used in first-line regimens within LMIC). Moreover, a child’s or caregiver’s improved motivation to adhere to treatment after failure of first-line treatment might also play a role. Finally, the risk of pretreatment HIV drug resistance (HIVDR) towards NNRTIs is typically higher than resistance towards PIs, especially after exposure to drugs for the prevention of mother-to-child transmission [28,29].
Our results are comparable to outcomes of adults on second-line ART in LMIC. In a study among adults in 12 Asian countries, the failure rate was 8.8 per 100 patient-years [20]. A large cohort study in six African countries among adults on second-line ART found that 15% experienced virologic failure after two years [30]. When only looking at the subgroup of younger children in our study, outcomes are even better than adult results, as the failure rate was 4.5 per 100 patient-years and 9.1% failed after two years. This again underscores the necessity for increasing virologic monitoring as children grow older.
Adolescent age was the strongest predictor of virologic failure. This finding was robust across several sensitivity analyses. This result is in line with previous paediatric studies which also identified adolescents to be at increased risk of treatment failure on first- and second-line ART [17,18,31,32]. Studies on treatment outcomes of adolescents living with HIV in LMIC are scarce, but the available data are worrisome. In sub-Saharan Africa, HIV is the leading cause of mortality in adolescents [33]. While the number of AIDS-related deaths worldwide decreased by 24% between 2004 and 2011, mortality increased by 50% among adolescents over the same time period [13]. The observation that perinatally infected children are now surviving into adolescence due to the large-scale introduction of ART is an enormous achievement. However, the poor treatment outcomes of these children once they reach adolescence call for increased attention for this age group, not only to prevent HIV-related morbidity and mortality but also to decrease the risk of HIV transmission in sexually active adolescents. Treatment of adolescents is known to be challenging because of physical, psychological and social changes in an adolescent’s life and the transition from paediatric into adult HIV care [12,14,34,35]. Strategies to retain adolescents in care and to improve treatment adherence need to be explored further and might include adherence clubs, mobile health technologies, support in dealing with stigma, weekends-off regimens, conditional cash incentives and training in life skills and problem-solving [12,13,36,37].
Children who spent more time on first-line ART had a lower risk of virological failure. This could be explained by the assumption that children who had been on first-line ART for a long time are possibly more adherent to treatment. Therefore, the risk of second-line failure is lower for these children. The association did not reach significance in sensitivity analyses.
It is reassuring to note that children who fail first-line NNRTI-based treatment still have a good chance of re-suppressing on LPV/r-based second-line ART. However, given that WHO guidelines have recommended PI regimens as first line for young children since 2013 [23], it is concerning that hardly any data exist on outcomes of children who have failed PI-based first line and need to be switched to second-line ART. In our literature search, we identified reports of only 30 children on second-line treatment after failure of a PI-based first-line regimen, indicating that this is a profoundly understudied topic.
The most recent WHO guidelines recommend the use of a raltegravir-based regimen as a second-line option after failure of first-line LPV/r-based ART in children younger than three years and the use of either raltegravir or efavirenz in children three years or older. Children failing second-line PI-based ART are advised to start raltegravir, darunavir or dolutegravir plus two nucleoside reverse transcriptase inhibitors as a salvage regimen [3]. However, despite recent Medicines Patent Pool licensing agreements allowing royalty-free manufacturing for sale in LMIC [38], these drugs are hardly available in programmatic settings in LMIC [23,39–41]. For children failing PI-based treatment (either as a first line for young children or as a second line for older children), treatment options are therefore still very limited.
Unfortunately, most cohorts included in this analysis did not perform genotypic HIVDR testing in children failing second-line ART. To our knowledge, only two published cohort studies in Asia described HIVDR patterns in a cohort of children on second-line ART. These reported relatively low rates of PI resistance of 11.3% and 8.0% in children failing second line [18,32]. In a cohort of 64 children on second line in Uganda, no PI mutations were detected after failure [42]. Studies among adults on second-line ART confirm that failure is driven mainly by non-adherence and not by PI resistance. Nevertheless, if adherence is suboptimal over longer periods of time, PI mutations will eventually develop [43–45].
One of the major strengths of this study is the fact that this is the largest analysis of paediatric outcomes on second-line ART in LMIC to date, combining data from both Asia and sub-Saharan Africa. Our results confirm the findings of previous smaller studies, showing that failure rates are relatively favourable for children, but worryingly high for adolescents. Our study also has some potential limitations. First, this was a multicentre analysis in which treatment protocols and the availability of data differed by study site. Therefore, the data used in this analysis are heterogeneous, and this heterogeneity should be kept in mind when interpreting the results. We attempted to minimize the influence of this heterogeneity by clustering our analysis by study cohort, by conducting a secondary analysis of the incidence of virological failure and by conducting various sensitivity analyses.
Second, by definition, a child could only be classified as experiencing failure when a VL result was available. A child with more VL results, therefore, had more chance to be classified as experiencing virologic failure, creating a bias towards more virological failure at study sites with more frequent VL monitoring. To correct for this, we stratified our Cox model for different number of VL measurements per child. It is striking to note that, even in controlled research settings, important clinical data such as VL and CD4 count are missing for a large proportion of children. To improve clinical outcomes of children on ART, intensified treatment monitoring is essential.
Third, some potentially relevant variables were not included in our analysis such as adherence, HIVDR, ART regimen and clinical status because not all studies had collected these data or because data were too heterogeneous to include.
Fourth, some cohorts we approached for this analysis either did not reply to our request or could not share their data. This might have created a bias in our analysis.
Finally, our study concerns children on second-line PI-based ART after failure of an NNRTI-based first-line regimen, which is not currently the recommended ART sequence for young children. However, since PI-based first-line treatment has not yet been widely implemented in LMIC and given that many children are only diagnosed with HIV after the age of three years, our data are applicable to the large number of HIV-infected children who will still receive NNRTI-based first-line ART. If we would have included children in our analysis on other second-line regimens, such as NNRTI-based second-line ART, the rate of virologic suppression we found might have been lower, given the poor results of NNRTI-based second-line ART found in studies in South Africa [46,47].
Conclusions
In conclusion, this multicentre analysis shows that treatment outcomes of children on second-line PI-based ART are encouraging with 16% experiencing virologic failure in the first two years. However, for the 16% who fail second-line ART, integrase inhibitors, which are currently not available in LMIC, are needed to construct salvage regimens. Data on second-line treatment outcomes after failure of a PI-based regimen are hardly available and therefore urgently needed. The poor outcomes of adolescents compared to younger children underscore the difficulties of adolescent HIV care and call for increased attention for this vulnerable population as they transition into adulthood.
Acknowledgements
We would like to thank all children and adolescents and their caregivers, who participated in the included cohorts, as well as the study teams of all study cohorts. We also thank René Spijker for librarian assistance and Maura de Groot for assistance with the literature search and study selection. This work was supported by internal funding.
Biography
RSB conducted the literature review, contacted study groups, collected all patient-level data, conducted the analyses and wrote the first draft of the paper. TFRdW, JCJC and KCES supervised the reviewing and analysis process. TB, DD, JF, AK, DL, CK, VM, PP, AS, SS and BZ are the coordinating researchers of the study cohorts included in the analysis. All authors participated in discussion of the results of the analysis and in writing of the final paper. All authors have read and approved the final version.
Competing interests
None to declare.
References
- 1. World Health Organization Global health sector response to HIV, 2000–2015: focus on innovations in Africa: progress report [Internet]. 2015. [cited 2016 September5] Available from: http://www.who.int/hiv/pub/progressreports/2015-progress-report/en/
- 2. World Health Organization Global HIV/AIDS response. Epidemic update and health sector progress towards Universal Access [Internet]. 2011. [cited 2016 September6] Available from: http://www.who.int/hiv/pub/progress_report2011/en/
- 3. World Health Organization Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach - Second Edition 2016 [Internet]. 2016. [cited 2016 September6] Available from: http://www.who.int/hiv/pub/arv/arv-2016/en/ [PubMed]
- 4. Naiwatanakul T, Voramongkol N, Punsuwan N, Lolekha R, Gass R, Thaisri H, et al. Uptake of early infant diagnosis in Thailand ’ s national program for preventing mother-to-child HIV transmission and linkage to care, 2008–2011. J Int AIDS Soc. 2016;19:20511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Amorissani-Folquet M, Coulibaly M, Avit-Edi D, Meda N, Timite-Konan M, Arendt V, et al. Missed opportunities of inclusion in a cohort of HIV-infected children to initiate antiretroviral treatment before the age of two in West Africa, 2011 to 2013. J Int AIDS Soc. 2016;19:20601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhang N, Bussell S, Wang G, Zhu X, Yang X, Tao H, et al. Disparities in HIV care along the path from infection to viral suppression: a cross-sectional study of HIV/AIDS patient records in 2013, Shandong Province, China. Clin Infect Dis. 2016;63(1):115–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization (WHO) WHO survey 2015. Geneva (Switzerland): WHO; 2015. [Google Scholar]
- 8. Jobanputra K, Parker LA, Azih C, Okello V, Maphalala G, Kershberger B, et al. Factors associated with virological failure and suppression after enhanced adherence counselling, in children, adolescents and adults on antiretroviral therapy for HIV in Swaziland. PLoS One. 2015;10(2):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kamya MR, Mayanja-Kizza H, Kambugu A, Bakeera-Kitaka S, Semitala F, Mwebaze-Songa P, et al. Predictors of long-term viral failure among Ugandan children and adults treated with antiretroviral therapy. J Acquir Immune Defic Syndr. 2007. October 1;46(2):187–93. [DOI] [PubMed] [Google Scholar]
- 10. Boender TS, Sigaloff KCE, Mcmahon JH, Kiertiburanakul S, Jordan MR, Barcarolo J, et al. Long-term virological outcomes of first-line antiretroviral therapy for HIV-1 in low- and middle-income countries: a systematic review and meta-analysis. Clin Infect Dis. 2015;61(9):1453–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Boerma RS, Boender TS, Boele van Hensbroek M, Rinke de Wit TF, Sigaloff KCE.. Sequencing paediatric antiretroviral therapy in the context of a public health approach. J Int AIDS Soc. 2015;18(Suppl 5):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lowenthal ED, Bakeera-Kitaka S, Marukutira T, Chapman J, Goldrath K, Ferrand RA. Perinatally acquired HIV infection in adolescents from sub-Saharan Africa: a review of emerging challenges. Lancet Infect Dis. 2014;14(7):627–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kasedde S, Luo C, McClure C, Chandan U. Reducing HIV and AIDS in adolescents: opportunities and challenges. Curr HIV/AIDS Rep. 2013;10(2):159–68. [DOI] [PubMed] [Google Scholar]
- 14. Mofenson LM, Cotton MF. The challenges of success: adolescents with perinatal HIV infection. J Int AIDS Soc. 2013;16:18650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ajose O, Mookerjee S, Mills EJ, Boulle A, Ford N. Treatment outcomes of patients on second-line antiretroviral therapy in resource-limited settings. Aids. 2012;26:929–38. [DOI] [PubMed] [Google Scholar]
- 16. Zanoni BC, Sunpath H, Feeney ME. Pediatric response to second-line antiretroviral therapy in South Africa. PLoS One. 2012;7(11):e49591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dow DE, Shayo AM, Cunningham CK, Reddy EA. Durability of antiretroviral therapy and predictors of virologic failure among perinatally HIV-infected children in Tanzania: a four-year follow-up. BMC Infect Dis. 2014;14(1):567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Suaysod R, Ngo-Giang-Huong N, Salvadori N, Cressey TR, Kanjanavanit S, Techakunakorn P, et al. Treatment failure in HIV-infected children on second-line protease inhibitor-based antiretroviral therapy. Clin Infect Dis. 2015;61(1):95–101. [DOI] [PubMed] [Google Scholar]
- 19. Fokam J, Salpini R, Santoro MM, Cento V, Perno C-F, Colizzi V, et al. Drug resistance among drug-naive and first-line antiretroviral treatment-failing children in Cameroon. Pediatr Infect Dis J. 2011;30(12):1062–68. [DOI] [PubMed] [Google Scholar]
- 20. Boettiger D, Nguyen VK, Durier N, Bui HV, Sim BLH, Azwa I, et al. Efficacy of second line antiretroviral therapy among people living with HIV /AIDS in Asia: results from the TREAT Asia HIV observational PubMed Commons. J Acquir Immune Defic Syndr. 2015;68(2):186–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. The World Bank Country and Lending Groups [Internet]. [cited 2015 December4] Available from: http://data.worldbank.org/about/country-and-lending-groups
- 23. World Health Organization Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection [Internet]. 2013. [cited 2016 September5] Available from: http://who.int/hiv/pub/guidelines/arv2013/download/en/
- 24. World Health Organization Antiretroviral therapy for HIV infection in infants and children: towards universal access. 2010 revision [Internet]. 2010. [cited 2016 September5] Available from: http://www.who.int/hiv/pub/paediatric/infants2010/en/ [PubMed]
- 25. Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Internet]. [cited 2015 August24] Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 26. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche C, Vandenbroucke JP. Policy and practice The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ. 2007;45120(August):867–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Higgins PT, Altman D, Sterne J. Chapter 8: assessing risk of bias in included studies In: Cochrane handbook for systematic reviews of interventions. Version 5. The Cochrane Collaboration; 2011. [Google Scholar]
- 28. Arrivé E, Newell M-L, Ekouevi DK, Chaix M-L, Thiebaut R, Masquelier B, et al. Prevalence of resistance to nevirapine in mothers and children after single-dose exposure to prevent vertical transmission of HIV-1: a meta-analysis. Int J Epidemiol. 2007. October;36(5):1009–21. [DOI] [PubMed] [Google Scholar]
- 29. Kuhn L, Hunt G, Technau K-G, Coovadia A, Ledwaba J, Pickerill S, et al. Drug resistance among newly diagnosed HIV-infected children in the era of more efficacious antiretroviral prophylaxis. Aids. 2014. July;28(11):1673–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Boender TS, Hamers RL, Ondoa P, Wellington M, Chimbetete C, Siwale M, et al. Protease inhibitor resistance in the first 3 years of second-line antiretroviral therapy for HIV-1 in Sub-Saharan Africa. J Infect Dis. 2016;214(6):873–83. [DOI] [PubMed] [Google Scholar]
- 31. Puthanakit T, Jourdain G, Suntarattiwong P, Chokephaibulkit K, Siangphoe U, Suwanlerk T, et al. High virologic response rate after second-line boosted protease inhibitor-based antiretroviral therapy regimens in children from a resource limited setting. AIDS Res Ther. 2012;9(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Prasitsuebsai W, Teeraananchai S, Singtoroj T, Van Nguyen L, Kosalaraksa P, Kurniati N, et al. Treatment outcomes and resistance patterns of children and adolescents on second-line antiretroviral therapy in Asia. JAIDS. 2016;72(4):380–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kyu HH, Pinho C, Wagner JA, Brown JC, Bertozzi-Villa A, Charlson FJ, et al. Global and national burden of diseases and injuries among children and adolescents between 1990 and 2013. JAMA Pediatr. 2016;170(3):267–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ferrand RA, Briggs D, Ferguson J, Penazzato M, Macpherson P, Ross DA, et al. Viral suppression in adolescents on antiretroviral treatment: a review of the literature and critical appraisal of methodological challenges. Trop Med Int Heal. 2016;21(3):325–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lee S, Hazra R. Achieving 90-90-90 in paediatric HIV: adolescence as the touchstone for transition success. J Int AIDS Soc. 2015;18(7 Suppl 6):20257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. The Breather Trial Group Weekends-off efavirenz-based antiretroviral therapy in HIV-infected children, adolescents, and young adults (BREATHER): a randomised, open-label, non-inferiority, phase 2/3 trial. Lancet HIV. 2016;3018(16):1–10. The BREATHER (PENTA 16) Trial Group. Open Access article distributed under the terms of CC BY. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cluver LD, Hodes RJ, Sherr L, Orkin FM, Meinck F, Lim PLAK, et al. Social protection: potential for improving HIV outcomes among adolescents. J Int AIDS Soc. 2015;18(Suppl 6):202607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Medicines Patent Pool Antiretoviral priorities of the Medicines Patent Pool [Internet]. Medicines Patent Pool; 2015. [cited 2016 September6] Available from: http://www.medicinespatentpool.org/wp-content/uploads/MPP_ARV_Priorities_Report_4th_Edition_web.pdf [Google Scholar]
- 39. Dehority W, Abadi J, Wiznia A, Viani RM. Use of integrase inhibitors in HIV-infected children and adolescents. Drugs. 2015;75(13):1483–97. Springer International Publishing. [DOI] [PubMed] [Google Scholar]
- 40. Penazzato M, Lee J, Capparelli E, Essajee SM, Ford N, Ojoo A, et al. Optimizing drugs to reach treatment targets for children and adolescents living with HIV. J Int AIDS Soc. 2015;18(Suppl 6):20270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kindra G, Sipambo N, Moultrie H, Fairlie L. Outcomes in treatment with darunavir/ritonavir in ART-experienced paediatric patients. South African Med J. 2015;105(5):330. [DOI] [PubMed] [Google Scholar]
- 42. Boerma RS, Kityo C, Boender TS, Kaudha E, Kayiwa J, Musiime V, et al. Favourable outcomes of paediatric second-line protease inhibitor-based antiretroviral treatment in Uganda Abstract presented at: 10th international workshop on HIV treatment, pathogenesis, and prevention research in resource-poor settings; Yaoundé, Cameroon; 2016. [Google Scholar]
- 43. Wallis CL, Mellors JW, Venter WDF, Sanne I, Stevens W. Protease inhibitor resistance is uncommon in HIV-1 subtype C infected patients on failing second-line lopinavir/r-containing antiretroviral therapy in South Africa. AIDS Res Treat. 2011;2011:769627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Boender T, Hamers RL, Ondoa P, Wellington M, Siwale M, Kityo C, et al. Protease inhibitor resistance at 2nd-line HIV treatment failure in Sub-Saharan Africa Abstract presented at: Conference on Retroviruses and Opportunistic Infections (CROI); Boston, USA; 2016. [Google Scholar]
- 45. Levison JH, Orrell C, Gallien S, Kuritzkes DR, Fu N, Losina E, et al. Virologic failure of protease inhibitor-based second-line antiretroviral therapy without resistance in a large HIV treatment program in South Africa. PLoS One. 2012;7(3):e32144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Meyers T, Sawry S, Wong JY, Moultrie H, Pinillos F, Fairlie L, et al. Virologic failure among children taking lopinavir/ritonavir-containing first-line antiretroviral therapy in South Africa. Pediatr Infect Dis J. 2015;34(2):175–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Zanoni BC, Sunpath H, Feeney ME. Pediatric response to second-line antiretroviral therapy in South Africa. PLoS One. 2012;7(11):5–9. [DOI] [PMC free article] [PubMed] [Google Scholar]


