Abstract
The study of vulnerabilities to depression typically identifies factors that are thought to be universally maladaptive or adaptive. In contrast, researchers recently have theorized that the ability to flexibly engage in different thoughts and behaviors that fit situational demands may be most indicative of psychological health. We review empirical evidence from 147 studies reporting associations between five components of flexibility (set-shifting, affective set-shifting, cardiac vagal control, explanatory flexibility, and coping flexibility) and depression and classify studies according to strength of study design. Evidence from correlational and case-controlled studies suggests cross-sectional relationships, but few prospective studies have been conducted. We discuss limitations of existing studies, identify new directions for programmatic research, and discuss implications that flexibility has for the prevention and treatment of depression.
Keywords: Flexibility, depression, major depressive disorder, vulnerability, risk factors, cognition
Major Depressive Disorder (MDD) is the most common mental disorder and is associated with tremendous social and occupational impairment, resulting in major personal, economic, and societal costs (Kessler & Wang, 2009). For many individuals, MDD is a chronic illness with recurrence rates ranging from 50% following the first episode to 90% among individuals with three or more episodes (Burcusa & Iacono, 2007). As a result, an increasingly important focus in public health is in determining ways to prevent the onset and recurrence of depression (Kessler & Wang, 2009). Identifying factors that predispose individuals to experiencing depression represents one important step in alleviating the personal and societal costs imposed by MDD.
Over the past few decades, many individual difference characteristics have been identified as factors that confer vulnerability to experiencing depression1 (e.g., Alloy, Salk, Stange, & Abramson, in press). These characteristics include cognitive styles, coping styles, strategies for regulating emotions, and interpersonal behaviors, among others (Dobson & Dozois, 2008). The majority of research on vulnerability to depression to date has focused on the use of particular thoughts, strategies, or behaviors that may increase the propensity for experiencing depression. In contrast with these standard approaches, researchers recently have theorized that some characteristics in and of themselves may not be adaptive or maladaptive per se; rather, the ability to flexibly engage in different thoughts and behaviors depending on the demands of the situation may be most indicative of psychological health (Aldao, 2013; Bonanno & Burton, 2013; Cheng, Lau, & Chan, 2014; Kashdan & Rottenberg, 2010).
In the current review, we consider whether viewing the literature through the lens of flexibility may offer a fresh perspective on understanding characteristics that may confer vulnerability to, or may protect against, the experience of depression. We intend this perspective to complement, but not replace, existing models of vulnerability to depression. In light of the increasing focus on dimensional approaches to the study of normative behavior and mechanisms of psychopathology (e.g., the Research Domain Criteria [RDoC] initiative; Sanislow et al., 2010), we will review selected aspects of flexibility in healthy samples before discussing how each aspect may be impaired in MDD, and how inflexibility could potentially confer vulnerability to the onset, maintenance, and recurrence of depression. By considering a normative to disordered perspective to flexibility and depression, we hope to facilitate an improved understanding of the psychological nature of depression and to introduce potentially novel targets to engage in the treatment of MDD and other psychopathology. Although recent reviews have highlighted the topic of flexibility in relation to health and individual differences in self-regulation (e.g., Bonanno & Burton, 2013; Kashdan & Rottenberg, 2010), to date, no comprehensive review has evaluated depression through the lens of (in)flexibility. We offer this review in hopes of filling this gap.
Defining Flexibility and Theoretical Relevance to Depression
We define flexibility as the ability to adapt in response to changes in external or internal circumstances (e.g., stressful events, or changes in emotions). Organisms with greater capacity for flexibility are able to identify contextual demands, choose responses from a repertoire of options, appropriately and efficiently match responses to the demands of the situation, and adjust responses as needed given ongoing changes in the environment or additional information obtained that is relevant to the goal at hand (e.g., Bonanno & Burton, 2013; Dobzhansky, 1970). Thus, the ultimate benefit of flexibility is the ability to adapt to external and internal contexts to advance toward one’s goals, which may range from improving one’s comfort in a situation, to promoting long-term occupational or social success, even to basic survival.
As a result of being able to appropriately adapt to contextual demands, individuals with a greater capacity for flexibility are often able to achieve a desired outcome even when faced with unexpected difficulties that may require a shift in behavior from the status quo. In contrast, individuals who are more inflexible may be unaware of changes in contextual demands, may perceive few possible response options, may have a small repertoire of implementable skills from which to choose, may ineffectively match strategies to situational demands, may be unable to identify strategies that are no longer effective, and may be unable or unwilling to modify behavior to strategies that are more likely to be effective in advancing their goals. Hence, whereas more flexible individuals are resilient and are able to adapt to the context to reach desired outcomes, individuals who are more inflexible may be less likely to overcome obstacles to achieve their goals.
Although we understand and acknowledged that many if not all psychological disorders are marked by inflexibility, which likely reflects (and constitutes non-specific vulnerability to) psychological difficulties more generally (e.g., Kashdan & Rottenberg, 2010), it may be particularly pronounced in MDD. Thus, in the present review, we aim to highlight depression as an example of how inflexibility may be studied as a correlate and as a vulnerability factor for psychopathology.
Components of Flexibility Included in the Current Review
We selected a subset of components of flexibility consistent with our operational definition of flexibility. Constructs selected assessed the ability to modify or switch between existing states (e.g., cognitions, behaviors, emotions, or physiological states) to adapt to contextual demands. These constructs included cognitive flexibility (specifically set-shifting; Miyake et al., 2000), which involves the ability to switch between mental sets by activating relevant material and disengaging from irrelevant material; affective flexibility (affective set-shifting; Genet & Siemer, 2011), which refers to the ability to attend to and disengage from emotional aspects of a situation or a stimulus; cardiac vagal control (CVC; Thayer & Lane, 2009), a measure of parasympathetic nervous system activity that is thought to index the ability to adapt autonomic and emotion-regulatory resources to meet the demands of emotional or stressful situations; explanatory flexibility (Fresco, Rytwinski, & Craighead, 2007a), or variability in individuals’ causal attributions about stressors that may represent a balanced interpretation of events with appropriate contextual information (Fresco et al., 2007a); and coping flexibility (Cheng, 2001), which represents the flexible deployment and subsequent adjustment of coping strategies to match situational demands. These components of flexibility clearly matched well with our definition of flexibility as the ability to modify or switch between existing states to adapt to contextual demands. Although not an exhaustive list of constructs broadly related to flexibility, these constructs share in common their relevance to our definition and may represent an overarching capacity for flexibility that is characterized by flexibility in each of these component domains. We did not include constructs such as rumination (Nolen-Hoeksema, Wisco, & Lyubomirsky, 2008), awareness (Teasdale et al., 2002), metacognition (Wells & Matthews, 1996), decentering (Fresco, Moore et al., 2007a; Fresco, Segal, Buis, & Kennedy, 2007b), mindfulness (Williams, 2008), cognitive inhibition (Miyake et al., 2000), or the “psychological flexibility” proposed by relational frame theory (which also has been referred to as experiential avoidance or acceptance; Hayes et al., 2006). Although arguments could be made for including these constructs as they may enhance or attenuate flexibility or could represent manifestations of inflexibility, we opted to exclude them because of their more peripheral fit with our theoretical definition of flexibility and to avoid redundancy with recent reviews in these areas (particularly rumination; e.g., Aldao et al., 2010; Alloy et al., in press; Koster et al., 2011; Nolen-Hoeksema et al., 2008; Rood et al., 2009; Smith & Alloy, 2009).
Next, we describe our strategy for reviewing empirical evidence for inflexibility as a vulnerability to depression. We then introduce each aspect of inflexibility, explain its measurement, and describe its theoretical relevance to our broader definition of flexibility and to risk for depression. We then review empirical evidence, within each type of study design, for each aspect of inflexibility as a vulnerability to depression.
Method
We conducted a systematic review of the literature to evaluate evidence about whether inflexibility confers vulnerability to depression. Studies were selected if they were empirical (i.e., collected data) and included a measure of one of the five types of flexibility described above, and a measure of depression (e.g., depressive symptoms, diagnoses, or episodes). Cross-sectional case-controlled studies reviewed included data from participants with MDD and healthy controls; case-controlled studies evaluating major depressive episodes exclusively in the context of other psychological disorders were not included. We decided it was premature to conduct a meta-analysis because there have been relatively few empirical studies in several of the areas of flexibility reviewed (explanatory flexibility, coping flexibility, and affective shifting) and recent meta-analyses have been completed for some areas (set-shifting and CVC).
Studies of shifting in depression were included only if shifting was assessed using a behavioral (i.e., not self-report) measure such as the Stroop color-word interference test, trail-making test part B, or internal shift task. Studies assessing CVC were included if they reported a measure of high-frequency heart rate variability (HF-HRV) or of respiratory sinus arrhythmia (RSA, which measures HRV during the respiration cycle), which represent the most commonly accepted indices of CVC (Rottenberg, 2007b). For two of the flexibilities reviewed, shifting and CVC, meta-analyses of cross-sectional case-controlled (MDD vs. healthy) studies have recently been published (Kemp et al., 2010; Lee, Hermens, Porter, & Redoblado-Hodge, 2012; Rottenberg, 2007b; Wagner, Doering, Helmreich, Lieb, & Tadić, 2012; Koenig et al., 2016). Thus, to avoid redundancy, we did not include studies if they were included in those reviews (i.e., if they evaluated shifting or CVC in case-controlled studies before the cutoff dates of those reviews). However, we review the results and implications of these existing review papers before reviewing the more recent literature in these areas. Because case-controlled designs provide stronger support for inflexibility as a vulnerability to depression than do cross-sectional correlational designs in nonclinical samples which include symptoms of lesser severity, we also excluded nonclinical cross-sectional correlational studies of set-shifting or CVC in relation to depression that were published prior to the cutoff dates of these reviews. However, we did include prospective studies of shifting predicting depression given that these studies provide stronger support for our hypotheses, and that these designs fell outside of the scope of these meta-analyses. Similarly, we included prospective studies of CVC predicting depression, although we excluded studies of CVC predicting the course of depression in MDD that were included in Rottenberg’s (2007b) meta-analysis. Because of the possibility of physical health confounds on CVC, and for consistency with prior reviews (Kemp et al., 2010; Rottenberg, 2007b), we excluded samples of patients exclusively recruited from medical settings, such as those with cardiovascular disease. Given the well-documented effect of antidepressants in reducing CVC (Kemp et al., 2010; Wagner et al., 2012), we excluded studies of MDD in which participants were receiving antidepressant treatment (and studies of MDD that did not report medication usage), following other reviews of CVC in depression (Kemp et al., 2010; Rottenberg et al., 2007).
To conduct the literature review, we searched the PsycINFO and PubMed databases in June 2016 using the following search terms: (inflexibility or flexibility or rigid or rigidity or “cardiac vagal control” or “respiratory sinus arrhythmia” or “heart rate variability” or “vagal tone” or switching or shifting or set-shifting) AND (depression or depressive or dysphoria or dysphoric). These search terms generated 3,731 papers in PsycINFO and 2,486 papers in PubMed. Of these papers, 147 met the a priori criteria specified above and were included in the review.
Theory and Evidence for Components of Flexibility
In the review below, we describe underlying theory and measurement of five aspects of flexibility (shifting, affective shifting, CVC, explanatory flexibility, and coping flexibility). We review evidence for each type of inflexibility as a vulnerability to depression by strength of study design, beginning with weaker evidence (from cross-sectional studies) and moving toward the strongest evidence in the literature (from prospective and experimental studies; Riskind & Alloy, 2006; Just, Abramson, & Alloy, 2001). Given that we hypothesized that flexibility would protect against the development of depression, we expected to find primarily negative associations between flexibility and depression (such that higher flexibility was associated with lower levels of depressive symptoms, lower likelihood of MDD, and better course of illness in MDD).
References for papers only included in the review are listed in the Appendix.
Set-Shifting
Theory and measurement
Set-shifting (or “shifting”) is an executive function and is a key component of cognitive flexibility (Miyake et al., 2000), involving the ability to switch between mental sets by activating relevant material and disengaging from irrelevant material. Individuals who are more flexible are able to consider and fluidly shift between different ways of thinking depending on contextual demands. Shifting ability facilitates the use of top-down strategies for controlling attention and behavior, and thus may be central for supporting flexible and effective self-regulation (Kashdan & Rottenberg, 2010). The ability to shift attention from a task at hand to new aspects of a situation that may be more critical (e.g., because they may represent the possibility of risk or reward) is highly adaptive and may allow for behavioral responses to the environment that are appropriate and that capitalize on important information that is newly available.
Individuals who are unable to shift their attention or behavior based on changes in contextual demands are less likely to adapt their behavior to fit the situation. They may maintain behaviors (e.g., thinking patterns, regulation strategies) that are no longer useful, failing to switch to strategies that are more likely to advance their goals (e.g., Joormann & Siemer, 2011). They therefore may be less able to overcome obstacles (such as stressful life events) to achieving their goals, which could lead to adjustment difficulties such as depression. Shifting clearly facilitates cognitive and behavioral flexibility; it is difficult to imagine a person who displays persistently flexible behavior without possessing a strong shifting ability. Thus, poor shifting ability could serve as a vulnerability to depression due to difficulty adjusting and regulating oneself following shifts in contextual demands (such as those that occur as a result of stressors).
A variety of tasks have been developed to measure shifting abilities. The strongest of such tasks typically are behavioral (as opposed to self-reported) in nature and compare reaction times on trials in which individuals must “shift” their mental set to trials in which no shifting is required, allowing for the computation of shifting costs (i.e., additional time taken on shifting trials), with higher costs indicating poorer shifting abilities. One commonly-used task for assessing shifting is the Wisconsin Card Sort Test (Chelune et al., 1993), which requires individuals to shift between mental sets of rules when sorting cards. Another common test of shifting is a variation of the Stroop task called the color-word interference test (e.g., Delis, Kaplan, & Kramer, 2001), in which individuals must alternate (or shift) between naming the color of some words printed on a page and reading some other words; this score is compared to general processing speed scores for an estimate of shifting ability. Another frequently-used shifting task is part B of the trail-making test (TMT-B) (Reitan, 1992), in which individuals must complete a visual search, connecting circles while alternating between numbers and letters in numerical and alphabetical order; this score can be (but often is not) compared to general processing speed scores on part A, which does not involve shifting, to estimate shifting ability. Recent studies also have used forms of an “internal shift task” (IST) that evaluates the ability to shift between mental representations of categories (e.g., De Lissnyder, Koster, & De Raedt, 2012a).
Empirical evidence
Since the publication of two recent meta-analyses evaluating cognitive deficits including shifting in case-controlled samples (reviewed below; Lee et al., 2012; Wagner et al., 2012), several cross-sectional correlational studies have produced inconsistent results for the association between shifting abilities and depressive symptoms using several different behavioral tasks. Better shifting performance on the TMT-B has been negatively correlated with depressive symptoms among older adults (Yochim et al., 2013), adults with bulimia or MDD (Giel et al., 2012), and attention-deficit hyperactivity disorder (Larochette et al., 2011), but not among adolescents with depressive disorders (Holler et al., 2014). Mixed results have been found with the WCST; perseverative errors have been significantly associated with depressive symptoms among depressed, bulimic, mixed psychiatric, and HIV+ adolescent samples (Galderisi et al., 2011; Giel et al., 2012; Han et al., 2016; Salama et al., 2013; Valentino et al., 2012; Zahodne et al., 2014), but not among community youths (Evans et al., 2016; Vergara-Lopez et al., 2013), a mixed sample of healthy and MDD adults (Vergara-Lopez et al., 2016), or adults with a suicide attempt history (Miranda et al., 2012). In MDD, perseverative errors were associated with greater average depression severity, but not with concurrent depressive symptoms (Sarapas et al., 2012). Shifting scores on verbal fluency tasks were associated with fewer symptoms of depression among children of depressed parents (Davidovich et al., 2016). Null associations between shifting and depressive symptoms also have been reported with the IST and similar tasks among students (De Lissnyder et al., 2010, 2011, 2012a), and on attentional shifting tasks in adolescents (Connolly et al., 2014; Wagner et al., 2015). Thus, despite heterogeneity in study samples and shifting tasks, some recent evidence exists that shifting deficits may be associated with greater depression severity, although studies with cross-sectional designs provide little evidence for shifting as a vulnerability to depression.
Shifting impairments in MDD (relative to healthy individuals) have been noted for many years (for a review of older literature, see Austin et al., 2001). Indeed, a pair of recent meta-analyses (Lee et al., 2012; Wagner et al., 2012) of case-controlled studies found evidence consistent with such impairments, although the literature among children is more mixed (Vilgis, Silk, & Vance, 2015). Wagner et al. reviewed six studies that used the TMT-B and found that individuals with MDD exhibited deficits in shifting ability relative to controls. Among patients with first-episode MDD, Lee et al. found significant impairments in shifting ability across six studies using the TMT-B, and impairments in cognitive flexibility across seven studies as assessed by measures including perseverative errors on the WCST. Although Lee et al.’s sample only included first-episode MDD, the fact that findings mirrored those of Wagner et al. and Austin et al. lends support to the hypothesis that shifting is impaired in MDD even among patients who have not experienced recurrent depression; however, it is still possible that shifting deficits could be a consequence of MDD rather than a cause. Nevertheless, given that shifting impairments may persist beyond the remission of depression, previous reviews have concluded that these shifting deficits are unlikely to be mood-state dependent (Austin et al., 2001; Trivedi & Greer, 2014).
Among children and adolescents, Vilgis et al. reviewed ten case-controlled studies of shifting in pediatric MDD. In a few of these studies, children with MDD exhibited poorer set-shifting on tasks including the TMT-B and WCST perseverative errors relative to healthy children. However, several studies reporting null results used similar measures, including TMT-B and WCST, as well as the CANTAB intra-extra-dimensional set-shift task. The authors speculate that depression chronicity (i.e., number and duration of past episodes) or the severity of current symptoms may explain discrepancies between cognitive deficits displayed in adult and pediatric MDD, as children with depression who are studied are likely to have had a shorter duration of illness with less time for the cumulative impact of multiple episodes of depression (Vilgis et al., 2015). An important related issue that few studies have addressed is how the presence of common comorbidities of MDD (such as anxiety disorders) may impact the presence of group differences in shifting abilities in depression.
Among more recent case-controlled studies, mixed evidence exists linking shifting impairments to MDD, with results generally indicating impairment or no impairment (as opposed to superior performance) in MDD. Several studies have found inferior performance in current MDD relative to controls on Stroop shifting tasks (Hammar et al., 2011; Schmid & Hammar, 2013a), as well as on perseverative responses on the WCST (Lin et al., 2014; Mowlaie et al., 2014), an addition-subtraction shifting task (Jermann et al., 2013), as well as with the IST (De Lissnyder et al., 2012b). Group differences were less-consistently reported on the TMT-B, with some studies reporting poorer shifting in MDD (Giel et al., 2012; Johnco et al., 2015) but others documenting no group differences (Hermens et al., 2013; Schmid & Hammar, 2013a; Thoma et al., 2011), potentially a result of failing to control for scores on the TMT-A (i.e., to account for individual differences in processing speed using non-shift trials). Similar null results have been recently reported with computerized shifting tasks such as a go/no-go task (Murphy et al., 2012), perseverative responses on the WCST (Johnco et al., 2015), a dual word-counting task (Lo & Allen, 2011), a rule-shifting task (Remijnse et al., 2013), and on a Stroop shifting task (Aker et al., 2014). On a computerized shape-sorting task, individuals with current MDD only displayed shifting impairments relative to controls during a rumination induction (Whitmer & Gotlib, 2012), suggesting the need for a closer examination of contextual factors that may influence the expression of shifting impairments in MDD (see also the review of Affective Shifting, below).
Few studies have evaluated shifting in remitted MDD and matched controls, which helps to improve confidence that group differences are not due to current mood state. Hasselbalch et al. (2012) found that shifting performance on the TMT-B was impaired in remitted MDD; in contrast, Peters et al. (2015) found no difference between remitted MDD and matched controls on the same task. On the AS task, remitted MDD patients did not differ from controls; however, individuals with current MDD performed more poorly than did remitted MDD patients, suggesting that shifting may worsen with depression severity (Jermann et al., 2013). Nevertheless, case-controlled designs are inadequate for determining whether shifting could be a vulnerability as opposed to simply a consequence or concomitant of MDD, even if shifting impairments in MDD are not entirely mood-state dependent.
The literature on shifting as a prospective predictor of depression is similarly sparse. Poorer shifting on a variety of tasks predicted the first onset of major depressive episodes among adolescents (Stange et al., in press-a), a greater likelihood of depressive relapse (Schmid & Hammar, 2013b), better response to psychotherapy for depression (Beaudreau et al., 2015), and fewer future symptoms of depression only in the context of better coping (Morris et al., 2015), supporting the hypothesis that individual differences in shifting could confer vulnerability to depression. In contrast, other studies of nonclinical samples have found that perseverative costs on the WCST were not associated with prospective symptoms of depression (Evans et al., 2016; Han et al., 2016).
In sum, many studies of shifting in relation to depression have been conducted to date, with mixed findings but overall indicating that shifting deficits are associated with current depression, with limited but initial evidence of vulnerability to future depression. Obscuring comparisons between these studies is the fact that many have used different measures of shifting. Additionally, tasks such as the TMT-B provide information on shifting that may be clouded by general deficits in accuracy or processing speed (Crowe, 1998), which are also impaired in MDD, as most studies reviewed here did not control for scores on the TMT-A (i.e., scores on non-shift trials). More systematic research is needed to evaluate these measures of shifting as vulnerabilities to depression prospectively, particularly in the context of life events, which has not been evaluated to date.
Affective Set-Shifting
Theory and measurement
Although set-shifting ability may be an important building block of flexibility (Kashdan & Rottenberg, 2010), perhaps more relevant to understanding the role of inflexibility in MDD is affective set-shifting (or “affective shifting”). Affective shifting refers to the ability to attend to and disengage from emotional aspects of a situation or a stimulus specifically. Individuals who have high levels of affective flexibility may be able to switch attention away from emotional aspects of a situation (e.g., feelings of embarrassment after misspeaking during a class lecture) and shift resources toward thoughts or behaviors that will facilitate the most important goal at hand. In contrast, individuals with poor affective shifting ability are likely to experience difficulty disengaging from emotionally-salient stimuli, even if these stimuli are not of high relevance to the primary goal at hand. In the example above, a person with poor affective shifting ability might become “stuck” on the feelings of embarrassment and have difficulty shifting her attention away from her affect, even if her primary goal is to continue with the lecture. Affective shifting thus is highly relevant to flexibility in that it allows individuals to appropriately attend to information that is contextually appropriate, and to disengage from stimuli that are no longer appropriate. Poor affective shifting ability could represent a vulnerability factor for depression, as individuals who experience events that precipitate negative affect, which may require cognitive or behavioral disengagement to attend to priorities other than the affect, would experience difficulty disengaging from this material, potentially resulting in the maintenance or exacerbation of this negative affect.
Relatedly, initial evidence suggests that affective shifting is associated with numerous aspects of effective self-regulation. For example, affective shifting predicted greater levels of trait resilience even beyond general cognitive flexibility (Genet & Siemer, 2011). Difficulties with affective shifting away from negative material were associated with greater use of rumination in daily life (Genet, Malooly, & Siemer, 2013) and poorer ability to use reappraisal to down-regulate emotions in response to a sad film clip (Malooly, Genet, & Siemer, 2013). These results suggest that affective shifting may be central to flexible and effective emotion regulation.
Affective shifting typically has been measured with behavioral tasks similar to those used to assess non-affective set-shifting. In contrast with general shifting tasks, affective shifting tasks require participants to switch between attending to the affective (e.g., positive/negative) and non-affective (emotionally neutral) aspects of stimuli (e.g., Genet & Siemer, 2011). Neutral and affective go/no-go tasks are also sometimes used, which allow for similar comparisons to be made between shifting costs for affective and non-affective stimuli (e.g., Murphy, Michael, & Sahakian, 2012). The ability of studies to make claims about affective shifting, versus shifting in general, are strengthened when they also include non-affective shifting trials, which allows for the comparison of shifting costs between affective and non-affective switch trials.
Empirical evidence
In comparison to the literature on general set-shifting, relatively few studies have examined affective set-shifting in relation to depression. Using an affective shifting task that involved sorting faces based on emotional or non-emotional content, De Lissnyder et al. (2010) found that students with elevated levels of depressive symptoms exhibited higher affective shifting costs when shifting from emotional to non-emotional trials than did students with non-elevated symptoms, suggesting perseveration during emotionally-relevant stimuli. However, using other affective shifting tasks such as the IST, depressive symptoms in nonclinical samples were not correlated with shift costs (Koster et al., 2013; Mocan et al., 2014; Vergara-Lopez et al., 2016). No studies of individuals with diagnoses of MDD were identified that evaluated associations between affective shifting and depression symptom severity.
A few case-controlled studies of affective shifting in current MDD have been conducted as well. On an affective shifting go/no-go task, Murphy et al. (1999) observed that patients with MDD performed more poorly on shifting trials than did controls. MDD participants exhibited significantly higher affective shifting costs than controls in studies using a dual-word counting affective IST (Lo & Allen, 2011) and an affective Stroop task (Kaiser et al., 2015), but not on an emotional picture-sorting task (Aker et al., 2014). These studies implicate affective shifting costs in MDD, but did not provide information about whether shifting costs differed based on the valence of the material. In contrast, using an emotionally-adapted version of the WCST, Deveney and Deldin (2006) reported that individuals with current MDD had poorer shifting costs for negative stimuli, but superior shifting costs for positive stimuli, relative to controls. These results suggest MDD may be characterized by greater attention to and perseveration on negative affective information, which may be detrimental to the ability to shift thinking in ways that are contextually appropriate. However, these studies did not address the specificity of these shifting costs to affective stimuli by comparing whether individuals with MDD exhibited greater affective shifting costs relative to regular shifting costs.
To address this issue, Murphy et al. (2012) compared performance on neutral and affective shifting go/no-go tasks between patients with MDD and controls. Relative to controls, depressed participants performed more poorly on affective shifting trials, particularly when shifting from sad to happy trials, than on neutral shifting trials. These results suggest that depressed individuals may have particular difficulty with shifting away from sad material, which is consistent with research demonstrating attentional biases to negative stimuli in MDD (Peckham, McHugh, & Otto, 2010). Finally, Lange et al. (2012) demonstrated similarly that remitted MDD patients showed impairments in shifting during an affective shifting go/no-go task relative to controls, indicating that inflexibility in shifting during affective material may not simply be a state marker of MDD.
These few studies suggest that affective shifting may help to account for mixed findings with non-affective shifting impairments and depression. However, no prospective or vulnerability-stress studies have been conducted with affective shifting and depression to date, so it is not yet clear how affective shifting compares to non-affective shifting in characterizing or conferring vulnerability to depression.
Cardiac Vagal Control (CVC)
Theory and measurement
CVC is a characteristic that is associated with parasympathetic nervous system functioning and that may underlie cognitive and behavioral forms of flexibility (Kashdan & Rottenberg, 2010; Thayer & Lane, 2009). Often measured by beat-to-beat variability in heart rate, CVC reflects parasympathetic control over the heart rate by regions of the brain stem via the vagus nerve. When individuals are resting, the vagal pathway serves as a brake on the sympathetic nervous system’s influence on the heart, allowing for conservation of resources, and resulting in greater variability in heart rate (Thayer & Lane, 2009). When the environment becomes more demanding, the vagal brake can be withdrawn, allowing for the mobilization of resources to cope with environmental challenges (e.g., negative emotions, survival threats, or physical activity). Thus, the withdrawal of the vagal brake allows the individual to flexibly adapt their behavior and cognition to changing contextual demands (Kashdan & Rottenberg, 2010; Rottenberg, 2007b).
Individuals who are flexible may display high resting levels of CVC and appropriate withdrawal of CVC during contextually demanding situations. In contrast, individuals who are inflexible may display low resting CVC and a poor ability to withdraw CVC, which may reflect poor self-regulation of attentional and emotional systems (Rottenberg, 2007b). Consistent with this theory, poor CVC has been related to a number of aspects of impairments in self-regulation (Kashdan & Rottenberg, 2010; Thayer & Lane, 2009), including higher emotional arousal in response to stressors and lower coping effectiveness, as well as inflexible deployment of attention and impairments in executive functioning, including on tasks of set-shifting, inhibition, and working memory (Kashdan & Rottenberg, 2010). Given that MDD is associated with inflexible, context-insensitive emotional and behavioral responding to environmental demands (Rottenberg, 2007a), CVC theoretically would be expected to be suppressed in MDD (Rottenberg, 2007b). Furthermore, because low resting CVC and poor ability to withdraw CVC reflect inflexibility to contextual demands, individuals without MDD but who have low CVC might be particularly vulnerable to experiencing depression following exposure to contexts that require flexible adaptation (e.g., negative life events).
CVC is assessed via an electrocardiogram and respiration measured from the chest wall, as indexed by variability in heart rate that is associated with the respiration cycle. There are two common approaches to measuring CVC. Respiratory sinus arrhythmia (RSA) is computed as the average range in time between each heart beat (the inter-beat interval) that occurs between inspiration and expiration. Heart rate variability (HRV) can be measured in the absence of respiration data by selecting high frequency HRV (HF-HRV), which assesses faster vagal-directed respiratory influence on HRV while excluding slower sources of HRV that may reflect both sympathetic and parasympathetic influences (Rottenberg, 2007b). Two aspects of CVC can be evaluated. First, CVC can be evaluated during periods of rest (“resting” CVC, RSA, or HRV), with high resting CVC considered to be adaptive. Second, comparing CVC during a resting period to CVC during a period during which vagal withdrawal is considered adaptive (such as by eliciting sad affect with a film, or during a stressor task) allows for the measurement of CVC “reactivity.” Greater reactivity (vagal withdrawal to stimuli) generally is considered to be adaptive (Rottenberg, 2007). However, emerging evidence suggests that moderate reactivity may be the most adaptive form of CVC reactivity, as too little or too much reactivity may be associated with maladjustment (e.g., Marcovitch et al., 2010; Kogan et al., 2013). However, most studies have evaluated linear effects of CVC, rather than quadratic effects, which would more effectively test such hypotheses.
Empirical evidence
In a recent meta-analysis of eighteen studies containing a total of 401 adults with current MDD, Kemp et al. (2010) demonstrated that depression symptom severity is moderately negatively correlated with resting HF-HRV. In contrast, a meta-analysis of six studies containing 2,625 healthy children and adolescents revealed no significant relationship between subclinical depressive symptoms and resting HF-HRV (Koenig et al., 2016). It is possible that the negative association between resting HF-HRV and depressive symptoms only is apparent when including a more complete range of symptoms (as in clinical samples), or that this relationship is less apparent among children and adolescents.
Several recent cross-sectional correlational studies have produced variable findings regarding the association between CVC and depressive symptoms. A few recent studies have documented that high resting CVC is associated with lower levels of depressive symptoms among healthy individuals (Blood et al., 2015; Hopp et al., 2013; Schwerdtfeger & Gerteis, 2013; Tucker et al., 2012) and in MDD (Chang et al., 2012, 2015; Yeh et al., 2016), findings consistent with the conclusions of the meta-analysis of adults with MDD noted above (Kemp et al., 2010). Many other recent studies have failed to find linear relationships between resting CVC (measured by HF-HRV or RSA) and symptoms of depression cross-sectionally among healthy individuals (Beevers et al., 2011; Bosch et al., 2009; El-Sheikh et al., 2013; Fagundes et al., 2012; Gentzler et al., 2009; Hawkins 2011; Koenig et al., 2016; Kogan et al., 2013; Kop et al., 2010; Mann et al., 2015; Musser et al., 2012; Quintana et al., 2012; Sanchez-Gonzalez et al., 2013; Shenk et al., 2010; Silva et al., 2014; Song et al., 2011; Stange et al., in press-b; Su et al., 2010; Taylor et al., 2011; Vazquez et al., 2016) and in MDD (Byrne et al., 2010; Tonhajzerova et al., 2012; Yaroslavsky et al., 2016).
However, the results of several additional studies that failed to find main effects of resting CVC on depressive symptoms suggest that this relationship may sometimes be moderated by other contextual factors such as gender (Chen et al., 2010), elevated cortisol levels (El-Shiekh et al., 2011), or the occurrence of stressful life events (McLaughlin et al., 2015) or unsupportive parenting (Mezulis et al., 2015). Although these studies are cross-sectional in nature, they suggest the possibility that low resting CVC increases susceptibility to symptoms of depression following stressors. Some studies also have suggested that resting CVC may be negatively associated with specific aspects of depression rather than the syndrome as a whole, such as somatic, anhedonic, and melancholic symptoms (Bosch et al., 2009; Chen et al., 2012; Kemp et al., 2014) and insomnia (Rottenberg et al., 2007). Findings from recent studies of CVC reactivity have provided evidence that is similarly mixed, including studies documenting the hypothesized negative association between CVC reactivity and symptoms of depression (Choi et al., 2011; Gentzler et al., 2009; Oppenheimer et al., 2013; Rottenberg, 2007b; Shinba et al., 2008), yet others failing to find the expected association (El-Sheikh et al., 2013; Fagundes et al., 2012; Gentzler et al., 2013; Shenk et al., 2010; Yaroslavsky et al., 2016). Other studies only showed an association with cognitive aspects of depressive symptoms (Gordon et al., 2012), or when examining interactions between CVC at rest and CVC reactivity (Yaroslavsky et al., 2016).
In terms of case-controlled studies of resting CVC in current MDD, Kemp et al.’s (2010) meta-analysis of eighteen case-controlled studies containing a total of 401 patients with MDD and 407 healthy controls demonstrated a medium and significant effect of reduced resting HF-HRV in MDD relative to controls. Consistent with these findings, Rottenberg’s (2007) meta-analysis of thirteen prior studies found a small-to-medium and significant effect of reduced resting CVC in a total of 262 individuals with MDD relative to 334 healthy individuals. Koenig et al.’s (2016) meta-analysis of six studies containing 99 children and adolescents with MDD compared to 160 controls corroborated these findings, documenting a medium effect of reduced resting HF-HRV in pediatric MDD. The majority of studies in our review of more recent papers parallel these earlier findings, with diminished levels of resting CVC in MDD relative to matched controls (Berger et al., 2012; Chang et al., 2012, 2015; Cyranowski et al., 2011; Garcia et al., 2012; Ha et al., 2015; Kemp et al., 2012; Kishore et al., 2014; Koschke et al., 2009; Pradeep et al, 2012; Shinba, 2014; Tonhajzerova et al., 2009, 2010, 2012; Yeh et al., 2016), with some other studies showing no impairment in CVC in MDD (Byrne et al., 2010; Garcia et al., 2016; Jiang et al., 2015; Kikuchi et al., 2009; Liang et al., 2015; Nugent et al., 2011; O’Regan et al., 2015; Voss et al., 2011), and others reporting atypical increases in CVC (attenuated reactivity or vagal withdrawal) in response to cognitive or stressor tasks in MDD (Liang et al., 2015; Shinba, 2014; for review, see Hamilton & Alloy, 2016). Despite some heterogeneity in findings, results of the literature generally point to the presence of attenuated resting CVC among individuals with current MDD. No studies that met review criteria were found examining CVC in remitted MDD relative to healthy individuals, so whether CVC may represent a state (vs. trait) effect of depression remains unclear. Given that measuring CVC reactivity still is relatively new, no studies of unmedicated MDD and healthy individuals were found.
Relatively few studies have been conducted of CVC predicting the course of depressive episodes or fluctuations in depressive symptoms. Rottenberg’s (2007b) qualitative review of such studies among individuals with current MDD reported mixed findings, with three studies showing that greater resting CVC at baseline predicted reduced MDD symptom severity over time, but two studies failing to document such effects, and two additional studies reporting the opposite effects, with one additional study reporting that lower HF-HRV reactivity to positively-(but not negatively-valenced) films predicted lower likelihood of recovery from MDD. In our more recent review, one study of current MDD found that higher resting CVC predicted prospective decreases in depressive symptoms (Jain et al., 2014), whereas additional studies reported nonsignificant effects of resting CVC (Fraguas et al., 2007; Kovacs et al., 2016; Rottenberg et al., 2007) or of the interaction between resting CVC and CVC reactivity (Kovacs et al., 2016) on illness course in MDD. Thus, the evidence for CVC as a prospective predictor of illness course in MDD is mixed and modest at best.
Among healthy individuals, resting CVC (Dieleman et al., 2016; Vazquez et al., 2016; Yaroslavsky et al., 2014) and CVC reactivity did not predict prospective symptoms alone, but one study found that their interaction did (Yaroslavsky et al., 2014). Results from other studies also suggested that low resting CVC could serve as a vulnerability to depression that is not apparent in the absence of certain contextual factors such as social support (Hopp et al., 2013) and social withdrawal (Morgan et al., 2013). Finally, only two true prospective vulnerability-stress studies of CVC have been conducted to date. Stange et al. (in press-b) evaluated RSA reactivity to sadness and amusement, as part of a multi-wave study of fluctuations in stressful events and symptoms of depression among university students. Providing strong support for the vulnerability-stress hypothesis, and using an idiographic (person-centered) approach to fluctuations in stressful events, Stange et al. found that individuals with less RSA reactivity to a sad film experienced more symptoms of depression across twelve weeks (four waves) of follow-up, and were more reactive to stressful events in the form of increased depressive symptoms, relative to individuals who experienced greater RSA reactivity. In contrast, RSA reactivity to an amusing film was not associated with prospective symptoms of depression as a main effect or in interaction with stressors. Finally, in a community sample of adolescents, Bosch et al. (2009) found that resting RSA did not predict prospective levels of depressive symptoms as a main effect or in interaction with stressful events.
Overall, although initial findings are promising, there is a clear need for additional prospective studies to elucidate the role of CVC (at rest, and in response to stimuli such as sadness and stressors) in predicting depression. There are several possible reasons for the heterogeneity in the findings documented above. For example, studies have reported substantial variability in the tasks and measures used to evaluate CVC. CVC is sometimes evaluated with or without measuring respiration (i.e., RSA vs. HRV, respectively), with power or spectral measures of HRV, at rest (unoccupied, watching a neutrally-valenced film, or during a neutral task involving cognitive load), reactivity (e.g., change in CVC in response to a stressor or films that evoke various emotions), and recovery (e.g., change from a stressor period to a resting period). Although variety in tasks could ultimately provide convergent evidence of the utility of CVC in predicting depression, it could also serve to obfuscate possible relationships that do exist because of a lack of systematic evaluation of CVC while maintaining consistency with tasks across samples. A few studies have found that CVC is associated only with certain symptoms of depression, which suggests the possibility that many of the null findings reviewed here could be a result of the way depression was measured (e.g., Rottenberg, 2007b). Studies evaluating moderators of the effects of CVC on depression also suggest the need to consider CVC in the context of other factors that confer vulnerability or protection against depression. Finally, although the results of the meta-analyses are less susceptible to power issues, many of the above studies used relatively small samples, which could have resulted in some Type I or II errors.
Explanatory Flexibility
Theory and measurement
Explanatory flexibility was derived from the learned helplessness model of depression (Abramson, Seligman, & Teasdale, 1978), which proposed that individuals who make internal, stable, and global attributions about the causes of negative events are vulnerable to experiencing hopelessness, and subsequent depression, after encountering negative events, because of their pessimistic explanations of the causes of the events. A great deal of empirical support for helplessness and the related hopelessness theory of depression (Abramson, Metalsky, & Alloy, 1989) have been established in the literature (Alloy et al., in press). The causal attributions featured in helplessness theory are typically evaluated with measures such as the Attributional Style Questionnaire (ASQ; Peterson et al., 1979) and the Cognitive Style Questionnaire (CSQ; Haeffel et al., 2008), which ask individuals to rate the perceived causes of twelve hypothetical events in terms of internality, stability, globality, and perceived consequences and self-implications. Composite scores are typically computed representing total cognitive vulnerability to depression.
In contrast with the helplessness and hopelessness theories, explanatory flexibility theory proposes that the flexibility, or variability, of individuals’ causal attributions may be as important as their valence (pessimistic/optimistic) (Fresco et al., 2007a). Individuals with explanatory flexibility demonstrate the ability to make different types of attributions for the causes of different situations, a characteristic thought to be adaptive given that all situations do not typically have the same types of causes. These individuals may effectively balance their interpretation of events with previous and current contextual information, which results in variability in the perceived causes of negative events, allowing for more adaptive responses to stressors. In contrast, individuals who rigidly make the same types of attributions for the causes of events, even if these attributions are optimistic, may display poorer ability to accurately perceive the causes of different event types depending on the context. These individuals may be less likely to perceive multiple factors that could have caused situations, leading them to make premature conclusions about events without taking into consideration appropriate contextual information that could affect the reason events occurred. Appropriately perceiving the causes of events may facilitate adaptive coping responses to stressors that are consistent with the context of the event’s occurrence (Fresco, Williams, & Nugent, 2006a), which may allow for appropriate behavioral and emotional adjustment to the event, thus preventing negative affective states such as depression. Thus, explanatory flexibility is consistent with our definition of flexibility in that it may facilitate adaptation to contextual demands.
Explanatory flexibility is typically evaluated with measures such as the ASQ or CSQ that are used to assess helplessness or hopelessness theories, by computing the standard deviation of individuals’ responses on the stability and globality dimensions. Thus, explanatory flexibility represents variability in perceived causes across different situation types, meeting the criterion for measuring flexibility in different contexts. Explanatory flexibility is conceptualized to be relatively independent of cognitive content because it captures the variability, but not the type, of responses participants provide. Explanatory flexibility and attributional style (as assessed by helplessness theory) are typically modestly negatively correlated, but have demonstrated relative independence from one another (Moore & Fresco, 2007). Reactivity of explanatory flexibility also has recently begun to be evaluated, with the hypothesis that greater reductions in flexibility (increases in rigidity) following experimentally-induced sadness is indicative of underlying inflexibility in explanatory style (Fresco, Heimberg, Abramowitz, & Bertram, 2006b).
Another measure relevant to explanatory flexibility is the tendency to make “extreme” attributions, which has been proposed as an index of rigid, extreme thinking (e.g., Teasdale et al., 2001; Stange et al., 2013). Extreme attributions are also evaluated using the ASQ or CSQ by summing the number of responses made using the endpoints of the Likert scales (e.g., the cause of event “leads to problems in all other areas of my life” or “will never again be present”). Individuals who make extreme attributions may be cognitively reactive to life events, generating all-or-nothing explanations for events, rather than making more moderate attributions after considering multiple possible causes and relevant contextual information. Extreme response styles on other measures also have been associated with intolerance of ambiguity, cognitive inflexibility, simplistic thinking, and taking a shorter time to complete measures (e.g., Naemi, Beale, & Payne, 2009). Thus, the tendency to make extreme responses on attributional measures could represent relatively automatic schematic processing that is uncorrected by deliberate reappraisal in more moderate terms (e.g., Teasdale et al., 2001). This extreme automatic processing could interfere with the ability to make contextually-appropriate attributions about the causes of stressful events.
Empirical evidence
Since the inception of the concept of explanatory flexibility, relatively few studies have evaluated its relationship with depression. Consistent with the flexibility hypothesis, greater explanatory flexibility was cross-sectionally correlated with lower levels of depressive symptoms in some studies of college students (Fresco et al., 2006a; Haeffel, 2010; Qi et al., 2012), but not in others (Fresco et al., 2007a), nor in recently unemployed men (Syzdek & Addis, 2010) or in adults receiving psychosocial treatment for bipolar depression (Stange et al., 2013a). Extreme attributions were positively correlated with depressive symptoms at two time points among college students (Haeffel, 2010), but not among adults receiving psychosocial treatment for bipolar depression (Stange et al., 2013a). Thus, the literature is limited in this area and evidence that does exist is mixed.
Few studies have evaluated explanatory flexibility in case-controlled studies of MDD. Lackner, Moore, Minerovic, and Fresco (2015) evaluated explanatory flexibility in treatment-seeking adults with current or lifetime MDD, generalized anxiety disorder, or other Axis I disorders (a psychiatric control group). Adults with a history of MDD exhibited lower explanatory flexibility than did psychiatric controls. These results are consistent with the hypothesis that explanatory flexibility is attenuated in MDD. However, they do not provide information about MDD relative to healthy individuals, which only one other study to date has evaluated. To this end, Fresco et al. (2006b) found that college students with a history of MDD did not differ from never-depressed participants on explanatory flexibility. However, following a negative mood induction, euthymic participants with a history of MDD displayed greater decreases in explanatory flexibility relative to control participants, and relative to currently dysphoric participants with a history of MDD. This study was limited, however, by the use of self-report measures to diagnose MDD and dysphoric subgroups, and relatively small sample sizes within depression subgroups. Together, these studies provide mixed evidence that explanatory flexibility is reduced in MDD, and provide partial support for the hypothesis that reactivity of explanatory (in)flexibility may be amplified in MDD.
Several studies have evaluated explanatory flexibility as a predictor of depression prospectively. Providing strong support for the vulnerability hypothesis, Fresco et al. (2007a) found that among college students, explanatory flexibility interacted with negative life events to predict prospective depressive symptoms, such that individuals with lower flexibility were more likely than individuals with higher flexibility to experience depressive symptoms following stressors. In a separate study, Fresco and Moore (2007) obtained the same pattern of results with explanatory flexibility reactivity, showing that individuals who experienced greater drops in explanatory flexibility following a negative mood induction were most likely to experience depressive symptoms following stressors, six weeks and six months after baseline. These studies provide evidence that explanatory (in) flexibility (and reactivity) confers vulnerability to depression in the context of stress. Moore, Fresco, Schumm, and Dobson (under review) also reported that among patients with remitted MDD, the combination of high levels of post-treatment explanatory flexibility and low levels of pessimistic explanatory style predicted the lowest rates of relapse, although explanatory flexibility alone did not predict relapse. In contrast with these studies, Haeffel (2010) reported that among college students, explanatory flexibility did not predict prospective levels of depressive symptoms alone or in interaction with life events; similarly, Syzdek and Addis (2010) found that explanatory flexibility did not predict depressive symptoms prospectively among recently unemployed men.
In contrast with these prospective findings, Stange et al. (2013a) found that greater explanatory flexibility predicted a longer duration of depression among adults with bipolar depression. Analyses revealed that individuals with greater explanatory flexibility endorsed more extreme optimistic and pessimistic attributions, and that more extreme attributions also predicted a longer course of depression as well as more lifetime episodes of depression (Stange et al., 2013b,c). These results suggest that explanatory flexibility could represent variability in attributions from multiple sources: one source being adaptive, contextually appropriate variability as proposed by Fresco et al. (2006a), and another being the maladaptive tendency to make extreme attributions (particularly those at opposing poles, which would inflate the variability in the flexibility metric). Consistent with these results in bipolar depression, extreme attributions have predicted a greater likelihood of depressive relapse in remitted MDD (Teasdale et al., 2001) and in remitted bipolar disorder (Stange et al., 2015) and a lower likelihood of response to pharmacotherapy for MDD (Petersen et al., 2007), although another study found that extreme attributions did not predict either of these outcomes in patients with remitted MDD (Ching & Dobson, 2010). However, extreme attributions did interact with life events to predict prospective levels of depressive symptoms among college students (Haeffel, 2010).
Thus, evidence overall suggests that explanatory inflexibility and extreme attributions each may confer vulnerability to depression, although additional research is needed to replicate the vulnerability-stress findings of both indices, to clarify the adaptive and maladaptive aspects of each measure, and to demonstrate the predictive validity of explanatory flexibility in clinical samples.
Coping Flexibility
Theory and measurement
Coping refers to behavioral and cognitive strategies that people use to manage the stress associated with difficult experiences, or to manage the experiences themselves. Two major functions of coping have been hypothesized. Problem-focused coping involves focusing on ways of solving a problem associated with a stressful event, such as figuring out how to share responsibilities after the death of a family member. Emotion-focused coping involves taking action with the goal of improving one’s emotions associated with a stressful event, such as reminiscing about fond memories of a family member after their passing away (Lazarus & Folkman, 1984).
Although theories of coping suggest that effective coping may be a matter of fit between the strategy and situational demands, previous research has generally considered strategies to be uniformly adaptive or maladaptive, a distinction Bonanno and Burton (2013) have termed the “fallacy of uniform efficacy.” Research that has focused on situation-strategy fit has indicated that these two types of coping strategies may be effective in certain types of situations, but may actually elicit distress in others (e.g., Cheng, 2001). Cheng (2001) proposed that the effectiveness of coping depends on the controllability of the outcomes of the stressful situation. Problem-focused coping may be most effective in situations that are controllable because problem-solving enables the individual to identify solutions and hence to potentially gain control over the stressful event. In contrast, emotion-focused coping may be most effective for events that are uncontrollable and hence require adjustment to the situation rather than attempts to fix it. Hence, effective coping may best be characterized by flexible deployment of coping strategies that match situational demands (Cheng, 2001). Although the ability to initially identify a coping strategy that is appropriate to the context is important, initial coping strategies do not always produce desirable outcomes. Hence, Kato (2012) proposed that the abilities to discontinue coping strategies when they are ineffective and identify alternative strategies are also important aspects of coping flexibility.
Coping flexibility thereby may impact depression as a consequence of the effectiveness of the chosen coping response. Given that depressed individuals tend to perceive events as uncontrollable (e.g., Brown & Siegel, 1988), show an over-reliance on perseverative coping strategies such as rumination (Alloy et al., in press), and have difficulties disengaging from unattainable goals and changing strategies (Johnson et al., 2010), they are likely to miss opportunities for improving situational outcomes by coping flexibly, potentially exacerbating or maintaining depression. It is not difficult to imagine that healthy individuals who display similar characteristics could be vulnerable to experiencing depression, particularly when they encounter difficult events that require coping.
Although a relatively new construct, coping flexibility has been measured a number of ways in the literature (for a more detailed discussion, see Cheng et al., 2014). Cheng (2001) has measured coping flexibility with the Coping Flexibility Questionnaire (CFQ), which evaluates perceived controllability and goal of coping strategies (problem- vs. emotion-focused) for managing recent stressful life events. A situation-strategy fit index, representing coping flexibility, is computed representing how well coping strategies were implemented based on the controllability of the event. By examining coping strategies across a variety of naturally-occurring life events, the researcher is able to determine how similarly individuals respond over time to different types of events. In addition, Kato (2012) developed the Coping Flexibility Scale (CFS), a self-report scale that measures evaluation coping and adaptive coping. This measure relies on individuals’ perceptions of their own ability to implement these types of flexible coping in situations in general.
Empirical evidence
Most of the research on coping flexibility and depression to date has been cross-sectional and correlational in nature. Cheng’s (2001) seminal study on the CFQ demonstrated with a cluster analysis that college students with greater inflexibility (poor situation-strategy fit) had the highest levels of depressive symptoms, a finding replicated by Zong et al. (2010a) in a mixed sample of students with high or low schizotypal personality features. Zong et al. (2010b) also demonstrated that poorer situation-strategy fit on the CFQ was correlated with higher levels of depressive symptoms in a non-clinical sample. Using a similar measure of situation-strategy fit with hypothetical events and a similar cluster analysis approach, however, Cheng and Cheung (2005) found that individuals who were classified as “inflexible” did not differ from “flexible” individuals on depressive symptoms. Using a different measure of coping flexibility, Fresco et al. (2006a) found that variability in coping strategies (conceptualized as greater coping flexibility) was associated with lower levels of depressive symptoms in college students.
In separate studies of college students, Kato (2001, 2012, 2015) found that the ability to abandon ineffective coping strategies, and the ability to identify and adopt new coping strategies, were negatively correlated with depressive symptoms, supporting the hypothesis that these aspects of coping flexibility are relevant to protection against depression. Using a conceptually similar measure in a sample of patients with rheumatic diseases, Vriezekolk et al. (2010) found that the ability to switch between types of coping strategies according to situational demands was associated with lower levels of depressive symptoms, whereas the ability to identify multiple coping options and their situational fit was not. In a cross-sectional test of the vulnerability-stress nature of coping flexibility among college students, Lam and McBride-Chang (2007) reported that greater diversity in coping strategies attenuated the impact of life events on concurrent depressive symptoms, consistent with the hypothesis that inflexibility in coping may confer vulnerability to symptoms of depression. However, the cross-sectional nature of the study makes it difficult to draw strong conclusions about the direction of these effects.
Notably, in a recent meta-analysis evaluating cross-sectional associations between coping flexibility and adjustment to stressful life situations, Cheng et al. (2014) found evidence for a small-to-moderate effect size, with coping flexibility being associated with greater psychological adjustment. Although broadly relevant to the current review, because of the relative dearth of literature on coping flexibility in depression, Cheng et al. collapsed across several measures of distress and well-being and did not report associations with depression specifically.
Only one case-controlled study of coping flexibility in MDD has been conducted to date, finding that situation-strategy fit was attenuated among acutely depressed patients with MDD relative to matched control participants (Gan et al., 2006). Finally, coping flexibility has been evaluated in just two prospective studies. First, Kato (2012) found that in three separate samples of college students, baseline coping flexibility (both the ability to discontinue coping strategies when they are ineffective and to identify alternative strategies) predicted lower levels of depressive symptoms twelve weeks later, even after accounting for Cheng’s (2001) measure of situation-strategy fit, which also significantly predicted lower levels of depressive symptoms. This study provides evidence that Kato’s CFS contains predictive validity beyond existing measures of coping flexibility. However, this study failed to control for baseline depressive symptoms, so it is unclear whether coping flexibility predicted residual changes in depressive symptoms, rendering the evidence not much stronger than cross-sectional correlational tests.
Perhaps the strongest test of coping flexibility as a vulnerability to depression was conducted in a randomized, controlled trial of a coping flexibility intervention by Cheng, Kogan, and Chio (2012). Working adults who received an intervention to improve coping flexibility exhibited greater decreases in depressive symptoms immediately following treatment and four months later relative to individuals who received a coping skills treatment only and relative to waitlisted controls, and this decrease in symptoms was mediated by an increase in coping flexibility in the coping flexibility treatment group. This study provides particularly strong evidence because it is a prospective test, and because coping flexibility was experimentally manipulated, suggesting that improvements in flexibility could have resulted in improvements in symptoms of depression. These data suggest that coping inflexibility could be a causal mechanism of symptoms of depression, although it is not possible to rule out all other mechanisms by which the coping flexibility intervention could have affected improvement in symptoms.
Collectively, these studies suggest that variability and the ability to modify coping strategies to appropriately fit the context is adaptive and may be protective against depression. However, more research is needed before strong claims can be made about whether coping flexibility is a vulnerability to depression, given that existing studies have used a variety of different measures (providing convergent evidence, but making comparisons between studies difficult), different analytical approaches (e.g., cluster analysis, correlation, and regression) without ruling out possible alternative causes, and that few prospective studies (and no prospective studies with a vulnerability-stress framework) have been conducted to date.
Limitations of Existing Research and Future Directions
Although the field has begun to recognize the potential that flexibility holds for understanding depression, research investigating these relationships is still in its early stages. Many limitations of existing studies prevent inferences about whether inflexibility confers vulnerability to depression. Different operational definitions exist within each type of flexibility reviewed here. These various definitions highlight the multiple components or dimensions within each aspect of flexibility, but they also prevent useful comparisons from being made between studies and could partially account for mixed findings in association with depression. Given that research on flexibility in depression is nascent, many types of flexibility (e.g., explanatory flexibility, coping flexibility, emotion regulation flexibility, and affective set-shifting) have not yet been widely studied, and those that have been more widely studied (e.g., set-shifting and CVC) have rarely used designs adequate to test the status of flexibility as a vulnerability to depression. Perhaps for these reasons, findings generally have been mixed, without clear consistent support for inflexibility in the onset of depression. However, evidence from extant correlational and case-controlled studies is suggestive that flexibility may be impaired among individuals with more severe depressive symptoms, indicating the need for studies to evaluate potential causal roles of inflexibility in depression.
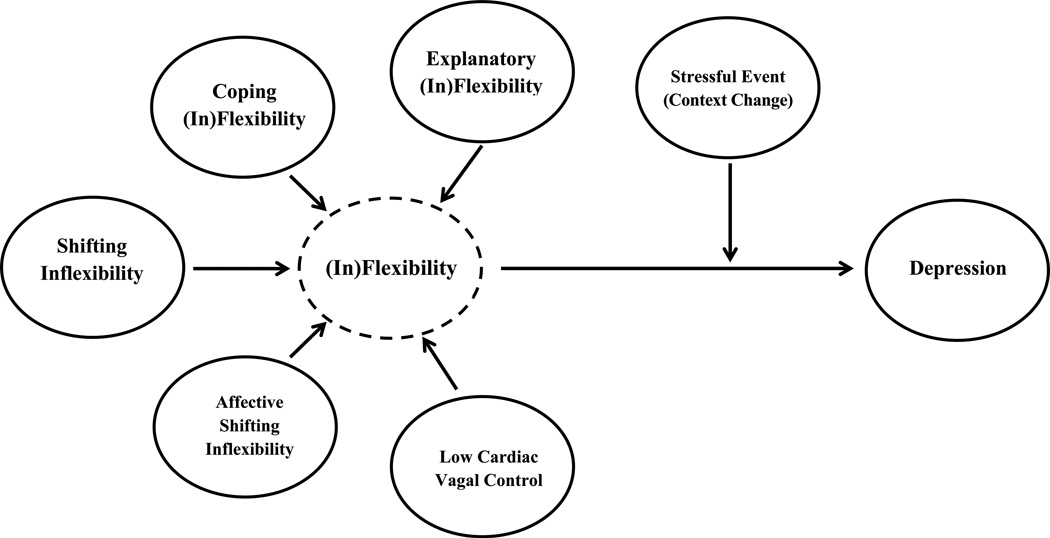
Broadly, this review suggests the possible presence of an overarching construct of flexibility that is characterized by flexibility in each of these component domains (Figure 1). This flexibility may reflect a core capacity to adapt thinking and behavior to match the demands of changing contexts in order to meet one’s goals. Although each of these aspects of flexibility has been reviewed separately, each reflects an aspect of the capacity for adaptive, flexible self-regulation in a dynamic environment. Programmatic research, as discussed below, is needed to further evaluate the presence of an overarching construct of flexibility and its relation to depression.
Figure 1.
Untested theoretical model displaying components reflecting a core capacity of flexibility, deficits in which may confer vulnerability to depression, particularly in the context of stressful life events when flexibility may be most adaptive.
The Role of Context in Evaluating Flexibility
Stressful life events represent one type of context that requires individuals to evaluate situational demands and choose strategies for self-regulation, which may explain the substantial variability in the extent to which life events precipitate depression (e.g., Monroe et al., 2009). To the extent that encountering context changes (such as stressors) throughout life is typical, flexibility will be adaptive in facilitating the ability to meet one’s goals and desires. Hence, a vulnerability-stress framework might be useful in viewing inflexibility in relation to depression. Relatedly, many of the studies reviewed here failed to document associations between flexibilities and depression. If inflexibilities only confer vulnerability to depression in contexts that require flexible shifting, however, main effects of inflexibility on depression might not be apparent unless contextual factors, which include, but are not limited to, life events, are assessed (e.g., Aldao, 2013).
To date, it is unclear whether inflexibility serves as a general risk factor for depression (i.e., as a main effect predictor), or whether it could confer vulnerability specifically when activated by stressful events or context shifts that require flexible adjustment for effective adaptation. Future research should also consider whether inflexibility could confer vulnerability to depression in other contexts that require successful self-adjustment, even if not considered “life events” per se. For example, inflexible individuals might not experience depression if they are only operating within one context (or one type of context) in which the current style of thinking or behavior is useful. However, upon changing contexts, the same strategies might be less useful, which could result in failure to attain goals, leading to problems such as frustration and sadness. Thus, whether inflexibility precipitates depression might depend on how many types of contexts (that require different strategies for effective adaptation) individuals encounter.
Additional theoretical work on “fit” indices such as Cheng’s (2001) measure of coping situation-strategy fit might also be useful for advancing the field of flexibility. For example, in addition to perceiving variability in the causes of events, do certain classes of situations have corresponding types of attributions or emotion-regulation strategies that would be most adaptive (cf. Troy et al., 2013)? Preliminary work has indicated the adaptiveness of the ability to flexibly engage in different emotion-regulation strategies depending on the demands of the situation (Aldao & Nolen-Hoeksema, 2012; Aldao, Sheppes, & Gross, 2015; Bonanno et al., 2004; Bonanno & Burton, 2013), a possibility that should be extended further to evaluating vulnerability to (and resilience against) depression.
Elucidating Components, Mechanisms, and Outcomes of Flexibility
A number of important questions remain regarding inflexibility and depression that are ripe for programmatic research. First, what are the building blocks of flexibility – are there more basic component processes (e.g., executive functions, neurobiological substrates) that underlie the capacity for flexibility? Flexibility may require a complex coordination of components and may draw upon multiple more basic systems. Second, under what conditions do these building blocks of flexibility actually lead to behavioral flexibility, and what characteristics facilitate (vs. detract from) the capacity for flexibility? For example, the impact of explanatory inflexibility on depression may be strengthened by poor shifting ability, which could further prevent individuals from considering multiple explanations because of difficulty switching attention away from salient negative material.
Third, by what mechanisms does inflexibility lead to depression? The domains and constructs proposed by RDoC (Sanislow et al., 2010) provide a promising framework for understanding causes and mechanisms of disorders; preliminary evidence in non-selected samples suggests that flexibility may be applicable to negative and positive valence systems involved in depression such as loss, frustrative nonreward, and low approach motivation, each of which may occur when inflexibility leads to failure to meet goals (Johnson et al., 2010). Additionally, aspects of flexibility are relevant to cognitive systems such as attention and cognitive control (e.g., shifting), systems for social processes including perception and understanding of the self and others (e.g., explanatory flexibility), and arousal and modulatory systems (e.g., CVC). Given the overarching conceptual similarities between aspects of flexibility, it is possible that some types of flexibility facilitate other aspects of flexibility, which serve to protect against depression (i.e., mediational pathways; e.g., Fresco et al., 2006a).
Additional work investigating how flexibility fits with other theories of depression also is warranted. For instance, other vulnerabilities proposed by theories of depression such as rumination, cognitive reactivity, or blunted cortisol responses could to some extent be manifestations of inflexibility, representing difficulty in successfully modulating cognition and affective responses to meet situational demands, or alternatively, that these vulnerabilities may subsequently lead to inflexible behavior. For example, recent work has suggested that the inability to flexibly engage and disengage the default mode network (DMN, a neural network implicated in self-focused thought that is active at rest) according to context may underlie cognitive vulnerability factors such as rumination, cognitive reactivity, and dysfunctional set-shifting (Hamilton et al., 2011; Marchetti et al., 2012; Whitfield-Gabrieli & Ford, 2012). Furthermore, Thayer’s theory of neurovisceral integration suggests that persistent activity and connectivity in the DMN (particularly in the medial prefrontal cortex) may result in a failure to integrate contextual information when determining adaptive behavioral responses (Thayer & Lane, 2009). In addition to exacerbating dysfunctional vagal responses to stressors, persistence of task-negative activity the DMN may manifest in forms of excessively inward-focused attention such as rumination (Marchetti et al., 2012; Thayer & Lane, 2009; Thayer et al., 2009). In turn, rumination further privileges negative self-referential cues, leading to greater insensitivity to contextual demands (e.g., impeding awareness of the punishing effects of rumination) and therefore inhibiting flexibility of cognition, affect, and behavior (e.g., Davis & Nolen-Hoeksema, 2000; Connolly et al., 2014; Koster et al., 2011; Whitmer & Gotlib, 2012, 2013). Future work should further elaborate the specific negative consequences of rumination for affective and behavioral flexibility, while examining the potential for metacognitive self-distancing strategies (e.g., decentering; Bernstein et al., 2015) to facilitate context sensitivity and hence flexibility.
Fourth, when does the development and stabilization of flexibility occur? Does flexibility change over time (e.g., as cognitive faculties increase and later decrease) or given variability in environmental contexts? When does situation-level or state flexibility become personality-level or trait-like flexibility (e.g., Hollenstein et al., 2013)? Fifth, is flexibility always adaptive, or are there any disadvantages to flexibility (e.g., the cognitive load associated with monitoring the context or possible actions)? Finally, the conditions under which inflexibility leads specifically to depression should be evaluated, given that inflexible cognition and behavior characterizes many forms of psychopathology (Kashdan & Rottenberg, 2010). For example, there is evidence that cognitive flexibility is impaired in psychotic disorders and eating disorders (Szoke et al., 2008; Roberts et al., 2007), that resting HRV is lower in anxiety disorders than in healthy individuals (Chalmers et al., 2014), that explanatory flexibility is attenuated in generalized anxiety disorder (Lackner et al., 2015), and that coping flexibility is associated with fewer symptoms of post-traumatic stress disorder following trauma (Park, Chang, & You, 2015).
Design Considerations for Future Research
Several design considerations should be taken into account in future studies evaluating whether flexibility confers vulnerability to depression. Behavioral high-risk designs are one of the most preferred designs, and would involve selecting individuals hypothesized to be at high versus low risk for depression based on some aspect(s) of flexibility, and following these individuals to see which develop the onset of depression. Studies of individuals at risk for depression (e.g., children of depressed parents) also could evaluate whether flexibility is impaired relative to individuals with lower risk for depression and whether flexibility could mediate this risk. These approaches could provide new information about risk beyond that available from patient samples and unselected university student samples. Although few studies to date have done so, experimental manipulation of flexibility also would allow for stronger claims to be made about the impact of flexibility (and changes in flexibility) on depression. Studies also are needed to test whether flexibility predicts additional variance in depression beyond other known vulnerabilities (e.g., negative cognitive styles, specific coping or emotion regulation strategies) to eliminate alternative explanations (Riskind & Alloy, 2006).
Given that measuring flexibility as defined here ideally involves evaluating across multiple contexts, within-subjects study designs (in which participants are exposed to multiple contexts) will generally allow for the most accurate assessment of flexibility; for example, one can test the flexible implementation of various strategies (e.g., attributions, coping or emotion regulation strategies) as well as the ability to switch between strategies to match contextual demands (e.g., Aldao et al., 2015; Bonanno et al., 2004). Studies also should consider using idiographic (participant-specific) approaches, such as asking participants to recall personally-relevant events for stimulus presentation (Aldao, 2013) or evaluating attributions or coping strategies for events that participants actually experienced (e.g., Cheng, 2001). Ecological momentary assessment designs also would provide a strong opportunity to counteract retrospective reporting biases when evaluating the extent to which inflexibility corresponds to depressed mood concurrently and prospectively.
Statistically, multi-wave studies will allow for superior tests of the directionality of the relationships between flexibilities and depression. They also will enable the idiographic assessment of life events (i.e., evaluating participants’ stress levels relative to their own mean), which may allow for more powerful tests of vulnerability-stress relationships. Latent variable modeling of flexibility measures would allow for more complex tests of flexibility (as indexed by multiple measures) predicting depression; although depicted in our theoretical model (Figure 1), this has not been empirically tested to date. Latent class analyses also could evaluate whether individuals with particular combinations of inflexibilities are most vulnerable to depression.
Future prospective studies of inflexibility and depression should also differentiate between predicting the first onset of depression in never-depressed individuals, recovery from depression in currently depressed individuals, and recurrence of depression in previously-depressed individuals. Although conceptually related, these study designs actually evaluate somewhat different questions. For example, flexibility measured during a current depressive episode may represent a truncated range of possible flexibility scores as a result of the selected nature of the sample (only depressed individuals) as well as the current mood state, which could affect flexibility even if flexibility is a relatively stable trait. Predicting the recurrence or recovery from depression is also distinct from predicting the first onset of MDD, because the depression could have impacted the flexibility (e.g., flexibility measured during or after a depressive episode could represent a consequence or scar of MDD) (Just et al., 2001).
Possible Clinical Implications of Flexibility
Although research on cognitive, behavioral, and psychophysiological flexibility is still in its early stages, it suggests a number of possible clinical implications. Given the possibility that inflexible individuals are vulnerable to experiencing the onset or maintenance of depression, assessing components of flexibility may help to improve efforts to identify individuals who are at risk. Although future work is needed to investigate this hypothesis, it is possible that improving flexibility among such individuals would reduce vulnerability or improve the course of depression for those with MDD.
Importantly, although they typically have not systematically evaluated components of flexibility, a number of existing treatments for emotional disorders could affect change in part as a result of improving flexibility. For example, several behavioral therapies (Mennin et al., 2013) emphasize techniques such as mindfulness training, which may facilitate the distancing of oneself from automatic thoughts (Fresco et al., 2007b) and the de-automization of behavioral responses (Kang, Gruber, & Gray, 2013), which may improve cognitive control (Teper, Segal, & Inzlicht, 2013) and allow for more deliberate choice about responses that meet situational demands, thereby improving flexibility and reducing stress reactivity (Feldman et al., 2016; Holzel et al., 2011). Some contemporary therapies also help individuals to improve their repertoires of emotion regulation strategies, potentially facilitating the flexible use of strategies to meet situational demands (e.g., Mennin & Fresco, 2013). For example, building from a solid foundation of traditional and contemporary CBT principles and informed by basic and translational findings in affect science, emotion regulation therapy (ERT; Fresco et al., 2013; Mennin & Fresco, 2013, 2014) was developed to specifically target the hypothesized neurobehavioral deficits of commonly co-occurring disorders such as generalized anxiety disorder (GAD) and MDD. ERT is a theoretically-derived, evidence based treatment that teaches clients skills of attention and metacognitive regulation so they can develop optimal behavioral repertoires associated with threat and reward learning. ERT has demonstrated promising preliminary clinical efficacy in open label and randomized clinical trials (Mennin, Fresco, Ritter, & Heimberg, 2015; Mennin, Fresco, Heimberg & O’Toole, under review; Renna et al., under review).
In addition, there is room for novel therapeutic approaches to target flexibility more explicitly. For example, Cheng et al.’s (2012) coping flexibility intervention was designed to specifically target coping flexibility, and evidence supported improved coping flexibility as a mechanism by which this treatment attenuated symptoms of depression. Future studies could target explanatory flexibility and extreme attributions by helping individuals to see that negative events may have multiple causes, not simply the causes that initially are most salient when experiencing negative affect. It is possible that existing treatments that emphasize distancing from one’s thoughts and emotions could be tailored to help individuals to experience less persistent negative affect following negative events by improving the flexibility or balanced nature of causal attributions about the events (e.g., Fresco et al., 2007b; Teasdale et al., 2001). Next, attentional control trainings (e.g., Siegle et al., 2014; Wells, 2011) have been developed to help people to learn to disengage from inflexible negative thinking, which potentially could reduce vulnerability to depression following stressors. Finally, interventions involving biofeedback (e.g., Siepmann et al., 2008) and repetitive transcranial magnetic stimulation (Remue et al., 2016) have shown initial promise for helping individuals to directly improve their autonomic flexibility in response to emotional or stressful stimuli. It is possible that improving autonomic flexibility would lead to more adaptive cognitive and behavioral responses to shifts in context, but these questions remain to be evaluated in future research.
Conclusions
The results of this review suggest that flexibility may be attenuated in MDD, and that inflexibility is associated with greater depression severity, consistent with the hypothesis that inflexibility may confer vulnerability to depression. However, few studies of the aspects of flexibility reviewed here have evaluated whether inflexibility predicts depression prospectively. Thus, a number of promising avenues exist for future research to be conducted to answer these questions. Future work should continue to investigate and clarify which aspects of inflexibility confer the greatest vulnerability to depression. In doing so, we may discover which features of inflexibility are the most suitable targets for prevention and treatment, which we hope will help to reduce the substantial global burden of MDD.
Acknowledgments
Preparation of this article was supported by National Research Service Award F31MH099761 from the National Institute of Mental Health to Jonathan P. Stange and NIMH grants MH79369 and MH101168 to Lauren B. Alloy. Jonathan P. Stange was supported by NIMH 5T32MH067631-12,
Appendix
References for Papers Included Only in Literature Review
- Aker M, Harmer C, Landrø NI. More rumination and less effective emotion regulation in previously depressed women with preserved executive functions. BMC Psychiatry. 2014;14(334):1. doi: 10.1186/s12888-014-0334-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin MP, Mitchell P, Goodwin GM. Cognitive deficits in depression: Possible implications for functional neuropathology. British Journal of Psychiatry. 2001;178(3):200–206. doi: 10.1192/bjp.178.3.200. [DOI] [PubMed] [Google Scholar]
- Beaudreau SA, Rideaux T, O'Hara R, Arean P. Does cognition predict treatment response and remission in psychotherapy for late-life depression? The American Journal of Geriatric Psychiatry. 2015;23(2):215–219. doi: 10.1016/j.jagp.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beevers CG, Ellis AJ, Reid RM. Heart rate variability predicts cognitive reactivity to a sad mood provocation. Cognitive Therapy and Research. 2011;35(5):395–403. [Google Scholar]
- Berger S, Kliem A, Yeragani V, Bär KJ. Cardio-respiratory coupling in untreated patients with major depression. Journal of Affective Disorders. 2012;139(2):166–171. doi: 10.1016/j.jad.2012.01.035. [DOI] [PubMed] [Google Scholar]
- Blood JD, Wu J, Chaplin TM, Hommer R, Vazquez L, Rutherford HJ, Crowley MJ. The variable heart: High frequency and very low frequency correlates of depressive symptoms in children and adolescents. Journal of Affective Disorders. 2015;186:119–126. doi: 10.1016/j.jad.2015.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosch NM, Riese H, Ormel J, Verhulst F, Oldehinkel AJ. Stressful life events and depressive symptoms in young adolescents: Modulation by respiratory sinus arrhythmia? The TRAILS study. Biological Psychology. 2009;81(1):40–47. doi: 10.1016/j.biopsycho.2009.01.005. [DOI] [PubMed] [Google Scholar]
- Byrne ML, Sheeber L, Simmons JG, Davis B, Shortt JW, Katz LF, Allen NB. Autonomic cardiac control in depressed adolescents. Depression & Anxiety. 2010;27(11):1050–1056. doi: 10.1002/da.20717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalmers JA, Quintana DS, Abbott MJ, Kemp AH. Anxiety disorders are associated with reduced heart rate variability: a meta-analysis. Frontiers in Psychiatry. 2014;5:80. doi: 10.3389/fpsyt.2014.00080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang HA, Chang CC, Chen CL, Kuo TB, Lu RB, Huang SY. Major depression is associated with cardiac autonomic dysregulation. Acta Neuropsychiatrica. 2012;24(6):318–327. doi: 10.1111/j.1601-5215.2011.00647.x. [DOI] [PubMed] [Google Scholar]
- Chang HA, Chang CC, Kuo TB, Huang SY. Distinguishing bipolar II depression from unipolar major depressive disorder: Differences in heart rate variability. The World Journal of Biological Psychiatry. 2015;16(5):351–360. doi: 10.3109/15622975.2015.1017606. [DOI] [PubMed] [Google Scholar]
- Chen HC, Yang CC, Kuo TB, Su TP, Chou P. Cardiac vagal control and theoretical models of co-occurring depression and anxiety: A cross-sectional psychophysiological study of community elderly. BMC Psychiatry. 2012;12(1):93. doi: 10.1186/1471-244X-12-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng C, Cheung MW. Cognitive processes underlying coping flexibility: differentiation and integration. Journal of Personality. 2005;73(4):859–886. doi: 10.1111/j.1467-6494.2005.00331.x. [DOI] [PubMed] [Google Scholar]
- Ching LE, Dobson KS. An investigation of extreme responding as a mediator of cognitive therapy for depression. Behaviour Research and Therapy. 2010;48(4):266–274. doi: 10.1016/j.brat.2009.12.007. [DOI] [PubMed] [Google Scholar]
- Choi CJ, Kim KS, Kim CM, Kim SH, Choi WS. Reactivity of heart rate variability after exposure to colored lights in healthy adults with symptoms of anxiety and depression. International Journal of Psychophysiology. 2011;79(2):83–88. doi: 10.1016/j.ijpsycho.2010.09.011. [DOI] [PubMed] [Google Scholar]
- Connolly SL, Wagner CA, Shapero BG, Pendergast LL, Abramson LY, Alloy LB. Rumination prospectively predicts executive functioning impairments in adolescents. Journal of Behavior Therapy and Experimental Psychiatry. 2014;45(1):46–56. doi: 10.1016/j.jbtep.2013.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowe SF. The differential contribution of mental tracking, cognitive flexibility, visual search, and motor speed to performance on parts A and B of the Trail Making Test. Journal of Clinical Psychology. 1998;54(5):585–591. doi: 10.1002/(sici)1097-4679(199808)54:5<585::aid-jclp4>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- Cyranowski JM, Hofkens TL, Swartz HA, Salomon K, Gianaros PJ. Cardiac vagal control in nonmedicated depressed women and nondepressed controls: impact of depression status, lifetime trauma history, and respiratory factors. Psychosomatic Medicine. 2011;73(4):336–343. doi: 10.1097/PSY.0b013e318213925d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidovich S, Collishaw S, Thapar AK, Harold G, Thapar A, Rice F. Do better executive functions buffer the effect of current parental depression on adolescent depressive symptoms? Journal of Affective Disorders. 2016;199:54–64. doi: 10.1016/j.jad.2016.03.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Lissnyder E, Derakshan N, De Raedt R, Koster EH. Depressive symptoms and cognitive control in a mixed antisaccade task: Specific effects of depressive rumination. Cognition & Emotion. 2011;25(5):886–897. doi: 10.1080/02699931.2010.514711. [DOI] [PubMed] [Google Scholar]
- De Lissnyder E, Koster EH, Derakshan N, De Raedt R. The association between depressive symptoms and executive control impairments in response to emotional and non-emotional information. Cognition & Emotion. 2010;24(2):264–280. [Google Scholar]
- Deveney CM, Deldin PJ. A preliminary investigation of cognitive flexibility for emotional information in major depressive disorder and non-psychiatric controls. Emotion. 2006;6(3):429–437. doi: 10.1037/1528-3542.6.3.429. [DOI] [PubMed] [Google Scholar]
- Dieleman GC, Huizink AC, Tulen JH, Utens EM, Tiemeier H. Stress reactivity predicts symptom improvement in children with anxiety disorders. Journal of Affective Disorders. 2016;196:190–199. doi: 10.1016/j.jad.2016.02.022. [DOI] [PubMed] [Google Scholar]
- Dobzhansky T. Genetics of the evolutionary process. New York, NY: Columbia University Press; 1970. [Google Scholar]
- El-Sheikh M, Keiley M, Erath S, Dyer WJ. Marital conflict and growth in children's internalizing symptoms: The role of autonomic nervous system activity. Developmental Psychology. 2013;49(1):92. doi: 10.1037/a0027703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans LD, Kouros CD, Samanez-Larkin S, Garber J. Concurrent and short-term prospective relations among neurocognitive functioning, coping, and depressive symptoms in youth. Journal of Clinical Child & Adolescent Psychology. 2015;45(1):6–20. doi: 10.1080/15374416.2014.982282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagundes CP, Diamond LM, Allen KP. Adolescent attachment insecurity and parasympathetic functioning predict future loss adjustment. Personality and Social Psychology Bulletin. 2012;38(6):821–832. doi: 10.1177/0146167212437429. [DOI] [PubMed] [Google Scholar]
- Fraguas R, Jr, Marci C, Fava M, Iosifescu DV, Bankier B, Loh R, Dougherty DD. Autonomic reactivity to induced emotion as potential predictor of response to antidepressant treatment. Psychiatry Research. 2007;151(1):169–172. doi: 10.1016/j.psychres.2006.08.008. [DOI] [PubMed] [Google Scholar]
- Fresco DM, Moore MT. Drops in explanatory flexibility following mood priming challenge interact with negative life events to predict future depression. OH: Kent State University; 2007. Unpublished manuscript. [Google Scholar]
- Galderisi S, Bucci P, Mucci A, Bellodi L, Cassano GB, Santonastaso P, Maj M. Neurocognitive functioning in bulimia nervosa: the role of neuroendocrine, personality and clinical aspects. Psychological Medicine. 2011;41(4):839–848. doi: 10.1017/S0033291710001303. [DOI] [PubMed] [Google Scholar]
- Gan Y, Zhang Y, Wang X, Wang S, Shen X. The coping flexibility of neurasthenia and depressive patients. Personality and Individual Differences. 2006;40(5):859–871. [Google Scholar]
- Garcia RG, Valenza G, Tomaz C, Barbieri R. Relationship between cardiac vagal activity and mood congruent memory bias in major depression. Journal of affective disorders. 2016;190:19–25. doi: 10.1016/j.jad.2015.09.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia RG, Zarruk JG, Guzman JC, Barrera C, Pinzon A, Trillos E, Tomaz C. Sex differences in cardiac autonomic function of depressed young adults. Biological Psychology. 2012;90(3):179–185. doi: 10.1016/j.biopsycho.2012.03.016. [DOI] [PubMed] [Google Scholar]
- Gentzler AL, Santucci AK, Kovacs M, Fox NA. Respiratory sinus arrhythmia reactivity predicts emotion regulation and depressive symptoms in at-risk and control children. Biological Psychology. 2009;82(2):156–163. doi: 10.1016/j.biopsycho.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentzler AL, Wheat AL, Palmer CA, Burwell RA. Children's responses to cognitive challenge and links to self-reported rumination. Cognition & Emotion. 2013;27(2):305–317. doi: 10.1080/02699931.2012.716394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giel KE, Wittorf A, Wolkenstein L, Klingberg S, Drimmer E, Schönenberg M, Zipfel S. Is impaired set-shifting a feature of"pure” anorexia nervosa? Investigating the role of depression in set-shifting ability in anorexia nervosa and unipolar depression. Psychiatry Research. 2012;200(2):538–543. doi: 10.1016/j.psychres.2012.06.004. [DOI] [PubMed] [Google Scholar]
- Gordon JL, Ditto B, D'Antono B. Cognitive depressive symptoms associated with delayed heart rate recovery following interpersonal stress in healthy men and women. Psychophysiology. 2012;49(8):1082–1089. doi: 10.1111/j.1469-8986.2012.01397.x. [DOI] [PubMed] [Google Scholar]
- Ha JH, Park S, Yoon D, Kim B. Short-term heart rate variability in older patients with newly diagnosed depression. Psychiatry Research. 2015;226(2):484–488. doi: 10.1016/j.psychres.2015.02.005. [DOI] [PubMed] [Google Scholar]
- Haeffel GJ. Cognitive vulnerability to depressive symptoms in college students: A comparison of traditional, weakest-link, and flexibility operationalizations. Cognitive Therapy and Research. 2010;34(1):92–98. [Google Scholar]
- Hamilton JL, Alloy LB. Atypical reactivity of heart rate variability to stress and depression: Systematic review of the literature and directions for future research. Clinical Psychology Review. 2016;50:67–79. doi: 10.1016/j.cpr.2016.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammar Å, Strand M, Årdal G, Schmid M, Lund A, Elliott R. Testing the cognitive effort hypothesis of cognitive impairment in major depression. Nordic Journal of Psychiatry. 2011;65(1):74–80. doi: 10.3109/08039488.2010.494311. [DOI] [PubMed] [Google Scholar]
- Han G, Helm J, Iucha C, Zahn-Waxler C, Hastings PD, Klimes-Dougan B. Are executive functioning deficits concurrently and predictively associated with depressive and anxiety symptoms in adolescents? Journal of Clinical Child & Adolescent Psychology. 2016;45(1):44–58. doi: 10.1080/15374416.2015.1041592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasselbalch BJ, Knorr U, Hasselbalch SG, Gade A, Kessing LV. Cognitive deficits in the remitted state of unipolar depressive disorder. Neuropsychology. 2012;26(5):642. doi: 10.1037/a0029301. [DOI] [PubMed] [Google Scholar]
- Hermens DF, Lee RS, De Regt T, Lagopoulos J, Naismith SL, Scott EM, Hickie IB. Neuropsychological functioning is compromised in binge drinking young adults with depression. Psychiatry Research. 2013;210(1):256–262. doi: 10.1016/j.psychres.2013.05.001. [DOI] [PubMed] [Google Scholar]
- Hopp H, Shallcross AJ, Ford BQ, Troy AS, Wilhelm FH, Mauss IB. High cardiac vagal control protects against future depressive symptoms under conditions of high social support. Biological Psychology. 2013;93(1):143–149. doi: 10.1016/j.biopsycho.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain FA, Cook IA, Leuchter AF, Hunter AM, Davydov DM, Ottaviani C, Shapiro D. Heart rate variability and treatment outcome in major depression: A pilot study. International Journal of Psychophysiology. 2014;93(2):204–210. doi: 10.1016/j.ijpsycho.2014.04.006. [DOI] [PubMed] [Google Scholar]
- Jermann F, Van der Linden M, Gex-Fabry M, Guarin A, Kosel M, Bertschy G, Bondolfi G. Cognitive functioning in patients remitted from recurrent depression: Comparison with acutely depressed patients and controls and follow-up of a Mindfulness-Based Cognitive Therapy Trial. Cognitive Therapy and Research. 2013;37:1004–1014. [Google Scholar]
- Jiang XL, Zhang ZG, Chen Y, Ye CP, Lei Y, Wu L, Xiao ZJ. A blunted sympathetic and accentuated parasympathetic response to postural change in subjects with depressive disorders. Journal of affective disorders. 2015;175:269–274. doi: 10.1016/j.jad.2015.01.009. [DOI] [PubMed] [Google Scholar]
- Johnco C, Wuthrich VM, Rapee RM. The impact of late-life anxiety and depression on cognitive flexibility and cognitive restructuring skill acquisition. Depression and Anxiety. 2015;32(10):754–762. doi: 10.1002/da.22375. [DOI] [PubMed] [Google Scholar]
- Kaiser RH, Andrews-Hanna JR, Spielberg JM, Warren SL, Sutton BP, Miller GA, Banich MT. Distracted and down: neural mechanisms of affective interference in subclinical depression. Social Cognitive and Affective Neuroscience. 2015;10(5):654–663. doi: 10.1093/scan/nsu100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kato T. The relationship between flexibility of coping to stress and depression. Japanese Journal of Psychology. 2001;72(1):57–63. doi: 10.4992/jjpsy.72.57. [DOI] [PubMed] [Google Scholar]
- Kato T. Testing of the coping flexibility hypothesis based on the dual-process theory: Relationships between coping flexibility and depressive Symptoms. Psychiatry Research. 2015;230(2):137–142. doi: 10.1016/j.psychres.2015.07.030. [DOI] [PubMed] [Google Scholar]
- Kemp AH, Quintana DS, Felmingham KL, Matthews S, Jelinek HF. Depression, comorbid anxiety disorders, and heart rate variability in physically healthy, unmedicated patients: implications for cardiovascular risk. PLoS One. 2012;7(2):e30777. doi: 10.1371/journal.pone.0030777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp AH, Quintana DS, Quinn CR, Hopkinson P, Harris AW. Major depressive disorder with melancholia displays robust alterations in resting state heart rate and its variability: implications for future morbidity and mortality. Frontiers in Psychology. 2014;5:1387. doi: 10.3389/fpsyg.2014.01387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kikuchi M, Hanaoka A, Kidani T, Remijn GB, Minabe Y, Munesue T, Koshino Y. Heart rate variability in drug-naive patients with panic disorder and major depressive disorder. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2009;33(8):1474–1478. doi: 10.1016/j.pnpbp.2009.08.002. [DOI] [PubMed] [Google Scholar]
- Kishore RK, Abhishekh HA, Udupa K, Thirthalli J, Lavekar GS, Gangadhar BN, Sathyaprabha TN. Evaluation of the influence of ayurvedic formulation (Ayushman-15) on psychopathology, heart rate variability and stress hormonal level in major depression (Vishada) Asian journal of psychiatry. 2014;12:100–107. doi: 10.1016/j.ajp.2014.07.002. [DOI] [PubMed] [Google Scholar]
- Koenig J, Kemp AH, Beauchaine TP, Thayer JF, Kaess M. Depression and resting state heart rate variability in children and adolescents—A systematic review and meta-analysis. Clinical Psychology Review. 2016;46:136–150. doi: 10.1016/j.cpr.2016.04.013. [DOI] [PubMed] [Google Scholar]
- Kogan A, Gruber J, Shallcross AJ, Ford BQ, Mauss IB. Too much of a good thing? Cardiac vagal tone’s nonlinear relationship with well-being. Emotion. 2013;13(4):599–604. doi: 10.1037/a0032725. [DOI] [PubMed] [Google Scholar]
- Koschke M, Boettger MK, Schulz S, Berger S, Terhaar J, Voss A, Bär KJ. Autonomy of autonomic dysfunction in major depression. Psychosomatic Medicine. 2009;71(8):852–860. doi: 10.1097/PSY.0b013e3181b8bb7a. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Yaroslavsky I, Rottenberg J, George CJ, Kiss E, Halas K, Makai A. Maladaptive mood repair, atypical respiratory sinus arrhythmia, and risk of a recurrent major depressive episode among adolescents with prior major depression. Psychological Medicine. 2016 doi: 10.1017/S003329171600057X. [DOI] [PubMed] [Google Scholar]
- Lackner RJ, Moore MT, Minerovic JR, Fresco DM. Explanatory Flexibility and Explanatory Style in Treatment-Seeking Patients with Axis I Psychopathology. Cognitive Therapy and Research. 2015;39(6):736–743. doi: 10.1007/s10608-015-9702-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange C, Adli M, Zschucke E, Beyer R, Ising M, Uhr M, Bermpohl F. Affective set-shifting deficits in patients with major depression in remission. Journal of Psychiatric Research. 2012;46(12):1623–1626. doi: 10.1016/j.jpsychires.2012.09.007. [DOI] [PubMed] [Google Scholar]
- Larochette AC, Harrison AG, Rosenblum Y, Bowie CR. Additive neurocognitive deficits in adults with attention-deficit/hyperactivity disorder and depressive symptoms. Archives of Clinical Neuropsychology. 2011;26(5):385–395. doi: 10.1093/arclin/acr033. [DOI] [PubMed] [Google Scholar]
- Liang CS, Lee JF, Chen CC, Chang YC. Reactive heart rate variability in male patients with first-episode major depressive disorder. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2015;56:52–57. doi: 10.1016/j.pnpbp.2014.08.004. [DOI] [PubMed] [Google Scholar]
- Lin K, Xu G, Lu W, Ouyang H, Dang Y, Lorenzo-Seva U, Lee TM. Neuropsychological performance in melancholic, atypical and undifferentiated major depression during depressed and remitted states: a prospective longitudinal study. Journal of Affective Disorders. 2014;168:184–191. doi: 10.1016/j.jad.2014.06.032. [DOI] [PubMed] [Google Scholar]
- Liang CS, Lee JF, Chen CC, Chang YC. Reactive heart rate variability in male patients with first-episode major depressive disorder. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2015;56:52–57. doi: 10.1016/j.pnpbp.2014.08.004. [DOI] [PubMed] [Google Scholar]
- Lin K, Xu G, Lu W, Ouyang H, Dang Y, Lorenzo-Seva U, Lee TM. Neuropsychological performance in melancholic, atypical and undifferentiated major depression during depressed and remitted states: a prospective longitudinal study. Journal of Affective Disorders. 2014;168:184–191. doi: 10.1016/j.jad.2014.06.032. [DOI] [PubMed] [Google Scholar]
- Lo BCY, Allen NB. Affective bias in internal attention shifting among depressed youth. Psychiatry Research. 2011;187(1):125–129. doi: 10.1016/j.psychres.2010.10.001. [DOI] [PubMed] [Google Scholar]
- Mann SL, Selby EA, Bates ME, Contrada RJ. Integrating affective and cognitive correlates of heart rate variability: A structural equation modeling approach. International Journal of Psychophysiology. 2015;98(1):76–86. doi: 10.1016/j.ijpsycho.2015.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Rith-Najarian L, Dirks MA, Sheridan MA. Low vagal tone magnifies the association between psychosocial stress exposure and internalizing psychopathology in adolescents. Journal of Clinical Child & Adolescent Psychology. 2015;44(2):314–328. doi: 10.1080/15374416.2013.843464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezulis AH, Crystal SI, Ahles JJ, Crowell SE. Examining biological vulnerability in environmental context: Parenting moderates effects of low resting respiratory sinus arrhythmia on adolescent depressive symptoms. Developmental Psychobiology. 2015;57(8):974–983. doi: 10.1002/dev.21347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda R, Gallagher M, Bauchner B, Vaysman R, Marroquín B. Cognitive inflexibility as a prospective predictor of suicidal ideation among young adults with a suicide attempt history. Depression & Anxiety. 2012;29(3):180–186. doi: 10.1002/da.20915. [DOI] [PubMed] [Google Scholar]
- Mocan O, Stanciu O, Visu-Petra L. Relating individual differences in internalizing symptoms to emotional attention set-shifting in children. Anxiety, Stress, & Coping. 2014;27(5):509–526. doi: 10.1080/10615806.2014.888419. [DOI] [PubMed] [Google Scholar]
- Moore MT, Fresco DM, Schumm JA, Dobson KS. Change in explanatory flexibility and explanatory style in cognitive therapy and its components. 2016 Manuscript in preparation. [Google Scholar]
- Morgan JK, Shaw DS, Forbes EE. Physiological and behavioral engagement in social contexts as predictors of adolescent depressive symptoms. Journal of Youth and Adolescence. 2013;42(8):1117–1127. doi: 10.1007/s10964-012-9815-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris MC, Evans LD, Rao U, Garber J. Executive function moderates the relation between coping and depressive symptoms. Anxiety, Stress, & Coping. 2015;28(1):31–49. doi: 10.1080/10615806.2014.925545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mowlaie M. The comparison of executive functions in obsessive-compulsive disorder and major depressive disorder patients with healthy individuals. Advances in Cognitive Science. 2014;16(3):61–71. [Google Scholar]
- Nugent AC, Bain EE, Thayer JF, Sollers JJ, III, Drevets WC. Heart rate variability during motor and cognitive tasks in females with major depressive disorder. Psychiatry Research: Neuroimaging. 2011;191(1):1–8. doi: 10.1016/j.pscychresns.2010.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oppenheimer JE, Measelle JR, Laurent HK, Ablow JC. Mothers’ vagal regulation during the still-face paradigm: normative reactivity and impact of depression symptoms. Infant Behavior and Development. 2013;36(2):255–267. doi: 10.1016/j.infbeh.2013.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Regan C, Kenny RA, Cronin H, Finucane C, Kearney PM. Antidepressants strongly influence the relationship between depression and heart rate variability: findings from The Irish Longitudinal Study on Ageing (TILDA) Psychological Medicine. 2015;45(03):623–636. doi: 10.1017/S0033291714001767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park M, Chang ER, You S. Protective role of coping flexibility in PTSD and depressive symptoms following trauma. Personality and Individual Differences. 2015;82:102–106. [Google Scholar]
- Peckham AD, McHugh RK, Otto MW. A meta-analysis of the magnitude of biased attention in depression. Depression & Anxiety. 2010;27(12):1135–1142. doi: 10.1002/da.20755. [DOI] [PubMed] [Google Scholar]
- Peters AT, Jacobs RH, Crane NA, Ryan KA, Weisenbach SL, Ajilore O, Zubieta JK. Domain-specific impairment in cognitive control among remitted youth with a history of major depression. Early Intervention in Psychiatry. 2015 doi: 10.1111/eip.12253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen TJ, Feldman G, Harley R, Fresco DM, Graves L, Holmes A, Segal ZV. Extreme response style in recurrent and chronically depressed patients: Change with antidepressant administration and stability during continuation treatment. Journal of Consulting and Clinical Psychology. 2007;75(1):145–153. doi: 10.1037/0022-006X.75.1.145. [DOI] [PubMed] [Google Scholar]
- Pradeep J, Sambashivaiah S, Thomas T, Radhakrishnan R, Vaz M, Srinivasan K. Heart rate variability responses to standing are attenuated in drug naive depressed patients. Indian Journal of Physiology and Pharmacology. 2012;56(3):213–221. [PubMed] [Google Scholar]
- Qi ZH, Chen J, Jiang H, Zhang HJ. Relation of attribution styles and attribution flexibility to mental health in college students. Chinese Mental Health Journal. 2012;26(4):310–314. [Google Scholar]
- Remijnse PL, van den Heuvel OA, Nielen MM, Vriend C, Hendriks GJ, Hoogendijk WJG, Veltman DJ. Cognitive inflexibility in obsessive-compulsive disorder and major depression is associated with distinct neural correlates. PloS one. 2013;8(4):e59600. doi: 10.1371/journal.pone.0059600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts ME, Tchanturia K, Stahl D, Southgate L, Treasure J. A systematic review and meta-analysis of set-shifting ability in eating disorders. Psychological Medicine. 2007;37(8):1075–1084. doi: 10.1017/S0033291707009877. [DOI] [PubMed] [Google Scholar]
- Rottenberg J, Chambers AS, Allen JJ, Manber R. Cardiac vagal control in the severity and course of depression: the importance of symptomatic heterogeneity. Journal of Affective Disorders. 2007;103(1):173–179. doi: 10.1016/j.jad.2007.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salama C, Morris M, Armistead L, Koenig LJ, Demas P, Ferdon C, Bachanas P. Depressive and conduct disorder symptoms in youth living with HIV: the independent and interactive roles of coping and neuropsychological functioning. AIDS Care. 2013;25(2):160–168. doi: 10.1080/09540121.2012.687815. [DOI] [PubMed] [Google Scholar]
- Sarapas C, Shankman SA, Harrow M, Goldberg JF. Parsing trait and state effects of depression severity on neurocognition: Evidence from a 26-year longitudinal study. Journal of Abnormal Psychology. 2012;121(4):830–837. doi: 10.1037/a0028141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmid M, Hammar Å. A follow-up study of first episode major depressive disorder. Impairment in inhibition and semantic fluency – potential predictors for relapse? Frontiers in Psychology. 2013b;4:633. doi: 10.3389/fpsyg.2013.00633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmid M, Hammar Å. Cognitive function in first episode major depressive disorder: poor inhibition and semantic fluency performance. Cognitive Neuropsychiatry. 2013a;18(6):515–530. doi: 10.1080/13546805.2012.754748. [DOI] [PubMed] [Google Scholar]
- Schwerdtfeger AR, Gerteis AKS. Is the blunted blood pressure reactivity in dysphoric individuals related to attenuated behavioral approach? International Journal of Psychophysiology. 2013;90(1):58–65. doi: 10.1016/j.ijpsycho.2013.01.015. [DOI] [PubMed] [Google Scholar]
- Shenk CE, Noll JG, Putnam FW, Trickett PK. A prospective examination of the role of childhood sexual abuse and physiological asymmetry in the development of psychopathology. Child Abuse & Neglect. 2010;34(10):752–761. doi: 10.1016/j.chiabu.2010.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinba T. Altered autonomic activity and reactivity in depression revealed by heart-rate variability measurement during rest and task conditions. Psychiatry and Clinical Neurosciences. 2014;68(3):225–233. doi: 10.1111/pcn.12123. [DOI] [PubMed] [Google Scholar]
- Shinba T, Kariya N, Matsui Y, Ozawa N, Matsuda Y, Yamamoto KI. Decrease in heart rate variability response to task is related to anxiety and depressiveness in normal subjects. Psychiatry and Clinical Neurosciences. 2008;62(5):603–609. doi: 10.1111/j.1440-1819.2008.01855.x. [DOI] [PubMed] [Google Scholar]
- Silvia PJ, Jackson BA, Sopko RS. Does baseline heart rate variability reflect stable positive emotionality? Personality and Individual Differences. 2014;70:183–187. doi: 10.1016/j.paid.2014.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stange JP, Connolly SL, Burke TA, Hamilton JL, Hamlat EJ, Abramson LY, Alloy LB. Inflexible cognition predicts first onset of major depression in adolescence. Depression and Anxiety. doi: 10.1002/da.22513. in press-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stange JP, Hamilton JL, Olino TM, Fresco DM, Alloy LB. Autonomic reactivity and vulnerability to depression: A multi-wave study. Emotion. doi: 10.1037/emo0000254. in press-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stange JP, Molz Adams AR, O’Garro-Moore J, Weiss RB, Ong ML, Walshaw PD, Abramson LY, Alloy LB. Extreme cognitions in bipolar spectrum disorders: Associations with personality disorder characteristics and risk for episode recurrence. Behavior Therapy. 2015;46(2):242–256. doi: 10.1016/j.beth.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stange JP, Sylvia LG, Magalhães PV, Frank E, Otto MW, Miklowitz DJ, Deckersbach T. Extreme attributions predict transition from depression to mania or hypomania in bipolar disorder. Journal of Psychiatric Research. 2013b;47(10):1329–1336. doi: 10.1016/j.jpsychires.2013.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stange JP, Sylvia LG, Magalhães PV, Miklowitz DJ, Otto MW, Frank E, Deckersbach T. Explanatory flexibility, extreme attributions, and depressive symptoms and illness course in adults receiving psychosocial treatment for bipolar depression. Unpublished raw data. 2013a [Google Scholar]
- Stange JP, Sylvia LG, Magalhães PV, Miklowitz DJ, Otto MW, Frank E, Deckersbach T. Extreme attributions predict the course of bipolar depression: results from the STEP-BD randomized controlled trial of psychosocial treatment. Journal of Clinical Psychiatry. 2013c;74(3):249–255. doi: 10.4088/JCP.12m08019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syzdek MR, Addis ME. Adherence to masculine norms and attributional processes predict depressive symptoms in recently unemployed men. Cognitive Therapy and Research. 2010;34(6):533–543. [Google Scholar]
- Szöke A, Trandafir A, Dupont ME, Méary A, Schürhoff F, Leboyer M. Longitudinal studies of cognition in schizophrenia: meta-analysis. British Journal of Psychiatry. 2008;192(4):248–257. doi: 10.1192/bjp.bp.106.029009. [DOI] [PubMed] [Google Scholar]
- Thoma P, Zalewski I, von Reventlow HG, Norra C, Juckel G, Daum I. Cognitive and affective empathy in depression linked to executive control. Psychiatry Research. 2011;189(3):373–378. doi: 10.1016/j.psychres.2011.07.030. [DOI] [PubMed] [Google Scholar]
- Tonhajzerova I, Ondrejka I, Chladekova L, Farsky I, Visnovcova Z, Calkovska A, Javorka M. Heart rate time irreversibility is impaired in adolescent major depression. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2012;39(1):212–217. doi: 10.1016/j.pnpbp.2012.06.023. [DOI] [PubMed] [Google Scholar]
- Tonhajzerova I, Ondrejka I, Javorka M, Adamik P, Turianikova Z, Kerna V, Calkovska A. Respiratory sinus arrhythmia is reduced in adolescent major depressive disorder. European Journal of Medical Research. 2009;14(Suppl 4):280–283. doi: 10.1186/2047-783X-14-S4-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonhajzerova I, Ondrejka I, Javorka K, Turianikova Z, Farsky I, Javorka M. Cardiac autonomic regulation is impaired in girls with major depression. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2010;34(4):613–618. doi: 10.1016/j.pnpbp.2010.02.023. [DOI] [PubMed] [Google Scholar]
- Trivedi MH, Greer TL. Cognitive dysfunction in unipolar depression: Implications for treatment. Journal of Affective Disorders. 2014;152:19–27. doi: 10.1016/j.jad.2013.09.012. [DOI] [PubMed] [Google Scholar]
- Tucker P, Pfefferbaum B, Jeon-Slaughter H, Khan Q, Garton T. Emotional stress and heart rate variability measures associated with cardiovascular risk in relocated Katrina survivors. Psychosomatic Medicine. 2012;74(2):160–168. doi: 10.1097/PSY.0b013e318240a801. [DOI] [PubMed] [Google Scholar]
- Valentino K, Bridgett DJ, Hayden LC, Nuttall AK. Abuse, depressive symptoms, executive functioning, and overgeneral memory among a psychiatric sample of children and adolescents. Journal of Clinical Child & Adolescent Psychology. 2012;41(4):491–498. doi: 10.1080/15374416.2012.660689. [DOI] [PubMed] [Google Scholar]
- Vazquez L, Blood JD, Wu J, Chaplin TM, Hommer RE, Rutherford HJ, Crowley MJ. High frequency heart-rate variability predicts adolescent depressive symptoms, particularly anhedonia, across one year. Journal of Affective Disorders. 2016;196:243–247. doi: 10.1016/j.jad.2016.02.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vergara-Lopez C, Lopez-Vergara HI, Colder CR. Executive functioning moderates the relationship between motivation and adolescent depressive symptoms. Personality and Individual Differences. 2013;54(1):18–22. doi: 10.1016/j.paid.2012.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vergara-Lopez C, Lopez-Vergara HI, Roberts JE. Testing a “content meets process” model of depression vulnerability and rumination: Exploring the moderating role of set-shifting deficits. Journal of Behavior Therapy and Experimental Psychiatry. 2016;50:201–208. doi: 10.1016/j.jbtep.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vilgis V, Silk TJ, Vance A. Executive function and attention in children and adolescents with depressive disorders: a systematic review. European Child and Adolescent Psychiatry. 2015;24(4):365–384. doi: 10.1007/s00787-015-0675-7. [DOI] [PubMed] [Google Scholar]
- Voss A, Boettger MK, Schulz S, Gross K, Bär KJ. Gender-dependent impact of major depression on autonomic cardiovascular modulation. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2011;35(4):1131–1138. doi: 10.1016/j.pnpbp.2011.03.015. [DOI] [PubMed] [Google Scholar]
- Vriezekolk JE, van Lankveld WG, Eijsbouts AM, van Helmond T, Geenen R, van den Ende CH. The coping flexibility questionnaire: development and initial validation in patients with chronic rheumatic diseases. Rheumatology International. 2012;32(8):2383–2391. doi: 10.1007/s00296-011-1975-y. [DOI] [PubMed] [Google Scholar]
- Wagner CA, Alloy LB, Abramson LY. Trait rumination, depression, and executive functions in early adolescence. Journal of Youth and Adolescence. 2015;44(1):18–36. doi: 10.1007/s10964-014-0133-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitmer AJ, Gotlib IH. Switching and backward inhibition in major depressive disorder: the role of rumination. Journal of Abnormal Psychology. 2012;121(3):570–578. doi: 10.1037/a0027474. [DOI] [PubMed] [Google Scholar]
- Yaroslavsky I, Rottenberg J, Bylsma LM, Jennings JR, George C, Baji I, Kovacs M. Parasympathetic nervous system activity predicts mood repair use and its effectiveness among adolescents with and without histories of major depression. Journal of Abnormal Psychology. 2016;125(3):323–336. doi: 10.1037/abn0000149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaroslavsky I, Rottenberg J, Kovacs M. Atypical patterns of respiratory sinus arrhythmia index an endophenotype for depression. Development and Psychopathology. 2014;26(4pt2):1337–1352. doi: 10.1017/S0954579414001060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh TC, Kao LC, Tzeng NS, Kuo TB, Huang SY, Chang CC, Chang HA. Heart rate variability in major depressive disorder and after antidepressant treatment with agomelatine and paroxetine: Findings from the Taiwan Study of Depression and Anxiety (TAISDA) Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2016;64:60–67. doi: 10.1016/j.pnpbp.2015.07.007. [DOI] [PubMed] [Google Scholar]
- Yochim BP, Mueller AE, Segal DL. Late life anxiety is associated with decreased memory and executive functioning in community dwelling older adults. Journal of Anxiety Disorders. 2013;27(6):567–575. doi: 10.1016/j.janxdis.2012.10.010. [DOI] [PubMed] [Google Scholar]
- Zahodne LB, Nowinski CJ, Gershon RC, Manly JJ. Which psychosocial factors best predict cognitive performance in older adults? Journal of the International Neuropsychological Society. 2014;20(05):487–495. doi: 10.1017/S1355617714000186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zong JG, Chan RC, Stone WS, His X, Cao XY, Zhao Q, Wang Y. Coping flexibility in young adults: comparison between subjects with and without schizotypal personality features. Schizophrenia Research. 2010a;122:185–192. doi: 10.1016/j.schres.2010.04.013. [DOI] [PubMed] [Google Scholar]
- Zong JG, Cao XY, Cao Y, Shi YF, Wang YN, Yan C, Chan RC. Coping flexibility in college students with depressive symptoms. Health and Quality of Life Outcomes. 2010b;8:66. doi: 10.1186/1477-7525-8-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Footnotes
Throughout the manuscript, when we refer to “depression” (e.g., “vulnerability to depression”) we are referring broadly to symptoms, episodes, and/or diagnoses of depression (MDD). In the review of specific studies, we specify when studies involved symptoms, episodes, or diagnoses of depression.
Contributor Information
Jonathan P. Stange, University of Illinois at Chicago
Lauren B. Alloy, Temple University
David M. Fresco, Kent State University
References
- Abramson LY, Metalsky GI, Alloy LB. Hopelessness depression: A theory-based subtype of depression. Psychological Review. 1989;96(2):358–372. [Google Scholar]
- Abramson LY, Seligman ME, Teasdale JD. Learned helplessness in humans: critique and reformulation. Journal of Abnormal Psychology. 1978;87(1):49–74. [PubMed] [Google Scholar]
- Aldao A. The future of emotion regulation research: Capturing context. Perspectives on Psychological Science. 2013;8(2):155–172. doi: 10.1177/1745691612459518. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S. The influence of context on the implementation of adaptive emotion regulation strategies. Behaviour Research and Therapy. 2012;50(7):493–501. doi: 10.1016/j.brat.2012.04.004. [DOI] [PubMed] [Google Scholar]
- Aldao A, Sheppes G, Gross JJ. Emotion regulation flexibility. Cognitive Therapy and Research. 2015;39(3):263–278. [Google Scholar]
- Alloy LB, Salk R, Stange JP, Abramson LY. Cognitive vulnerability and unipolar depression. In: DeRubeis RJ, Strunk DR, editors. The Oxford Handbook of Mood Disorders. New York: Oxford University Press; (in press) [Google Scholar]
- Bonanno GA, Burton CL. Regulatory flexibility: An individual differences perspective on coping and emotion regulation. Perspectives on Psychological Science. 2013;8(6):591–612. doi: 10.1177/1745691613504116. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Papa A, Lalande K, Westphal M, Coifman K. The importance of being flexible: The ability to both enhance and suppress emotional expression predicts long-term adjustment. Psychological Science. 2004;15(7):482–487. doi: 10.1111/j.0956-7976.2004.00705.x. [DOI] [PubMed] [Google Scholar]
- Brown JD, Siegel JM. Attributions for negative life events and depression: The role of perceived control. Journal of Personality and Social Psychology. 1988;54(2):316–322. doi: 10.1037//0022-3514.54.2.316. [DOI] [PubMed] [Google Scholar]
- Burcusa SL, Iacono WG. Risk for recurrence in depression. Clinical Psychology Review. 2007;27(8):959–985. doi: 10.1016/j.cpr.2007.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng C. Assessing coping flexibility in real-life and laboratory settings: a multimethod approach. Journal of Personality and Social Psychology. 2001;80(5):814–833. doi: 10.1037//0022-3514.80.5.814. [DOI] [PubMed] [Google Scholar]
- Cheng C, Kogan A, Chio JHM. The effectiveness of a new, coping flexibility intervention as compared with a cognitive-behavioural intervention in managing work stress. Work & Stress. 2012;26(3):272–288. [Google Scholar]
- Cheng C, Lau HPB, Chan MPS. Coping flexibility and psychological adjustment to stressful life changes: A meta-analytic review. Psychological Bulletin. 2014;140(6):1582–1607. doi: 10.1037/a0037913. [DOI] [PubMed] [Google Scholar]
- De Lissnyder E, Koster EH, De Raedt R. Emotional interference in working memory is related to rumination. Cognitive Therapy and Research. 2012a;36(4):348–357. [Google Scholar]
- De Lissnyder E, Koster EH, Everaert J, Schacht R, Van den Abeele D, De Raedt R. Internal cognitive control in clinical depression: General but no emotion-specific impairments. Psychiatry Research. 2012b;199(2):124–130. doi: 10.1016/j.psychres.2012.04.019. [DOI] [PubMed] [Google Scholar]
- Delis DC, Kaplan E, Kramer J. Delis-Kaplan Executive Function System. San Antonio, TX: Psychological Corporation; 2001. [Google Scholar]
- Dobson KS, Dozois DJ. Risk factors in depression. San Diego: Academic Press; 2008. [Google Scholar]
- Feldman G, Lavallee J, Gildawie K, Greeson JM. Dispositional mindfulness uncouples physiological and emotional reactivity to a laboratory stressor and emotional reactivity to executive functioning lapses in daily life. Mindfulness. 2016 doi: 10.1007/s12671-015-0487-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fresco DM, Heimberg RG, Abramowitz A, Bertram TL. The effect of a negative mood priming challenge on dysfunctional attitudes, explanatory style, and explanatory flexibility. British Journal of Clinical Psychology. 2006b;45:167–183. doi: 10.1348/014466505X35137. [DOI] [PubMed] [Google Scholar]
- Fresco DM, Mennin DS, Heimberg RG, Ritter M. Emotion regulation therapy for generalized anxiety disorder. Cognitive and Behavioral Practice. 2013;20(3):282–300. doi: 10.1016/j.cbpra.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fresco DM, Rytwinski NK, Craighead LW. Explanatory flexibility and negative life events interact to predict depression symptoms. Journal of Social and Clinical Psychology. 2007a;26:595–608. [Google Scholar]
- Fresco DM, Segal ZV, Buis T, Kennedy S. Relationship of posttreatment decentering and cognitive reactivity to relapse in major depression. Journal of Consulting and Clinical Psychology. 2007b;75(3):447–455. doi: 10.1037/0022-006X.75.3.447. [DOI] [PubMed] [Google Scholar]
- Fresco DM, Williams NL, Nugent NR. Flexibility and negative affect: Examining the associations of explanatory flexibility and coping flexibility to each other and to depression and anxiety. Cognitive Therapy and Research. 2006a;30:201–210. [Google Scholar]
- Genet JJ, Malooly AM, Siemer M. Flexibility is not always adaptive: Affective flexibility and inflexibility predict rumination use in everyday life. Cognition & Emotion. 2013;27(4):685–695. doi: 10.1080/02699931.2012.733351. [DOI] [PubMed] [Google Scholar]
- Genet JJ, Siemer M. Flexible control in processing affective and non-affective material predicts individual differences in trait resilience. Cognition & Emotion. 2011;25(2):380–388. doi: 10.1080/02699931.2010.491647. [DOI] [PubMed] [Google Scholar]
- Goldberg E. The executive brain: Frontal lobes and the civilized mind. New York: Oxford University Press; 2001. [Google Scholar]
- Haeffel GJ, Gibb BE, Metalsky GI, Alloy LB, Abramson LY, Hankin BL, Swendsen JD. Measuring cognitive vulnerability to depression: Development and validation of the cognitive style questionnaire. Clinical Psychology Review. 2008;28(5):824–836. doi: 10.1016/j.cpr.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy. 2006;44(1):1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Heaton RK. Wisconsin card sorting test: computer version 2. Odessa: Psychological Assessment Resources; 1993. [DOI] [PubMed] [Google Scholar]
- Hollenstein T, Lichtwarck-Aschoff A, Potworowski G. A model of socioemotional flexibility at three time scales. Emotion Review. 2013;5(4):397–405. [Google Scholar]
- Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science. 2011;6(6):537–559. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Carver CS, Fulford D. Goal dysregulation in the affective disorders. In: Kring AM, Sloan DM, editors. Emotion regulation and psychopathology: A transdiagnostic approach to etiology and treatment. New York: Guilford; 2010. pp. 204–228. [Google Scholar]
- Joormann J, Siemer M. Affective processing and emotion regulation in dysphoria and depression: cognitive biases and deficits in cognitive control. Social and Personality Psychology Compass. 2011;5(1):13–28. [Google Scholar]
- Just N, Abramson LY, Alloy LB. Remitted depression studies as tests of the cognitive vulnerability hypotheses of depression onset: A critique and conceptual analysis. Clinical Psychology Review. 2001;21(1):63–83. doi: 10.1016/s0272-7358(99)00035-5. [DOI] [PubMed] [Google Scholar]
- Kang Y, Gruber J, Gray JR. Mindfulness and de-automatization. Emotion Review. 2013;5(2):192–201. [Google Scholar]
- Kashdan TB, Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review. 2010;30(7):865–878. doi: 10.1016/j.cpr.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kato T. Development of the Coping Flexibility Scale: evidence for the coping flexibility hypothesis. Journal of Counseling Psychology. 2012;59(2):262. doi: 10.1037/a0027770. [DOI] [PubMed] [Google Scholar]
- Kemp AH, Quintana DS, Gray MA, Felmingham KL, Brown K, Gatt JM. Impact of depression and antidepressant treatment on heart rate variability: a review and meta-analysis. Biological Psychiatry. 2010;67(11):1067–1074. doi: 10.1016/j.biopsych.2009.12.012. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Wang PS. Epidemiology of depression. In: Gotlib IH, Hammen CL, editors. Handbook of depression. 2nd. New York: Guilford; 2009. pp. 5–22. [Google Scholar]
- Koster EH, De Lissnyder E, De Raedt R. Rumination is characterized by valence-specific impairments in switching of attention. Acta psychologica. 2013;144(3):563–570. doi: 10.1016/j.actpsy.2013.09.008. [DOI] [PubMed] [Google Scholar]
- Lam CB, McBride-Chang CA. Resilience in young adulthood: The moderating influences of gender-related personality traits and coping flexibility. Sex Roles. 2007;56:159–172. [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984. [Google Scholar]
- Lee RS, Hermens DF, Porter MA, Redoblado-Hodge MA. A meta-analysis of cognitive deficits in first-episode major depressive disorder. Journal of Affective Disorders. 2012;140(2):113–124. doi: 10.1016/j.jad.2011.10.023. [DOI] [PubMed] [Google Scholar]
- Malooly AM, Genet JJ, Siemer M. Individual differences in reappraisal effectiveness: The role of affective flexibility. Emotion. 2013;13(2):302–313. doi: 10.1037/a0029980. [DOI] [PubMed] [Google Scholar]
- Marcovitch S, Leigh J, Calkins SD, Leerks EM, O'Brien M, Blankson AN. Moderate vagal withdrawal in 3.5-year-old children is associated with optimal performance on executive function tasks. Developmental Psychobiology. 2010;52(6):603–608. doi: 10.1002/dev.20462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mennin DS, Ellard KK, Fresco DM, Gross JJ. United we stand: Emphasizing commonalities across cognitive-behavioral therapies. Behavior Therapy. 2013;44(2):234–248. doi: 10.1016/j.beth.2013.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mennin DS, Fresco DM. What, Me Worry and Ruminate About DSM-5 and RDoC? The Importance of Targeting Negative Self-Referential Processing. Clinical Psychology: Science and Practice. 2013;20:258–267. doi: 10.1111/cpsp.12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mennin DS, Fresco DM. Emotion regulation therapy. In: Gross JJ, editor. Handbook of Emotion Regulation. 2nd. New York: Guilford Press; 2014. pp. 469–490. [Google Scholar]
- Mennin DS, Fresco DM, Heimberg RG, O'Toole M. A randomized controlled trial of Emotion Regulation Therapy for generalized anxiety and co-occurring depression. doi: 10.1037/ccp0000289. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mennin DS, Fresco DM, Ritter M, Heimberg RG. An open trial of emotion regulation therapy for generalized anxiety disorder and cooccurring depression. Depression and Anxiety. 2015;32(8):614–623. doi: 10.1002/da.22377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A, Wager TD. The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: A latent variable analysis. Cognitive Psychology. 2000;41(1):49–100. doi: 10.1006/cogp.1999.0734. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Slavich GM, Georgiades K. The social environment and life stress in depression. In: Gotlib IH, Hammen CL, editors. Handbook of Depression. New York: Guilford; 2009. pp. 340–360. [Google Scholar]
- Moore MT, Fresco DM. The relationship of explanatory flexibility to explanatory style. Behavior Therapy. 2007;38(4):325–332. doi: 10.1016/j.beth.2006.06.007. [DOI] [PubMed] [Google Scholar]
- Murphy FC, Michael A, Sahakian BJ. Emotion modulates cognitive flexibility in patients with major depression. Psychological Medicine. 2012;42(7):1373–1382. doi: 10.1017/S0033291711002418. [DOI] [PubMed] [Google Scholar]
- Murphy FC, Sahakian BJ, Rubinsztein JS, Michael A, Rogers RD, Robbins TW, Paykel ES. Emotional bias and inhibitory control processes in mania and depression. Psychological Medicine. 1999;29(6):1307–1321. doi: 10.1017/s0033291799001233. [DOI] [PubMed] [Google Scholar]
- Naemi BD, Beal DJ, Payne SC. Personality predictors of extreme response style. Journal of Personality. 2009;77(1):261–286. doi: 10.1111/j.1467-6494.2008.00545.x. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspectives on Psychological Science. 2008;3(5):400–424. doi: 10.1111/j.1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- Peterson C, Semmel A, von Baeyer C, Abramson LY, Metalsky GI, Seligman ME. The attributional style questionnaire. Cognitive Therapy and Research. 1982;6(3):287–299. [Google Scholar]
- Reitan RM. Trail Making Test: Manual for administration and scoring. Reitan Neuropsychology Laboratory; 1992. [Google Scholar]
- Remue J, Vanderhasselt MA, Baeken C, Rossi V, Tullo J, De Raedt R. The effect of a single HF-rTMS session over the left DLPFC on the physiological stress response as measured by heart rate variability. Neuropsychology. 2016 doi: 10.1037/neu0000255. [DOI] [PubMed] [Google Scholar]
- Riskind JH, Alloy LB. Cognitive vulnerability to emotional disorders: Theory and research design/methodology. In: Alloy LB, Riskind JH, editors. Cognitive vulnerability to emotional disorders. Mahwah, NJ: Lawrence Erlbaum; 2006. pp. 1–29. [Google Scholar]
- Rottenberg J. Cardiac vagal control in depression: a critical analysis. Biological Psychology. 2007b;74(2):200–211. doi: 10.1016/j.biopsycho.2005.08.010. [DOI] [PubMed] [Google Scholar]
- Rottenberg J. Major depressive disorder: Emerging evidence for emotion context insensitivity. In: Rottenberg J, Johnson SL, editors. Emotion and psychopathology: Bridging affective and clinical science. Washington, DC: American Psychological Association; 2007a. pp. 151–165. [Google Scholar]
- Rottenberg J, Salomon K, Gross JJ, Gotlib IH. Vagal withdrawal to a sad film predicts subsequent recovery from depression. Psychophysiology. 2005;42(3):277–281. doi: 10.1111/j.1469-8986.2005.00289.x. [DOI] [PubMed] [Google Scholar]
- Sanislow CA, Pine DS, Quinn KJ, Kozak MJ, Garvey MA, Heinssen RK, Cuthbert BN. Developing constructs for psychopathology research: research domain criteria. Journal of Abnormal Psychology. 2010;119(4):631–639. doi: 10.1037/a0020909. [DOI] [PubMed] [Google Scholar]
- Siegle GJ, Price RB, Jones NP, Ghinassi F, Painter T, Thase ME. You gotta work at it pupillary indices of task focus are prognostic for response to a neurocognitive intervention for rumination in depression. Clinical Psychological Science. 2014;2(4):455–471. [Google Scholar]
- Siepmann M, Aykac V, Unterdörfer J, Petrowski K, Mueck-Weymann M. A pilot study on the effects of heart rate variability biofeedback in patients with depression and in healthy subjects. Applied Psychophysiology and Biofeedback. 2008;33(4):195–201. doi: 10.1007/s10484-008-9064-z. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Moore RG, Hayhurst H, Pope M, Williams S, Segal ZV. Metacognitive awareness and prevention of relapse in depression: empirical evidence. Journal of Consulting and Clinical Psychology. 2002;70(2):275–287. doi: 10.1037//0022-006x.70.2.275. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Scott J, Moore RG, Hayhurst H, Pope M, Paykel ES. How does cognitive therapy prevent relapse in residual depression? Evidence from a controlled trial. Journal of Consulting and Clinical Psychology. 2001;69(3):347–357. doi: 10.1037//0022-006x.69.3.347. [DOI] [PubMed] [Google Scholar]
- Teper R, Segal ZV, Inzlicht M. Inside the mindful mind: How mindfulness enhances emotion regulation through improvements in executive control. Current Directions in Psychological Science. 2013;22(6):449–454. [Google Scholar]
- Thayer JF, Lane RD. Claude Bernard and the heart–brain connection: Further elaboration of a model of neurovisceral integration. Neuroscience & Biobehavioral Reviews. 2009;33(2):81–88. doi: 10.1016/j.neubiorev.2008.08.004. [DOI] [PubMed] [Google Scholar]
- Wagner S, Doering B, Helmreich I, Lieb K, Tadić A. A meta-analysis of executive dysfunctions in unipolar major depressive disorder without psychotic symptoms and their changes during antidepressant treatment. Acta Psychiatrica Scandinavica. 2012;125(4):281–292. doi: 10.1111/j.1600-0447.2011.01762.x. [DOI] [PubMed] [Google Scholar]
- Wells A. Metacognitive therapy for anxiety and depression. New York: Guilford; 2011. [Google Scholar]
- Wells A, Matthews G. Modelling cognition in emotional disorder: The S-REF model. Behaviour Research and Therapy. 1996;34(11):881–888. doi: 10.1016/s0005-7967(96)00050-2. [DOI] [PubMed] [Google Scholar]
- Whitfield-Gabrieli S, Ford JM. Default mode network activity and connectivity in psychopathology. Annual Review of Clinical Psychology. 2012;8:49–76. doi: 10.1146/annurev-clinpsy-032511-143049. [DOI] [PubMed] [Google Scholar]
- Williams JMG. Mindfulness, depression and modes of mind. Cognitive Therapy and Research. 2008;32(6):721–733. [Google Scholar]