Supplemental Digital Content is available in the text.
Abstract
Background:
The inverted T/keyhole pattern is commonly used for large breast reductions. This technique relies on the breast skin to retain the shape. With the passage of time “fallout” (pseudoptosis) occurs impairing the cosmetic result. A technique is described that uses parenchymal sutures and inframammary fold (IMF) reinforcement sutures to maintain the intraoperative shape.
Methods:
A retrospective study of 25 consecutive patients (50 breasts) where the IMF was reinforced and parenchymal sutures were inserted. The patients were followed up and the nipple to notch and nipple to IMF distance was measured and compared with that marked preoperatively and set intraoperatively. Complications, especially T junction breakdown, were also recorded.
Results:
The mean age was 38 years (range, 16–62 years) with a mean follow-up of 12 months. The mean body mass index was 31 (range, 22–41). The mean mass of tissue excised was 925 g (range, 340–1,800 g) per side. The distance from the suprasternal notch to the nipple remained unchanged. The distance from the nipple to the IMF remained the same as that marked preoperatively except in 3 patients who developed pseudoptosis. Only 3 patients had wound dehiscence.
Conclusion:
Parenchymal and superficial fascial system sutures combined with IMF reinforcement contributes to maintaining the aesthetic result and decreasing complications, in weight stable patients.
INTRODUCTION
Breast reduction has become a routine procedure,1–3 even in patients with gigantomastia.4,5 The Wise keyhole/inverted T pattern is commonly used to reduce larger breasts.1–5 Advances in the understanding of the blood supply to the nipple areolar complex have resulted in less nipple areolar complex ischemia.6 Short-term complications are usually self limiting—commonly the T point (sometimes called the angle of sorrow) undergoes necrosis and/or dehiscence.
However, while the common complications are self-limiting, the aesthetic result may deteriorate with time.1 In particular, “bottoming out” (dropout) occurs. This is due to the effect of gravity in that the tissue descends to the inferior pole. This is reflected as a lengthening of the distance between the nipple and the inframammary fold (IMF), leading to pseudoptosis and impairment of the initial aesthetic result.
A number of parenchymal suture modifications have been applied to the Wise keyhole/inverted T with a superomedial pedicle in an endeavor to reduce complications and also improve the long-term aesthetic outcome. The results of these maneuvers are reported in 25 consecutive patients undergoing breast reduction during a 26-month period.
METHODS
The breast is marked standing. The distance from the suprasternal notch to the nipple and the distance from the nipple to the IMF are measured in centimeters and recorded. The Wise keyhole/inverted T is marked preoperatively with the new nipple position set at the level of the projected IMF.
The distance from the suprasternal notch to the planned new nipple position was recorded, as well as the planned length of the vertical limb of the keyhole/inverted T. These measurements were subsequently measured at all the postoperative visits and compared with the measurements set preoperatively. To account for observer bias, a difference of > 1 cm from that marked preoperatively (and set intraoperatively) was considered as leading to pseudoptosis.
A retrospective study was performed on 25 consecutive patients (50 breasts) undergoing breast reduction. Data captured included age, body mass index (BMI), and associated illnesses, including smoking. The amount of breast tissue excised (in grams) was also noted, as well as the total volume removed by liposuction. Additionally, complications were recorded, and the follow-up period was noted. Only patients with a follow-up greater than 6 months were included. Exclusion criteria were mastopexy or revision surgery. Wound dehiscence at the T was defined as a defect greater than 1 × 1 cm and/or requiring more than 10 days of dressings to heal. The study was approved by the local ethics committee.
RESULTS
There were 27 patients entered into the study. One patient became pregnant after her reduction and was excluded. Another was lost to follow-up after 4 months and also excluded, leaving 25 patients for assessment. Only patients with a follow-up of at least 6 months were included in the study.
The average age of the patients was 38 years (range, 16–62 years). The average BMI was 31 (range, 22–41). Fourteen patients had a preoperative BMI of 30 or more. Three of the 25 patients were active smokers. The average mass of tissue excised was 925 g per side (range, 340–1,800 g). The average volume of aspirate after liposuction of the axilla was approximately 200 ml/side.
The distance from the suprasternal notch to the new nipple position remained at the level set preoperatively in all patients. The nipple to IMF distance also remained at the level set preoperatively in all but 3 patients (Table 1). One patient had a history of marked weight fluctuation. Her preoperative BMI was 32. She had had a BMI of 39 at a consultation a few years previously. She had multiple stretch marks on her breasts and very thin skin. She also developed wound dehiscence. The other patient, also with a history of weight fluctuation, had a preoperative BMI of 33. The third patient, also a smoker, had lost 10 kg at her postoperative visit at 10 months.
Table 1.
Patient Characteristics
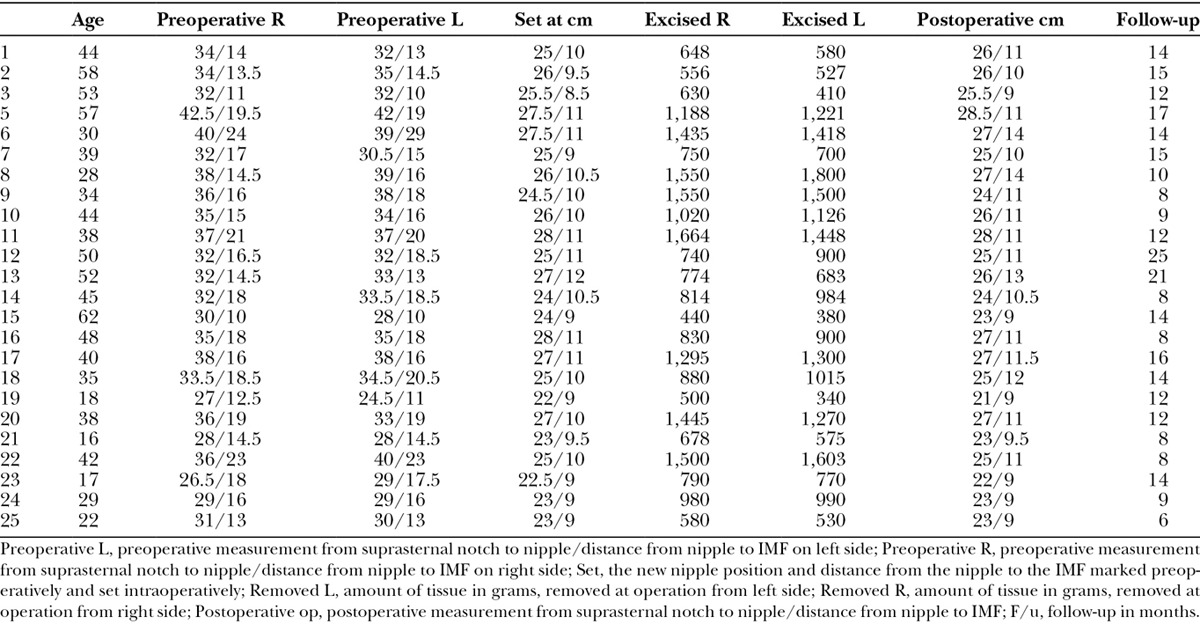
In the 3 patients who developed lengthening of the distance from the nipple to the IMF, this was already evident at 3 months postoperatively. There were no infections. Flap dehiscence at the T occurred in 3 patients (12%.) All patients had a BMI > 30, with 1 patient having a BMI of 41. One of these patients smoked 10 cigarettes a day. Another patient had lost 15 kg before surgery but was unable to reach her desired weight. One patient had persistent bogginess of her axilla for 2 months postoperatively, and this resolved with conservative treatment. There were no seromas in this study clinically.The mean follow-up was 12 months (range, 6–25 months).
TECHNICAL ASPECTS
1. Liposuction of the axilla7 is performed, using the SAFE technique8 after infiltration of tumescent fluid.
2. The supero medial pedicle is always used, and a backcut of the pedicle is always performed.
3. The IMF is then reinforced and secured using a 1/0 vicryl suture (see video Supplemental Digital Content 1, which shows the insertion of IMF suture at the meridian of the breast. The blue line marks the midline of the breast. The video is filmed from above (cranial) the patient. This video is available in the “Related Videos” section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A517). At the midpoint of the breast, a mattress suture is made by passing the needle through Scarpa’s fascia [superficial fascial system (SFS)], then along rib periosteum and then back through Scarpa’s fascia (SFS) and tied (Fig. 1). The IMF is seen to invert slightly at the meridian of the breast as the suture is tied.
Fig. 1.
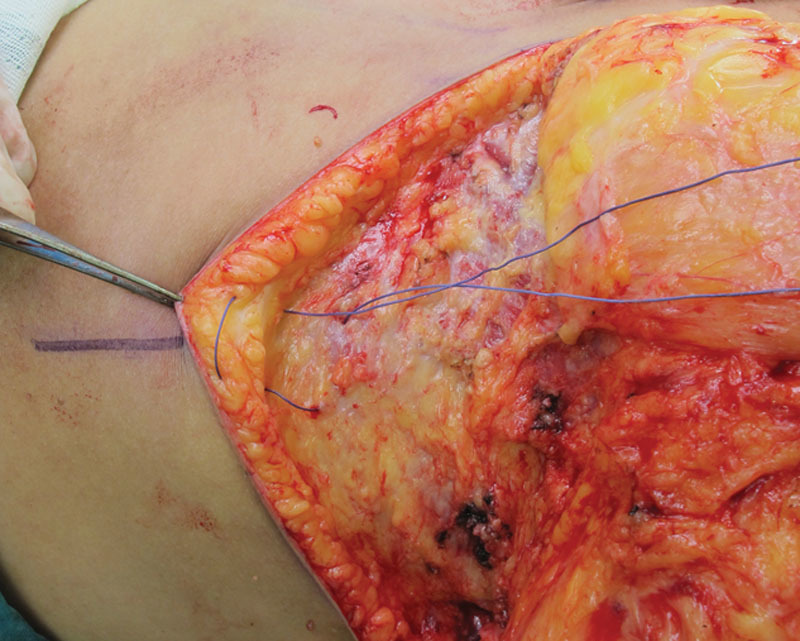
Insertion of inframammary suture at the breast meridian. The mattress suture passes from Scarpa’s fascia (SFS) through rib periosteum and back through Scarpa’s fascia (SFS). Another 2 sutures are inserted equilaterally (medial and lateral to this suture) along the IMF. A forceps retracts the skin. The blue line marks the breast meridian.
The IMF is also reinforced medially and laterally but using the pectoral fascia as the buttress for the suture
4. Quilting/deep parenchymal sutures are inserted from both the medial and lateral skin flaps to the pectoral fascia. Usually 2 or 3 sutures are used for both the medial and lateral flaps (similar to quilting in abdominoplasty9; Fig. 2).
Fig. 2.
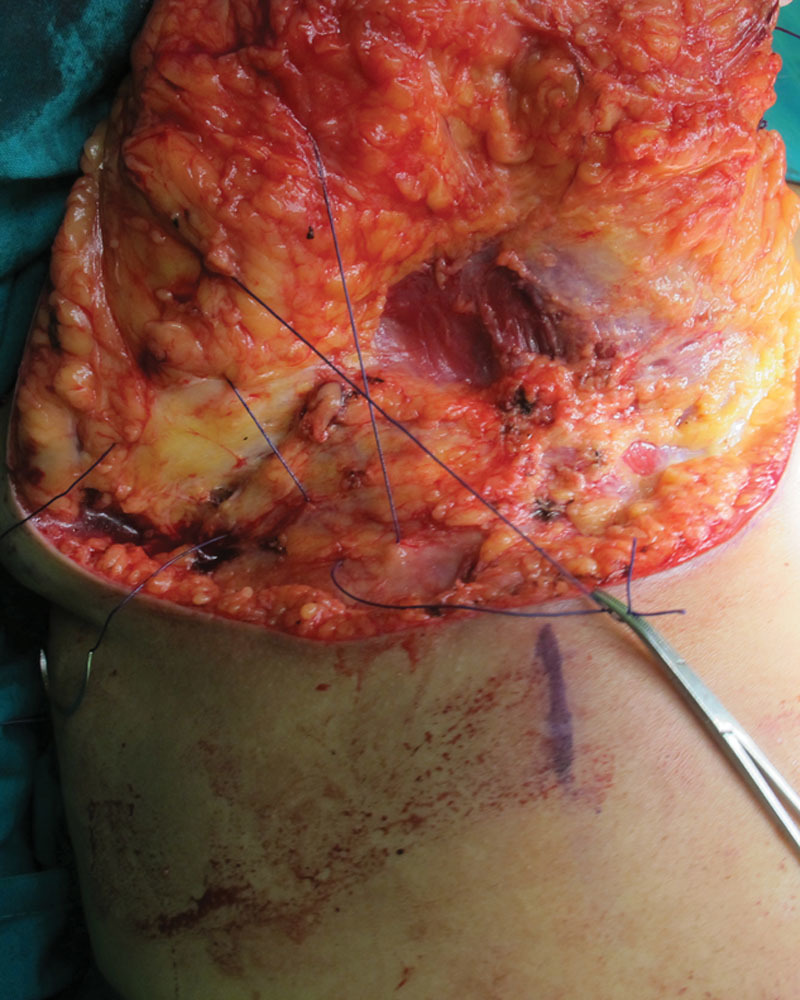
Parenchymal (quilting) sutures pass from the medial and (lateral) breast flaps through the pectoral fascia. In this photograph, the lateral quilting sutures are being inserted. View from lateral of right breast, surgeon standing to right of the patient.
Similarly, the undersurface/deep layer of the “pillar” is also secured to the pectoral fascia.
5. Superficial fascial system (SFS) sutures are inserted.10 These suture pass from (SFS) Scarpa’s fascia of the superior skin flap through (SFS) Scarpa’s fascia of the lower breast incision and also take a bite of pectoral fascia (see video Supplemental Digital Content 2, which shows the insertion of the SFS (Scarpa’s fascial sutures) beginning at the medial aspect of the breast. This video is available in the “Related Videos” section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A518). These sutures are inserted along the whole of the length of the inferior incision.
These sutures reduce the tension required when closing the skin along the horizontal incision.
DISCUSSION
The original Wise keyhole pattern/inverted T is one of the commonest techniques used in breast reduction.11 It removes excess tissue in both a horizontal and vertical plane and is advantageous in the patient with a raised BMI or gigantomastia.1–5 In fact, Wise designed the skin pattern as a skin brassiere: this technique relies mainly on the quality of the skin to maintain the breast shape.1,12 However, “bottoming out” commonly follows.1 Additionally, tension at the T junction often results in flap dehiscence and delayed wound healing.13
Pseudoptosis (bottoming out) is a common sequel following breast reduction2 leading to impairment of the cosmetic result. This occurs due to descent of tissue to the inferior pole of the breast, creating more volume in the inferior pole of the breast. The increased volume of tissue stretches the overlying skin, increasing the distance between nipple and IMF. In the original Wise design, the elasticity of the skin could limit this lengthening from occurring. Now 3 maneuvers are designed to retard tissue descent into the inferior pole. First, quilting sutures (Fig. 2) are inserted to appose and fix the breast parenchyma/skin flaps to the chest wall/pectoralis fascia. Second, the pedicle is propped up and supported with pillar sutures, which are also secured to the pectoral fascia. Third, both the IMF (Fig. 1, video 1) and Scarpa’s fascia/SFS10 are also fixed (video 2) to the pectoral fascia (IMF is fixed centrally to rib periosteum). The value of these maneuvers is shown in this study where the distance from the nipple to the IMF (Table 1) remained relatively static (Figs. 3, 4) at a mean of 12 months in 88% of patients.
Video Graphic 1.

See video Supplemental Digital Content 1, which shows the insertion of IMF suture at the meridian of the breast. The blue line marks the midline of the breast. The video is filmed from above (cranial) the patient. This video is available in the “Related Videos” section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A517.
Video Graphic 2.

See video Supplemental Digital Content 2, which shows the insertion of the SFS (Scarpa’s fascial sutures) beginning at the medial aspect of the breast. This video is available in the “Related Videos” section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A518.
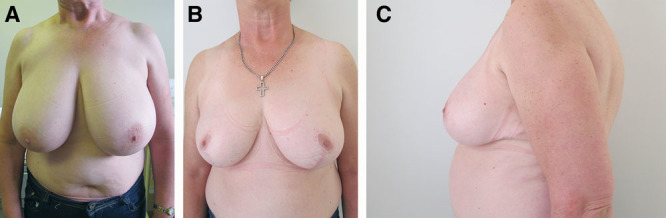
Fig. 3.
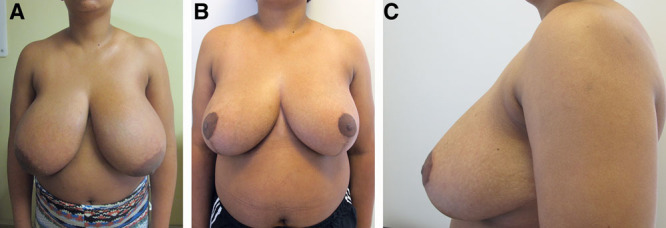
A, A preoperative anterior view of a 40-year-old patient (BMI, 29; number 17 in Table 1) B, One thousand two hundred ninety-five grams removed from the right breast, and 1,300 g removed from her left breast, now 16 months postoperatively. C, Lateral view.
Fig. 4.
A, A 50-year-old lady (BMI, 30), preoperative anterior view (number 12 in Table 1) who had 740 g removed from her right breast and 900 g removed from her left breast (B), now 25 months postoperatively. C, Lateral view.
It is recognized that the IMF descends with age14 and in patients with a raised BMI. IMF asymmetry and position have been investigated in patients seeking breast augmentation,15 and reinforcement of the IMF is well described in breast augmentation, but curiously has received little attention in breast reduction. The purpose of reinforcing the IMF is two-fold: to fix and secure the position of the IMF to prevent further descent. If the IMF is not fixed and secured, the horizontal scar of the inverted T will remain more or less where it was set intraoperatively, but the IMF will descend below the scar (Fig. 5).
Fig. 5.

Patient (not included in this study) in whom the IMF was not fixed as described, now 2 1/2 years postoperatively. Pseudoptosis has occurred and a “new” IMF has been formed (blue line) below the inframmamary scar. The inframammary scar (stippled black line) was originally set at the level of the IMF.
Another reason for securing the IMF is to reduce tension along the horizontal skin suture line. Consequently, there is less movement at the angle of sorrow and less wound dehiscence. This study had a T angle breakdown of 12%, which is deemed acceptable considering that resection weight and raised BMI are correlated with delayed wound healing.13 This is much less than in a similar study from the same unit.4 Additionally, the sutures that appose the SFS/Scarpa’s fascia (video 2) also help to oppose the skin flaps and further reduce tension during skin closure.
The quilting parenchymal sutures are applied deeply from breast parenchyma to pectoralis fascia, to secure the position of the lateral and medial skin flaps (Fig. 2). An additional advantage of these sutures is that dead space is obliterated; hence drains are not required. There were no seromas clinically in this series.
There are some disadvantages to this technique. It takes about 30 minutes longer to perform due to the extra sutures required. The patients often complain of pain along the reinforced IMF, and additional analgesia may be required. This technique cannot be applied where an inferior pedicle is used.
Ultimately, the results depend on the patient’s quality of tissue. In this study, 3 patients developed pseudoptosis. Two patients had very thin skin with multiple stretch marks and a history of weight fluctuation, whereas the third patient had lost 10 kg in the postoperative period. The thin skin is also reflected in the breast parenchymal tissue as attenuated Cooper’s ligaments which “cheese wire” when sutures are inserted. However, it is pleasing to note that most (88%) patients retained their breast shape postoperatively, and the distance from the nipple to the IMF remained unchanged after a mean follow-up of 12 months. Perhaps, another feature of this study is that in 9 patients who had gigantomastia (mean reduction of 1,262 g per side) 7 maintained the vertical length of the scar.
There are differing results reported in the literature regarding the change in length of the scar between the nipple and IMF postoperatively.7,16,17 Some studies examining outcome after vertical mammaplasty report that the scar length remains unchanged7; Matthews et al.,16 who followed up vertical mammaplasty patients, noted that the scar length increased weekly after surgery but then stabilized at 36 weeks—roughly 8 months. Souza et al.17 noted that patients with moderate breast hypertrophy (not defined) who underwent superior pedicle inverted T reductions developed an increase in the vertical limb of the scar. In the patients who developed pseudoptosis in this study, the vertical limb of the keyhole/inverted T was already lengthened after 3 months.
There are 2 unique aspects to this study. First, it appears that no other studies have investigated the change in length of the vertical scar using an inverted T combined with a superomedial pedicle. Second, this appears to be the first instance where the IMF was fixed. This means that if the horizontal aspect of the scar is fixed by the IMF suture, and tissue descends to the inferior pole, this will be reflected by an increase in length of the distance between nipple and the fixed IMF. It is our observation that where the IMF is not fixed, and pseudoptosis occurs, a new IMF is formed below the original scar (Fig. 5).
CONCLUSIONS
Previously, an inverted T/keyhole breast reduction depended on the quality of the skin to retain shape postoperatively. Now a number of parenchymal sutures and IMF reinforcement have been applied to reduce tissue descent. These sutures also reduce skin tension and splint the horizontal suture line. It is suggested that these technical modifications may improve the long-term aesthetic results, reducing the incidence of pseudoptosis, and the incidence of T point ischemia, of a commonly performed plastic surgical operation.
Supplementary Material
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Hall-Findley EJ, Shestak KC. Breast reduction. Plast Reconstr Surg. 2015;00136:531e–544e.. [DOI] [PubMed] [Google Scholar]
- 2.Nahai F, Nahai F. Breast reduction. Plast Reconstr Surg. 2008;121:1–13.. [DOI] [PubMed] [Google Scholar]
- 3.Davison SP, Mesbahi AN, Ducic I, et al. The versatility of the superomedial pedicle and various skin reduction patterns. Plast Reconstr Surg. 2001;107:693–699.. [DOI] [PubMed] [Google Scholar]
- 4.Landau AG, Hudson DA. Choosing the superomedial pedicle for reduction mammaplasty in gigantomastia. Plast Reconstr Surg. 2008;121:735–739.. [DOI] [PubMed] [Google Scholar]
- 5.Lugo LM, Prada M, Kohanzadeh S, et al. Surgical outcomes of gigantomastia breast reduction superomedial pedicle technique: a 12-year retrospective study. Ann Plast Surg. 2013;70:533–537.. [DOI] [PubMed] [Google Scholar]
- 6.Taylor GI, Corlett RJ, Dhar SC, et al. The anatomical (angiosome) and clinical territories of cutaneous perforating arteries: development of the concept and designing safe flaps. Plast Reconstr Surg. 2011;127:1447–1459.. [DOI] [PubMed] [Google Scholar]
- 7.Lista F, Austin RE, Singh Y, et al. Vertical scar reduction mammaplasty. Plast Reconstr Surg. 2015;136:23–25.. [DOI] [PubMed] [Google Scholar]
- 8.Wall S., Jr. SAFE circumferential liposuction with abdominoplasty. Clin Plast Surg. 2010;37:485–501.. [DOI] [PubMed] [Google Scholar]
- 9.Pollock H, Pollock T. Reducing abdominoplasty complications. Aesthet Surg J. 2002;22:475–476.. [DOI] [PubMed] [Google Scholar]
- 10.Lockwood TE. Superficial fascial system (SFS) of the trunk and extremities: a new concept. Plast Reconstr Surg. 1991;87:1009–1018.. [DOI] [PubMed] [Google Scholar]
- 11.Rohrich RJ, Gosman AA, Brown SA, et al. Current preferences for breast reduction techniques: a survey of board-certified plastic surgeons 2002. Plast Reconstr Surg. 2004;114:1724–1733.; discussion 1734. [DOI] [PubMed] [Google Scholar]
- 12.Tebbetts JB. A process for qualitifying aesthetic and functional breast surgery I: quantifying nipple position and vertical and horizontal skin excess for mastopexy and breast reduction. Plast Reconstr Surg. 2013;132:65–73.. [DOI] [PubMed] [Google Scholar]
- 13.Cunningham BL, Gear AJL, Kerrigan CL, Collins ED. Analysis of breast reduction complications derived from the BRAVO study. Plast Reconstr Surg. 2005;115:1597–1604.. [DOI] [PubMed] [Google Scholar]
- 14.Hammond DC. Atlas of Aesthetic Breast Surgery. 2009New York: Elsevier. [Google Scholar]
- 15.Yeslev M, Braun SA, Maxwell GP. Asymmetry of inframammary folds in patients undergoing augmentation mammaplasty. Aesthet Surg J. 2016;36:156–166.. [DOI] [PubMed] [Google Scholar]
- 16.Matthews JL, Oddone-Paolucci E, Lawson DM, et al. Vertical scar breast reduction: does gathering the incision matter? Ann Plast Surg. 2016;77:25–31.. [DOI] [PubMed] [Google Scholar]
- 17.Souza AA, Faiwichow L, Ferreira AA, et al. Comparative analysis of mammaplasty techniques based on the long term effect on nipple- areolar- complex to inframammary crease distance. Rev Bras Cir Plast. 2011;26:664–669.. [Google Scholar]


