Abstract
Introduction
Family factors are directly associated with the psychosocial adjustment of children with chronic illnesses such as asthma (Kaugars et al., 2004). Research indicates that negative family factors may also contribute to child disease severity via bio-behavioral mechanisms of effect. For instance, children from more conflicted families often experience greater internalizing symptoms that subsequently impact their asthma severity (Wood et al., 2006). These pathways have yet to be examined with a comprehensive focus on strength-based family factors. This study examined whether factors such as family cohesion, problem-solving abilities, and communication influence asthma severity via their effects on child depression and anxiety symptoms.
Methods
Participants were 215 children (136 males and 79 females), ages five to twelve years old, and their families. Primary caregiver, child, and teacher ratings of child and family functioning in addition to objective measures of parent-child interactions and asthma severity were collected.
Results
Using structural equation modeling, we identified significant indirect associations between family factors and child asthma severity via child depressive symptoms; however, these associations were not present in models with child anxiety symptoms.
Discussion
Results suggest an indirect effect of family functioning on children’s lung function, with differential roles of anxiety and depression in these pathways. This paper also highlights the importance of incorporating multi-rater multi-method measures to understand children’s experiences in pediatric asthma.
Keywords: pediatric asthma, family functioning, depression, anxiety, adaptation
Despite available preventative treatments, asthma prevalence continues to increase, with roughly 14% of children affected around the world (Global Asthma Network, 2014). In 2014, pediatric asthma affected more than seven million children in the United States, with a disproportionate amount of them being low-income and urban (Centers for Disease Control and Prevention, 2016). Approximately 49% of children with asthma report missing at least one day of school each year and 10.9 % report moderate to severe limitations in daily activities (Akinbami, 2012). Given high rates of poorly controlled asthma, public health research has focused on identifying factors that contribute to severity level and daily functioning. Whereas past studies have examined the effects of distinct family characteristics on child asthma outcomes, few studies have used strength-based, multi-rater, multi-method (MRMM) approaches to examining family effects on child pulmonary functioning via distinct anxiety and depression pathways (Fiese, Winter, & Botti, 2011; Wood et al., 2006).
Family Functioning and Child Well-Being
The family is the closest contextual system to a child, and therefore bidirectional associations between children and their families are important in understanding how various processes influence children’s well-being in the context of asthma (Spagnola & Fiese, 2010; Wood et al., 2006). The utility in examining the effects of protective family factors on outcomes in pediatric asthma lies in its ability to highlight family strengths associated with children’s resilience (e.g., better quality of life, less severe asthma, and lower functional severity).
Positive family factors that have been consistently emphasized in family systems models (e.g., Olson, Sprenkle, & Russell, 1979) and identified in developmental and pediatric asthma research include family communication, cohesion, and problem-solving abilities (Drotar & Bonner, 2009; Reichenberg & Anders, 2005). Positive family communication, typically defined as openness and members showing interest in and support for one-another’s statements during group interactions (Kaugars, Klinnert, & Bender, 2004), has been shown to predict quality of life (QOL) in children with asthma (Fiese et al., 2011). Cohesion, defined as cooperative interactions among family members, is also associated with better child outcomes such as higher self-worth and fewer emotional problems (Lindahl & Malik, 2001; Reichenberg & Anders, 2005). Finally, problem-solving, characterized by the family’s ability to face issues and resolve emotional upset that may arise, has been a target of pediatric psychosocial interventions (Herzer et al., 2011).
Family Functioning and Asthma Severity
Family functioning also influences disease management and health outcomes. Poor family functioning is theorized to foster more stress, which in turn causes physiological reactivity that influences asthma symptoms (e.g., Marin et al., 2009; Miller & Wood, 1997). The bio-behavioral family model (BBFM; Wood, 1994) proposes that familial contributions to the exacerbation of pediatric asthma occur through effects on children’s bio-behavioral reactivity (i.e., anxiety or depression; Wood et al., 2008). Children in families characterized by more negative emotional climates have reported more internalizing symptoms and poorer pulmonary function (Wood et al., 2015). Results are less conclusive when the effects of anxiety and depression symptoms on pulmonary function are examined separately. Associations between child depressive and asthma symptoms, albeit limited to cross-sectional studies, have been consistently identified even after controlling for anxiety symptoms (Goodwin et al., 2014; Wood et al., 2006). For anxiety, results are less clear; while some studies found direct associations between anxiety and asthma severity, others did not (McCauley et al., 2007; Wood et al., 2007).
One explanation for these discrepant findings is suggested by Miller’s Autonomic Dysregulation Model, which postulates that depression is linked to asthma severity via airway restriction. Depression is associated with a predominance of vagal/cholinergic reactivity over sympathetic reactivity to stress. This “vagal bias” constitutes vulnerability for children with asthma: when depressive symptoms are coupled with stress, the body experiences an increase in acetylcholine (ACH) production and bronchoconstriction (Miller et al., 2009).” Therefore, children with more depressive symptoms are expected to have increased asthma severity due to their heightened cholinergic states, vagal bias, and increased airway resistance. Other researchers suggest that many negative states, including irritability and panic, may relate to physical symptoms of atopic disorders by causing immune dysregulation (Kewalramani, Bollinger, & Postolache, 2008). Thus, differential associations of anxiety and depression with asthma symptomatology remain unclear.
This study was designed to examine mechanisms by which positive family characteristics (communication, cohesion, and problem-solving) are associated with asthma severity and adaptation. The proposed pathways were tested with structural equation models controlling for child age, sex, and medication adherence. We hypothesized significant, negative direct relationships between positive family factors and child anxiety and depressive symptoms. Additionally, we examined the differential effects of child depressive and anxiety symptoms on asthma symptom severity and adaptation, as defined by measures of subjective functional asthma severity, child reported QOL, and objective pulmonary functioning. Finally, we tested the distinct roles of child depressive and anxiety symptoms in mediating the effect of family positive factors on child asthma severity. In accord Miller’s ANS dysregulation model, it was predicted that child depressive symptoms would uniquely be associated with more severe asthma and would significantly mediate the effects of family positive factors on child asthma severity.
Methods
Participants
Participants were 215 children (136 males and 79 females), five to twelve years old (M = 7.86, SD = 2.18) and their families from the Institutional Review Board approved <blinded for submission> Project. Families were recruited from a hospital-based ambulatory clinic, a pediatric pulmonary clinic, and pediatric practices. Inclusion criteria included an asthma diagnosis for at least one year, prescription of asthma controller medication for at least six months, and absence of other chronic illnesses. Families self-reported race/ethnicity (53% White, 31% African-American, 3% Hispanic, 0.5% Asian American, and 12.5% other) and socioeconomic status (Hollingshead index 8.00–66.00; M=38.58, SD=16.34). Children varied with regard to objective asthma severity, with 22% classified as mild, 30% mild-persistent, 37% moderate-persistent, and 11% severe.
Procedure
Families were approached at clinic visits and informed about the study. Interested families were invited to a university-based lab, where caregiver consent and child assent were obtained and child and caregiver measures were completed. Caregiver permission was obtained to contact teachers, who completed questionnaires regarding child behavior.
Measures
Family cohesion
Children and caregivers completed a fifteen-minute activity in which they drew a “family crest” together. Interactions were videotaped and coded via the System for Coding Interactions and Family Functioning (SCIFF; Lindahl & Malik, 2001). The cohesiveness/cohesion scale used in this study assesses mutual appreciation and unity families display as they work toward a goal. Two coders viewed the interactions separately then rated cohesion, the extent to which families displayed affection, respect, and warmth toward one-another, on a scale from very low (1) to very high (5) (Lindahl & Malik, 2001). Consensus was reached for all ratings. Interrater rater reliability in our sample, obtained from 45 families (12 with fathers present), was adequate (α=.82).
Family functioning
The Family Assessment Device (FAD; Epstein, Baldwin, & Bishop, 1983) asks respondents to indicate on a 4-point scale how well each of 60 statements describes their family. Two of the six measured domains of family functioning were used in this study: problem solving and communication. Items were averaged to calculate subscale scores in which higher scores indicate poorer family functioning. The FAD has demonstrated adequate test-retest reliability (Cronbach’s alpha = .66 to .76) and internal consistency (α=.72–.92) (Miller et al., 1985). Internal consistency in this study was acceptable for the problem-solving (α=.67) and communication (α=.65) subscales.
Child depressive and anxiety symptoms
Primary caregivers completed the Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001). Respondents rated child behaviors on a three-point scale (0=absent, 1=occurs sometimes, 2=occurs often). For this study, the DSM-oriented scales of affective problems and anxiety problems were used; both scales have shown high levels of test-retest reliabilities (α=.82 and .72, respectively) and significant cross-informant agreement (Pearson’s r=.69 and .66, respectively) (Achenbach & Rescorla, 2001).
Teachers completed the Teacher Rating Form (TRF; Achenbach & Rescorla, 2001), an equivalent form to the CBCL with acceptable test-retest (.60–.96) and internal consistency scores (.72–.92). Significant TRF-CBCL cross-informant agreement has been supported for the affective and anxiety subscales (Achenbach & Rescorla, 2001).
Objective pulmonary functioning
Child lung function was measured by a respiratory therapist via a PDS313100-WSO KOKO Spirometer, yielding measurements of forced expiratory flow in one second (FEV1) and forced expiratory flow for 25–75% of vital capacity (FEV25–75; Raymond et al., 2012). After coaching on the procedure, children exhaled three times into the spirometer at rest and results with the highest sum of FEV1 and FVC were recorded. Children repeated testing ten minutes after Albuterol administration. A board-certified pediatric pulmonologist reviewed results and classified asthma severity according to NHLBI guidelines; higher scores indicate poorer lung function (1=slight/normal, 2=mild, 3=moderate, 4=severe).
Subjective asthma symptoms
Primary caregivers reported perceived severity of six symptoms (e.g., wheezing, activity limitations) over the past year via the Functional Severity Scale (FSS; Rosier et al., 1994). A total severity score was calculated by combining ratings across items (internal consistency in this sample, α=.71).
Asthma QOL
The Pediatric Asthma QOL Questionnaire (PAQLQ; Juniper et al., 1996) is a 23-item self-report measure on which children ages 7 and older reported their impairment on a seven-point scale. For children ages 5–7, we used the Pictorial Version of the PAQLQ; children responded using a picture of a thermometer ranging from empty to full on how much a symptom bothered them in the past week (Everhart & Fiese, 2009). For this study, we used symptom domain/subscale scores (PAQLQ α=.86 and Pictoral α=.83), which were standardized. Elevated scores indicated better QOL.
Asthma medication adherence
Consistent with prior research (Bender et al., 2000), each child’s adherence to prescribed asthma medication was tracked over a six-week period via an electronic recording device (MDIlog-II) or telephone diaries (for oral controller medication). Adherence was calculated as the number of doses taken each day divided by prescribed doses, averaged over a six-week period.
Statistical analyses
Statistical analyses were conducted using Mplus version 7.31 (Muthen, 2014). Initial data checking detected significant multivariate non-normality via Mardia’s normalized estimates (mij > 5, p <.001; Yuan, Bentler, & Zhang, 2006). Thus, Maximum Likelihood Robust estimation methods were used. Full Information Maximum Likelihood (FIML) accounted for missing data (Enders, 2001; Muthen, 2011).
To identify whether our hypothesized models fit the data appropriately (Muthen & Muthen, 2014), confirmatory factor analysis (CFA) was initially used to confirm the anxiety and depression models. Model fit was assessed using a combination of fit indices and strict cutoffs (see Figures 1 and 2; Hu & Bentler, 1999; Hooper et al., 2008; Jackson et al., 2009). Initial CFAs were followed by SEM analyses for each hypothesized mediation model. Covariates were included in models to control for their association with latent constructs. Finally, bootstrapping analyses with 5000 samples provided a 95% confidence interval for the effect of each mediation pathway; a confidence interval not containing zero indicated significant mediation (Cheung & Lau, 2007).
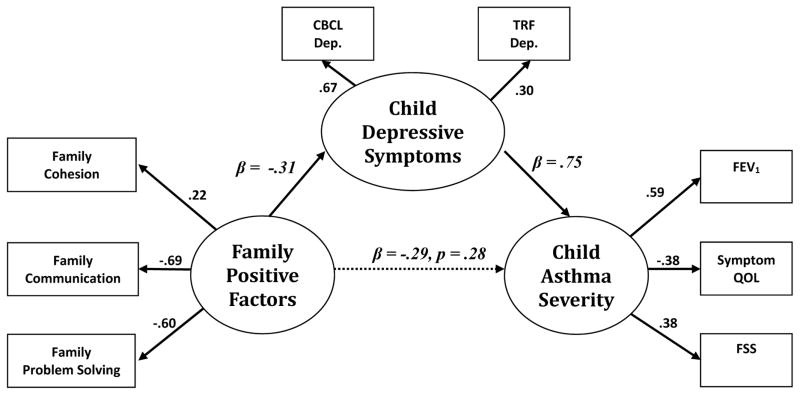
Figure 1.
Structural equation model of the significant indirect association between family positive factors and asthma severity via child depressive symptoms; χ2(23, n=215)=25.60, p=.31; RMSEA=.02 (.000–.062); CFI=0.97; TLI/NNFI=0.96; Values reported are all standardized; Ab=−.29; 95% CI (−5.038, −0.011).
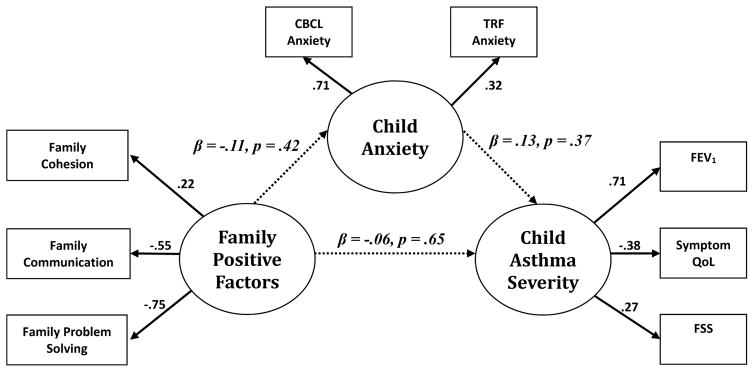
Figure 2.
Structural equation model of the non-significant indirect association between family positive factors and asthma severity via child anxiety symptoms; χ2(23, n=215) = 23.60, p=.32; RMSEA=.04 (.000–.075); CFI=0.96; TLI/NNFI=0.94; Values reported are all standardized; Ab=−.01; 95% CI (−0.289, 0.026).
Results
Preliminary analyses identified the absence of 17.7 % of teacher and 7% of primary caregiver ratings of child functioning; however, no patterns of missingness were detected. On average, families were rated as having moderate levels of cohesion, communication, and problem solving abilities, while mean child anxiety and depression scores fell in the non-clinical range for parent and teacher reports. Descriptive statistics for all variables are in Table 1 and bivariate correlations are presented in Table 2.
Table 1.
Descriptive Statistics for Family, Psychological, and Asthma Variables
| Variable | N | M (SD) | Range |
|---|---|---|---|
| Child age | 215 | 7.86 (2.18) | 5–12 |
| Medication adherence | 180 | 0.72 (0.31) | 0–1 |
| Family cohesion | 208 | 3.49 (1.10) | 1–5 |
| Family problem-solvinga | 208 | 1.91 (0.36) | 1–4 |
| Family communicationa | 208 | 1.99 (0.36) | 1–4 |
| Child anxiety (PC report)b | 200 | 55.15 (7.02) | 50–86 |
| Child anxiety (Teacher report)c | 177 | 54.30 (6.66) | 50–91 |
| Child depression (PC report)b | 200 | 55.02 (7.24) | 50–88 |
| Child depression (Teacher report)c | 177 | 55.37 (7.16) | 50–80 |
| Asthma severity/Lung dysfunction | 207 | 1.95 (.99) | 1–4 |
| Functional Severity Scale (PC report) | 215 | 8.57 (4.77) | 0–23 |
| Symptom-related QOL (Child report)d | 210 | 0.00 (1.00) | −2.63–1.84 |
Note.
Family Assessment Device scale scores: higher scores indicate poorer family functioning.
Primary caregiver ratings on Child Behavior Checklist (CBCL): higher scores indicate poorer functioning.
Teacher Rating Form(TRF): higher scores indicate poorer functioning.
Centered child-report on Pediatric Asthma Quality of Life Questionnaire (PAQLQ): higher scores indicate better symptom-related QOL.
Table 2.
Correlations among Family, Psychological, and Asthma Variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Cohesion | -- | ||||||||||||
| 2. Problem solvinga | −.16* | -- | |||||||||||
| 3. Communicationa | −.16* | .39** | -- | ||||||||||
| 4. Anxiety (PC)b | −.19** | .03 | .05 | -- | |||||||||
| 5. Anxiety (TRF)c | −.11 | −.01 | −.10 | .23** | -- | ||||||||
| 6. Depression (PC)b | −.16* | .16* | .09 | .66** | .05 | -- | |||||||
| 7. Depression (TRF)c | −.09 | .10 | .11 | .18* | .45** | .18* | -- | ||||||
| 8. Asthma severity | −.12 | .03 | .05 | .08 | .23** | .09 | .34** | -- | |||||
| 9. FSS | −.16* | −.07 | .02 | .15* | .003 | .19** | .18* | .16* | -- | ||||
| 10. Symptom QoLd | .03 | .09 | .04 | .04 | .03 | −.01 | −.20** | −.27** | −.12+ | -- | |||
| 11. Child age | .06 | −.04 | .03 | −.10 | −.03 | −.04 | −.08 | .02 | −.12 | .05 | -- | ||
| 12. Child sex | −.09 | .07 | .09 | .10 | −.09 | .19** | −.04 | −.03 | .06 | .09 | −.03 | -- | |
| 13. Med. adherence | .13 | −.04 | .03 | −.04 | −.06 | −.04 | −.20* | −.24 | −.17* | .17* | −.02 | .01 | -- |
Note.
Family Assessment Device scale scores: higher scores indicate worse family functioning.
Achenbach Child Behavior Checklist (CBCL): higher scores indicate poorer functioning.
Achenbach Teacher Rating Form(TRF): higher scores indicate poorer functioning.
Child-report on Pediatric Asthma Quality of Life Questionnaire (PAQLQ): higher scores indicate better symptom-related quality of life.
p < .10,
p < .05,
p < .01,
p < .001
Depression Pathway Model
CFA evaluated the hypothesized depression model’s fit to the observed sample values. Results indicated that this model appropriately fit the sample data (χ2 [17, n=215])=22.34, p=.17; CFI=.94; RMSEA=.04; TLI=.91). Additionally, all indicators significantly predicted their hypothesized latent constructs. No modification indices greater than 4 were suggested.
The depression pathway model was then tested with SEM. The model included child sex, age, and medication adherence as covariates, but only adherence was significantly associated with constructs and included in subsequent models. The model fit the data well, (χ2[23, n=215])=25.60, p=.31; CFI=.97; RMSEA=.02; TLI=.96). Positive family factors were inversely associated with child depression (β=−.31, p=.048) but were not directly associated with asthma severity (β=−.27, ns). Child depression was significantly associated with asthma severity (β=.75, p=.03) and the indirect path from family positive factors to asthma severity via child depression was also significant: point estimate of −.29, 95% CI=[−5.038, −0.011].
Anxiety Pathway Model
A confirmatory factor analysis, with family factors, child anxiety, and child asthma severity as latent constructs, indicated adequate model fit to the sample data (χ2 [17, n=215])= 22.50, p =.17; CFI=.93; RMSEA=.04; TLI=.88). All indicators significantly predicted their hypothesized latent constructs. However, structural equation modeling did not support the anxiety mediation pathway. No direct associations between child anxiety and family factors (β=−.11, ns) or between child asthma severity and family factors (β=−.06, ns) emerged. There were also no direct associations between child anxiety and asthma symptom severity (β=.13, ns). Bootstrapping analyses confirmed the absence of a mediation pathway, with a point estimate of −.01, 95% CI=[−0.289–0.026].
Discussion
The current study examined associations between positive family factors and child asthma outcomes via child depressive and anxiety symptoms, in order to identify potential skills for future family interventions. This study built upon previous findings by providing a MRMM approach, which provides a more comprehensive view of child and family functioning while minimizing single rater biases (Achenbach, 2006). These models also extend past research by jointly assessing family’s effects on subjective and objective measures of asthma severity (Cowen et al., 2007) and examining bio-behavioral pathways of effect while controlling for medication adherence.
Family Factors, Child Depression, and Asthma
Family functioning was inversely related to child depressive symptoms, confirming the important role families play in children’s psychological and physiological adjustment to chronic health conditions (Reichenberg & Anders, 2005). The way families openly communicate, unite in solving particular problems, and adapt in the face of threat to optimize family functioning are important in the way a child may adapt to his/her asthma. As they begin to gain more responsibilities, children rely on their families to help them adjust to developmental shifts and asthma management (Kaugars et al., 2004). Thus, it is crucial for families to communicate well and provide children with extra support during this period (Fulligni & Ecles, 1993; Wigfield et al., 1997). It is equally important for physicians to be cognizant of the family climate and provide families with psycho-education on the various contextual factors that can be associated with depressive symptoms and asthma management (e.g., family stress; Wood et al., 2015).
Children with more depressive symptoms also had poorer lung function. When children are depressed, they are more likely to respond to environmental stressors via parasympathetic nervous system (PNS) activation; consequently, with the domination of the PNS, they are more likely to have constricted airways and greater mucus secretion (Van der Velden & Hulsmann, 1999). It may be beneficial for children with comorbid asthma and depressive symptoms to receive a referral for evidence-based therapy to minimize depressive symptoms.
Although family functioning did not directly relate to child asthma symptoms, children from families with more positive functioning had fewer depressive symptoms; fewer depressive symptoms were in turn associated with better asthma status. Findings from this study support the notion that the family influences asthma severity via its effects on children’s bio-behavioral reactivity (Wood et al., 2006). Children may feel insecure if the family is not united or lacks effective communication methods (Winter et al., 2011). Similarly, children from families with higher levels of cohesion have been shown to have better asthma management behaviors (e.g., asthma knowledge; medication adherence; Rosales et al., 2016). As primary care settings transition into integrated care, physicians may provide families with opportunities to participate in family-based interventions (Yeh et al., 2016). Such interventions aim to empower families by providing them with the tools necessary to successfully manage pediatric asthma.
Family Factors, Child Anxiety, and Asthma
Though family functioning is generally associated with fewer anxiety symptoms (Bogels & Brechman-Toussaint, 2006), we did not find a significant association between positive family factors and anxiety symptoms. This finding contradicts previously found research suggesting cohesion and conflict contribute to children’s anxiety symptoms (Davies et al., 2004; Reichenberg & Anders, 2005). We used a broad construct of family protective factors, including problem-solving abilities, cohesion, and communication. Similar studies have found that although broad family constructs do not relate to child anxiety, specific attachment quality and autonomy granting are significant contributors to children’s sense of anxiety (Stuart Parrigon & Kerns, 2016). It may also be that children with asthma who experience poor family functioning develop specific types of anxiety, such as separation anxiety or panic attacks, that may not be captured in an overall measure of child anxiety (Fiese et al., 2010; Goodwin el al., 2004).
As hypothesized, we did not find a direct link between child anxiety and asthma severity. Results indicated that anxiety, being primarily associated with the SNS, may not be associated with asthma severity to the same extent as depression. These findings must be interpreted with caution, given the skewed nature of anxiety symptoms in our population. Similarly, only 11% of the children included in the study had asthma in the severe range, which may have limited our ability to detect bio-behavioral effects. However, our findings concur with past studies that have failed to identify a relationship between anxiety and objective measures of asthma severity (Steptoe & Vogele, 1992; Wamboldt et al., 1998). It may be that children with anxiety symptoms report increased subjective symptoms of asthma, but those associations are absent with objective measures of lung function. Anxiety symptoms, such as shortness of breath, may mimic asthma symptoms such that individuals misattribute their bodily responses to asthma (Peters & Fritz, 2011).
The mediational role of child anxiety in the association between family factors and child asthma symptoms was also examined. In agreement with the ANS dysregulation theory (Miller et al., 2009), anxiety did not play a significant role in linking family functioning to child asthma severity. It is important to note that the narrow range of symptoms reported in our sample may have limited the power of the anxiety pathway to a greater extent than the depression pathway, as anxiety is hypothesized to have a smaller effect on child asthma severity (Wood et al., 2006). Future studies should evaluate whether associations between family factors, asthma, and anxiety exist for children with diagnosed anxiety disorders; whereas slightly elevated symptoms may be manageable, more severe anxiety may directly influence children’s asthma management behaviors. Finally, studies should examine the effects of parental depression on these associations; because parents may influence child symptomology and family functioning, it is important to determine how these associations exist at different levels of parental psychopathology (Feldman et al., 2013).
Research thus far has focused on examining interrelationships among family factors, internalizing symptoms, and asthma severity; however, few studies have considered separate pathways for child anxiety and depressive symptoms in these associations (McQuaid et al., 2001). Our findings suggest that there are different roles for these internalizing symptoms in linking family factors to child pulmonary functioning. Results are consistent with past research focused on family conflict: Wood et al. (2006) found that while depressive symptoms mediated the relationship between family conflict and child asthma symptoms, anxiety symptoms did not (Wood et al., 2006). The MRMM approach strengthens our findings and study implications by providing a strength-based approach to examining functioning across multiple settings.
Findings should be interpreted with caution, given methodological limitations. First, this study cannot infer causality, given its cross-sectional design. For example, our findings could also be explained by a plausible alternative model in which child asthma severity influences family functioning via its effects on child depressive symptoms. Additionally, we may not have captured the true nature of children’s internalizing symptoms without obtaining their own subjective ratings (Cosi et al., 2010). Also, the study’s sample size did not provide adequate statistical power to control for anxiety symptoms in our depression mediation model; thus, we cannot infer whether depression predicts child asthma symptoms over and above the effects of anxiety symptoms. Findings require replication with a larger, more diverse sample to ensure greater variability in internalizing symptoms, family functioning, and asthma severity.
Recommendations and Future Directions
Study findings offer preliminary evidence for the relationship between positive family factors and child asthma severity via child depressive symptoms. Future studies should incorporate biological markers (e.g., acetylcholine) and longitudinal designs that can more adequately test directionality and bio-behavioral mechanisms of effect, and more thoroughly explore the multiple contexts of child development that can influence child internalizing (e.g., expanding to peer functioning). Studies should then turn to testing family-focused interventions, aimed at enhancing communication and increasing family unity, for children with poor asthma symptom control. Finally, as dynamic care models such as integrated primary care and the patient-centered medical home continue to grow, pediatricians can be encouraged to share knowledge regarding bio-behavioral associations with families to demonstrate how family functioning can affect children’s psychological well-being and ultimately, asthma severity.
Contributor Information
Nour Al Ghriwati, Department of Psychology, Virginia Commonwealth University
Marcia A. Winter, Department of Psychology, Virginia Commonwealth University
Robin S. Everhart, Department of Psychology, Virginia Commonwealth University
Barbara H. Fiese, Family Resiliency Center, University of Illinois at Urbana-Champaign
References
- Achenbach TM. As others see us clinical and research implications of cross-informant correlations for psychopathology. Current Directions in Psychological Science. 2006;15(2):94–98. [Google Scholar]
- Achenbach TM, Rescorla L. ASEBA school-age forms & profiles. Burlington, VT: Queen City Printers; 2001. [Google Scholar]
- Akinbami OJ. Trends in asthma prevalence, health care use, and mortality in the United States, 2001–2010. 2012 Retrieved from http://www.cdc.gov/nchs/data/databriefs/db94.htm. [PubMed]
- Bender B, Wamboldt F, O'Connor SL, Rand C, Szefler S, Milgrom H, Wamboldt MZ. Measurement of children's asthma medication adherence by self report, mother report, canister weight, and Doser CT. Annals of Allergy, Asthma & Immunology. 2000;85(5):416–421. doi: 10.1016/s1081-1206(10)62557-4. [DOI] [PubMed] [Google Scholar]
- Bögels SM, Brechman-Toussaint ML. Family issues in child anxiety: Attachment, family functioning, parental rearing and beliefs. Clinical Psychology Review. 2006;26(7):834–856. doi: 10.1016/j.cpr.2005.08.001. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Most recent asthma data. 2016 Retrieved from http://www.cdc.gov/asthma/most_recent_data.htm.
- Cheung GW, Lau RS. Testing mediation and suppression effects of latent variables: Bootstrapping with structural equation models. Organizational Research Methods. 2007;11(2):296–325. [Google Scholar]
- Cosi S, Canals J, Hernández-Martinez C, Vigil-Colet A. Parent–child agreement in SCARED and its relationship to anxiety symptoms. Journal of Anxiety Disorders. 2010;24(1):129–133. doi: 10.1016/j.janxdis.2009.09.008. [DOI] [PubMed] [Google Scholar]
- Cowen MK, Wakefield DB, Cloutier MM. Classifying asthma severity: objective versus subjective measures. Journal of Asthma. 2007;44(9):711–715. doi: 10.1080/02770900701595576. [DOI] [PubMed] [Google Scholar]
- Davies PT, Cummings EM, Winter MA. Pathways between profiles of family functioning, child security in the interparental subsystem, and child psychological problems. Development and psychopathology. 2004;16(03):525–550. doi: 10.1017/s0954579404004651. [DOI] [PubMed] [Google Scholar]
- Drotar D, Bonner MS. Influences on adherence to pediatric asthma treatment: a review of correlates and predictors. Journal of Developmental & Behavioral Pediatrics. 2009;30(6):574–582. doi: 10.1097/DBP.0b013e3181c3c3bb. [DOI] [PubMed] [Google Scholar]
- Enders CK. The impact of nonnormality on full information maximum-likelihood estimation for structural equation modelswith missing data. Psychological Methods. 2001;6:352–370. [PubMed] [Google Scholar]
- Epstein NB, Baldwin LM, Bishop DS. The McMaster family assessment device. Journal of Marital and Family Therapy. 1983;9(2):171–180. [Google Scholar]
- Everhart RS, Fiese BH. Development and initial validation of a pictorial quality of life measure for young children with asthma. Journal of Pediatric Psychology. 2009;34(9):966–976. doi: 10.1093/jpepsy/jsn145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman JM, Steinberg D, Kutner H, Eisenberg N, Hottinger K, Sidora-Arcoleo K, Serebrisky D. Perception of pulmonary function and asthma control: the differential role of child versus caregiver anxiety and depression. Journal of Pediatric Psychology. 2013;38(10):1091–1100. doi: 10.1093/jpepsy/jst052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiese BH, Winter MA, Wamboldt FS, Anbar RD, Wamboldt MZ. Do family mealtime interactions mediate the association between asthma symptoms and separation anxiety? Journal of Child Psychology and Psychiatry. 2010;51(2):144–151. doi: 10.1111/j.1469-7610.2009.02138.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiese BH, Winter MA, Botti JC. The ABCs of family mealtimes: Observational lessons for promoting healthy outcomes for children with persistent asthma. Child Development. 2011;82(1):133–145. doi: 10.1111/j.1467-8624.2010.01545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuligni AJ, Eccles JS. Perceived parent-child relationships and early adolescents' orientation toward peers. Developmental psychology. 1993;29(4):622. [Google Scholar]
- Global Asthma Network. The global asthma report 2014. Auckland, New Zealand: Global Asthma Network; 2014. [Google Scholar]
- Goodwin RD, Bandiera FC, Steinberg D, Ortega AN, Feldman JM. Asthma and mental health among youth: etiology, current knowledge and future directions. Expert review of respiratory medicine. 2014 doi: 10.1586/ers.12.34. [DOI] [PubMed] [Google Scholar]
- Goodwin R, Fergusson D, Horwood L. Asthma and depressive and anxiety disorders among young persons in the community. Psychological Medicine. 2004;34(8):1465–1474. doi: 10.1017/s0033291704002739. [DOI] [PubMed] [Google Scholar]
- Herzer M, Denson LA, Baldassano RN, Hommel KA. Family functioning and health-related quality of life in adolescents with pediatric inflammatory bowel disease. European Journal of Gastroenterology and Hepatology. 2011;23:95–100. doi: 10.1097/MEG.0b013e3283417abb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper D, Coughlan J, Mullen M. Structural equation modelling: Guidelines for determining model fit. Articles. 2008:2. [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling: a multidisciplinary journal. 1999;6(1):1–55. [Google Scholar]
- Jackson DL, Gillaspy JA, Jr, Purc-Stephenson R. Reporting practices in confirmatory factor analysis: an overview and some recommendations. Psychological methods. 2009;14(1):6. doi: 10.1037/a0014694. [DOI] [PubMed] [Google Scholar]
- Juniper EF. How important is quality of life in pediatric asthma? Pediatric Pulmonology. 1997;24(S15):17–21. [PubMed] [Google Scholar]
- Juniper EF, Guyatt G, Feeny D, Griffith L, Ferrie P, Townsend M. Measuring quality of life in children with asthma. Quality of Life Research. 1996;5:35–46. doi: 10.1007/BF00435967. [DOI] [PubMed] [Google Scholar]
- Kaugars A, Klinnert M, Bender B. Family influences on pediatric asthma. Journal of Pediatric Psychology. 2004;29(7):475–491. doi: 10.1093/jpepsy/jsh051. [DOI] [PubMed] [Google Scholar]
- Kewalramani A, Bollinger ME, Postolache TT. Asthma and mood disorders. International journal of child health and human development: IJCHD. 2008;1(2):115. [PMC free article] [PubMed] [Google Scholar]
- Lindahl KM, Malik NM. The system for coding interactions and family functioning. In: Kerig P, Lindahl K, editors. Handbook of family observation coding systems. New Jersey, NJ: Erlbaum: Hillsdale; 2001. pp. 77–91. [Google Scholar]
- Marin TJ, Chen E, Munch JA, Miller GE. Double-exposure to acute stress and chronic family stress is associated with immune changes in children with asthma. Psychosomatic medicine. 2009;71(4):378. doi: 10.1097/PSY.0b013e318199dbc3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCauley E, Katon W, Russo J, Richardson L, Lozano P. Impact of anxiety and depression on functional impairment in adolescents with asthma. General hospital psychiatry. 2007;29(3):214–222. doi: 10.1016/j.genhosppsych.2007.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQuaid EL, Kopel SJ, Nassau JH. Behavioral adjustment in children with asthma: a meta-analysis. Journal of Developmental & Behavioral Pediatrics. 2001;22(6):430–439. doi: 10.1097/00004703-200112000-00011. [DOI] [PubMed] [Google Scholar]
- Miller IW, Epstein NB, Bishop DS, Keitner GI. The McMaster Family Assessment Device: Reliability and validity. Journal of Marital & Family Therapy. 1985;11(4):345–356. [Google Scholar]
- Miller BD, Wood BL. Influence of specific emotional states on Autonomic Reactivity and pulmonary function in asthmatic children. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(5):669–677. doi: 10.1097/00004583-199705000-00018. [DOI] [PubMed] [Google Scholar]
- Miller BD, Wood BL, Lim J, Ballow M, Hsu C. Depressed children with asthma evidence increased airway resistance:“Vagal bias” as a mechanism? Journal of Allergy and Clinical Immunology. 2009;124(1):66–73. doi: 10.1016/j.jaci.2009.04.038. [DOI] [PubMed] [Google Scholar]
- Muthén B. Applications of causally defined direct and indirect effects in mediation analysis using SEM in Mplus. 2011 http://statmodel2.com/download/causalmediation.pdf.
- National Heart Lung and Blood Institute. Expert Panel Report 3 (EPR 3): guidelines for the diagnosis and management of asthma. Bethesda: National Institutes of Health; 2007. [Google Scholar]
- Olson DH, Sprenkle DH, Russell CS. Circumplex model of marital and family systems: I. Cohesion and adaptability dimensions, family types, and clinical applications. Family process. 1979;18(1):3–28. doi: 10.1111/j.1545-5300.1979.00003.x. [DOI] [PubMed] [Google Scholar]
- Peters TE, Fritz GK. Psychological considerations of the child with asthma. The Pediatric Clinics of North America. 2011;58(4):921–935. doi: 10.1016/j.pcl.2011.06.006. [DOI] [PubMed] [Google Scholar]
- Raymond KP, Fiese BH, Winter MA, Knestel A, Everhart RS. Helpful hints: caregiver-generated asthma management strategies and their relation to pediatric asthma symptoms and quality of life. Journal of pediatric psychology. 2012;37(4):414–423. doi: 10.1093/jpepsy/jss001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichenberg K, Anders GB. Children with asthma: Few adjustment problems are related to high perceived parental capacity and family cohesion. Nordic Journal of Psychiatry. 2005;59(1):13–18. doi: 10.1080/08039480510018878. [DOI] [PubMed] [Google Scholar]
- Rosales A, Mcquaid E, Koinis-Mitchell D. Family Connectedness and Pediatric Asthma Management: The Roles of Child Age and Race or Ethnicity. Children's Health Care. 2016 doi: 10.1080/02739615.2016.1227934. [DOI] [Google Scholar]
- Rosier MJ, Bishop J, Nolan T, Robertson CF, Carlin JB, Phelan PD. Measurement of functional severity of asthma in children. American Journal of Respiratory and Critical Care Medicine. 1994;149(6):1434–1441. doi: 10.1164/ajrccm.149.6.8004295. [DOI] [PubMed] [Google Scholar]
- Smith SR. Making sense of multiple informants in child and adolescent psychopathology: A guide for clinicians. Journal of Psychoeducational Assessment. 2007;25(2):139–149. [Google Scholar]
- Spagnola M, Fiese B. Preschoolers with asthma: narratives of family functioning predict behavior problems. Family process. 2010;49(1):74–91. doi: 10.1111/j.1545-5300.2010.01309.x. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Vögele C. Individual differences in the perception of bodily sensations: the role of trait anxiety and coping style. Behaviour Research and Therapy. 1992;30(6):597–607. doi: 10.1016/0005-7967(92)90005-2. [DOI] [PubMed] [Google Scholar]
- Stuart Parrigon K, Kerns L. Family Processes in Child Anxiety: The Long-Term Impact of Fathers and Mothers. Journal of Abnormal Child Psychology. 2016;44(7):1253–1266. doi: 10.1007/s10802-015-0118-4. [DOI] [PubMed] [Google Scholar]
- Van der Velden VH, Hulsmann AR. Autonomic innervation of human airways: structure, function, and pathophysiology in asthma. Neuroimmunomodulation. 1999;6(3):145–159. doi: 10.1159/000026376. [DOI] [PubMed] [Google Scholar]
- Wamboldt MZ, Fritz G, Mansell A, Mcquaid EL, Klein RB. Relationship of asthma severity and psychological problems in children. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37(9):943–950. doi: 10.1097/00004583-199809000-00014. [DOI] [PubMed] [Google Scholar]
- Wigfield A, Eccles JS, Yoon KS, Harold RD, Arbreton AJ, Freedman-Doan C, Blumenfeld PC. Change in children's competence beliefs and subjective task values across the elementary school years: A 3-year study. Journal of Educational Psychology. 1997;89(3):451. [Google Scholar]
- Winter MA, Fiese BH, Spagnola M, Anbar RD. Asthma severity, child security, and child internalizing: Using story stem techniques to assess the meaning children give to family and disease-specific events. Journal of Family Psychology. 2011;25(6):857. doi: 10.1037/a0026191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood B. One articulation of the structural family therapy model: A biobehavioral family model of chronic illness in children. Journal of Family Therapy. 1994;16(1):53–72. [Google Scholar]
- Wood B, Lim J, Miller B, Cheah P, Simmens S, Stern T, … Ballow M. Family emotional climate, depression, emotional triggering of asthma, and disease severity in pediatric asthma: Examination of pathways of effect. Journal of Pediatric Psychology. 2007;32(5):542–551. doi: 10.1093/jpepsy/jsl044. [DOI] [PubMed] [Google Scholar]
- Wood B, Lim J, Miller B, Cheah P, Zwetsch T, Ramesh S, Simmens S. Testing the Biobehavioral Family Model in pediatric asthma: Pathways of effect. Family Process. 2008;47(1):21–40. doi: 10.1111/j.1545-5300.2008.00237.x. [DOI] [PubMed] [Google Scholar]
- Wood B, Miller B, Lehman H. Review of Family Relational Stress and Pediatric Asthma: The Value of Biopsychosocial Systemic Models. Family Process. 2015;54(2):376–389. doi: 10.1111/famp.12139. [DOI] [PubMed] [Google Scholar]
- Wood B, Miller B, Lim J, Lillis K, Ballow M, Stern T, Simmens S. Family relational factors in pediatric depression and asthma: Pathways of effect. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(12):1494–1502. doi: 10.1097/01.chi.0000237711.81378.46. [DOI] [PubMed] [Google Scholar]
- Yeh HY, Ma WF, Huang JL, Hsueh KC, Chiang LC. Evaluating the effectiveness of a family empowerment program on family function and pulmonary function of children with asthma: A randomized control trial. International Journal of Nursing Studies. 2016;60:133–144. doi: 10.1016/j.ijnurstu.2016.04.013. [DOI] [PubMed] [Google Scholar]
- Yuan KH, Bentler PM, Zhang W. The Effect of Skewness and Kurtosis on Mean and Covariance Structure Analysis The Univariate Case and Its Multivariate Implication. Sociological Methods & Research. 2005;34(2):240–258. [Google Scholar]