Abstract
In liver hepatocytes, the HFE gene regulates cellular and systemic iron homeostasis by modulating cellular iron-uptake and producing the iron-hormone hepcidin in response to systemic iron elevation. However, the mechanism of iron-sensing in hepatocytes remain enigmatic. Therefore, to study the effect of iron on HFE and hepcidin (HAMP) expressions under distinct extracellular and intracellular iron-loading, we examined the effect of holotransferrin treatment (1, 2, 5 and 8 g/L for 6 h) on intracellular iron levels, and mRNA expressions of HFE and HAMP in wild-type HepG2 and previously characterized iron-loaded recombinant-TfR1 HepG2 cells. Gene expression was analyzed by real-time PCR and intracellular iron was measured by ferrozine assay. Data showed that in the wild-type cells, where intracellular iron content remained unchanged, HFE expression remained unaltered at low holotransferrin treatments but was upregulated upon 5 g/L (p < 0.04) and 8 g/L (p = 0.05) treatments. HAMP expression showed alternating elevations and increased upon 1 g/L (p < 0.05) and 5 g/L (p < 0.05). However, in the recombinant cells that showed higher intracellular iron levels than wild-type cells, HFE and HAMP expressions were elevated only at low 1 g/L treatment (p < 0.03) and were repressed at 2 g/L treatment (p < 0.03). Under holotransferrin-untreated conditions, the iron-loaded recombinant cells showed higher expressions of HFE (p < 0.03) and HAMP (p = 0.05) than wild-type cells. HFE mRNA was independently elevated by extracellular and intracellular iron-excess. Thus, it may be involved in sensing both, extracellular and intracellular iron. Repression of HAMP expression under simultaneous intracellular and extracellular iron-loading resembles non-hereditary iron-excess pathologies.
Electronic supplementary material
The online version of this article (doi:10.1007/s11033-017-4123-2) contains supplementary material, which is available to authorized users.
Keywords: HFE, Iron-sensing, Holotransferrin, Hepcidin
Introduction
Maintenance of cellular and systemic iron homeostasis in the body is a dynamic process involving several signal transduction pathways. The haemochromatosis protein HFE maintains body iron homeostasis by participating in the induction of hepcidin (HAMP), the systemic iron regulator, by a yet incompletely understood mechanism [1–3]. Mutations in the genes HFE or HAMP causes diminished hepcidin production which results in systemic and tissue iron overload, referred as hereditary haemochromatosis [4]. However, despite the presence of functional wild-type alleles of these genes, low to moderate tissue iron excess is also observed in non-hereditary conditions such as alcoholic liver disease, hepatitis C infections, non-alcoholic fatty liver disease, non-alcoholic steato hepatitis and type 2 diabetes [5–8]. In these cases, iron loading can exacerbate the pathophysiology via excess-iron-induced oxidative stress [9]. Thus, it is important to fully delineate their iron-sensing mechanisms to formulate therapeutic interventions, particularly for the low-moderate iron-loaded conditions where, unlike hereditary hemochromatosis, phlebotomy is not practiced for removal of excess iron.
The mRNA response of HFE to increasing extracellular and intracellular iron and its relationship with HAMP expression at transcript level have not been studied so far. Hence, in this short study, we investigated the effect of a range of holotransferrin (holo-Tf) concentrations (1–8 g/L) on HFE and HAMP mRNA expressions, and intracellular iron content. First, we observed these responses in the wild type (Wt) HepG2 cells, where holo-Tf supplementation represent physiological conditions with extracellular (systemic) iron elevation prior to intracellular/tissue iron loading. Then, we examined the responses in the previously characterized recombinant (rec)-TfR1 HepG2 cells [10]. As these cells can achieve intracellular iron overloading [10], holo-Tf supplementation to these cells represent pathological conditions, which show simultaneously increased extracellular (systemic) and intracellular iron levels. Finally, to understand the exclusive effect of high intracellular iron content, we compared the expression levels between holo-Tf-untreated Wt and recombinant cells. Unlike most previous holo-Tf supplementation studies that were conducted at longer time-points of 24, 48 or 72 h [11–13], here, we studied the effect following 6 h of holotransferrin treatment to examine early responses.
Materials and methods
Cell culture and treatments
Maintenance of cells and holo-Tf supplementation to the Wt HepG2 cells (Health Protection Agency, UK) and rec-TfR1 HepG2 cells was as described previously [10]. Cells were treated with holo-Tf (1, 2, 5 and 8 g/L) prepared in serum-free EMEM (0 g/L) for 6 h and assessed for various parameters. As 8 g/L holo-Tf represent a very high concentration and the rec-TfR1 HepG2 cells had the potential for intracellular iron-overloading following holo-Tf supplementation [10], the effect of this concentration was studied only in Wt cells.
Determination of intracellular iron content
Cellular iron content determined by ferrozine assay [14] was normalized to protein, content, as quantified by Bradford method. Iron levels were expressed as nmoles iron/mg protein.
Gene expression analysis
Primers (Invitrogen, UK) for expression analyses, RNA extraction, cDNA conversion and assessment for mRNA expression via real-time PCR by using Quantifast SYBR green kit (Qiagen, UK), was as previously described [10, 15]. Data was analyzed by the relative quantification method, Delta–Delta Ct (∆∆Ct) and expressed as 2−∆∆Ct [16].
Statistical analysis
Data analysis was performed using one-way ANOVA. The level of significance was set at p < 0.05. Data was presented as mean ± SEM (n = 3).
Results
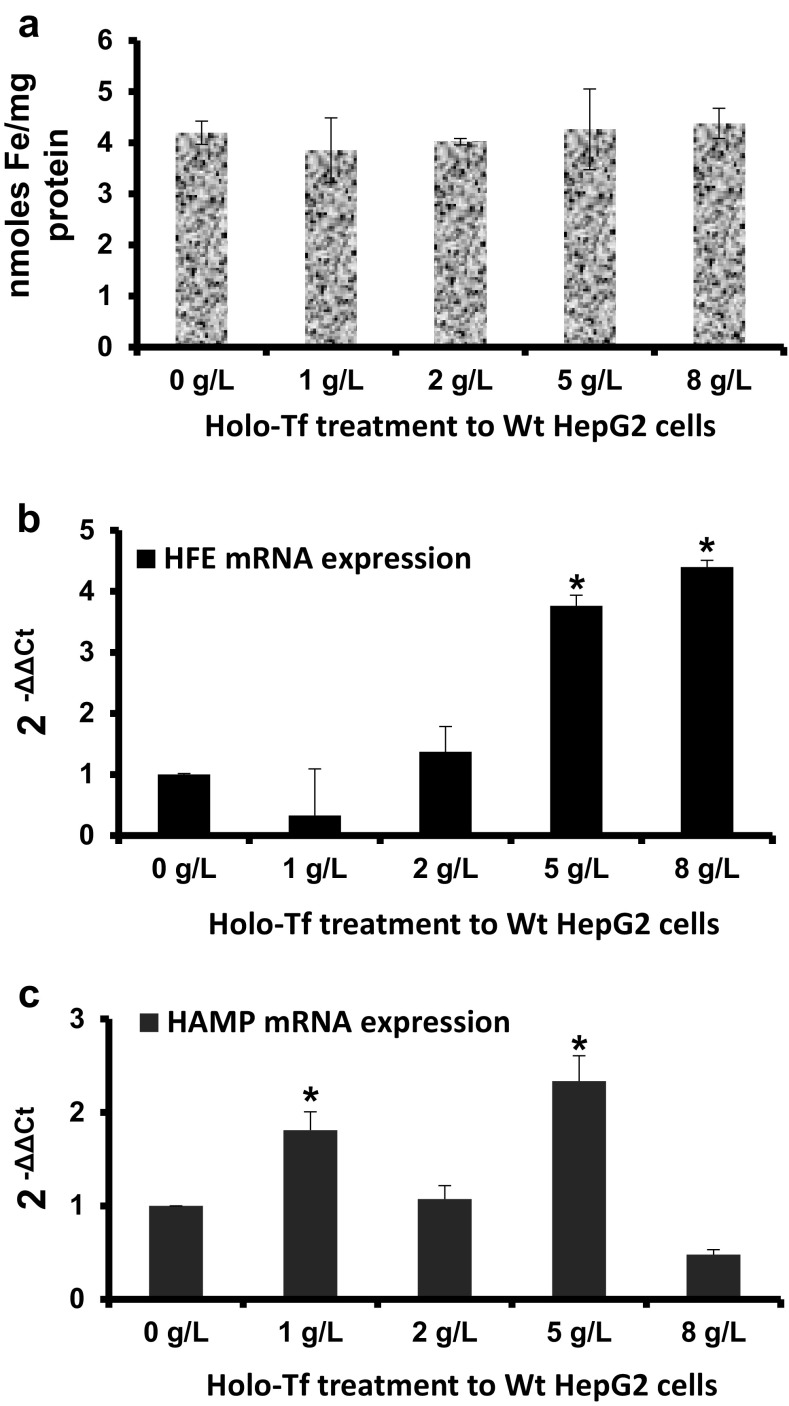
In the Wt cells, while intracellular iron content remained unaltered following holo-Tf supplementation (Fig. 1a), HFE mRNA expression significantly increased by 3.5-fold (p < 0.04) upon 5 g/L treatment and further increased by 4.5-fold (p = 0.05) upon 8 g/L treatment (Fig. 1b). Expression levels remained unaltered at lower concentrations of 1 and 2 g/L (Fig. 1b). Differentially, HAMP expression showed a pattern of alternating responses i.e. a significant 1.8-fold (p < 0.05) up-regulation upon 1 g/L treatment, unaltered expression upon 2 g/L treatment followed by a significant 2.3-fold up-regulation upon 5 g/L treatment (p < 0.05) and then, down-regulation upon 8 g/L treatment (Fig. 1c).
Fig. 1.
Effects of holo-Tf supplementation in Wt HepG2 cells. Wt HepG2 cells were treated with holo-Tf for 6 h. Following the treatment, intracellular iron levels were measured and expressed per mg protein (a). HFE (b) and HAMP (c) mRNA expressions was assessed and expressed relative to untreated (0 g/L) cells. Data is presented as mean ± SEM (n = 3). *p ≤ 0.05 compared to untreated (0 g/L) controls
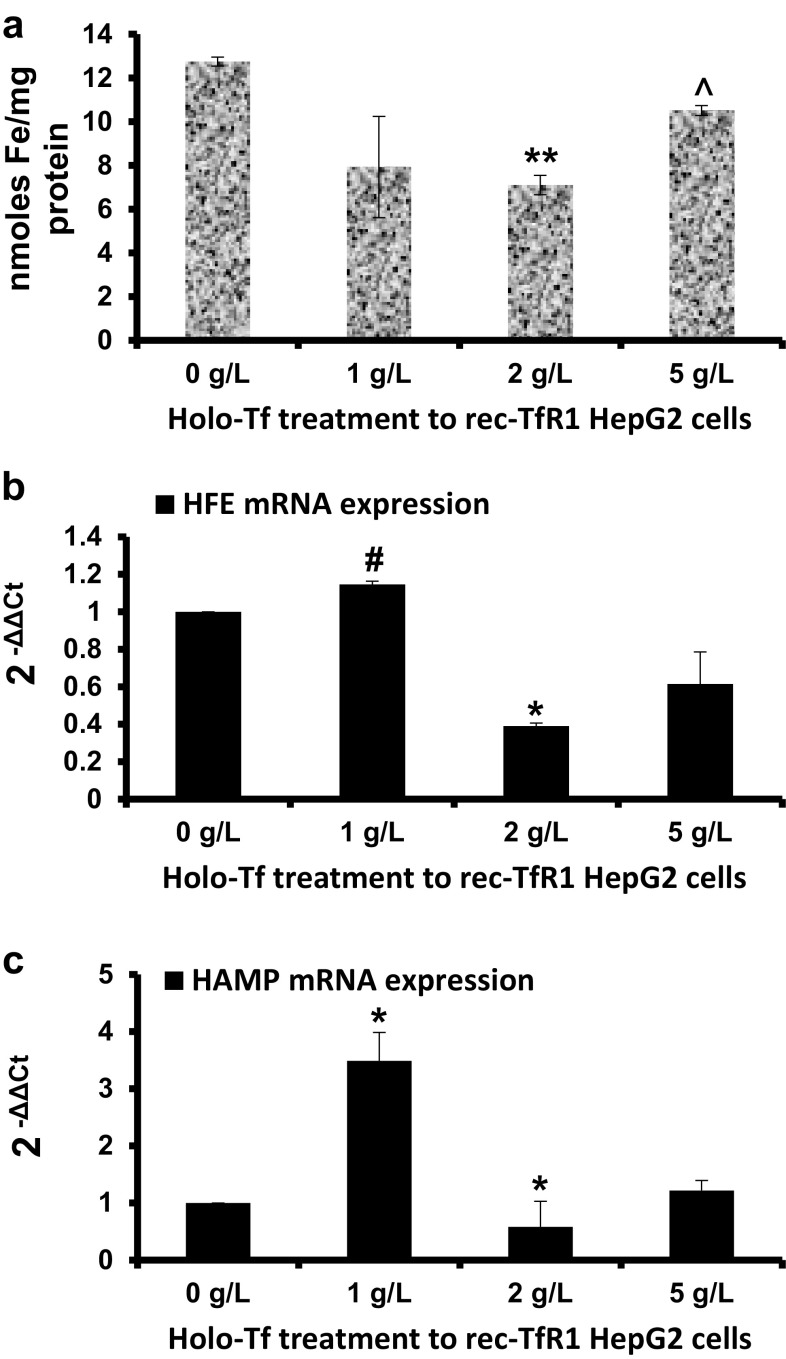
Prior to expression studies in the recombinant cells, intracellular iron loading was confirmed. Data showed that following treatment with most holo-Tf concentrations, intracellular iron content in these cells was higher than Wt cells (Figs. 1a, 2a). In the recombinant cells, over the increasing holo-Tf concentrations, although intracellular iron content decreased at 2 g/L (p < 0.01), it increased at 5 g/L treatment (p < 0.03) that restored the high levels, as in untreated conditions (Fig. 2a). These cells differed from the Wt cells in HFE and HAMP expression patterns. Here, HFE expression increased upon 1 g/L (p = 0.07), but then decreased upon 2 g/L holo-Tf treatment (p < 0.03), and remained unaltered at 5 g/L (Fig. 2b). Similarly, HAMP expression increased by 3.5-fold at 1 g/L (p < 0.03) followed by a repression at 2 g/L (p < 0.03)and remained unaltered at 5 g/L treatment (Fig. 2c).
Fig. 2.
Effects of holo-Tf supplementation in rec-TfR1 HepG2 cells. Rec-TfR1 HepG2 cells were treated with holo-Tf for 6 h. Following the treatment, intracellular iron levels were measured and expressed per mg protein (a). HFE (b) and HAMP (c) mRNA expressions was assessed and expressed relative to untreated (0 g/L) cells. Data is presented as mean ± SEM (n = 3). *p < 0.03, **p < 0.01 and #p = 0.07 compared to untreated (0 g/L) controls. ^p < 0.03 compared to 2 g/L treatment
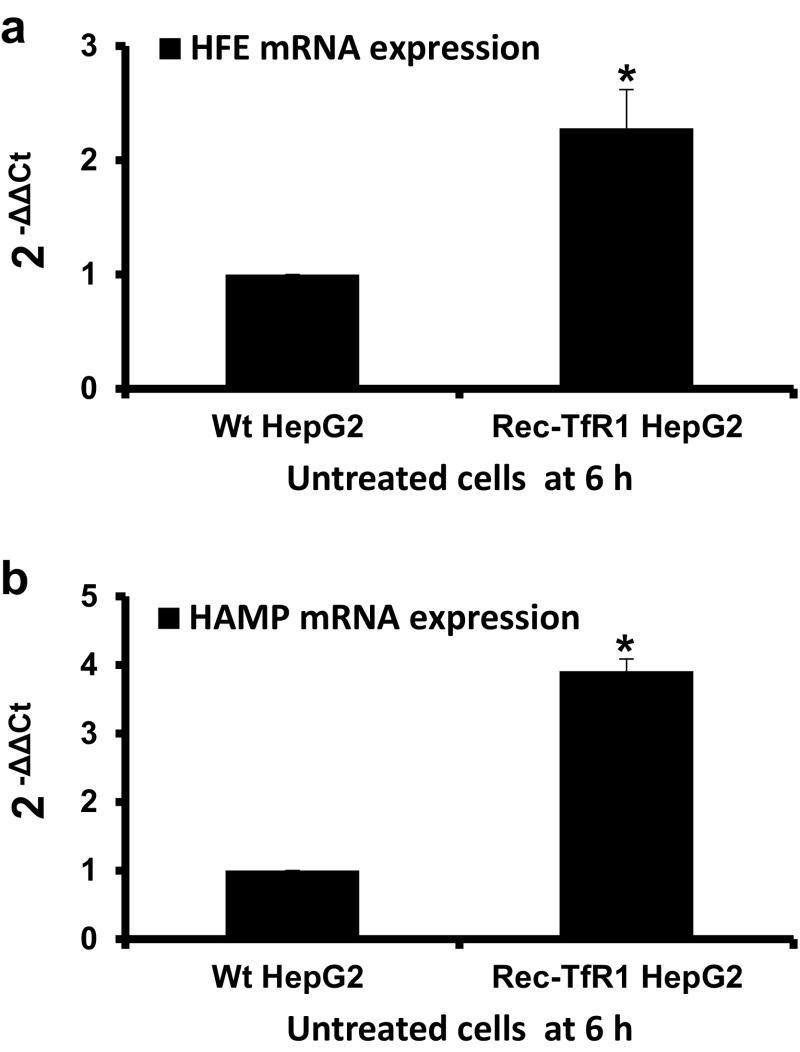
Further, to understand the exclusive effect of intracellular iron loading, HFE and HAMP expressions in untreated cells were compared. Data showed that the recombinant cells expressed higher levels of HFE and HAMP mRNA than Wt cells (2.3-fold; p < 0.03 and 3.9-fold; p = 0.05, respectively) (Fig. 3a, b).
Fig. 3.
HFE and HAMP mRNA expressions in rec-TfR1 HepG2 cells relative to Wt HepG2 cells. The mRNA expressions of HFE (a) and HAMP (b) in the recombinant cells were expressed relative to Wt HepG2 cells under untreated conditions at the 6 h time point. Data is presented as mean ± SEM (n = 3). *p ≤ 0.05 compared to Wt HepG2 cells
Discussion
The genes HFE and HAMP are extremely important for maintaining body iron homeostasis, where the protein HFE modulates HAMP induction [1, 2] and the induced peptide hepcidin regulates systemic iron homeostasis upon systemic iron elevation [17, 18]. However, the intracellular and extracellular iron-sensing mechanisms remain unclear and the upstream responses of the HFE mRNA to increasing extracellular and intracellular iron levels and its co-relation with HAMP mRNA have been rarely studied. Therefore, in this short study we aimed to discriminate between the effects of intracellular and extracellular iron-loading. Hence, we examined HFE and HAMP expressions under high extracellular iron levels, high intracellular iron levels, and simultaneously increased intracellular and extracellular iron levels by treating Wt and recombinant HepG2 cells with/without a range of increasing holo-Tf concentrations. Such studies will not only help in elucidating the iron-sensing mechanisms but also in understanding iron-acquisition in non-hereditary iron-excess conditions.
HFE mRNA expression is responsive to excess extracellular and intracellular iron
In our knowledge, no study has yet reported the effect of increasing holo-Tf concentration or saturation on HFE mRNA levels. We report for the first time, that increasing extracellular holo-Tf concentration causes elevation in HFE mRNA expression in the Wt HepG2 cells (Fig. 1b). As this increase occurred in the absence of intracellular iron elevation (Fig. 1a), it could be attributed exclusively to the elevated extracellular holo-Tf concentrations, thereby demonstrating the responsiveness of HFE mRNA towards excess extracellular iron. Furthermore, high HFE mRNA expression in the absence of extracellular iron, but presence of high intracellular iron (as observed in untreated recombinant cells) can be attributed exclusively to the high intracellular iron content (Figs. 1a, 2a, 3a). This indicates the responsiveness of HFE mRNA exclusively to high intracellular content. Collectively, HFE mRNA expression showed independent sensitivity to extracellular and intracellular iron loading.
HAMP mRNA expression and iron
In the Wt cells, elevation of HAMP expression following holo-Tf supplementation (Fig. 1c) is an expected response following an iron stimulus [17, 19, 20]. These elevations occurred in the absence of increased intracellular iron, indicating that an increase in extracellular iron was sufficient for the induction and a major increase in intracellular iron content was not necessary. Interestingly, its wavy pattern of expression over the increasing holo-Tf concentrations displayed a typical hormonal characteristic where increased levels of a stimulant (here, holo-Tf) may not lead to a directly proportional mRNA response. This is because, unlike cytokines, hormone-peptides are ‘premade’ and released from vesicles following a stimulus, like incase of insulin [21]. In the absence of extracellular iron (untreated cells), the high HAMP expression in recombinant cells (Fig. 3b), indicated that HAMP could be induced exclusively due to high intracellular iron content (Figs. 1a, 2a).
Interrelationship between HFE and HAMP expression patterns
A correlation between the mRNA responses of HFE and HAMP over the increasing holo-Tf concentrations was envisaged. The Wt cells showed no co-relation between the patterns of their responses (Fig. 1b, c), probably reflecting the hormonal characteristic of hepcidin. Conversely, the recombinant cells showed similarities between the patterns of HFE and HAMP expressions (Fig. 2b, c). Data in the recombinant showed that under intracellular iron excess, only subtle extracellular iron elevation could elevate HFE and HAMP expressions and further increase in extracellular iron led to either repression or an unaltered effect. This implies that both these genes can be induced by an external iron stimulus to regulate iron homeostasis, but preferably in the absence of intracellular iron loading. This could be a reason for deregulated iron metabolism and insufficient hepcidin production in non-hereditary iron excess conditions that show both, systemic and cellular iron loading, despite the presence of functional alleles of these genes.
Further studies are required to elucidate these mechanisms to better understand the iron-sensing and iron-loading mechanisms; aiming to design therapeutic interventions for the non-hereditary iron-excess pathologies.
Conclusion
In this short study, the independent effects of extracellular and intracellular iron on HFE and HAMP expressions were examined. HFE mRNA demonstrated independent responsiveness to elevated extracellular and intracellular iron content, suggesting its involvement in sensing both, extracellular and intracellular iron. Under combined intracellular and extracellular iron loading, HFE and HAMP expressions showed similar patterns and HAMP was induced only by low holo-Tf concentration, a scenario resembling iron excess pathologies.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Funding
Dr. Kosha Mehta was supported by a scholarship from the University of Westminster.
Abbreviations
- EMEM
Eagle’s minimal essential medium
- Holo-Tf
Holotransferrin
- H
Hours
Gene annotations
- HAMP
Gene encoding hepcidin
- HFE
Gene encoding haemochromatosis protein HFE
Author contributions
KM: key researcher; carried out experimental work, performed statistical analyses and wrote the article. SF: concept of the research. VBP: director of studies and final approver for the version of the article to be published.
Compliance with ethical standards
Ethical approval
This article does not contain any studies conducted on human or animal subjects.
Footnotes
The original version of this article has been changed to reflect the correct co-author name: Sebastien Farnaud.
Electronic supplementary material
The online version of this article (doi:10.1007/s11033-017-4123-2) contains supplementary material, which is available to authorized users.
An erratum to this article is available at https://doi.org/10.1007/s11033-017-4127-y.
References
- 1.D’Alessio F, Hentze MW, Muckenthaler MU. The hemochromatosis proteins HFE, TfR2, and HJV form a membrane-associated protein complex for hepcidin regulation. J Hepatol. 2012;57(5):1052–1060. doi: 10.1016/j.jhep.2012.06.015. [DOI] [PubMed] [Google Scholar]
- 2.Rishi G, Crampton EM, Wallace DF, Subramaniam VN. In situ proximity ligation assays indicate that hemochromatosis proteins Hfe and transferrin receptor 2 (Tfr2) do not interact. PLoS ONE. 2013;8(10):e77267. doi: 10.1371/journal.pone.0077267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gao J, Chen J, Kramer M, Tsukamoto H, Zhang A-S, Enns CA. Interaction of the hereditary hemochromatosis protein HFE with transferrin receptor 2 is required for transferrin-induced hepcidin expression. Cell Metab. 2009;9(3):217–227. doi: 10.1016/j.cmet.2009.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Feder JN, Gnirke A, Thomas W, Tsuchihashi Z, Ruddy DA, Basava A, et al. A novel MHC class I-like gene is mutated in patients with hereditary haemochromatosis. Nat Genet. 1996;13(4):399–408. doi: 10.1038/ng0896-399. [DOI] [PubMed] [Google Scholar]
- 5.Costa-Matos L, Batista P, Monteiro N, Simões M, Egas C, Pereira J, et al. Liver hepcidin mRNA expression is inappropriately low in alcoholic patients compared with healthy controls. Eur J Gastroenterol Hepatol. 2012;24(10):1158–1165. doi: 10.1097/MEG.0b013e328355cfd0. [DOI] [PubMed] [Google Scholar]
- 6.Fujita N, Takei Y. Iron overload in nonalcoholic steatohepatitis. Adv Clin Chem. 2011;55:105–132. doi: 10.1016/B978-0-12-387042-1.00006-X. [DOI] [PubMed] [Google Scholar]
- 7.Hörl WH, Schmidt A. Low hepcidin triggers hepatic iron accumulation in patients with hepatitis C. Nephrol Dial Transplant. 2014;29(6):1141–1144. doi: 10.1093/ndt/gft467. [DOI] [PubMed] [Google Scholar]
- 8.Nelson JE, Klintworth H, Kowdley KV. Iron metabolism in nonalcoholic fatty liver disease. Curr Gastroenterol Rep. 2012;14(1):8–16. doi: 10.1007/s11894-011-0234-4. [DOI] [PubMed] [Google Scholar]
- 9.Cichoż-Lach H, Michalak A. Oxidative stress as a crucial factor in liver diseases. World J Gastroenterol. 2014;20(25):8082–8091. doi: 10.3748/wjg.v20.i25.8082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehta K, Busbridge M, Renshaw D, Evans RW, Farnaud S, Patel VB. Characterization of hepcidin response to holotransferrin in novel recombinant TfR1 HepG2 cells. Blood Cells Mol Dis. 2016;61:37–45. doi: 10.1016/j.bcmd.2016.06.008. [DOI] [PubMed] [Google Scholar]
- 11.Jacolot S, Férec C, Mura C. Iron responses in hepatic, intestinal and macrophage/monocyte cell lines under different culture conditions. Blood Cells Mol Dis. 2008;41(1):100–108. doi: 10.1016/j.bcmd.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 12.Rapisarda C, Puppi J, Hughes RD, Dhawan A, Farnaud S, Evans RW, et al. Transferrin receptor 2 is crucial for iron sensing in human hepatocytes. Am J Physiol Gastrointest Liver Physiol. 2010;299(3):G778-783. doi: 10.1152/ajpgi.00157.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gehrke SG, Kulaksiz H, Herrmann T, Riedel H-D, Bents K, Veltkamp C, et al. Expression of hepcidin in hereditary hemochromatosis: evidence for a regulation in response to the serum transferrin saturation and to non-transferrin-bound iron. Blood. 2003;102(1):371–376. doi: 10.1182/blood-2002-11-3610. [DOI] [PubMed] [Google Scholar]
- 14.Riemer J, Hoepken HH, Czerwinska H, Robinson SR, Dringen R. Colorimetric ferrozine-based assay for the quantitation of iron in cultured cells. Anal Biochem. 2004;331(2):370–375. doi: 10.1016/j.ab.2004.03.049. [DOI] [PubMed] [Google Scholar]
- 15.Mehta K, Greenwell P, Renshaw D, Busbridge M, Garcia M, Farnaud S, et al. Characterisation of hepcidin response to holotransferrin treatment in CHO TRVb-1 cells. Blood Cells Mol Dis. 2015;55(2):110–118. doi: 10.1016/j.bcmd.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 16.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-delta delta C(T)) method. Methods San Diego Calif. 2001;25(4):402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 17.Pigeon C, Ilyin G, Courselaud B, Leroyer P, Turlin B, Brissot P, et al. A new mouse liver-specific gene, encoding a protein homologous to human antimicrobial peptide hepcidin, is overexpressed during iron overload. J Biol Chem. 2001;276(11):7811–7819. doi: 10.1074/jbc.M008923200. [DOI] [PubMed] [Google Scholar]
- 18.Park CH, Valore EV, Waring AJ, Ganz T. Hepcidin, a urinary antimicrobial peptide synthesized in the liver. J Biol Chem. 2001;276(11):7806–7810. doi: 10.1074/jbc.M008922200. [DOI] [PubMed] [Google Scholar]
- 19.Moretti D, Goede JS, Zeder C, Jiskra M, Chatzinakou V, Tjalsma H, et al. Oral iron supplements increase hepcidin and decrease iron absorption from daily or twice-daily doses in iron-depleted young women. Blood. 2015;126(17):1981–1989. doi: 10.1182/blood-2015-05-642223. [DOI] [PubMed] [Google Scholar]
- 20.Girelli D, Trombini P, Busti F, Campostrini N, Sandri M, Pelucchi S, et al. A time course of hepcidin response to iron challenge in patients with HFE and TFR2 hemochromatosis. Haematologica. 2011;96(4):500–506. doi: 10.3324/haematol.2010.033449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rorsman P, Braun M. Regulation of insulin secretion in human pancreatic islets. Annu Rev Physiol. 2013;75:155–179. doi: 10.1146/annurev-physiol-030212-183754. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.