ABSTRACT
HIV-1 poorly infects monocyte-derived dendritic cells (MDDCs). This is in large part due to SAMHD1, which restricts viral reverse transcription. Pseudotyping HIV-1 with vesicular stomatitis virus G protein (VSV-G) strongly enhances infection, suggesting that earlier steps of viral replication, including fusion, are also inefficient in MDDCs. The site of HIV-1 fusion remains controversial and may depend on the cell type, with reports indicating that it occurs at the plasma membrane or, conversely, in an endocytic compartment. Here, we examined the pathways of HIV-1 entry in MDDCs. Using a combination of temperature shift and fusion inhibitors, we show that HIV-1 fusion mainly occurs at the cell surface. We then asked whether surface levels or intracellular localization of CD4 modulates HIV-1 entry. Increasing CD4 levels strongly enhanced fusion and infection with various HIV-1 isolates, including reference and transmitted/founder strains, but not with BaL, which uses low CD4 levels for entry. Overexpressing coreceptors did not facilitate viral infection. To further study the localization of fusion events, we generated CD4 mutants carrying heterologous cytoplasmic tails (LAMP1 or Toll-like receptor 7 [TLR7]) to redirect the molecule to intracellular compartments. The intracellular CD4 mutants did not facilitate HIV-1 fusion and replication in MDDCs. Fusion of an HIV-2 isolate with MDDCs was also enhanced by increasing surface CD4 levels. Our results demonstrate that MDDCs are inefficiently infected by various HIV-1 and HIV-2 strains, in part because of low CD4 levels. In these cells, viral fusion occurs mainly at the surface, and probably not after internalization.
IMPORTANCE Dendritic cells (DCs) are professional antigen-presenting cells inducing innate and adaptive immune responses. DCs express the HIV receptor CD4 and are potential target cells for HIV. There is debate about the sensitivity of DCs to productive HIV-1 and HIV-2 infection. The fusion step of the viral replication cycle is inefficient in DCs, and the underlying mechanisms are poorly characterized. We show that increasing the levels of CD4 at the plasma membrane allows more HIV fusion and productive infection in DCs. We further demonstrate that HIV fusion occurs mainly at the cell surface and not in an intracellular compartment. Our results help us understand why DCs are poorly sensitive to HIV infection.
KEYWORDS: dendritic cells, human immunodeficiency virus, virus entry
INTRODUCTION
Human immunodeficiency virus (HIV) infects immune cells, using CD4 as a receptor and CXCR4 or CCR5 as its main coreceptors. The target cells of the virus are CD4+ T lymphocytes and, to a lesser extent, dendritic cells (DCs) and macrophages. DCs are central components of the immune response. They patrol peripheral tissues, including mucosal sites of HIV-1 transmission; sense pathogens; and produce cytokines that can induce an antiviral state in the host. They also present antigens to effector immune cells, thereby inducing cytotoxic or helper activity in T cells and humoral responses in B cells. Different pathways for viral sensing and antigen presentation have been described in DCs. Some pathways require a productive infection, but antigens from captured viruses are also potently presented or cross-presented by DCs (1, 2). DCs can be divided into plasmacytoid DCs (pDCs) and myeloid-derived DCs (mDCs), which are composed of resident and migratory DCs. Resident DCs populate and remain in secondary lymphoid organs. Migratory DCs are present in peripheral tissues and can migrate through the lymph to the closest draining lymph nodes. Resident and migratory DCs can be further separated into subsets according to their ontogeny, function, and surface phenotype (3, 4). Recent multidimensional techniques have revealed that the myeloid compartment is more complex than initially thought and comprises at least four monocyte and six DC subsets, including novel pre-DC and pDC populations (5, 6).
The interaction of HIV with DCs has been the subject of extensive research (7–9). In addition to CD4 and CCR5, and depending on the cell subset and the maturation state of the DCs, they express various lectins, such as DC-SIGN (dendritic cell-specific intercellular adhesion molecule-3-grabbing nonintegrin) or Siglec-1, that allow viral capture and facilitate viral transmission to bystander CD4+ T cells (7–11). In monocyte-derived dendritic cells (MDDCs) and other noncycling cells, HIV-1 infection is restricted by SAMHD1, which impairs HIV-1 reverse transcription by maintaining a low intracellular level of deoxynucleoside triphosphates (dNTPs) (12–15). The HIV-2/simian immunodeficiency virus (SIV) Vpx protein degrades SAMHD1 and enhances HIV infection in MDDCs in vitro (12–15). Whether DCs are productively infected in vivo is not fully characterized. Ex vivo studies in viremic patients reported the presence of viral DNA in splenic and blood DCs at frequencies that may be 10 to 100 times lower than in CD4+ T lymphocytes (16, 17). Whether the presence of viral DNA in these DCs corresponds to replication-competent virus deserves further investigation. In the macaque model, myeloid cells are not a site of productive SIV infection, regardless of Vpx (18, 19). Rather, the viral DNA present in myeloid cells of these animals may result from phagocytosis of infected T cells (18). The role of Vpx is more likely to promote infection of noncycling CD4+ T cells than that of myeloid cells (19, 20). In vitro studies using cells isolated from healthy donors show low permissivity of myeloid DCs to HIV-1 infection in the absence of exogenous Vpx (14, 15, 21–23). There is debate regarding the sensitivity of DCs to HIV-2 infection. It has been proposed that HIV-2 naturally infects MDDCs, based on experiments using the laboratory-adapted HIV-2 ROD strain pseudotyped with vesicular stomatitis virus G protein (VSV-G) (24, 25). This replication was associated with immune detection of incoming viral cDNA by the innate sensor cGAS and with DC maturation (24). In contrast, we and others observed that primary HIV-2 isolates do not efficiently infect myeloid DCs or pDCs (20, 23). The sensitivity of DCs to HIV infection may vary depending on the cell subset or their anatomical distribution, and it was, for instance, recently reported that CD1c+ DCs, but not CD141+ DCs, are sensitive to HIV-1 and HIV-2 infection (26).
The localization of HIV fusion events in target cells is a matter of controversy (27–29). Some studies suggested that fusion may occur from within endosomes in lymphocytes and other cell lines (30, 31). However, it was also reported that fusion mainly takes place at the surfaces of primary CD4+ T cells (27). The localization of HIV fusion in DCs is not fully characterized. Due to their high phagocytic activity and their ability to capture viral particles upon lectin binding, DCs might allow fusion after virion internalization. However, compared to CD4+ T lymphocytes, DCs display lower levels of CD4 and CXCR4, whereas levels of CCR5 are higher (32, 33). HIV-1 or HIV-2 infection is significantly enhanced by pseudotyping viral particles with a VSV-G envelope (20, 22). In the absence of the VSV-G envelope, most incoming HIV particles in MDDCs are found in the endosomal compartment but do not efficiently enter the cytoplasm (34).
Here, we investigated the ability of HIV-1 to fuse with MDDCs. We asked whether HIV fusion occurs mainly at the cell surface or if virions captured in intracellular compartments can also establish infection. We used a recently described combination of temperature shift experiments and drugs blocking fusion (27, 35) to show that most entry events occur at the cell surface. Blocking macropinocytosis in MDDCs, an important pathway for HIV internalization in DCs (36), also had no effect on HIV-1 fusion, suggesting that viral particles fuse at the cell surface. Increasing the levels of CD4, but not those of CCR5, enhanced HIV-1 infection and fusion. Conversely, augmenting CXCR4 levels enhanced fusion of an X4-tropic HIV-1 strain. We further show that the presence of CD4 at the plasma membrane, and not within the cell, is required for optimal fusion.
RESULTS
HIV-1 NLAD8 fusion mainly occurs at the surfaces of MDDCs.
We first asked whether HIV fusion in MDDCs takes place at the surface and/or after viral internalization. MDDCs take up viral particles that can be transferred to CD4+ T cells or degraded in pathways leading to antigen presentation (37–39). Whether internalized virions may fuse with the endosomal membrane to establish a productive infection in MDDCs has not been fully characterized. To distinguish fusion at the cell surface from fusion in endosomes, we used a temperature-arrested state (TAS) protocol (27, 35), as outlined in Fig. 1A. At 22°C, virus binding or uptake is not affected, but the Env protein does not undergo the conformational changes required for fusion. T20 and maraviroc (MVC) are HIV fusion inhibitors that bind, respectively, to Env and the coreceptor CCR5. T20 is membrane impermeable, and therefore, it cannot access viral particles that have been previously endocytosed (27, 40, 41). The fusion events blocked by T20 thus occur at the cell surface. MVC, as a small-molecule inhibitor of fusion by R5-tropic viruses, is able to access endocytosed particles and was used as a positive control of inhibition. We incubated MDDCs with HIV-1 NLAD8 at 22°C for 2 h to allow viral internalization. T20 or MVC was then added for an additional 1 h at 22°C. The cells were then shifted to 37°C for 2 h to permit fusion, which was subsequently measured with a Vpr–β-lactamase (Vpr-Blam) fusion assay (20, 42). Briefly, viruses are produced in the presence of a Vpr-Blam chimeric protein that is incorporated into the virions. Target cells are loaded with CCF2-AM, a fluorescent substrate of β-lactamase. When the Vpr-Blam-containing viruses fuse with the target cells and β-lactamase gains access to the cytoplasm, the shift in fluorescence resulting from CCF2-AM cleavage is measured by flow cytometry.
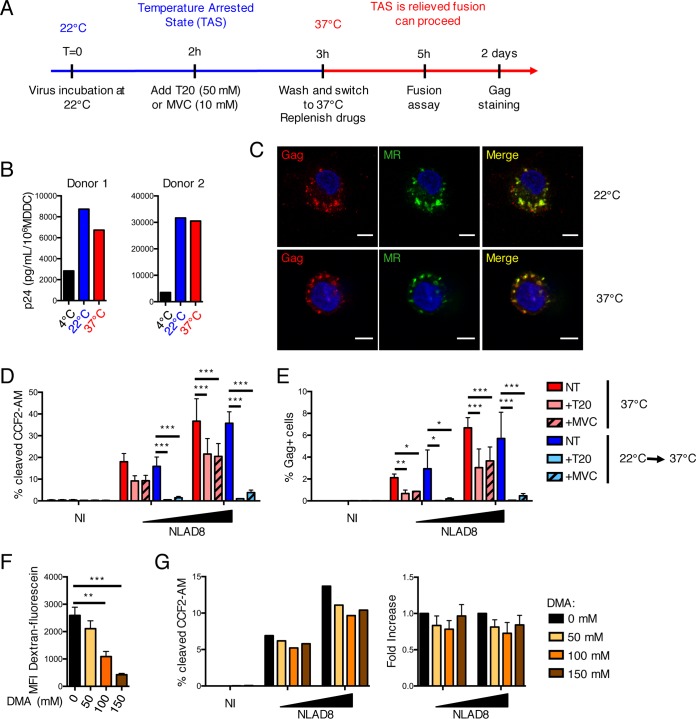
FIG 1.
HIV-1 NLAD8 fusion occurs at the cell surface in MDDCs. (A) Experimental outline. MDDCs were infected with HIV-1 NLAD8 at 22°C to induce the TAS. Before allowing fusion to proceed by shifting the temperature, the cells were treated or not with the fusion inhibitor T20 or MVC. After washing the virus, replenishing the drugs, and shifting the cells to 37°C, the cells were used for a fusion assay or further maintained in culture for 2 days to assess productive infection. (B and C) Incubation at 22°C does not impair HIV uptake in MDDCs. Cells incubated with NLAD8 at 4°C, 22°C, or 37°C for 2 h were lysed or analyzed by immunofluorescence. (B) Gag p24 levels were measured in cell lysates from 2 donors. (C) Cells were stained for Gag and mannose receptor, a marker of early endosomes. Scale bars, 5 μm. (D) T20 and MVC inhibit HIV-1 fusion in the TAS assay. Cells were exposed to virions containing the Vpr-Blam protein. The cells were then loaded with CCF2-AM for 2 h and analyzed by flow cytometry. Cells maintained at 37°C were used as controls. The data are means and standard errors of the mean (SEM) for 4 different donors. (E) T20 and MVC inhibit HIV-1 infection. MDDCs were treated as described for panel A, and productive infection was monitored by measuring the proportion of Gag-positive cells by flow cytometry 2 days after infection. The data are means and SEM for 3 to 5 different donors. (F and G) Macropinocytosis does not lead to viral fusion in MDDCs. The indicated amounts of DMA were used to inhibit macropinocytosis. (F) Effect of DMA on the uptake of dextran-fluorescein, as measured by flow cytometry as a control. Means and SEM for 4 different donors are shown. (G) Effect of DMA on HIV-1 fusion, assessed with the Vpr-Blam assay. (Left) One representative donor is shown. (Right) Fold increase in fusion compared to nontreated cells. The data are means and SEM for 4 different donors. *, P < 0.05; **, P < 0.01; ***, P < 0.001.
We first assessed whether incubation at 22°C altered binding and uptake of the virus relative to incubation at 37°C. With this aim, MDDCs were incubated with HIV-1 at 22°C or 37°C for 2 h. The amount of bound and/or internalized virus was quantified in cell lysates using the ultrasensitive SIMOA p24 assay (43), whereas the localization of incoming virions was examined by immunofluorescence and confocal microscopy analysis. As shown for 2 donors in Fig. 1B, we did not detect significant differences in cell-associated p24 levels at 22°C or 37°C. Moreover, we observed colocalization of incoming p24 with the mannose receptor (MR), a marker of endosomal compartments, with no detectable differences when viruses were incubated at 22°C or 37°C (Fig. 1C). Thus, as expected, incubating MDDCs at 22°C during viral exposure did not significantly modify the ability of the cells to bind and/or take up HIV-1.
Cells were also kept at 37°C throughout the fusion experiment to verify that preincubation at 22°C did not affect the capacity of viral particles to fuse. Fusion was similar after the TAS protocol and after continuous incubation at 37°C (Fig. 1D). When cells were exposed to HIV-1 at 37°C for 2 h before addition of T20 and MVC, partial inhibition of fusion occurred (Fig. 1D). As expected, adding drugs at the time of infection abrogated fusion (not shown). When cells were exposed to HIV-1 at 22°C for 2 h before drug treatment, both T20 and MVC inhibited HIV-1 fusion (Fig. 1D). Since T20 cannot block fusion of viral particles that were internalized before addition of the drug, these data strongly suggest that the viral particles that have been captured do not detectably gain access to the cytoplasm. We also followed productive infection of MDDCs by measuring the percentage of Gag+ cells at day 2 postinfection. Cells were preincubated with Vpx-containing virus-like particles (VLPs) prior to incubation at 22°C to degrade SAMHD1 and allow productive infection. The cells were then treated as described in the TAS protocol, and infection was assessed by flow cytometry (Fig. 1E). Productive infection after TAS was inhibited by T20 and MVC (Fig. 1E), confirming the results obtained in the fusion assay.
We next asked whether small-molecule inhibitors of endocytosis or macropinocytosis could impact HIV-1 fusion in MDDCs. The endocytosis inhibitors Dynasor and Dyngo-4a impair the activity of dynamin (30, 44). However, when tested at nontoxic concentrations, these compounds did not significantly inhibit the endocytosis of a control cellular protein (transferrin receptor) in MDDCs, precluding their further use on HIV-exposed cells (not shown). Dimethyl amiloride (DMA) is a macropinocytosis inhibitor that does not affect receptor-mediated endocytosis but decreases internalization of HIV particles in MDDCs (36). We examined the impact of DMA on the fusion of HIV in MDDCs. As a positive control, we treated cells with DMA before incubation with dextran-fluorescein, which enter cells through macropinocytosis. DMA inhibited dextran-fluorescein capture in a dose-dependent manner, as quantified by flow cytometry (Fig. 1F). In contrast, preincubation of MDDCs with the same doses of DMA did not prevent viral fusion (Fig. 1G). Macropinocytosed HIV-1 particles thus probably do not undergo fusion in MDDCs.
Taken together, these experiments strongly suggest that HIV-1 predominantly fuses at the surfaces of MDDCs.
Low levels of CD4 in MDDCs limit HIV-1 infection and fusion.
DCs express relatively low levels of CD4 compared to CD4+ T lymphocytes (32, 33, 45, 46). We assessed CD4 surface levels in blood CD11c+ mDCs. In peripheral blood mononuclear cells (PBMC) isolated from healthy donors, three different patterns of CD4 levels were observed (Fig. 2A). As expected, one population was negative for CD4, the second one displayed low levels of CD4 and included CD11c+ cells, and the third population expressed high CD4 levels and corresponded to CD4+ T lymphocytes. We then measured CD4, CXCR4, and CCR5 levels in MDDCs and CD4+ T cells (Fig. 2B). MDDCs expressed levels of CD4 similar to those expressed by myeloid DCs. They also expressed low CXCR4 and high CCR5 levels.
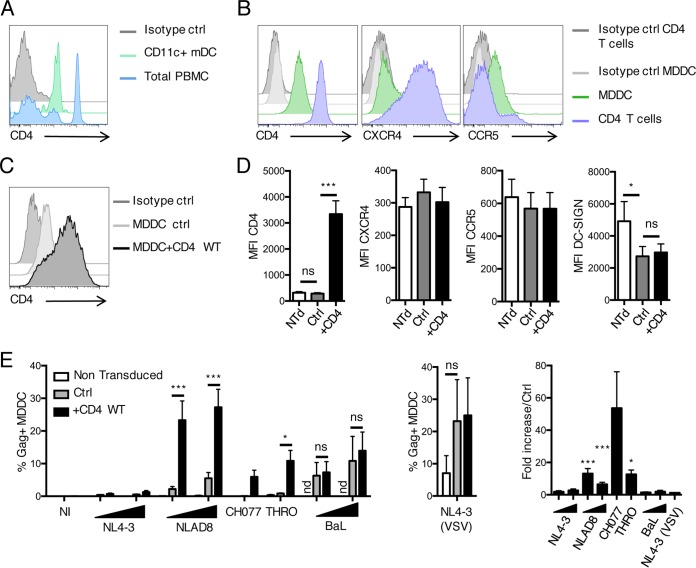
FIG 2.
CD4 levels modulate HIV infection in DCs. (A) CD11c+ mDCs express intermediate levels of CD4. Total PBMCs and mDCs (positive for HLA-DR and CD11c and negative for CD3, CD14, CD16, CD19, and CD56) were stained for CD4 surface expression. CD4 levels in one representative donor out of four are shown. (B) MDDCs and activated CD4+ T cells were stained for CD4, CXCR4, and CCR5 expression. One representative donor out of 4 is shown. (C and D) Nontransduced (Ntd) MDDCs or cells transduced with a lentiviral vector encoding CD4 (MDDC+CD4 WT) or luciferase (MDDC Ctrl) were stained for CD4 and, as controls, CXCR4, CCR5, and DC-SIGN. CD4 staining for 1 representative donor out of 4 (C) and the mean fluorescence intensity (MFI) of the indicated proteins (D) are shown as means and SEM from 4 donors. (E) HIV-1 infection is increased in MDDC plus CD4 WT. The cells described in panel C were infected with the indicated strains of HIV-1. After 3 days, productive infection was monitored by measuring the proportion of Gag-positive cells by flow cytometry. The results are means and SEM from 4 donors for HIV-1 strains (left) or as a control VSV-G-pseudotyped HIV-1 NL4-3 (middle); the fold increase of infection was calculated by comparing MDDC plus CD4 WT with MDDC Ctrl (right). *, P < 0.05; ***, P < 0.001; ns, not significant; nd, not done.
We then asked whether the low levels of CD4 may impact the sensitivity of MDDCs to HIV infection. With this aim, we transduced the cells with lentiviral vectors encoding CD4 (MDDC plus CD4 WT) or luciferase as a control (MDDC Ctrl). The cells were first treated with Vpx-containing VLPs to degrade SAMHD1 and allow lentiviral transduction. Compared with the control vector (Fig. 2C and D), transduction with the CD4 vector significantly increased CD4 surface levels without affecting those of CXCR4, CCR5, or DC-SIGN (Fig. 2D). We then exposed the transduced cells to four HIV-1 strains with different coreceptor usage: NLAD8 and the transmitted/founder (T/F) viruses CH077 and THRO mainly use CCR5 as a coreceptor (R5 viruses), whereas HIV-1 NL4-3 uses CXCR4 (X4 virus). In all infection experiments, cells were pretreated with Vpx-containing VLPs to ensure that SAMHD1 was degraded to allow productive infection. The extent of infection was assessed 3 days later by measuring the proportion of Gag-positive cells by flow cytometry. Increasing CD4 levels significantly enhanced the sensitivity of MDDCs to infection by all 4 viral strains (Fig. 2E). As expected, infection with VSV-G-pseudotyped HIV-1 was not modulated by overexpression of CD4 (Fig. 2E). Infection with HIV-1 NL4-3 was modestly enhanced (2-fold increase), whereas the R5 strains were increased by 5- to 50-fold (Fig. 2E).
HIV-1 BaL is a macrophage-adapted R5 strain that infects cells with low CD4 density (47). HIV-1 BaL infected control MDDCs and cells overexpressing CD4 WT at similar levels (Fig. 2E). Therefore, increasing CD4 levels in target cells does not enhance sensitivity of infection for strains that can efficiently use low CD4 levels for entry.
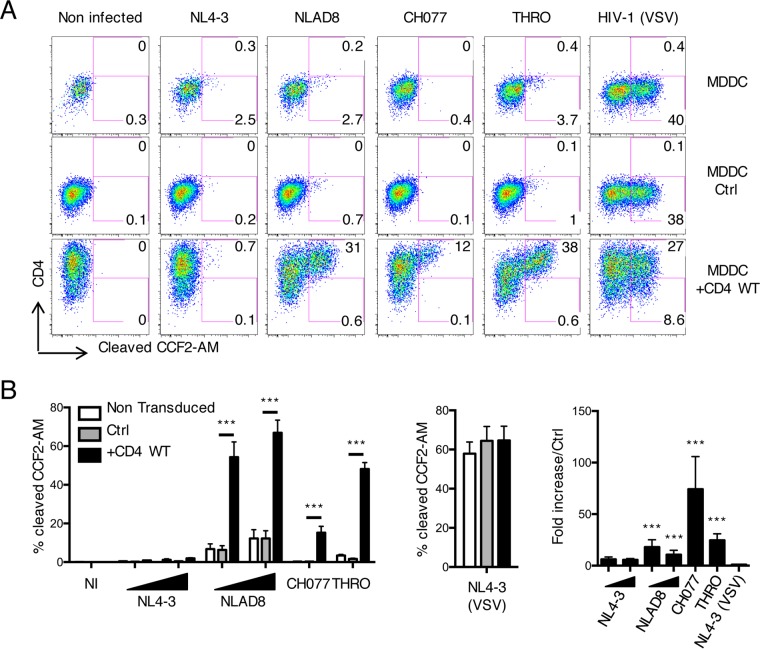
We next asked whether this increase of infection was due to an enhancement of fusion. Fusion events were measured with the Vpr-Blam fusion assay as described above. A representative experiment with cells from one donor is presented Fig. 3A, whereas the means of the results of independent experiments with at least 4 donors are displayed in Fig. 3B. Fusion in nontransduced MDDCs and in cells transduced with the control vector was low for all HIV-1 strains tested (Fig. 3A and B). In MDDCs plus CD4 WT, HIV-1 fusion was selectively enhanced in the fraction of cells expressing high levels of CD4 (Fig. 3A). NL4-3 fusion was modestly increased (2-fold), whereas fusion with R5 strains was increased by 5- to 70-fold (Fig. 3B), corresponding to the differences observed in infection. The VSV-G-pseudotyped HIV-1 particles efficiently fused in MDDCs, irrespective of CD4 surface levels (Fig. 3A and B).
FIG 3.
High levels of CD4 enhance HIV-1 fusion in MDDCs. MDDCs were transduced with vectors encoding luciferase (MDDC Ctrl) or CD4 WT (MDDC+CD4 WT). Nontransduced MDDCs were used as an additional control. The cells were exposed to the indicated viral particles containing the Vpr-Blam protein for 2 h. The cells were then loaded with CCF2-AM for 2 h, stained for CD4, and analyzed by flow cytometry. (A) One representative experiment. (B) Results (means and SEM from at least 4 donors for HIV-1 strains [left] or VSV-G-pseudotyped HIV-1 NL4-3 [middle]); the fold increase in fusion was calculated by comparing MDDC plus CD4 WT with MDDC Ctrl (right). ***, P < 0.001.
Altogether, these experiments show that HIV-1 infection and fusion are low in MDDCs but are strongly enhanced by the overexpression of CD4 for strains that did not acquire the ability to use low levels of CD4 for fusion.
Importance of coreceptor levels for HIV-1 infection in MDDCs.
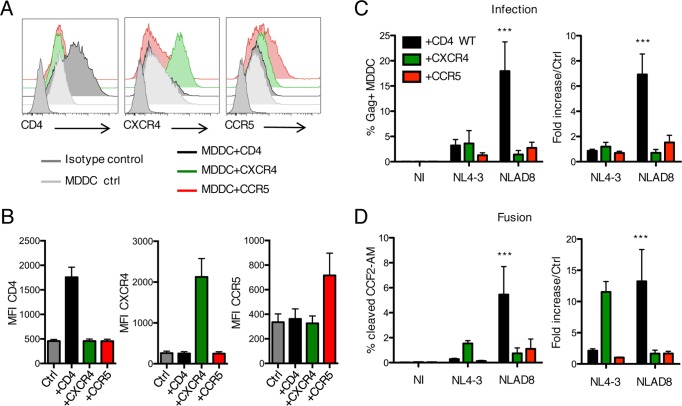
We then used overexpression experiments to ask whether CXCR4 and CCR5 levels also modulate HIV-1 infection in MDDCs. We transduced cells with lentiviral vectors encoding CXCR4 (MDDC plus CXCR4) or CCR5 (MDDC plus CCR5) (Fig. 4A and B). The increase of CCR5 was modest, either because MDDCs already display high basal levels of the molecule or because the process of transduction was not optimal with the vector. As a positive control, we generated MDDCs plus CD4 WT. We then measured infection and fusion, using one X4 (NL4-3) and one R5 (NLAD8) strain (Fig. 4C and D). Increasing CXCR4 levels enhanced NL4-3 fusion by 10-fold but did not enhance productive infection. As expected, NLAD8 fusion and infection were not enhanced by the overexpression of CXCR4. Interestingly, increasing CCR5 levels did not enhance fusion or infection by the two strains.
FIG 4.
Importance of coreceptor levels for HIV-1 infection of MDDCs. (A and B) MDDCs were transduced with vectors encoding CXCR4 (MDDC+CXCR4) or CCR5 (MDDC+CCR5); stained for expression of CD4, CXCR4, and CCR5; and analyzed by flow cytometry. One representative donor out of 4 (A) and MFI of the indicated markers (B) are shown as means and SEM for 4 donors. (C) The transduced MDDCs were infected with NL4-3 or NLAD8 HIV-1 strains. After 3 days, productive infection was monitored by measuring the proportion of Gag-positive cells by flow cytometry. (Left) The results are means and SEM for at least 4 donors. (Right) The fold increase in infection was calculated by comparing transduced cells to MDDC Ctrl. (D) The transduced cells were used for a fusion assay as described in the legend to Fig. 3. (Left) The results are means and SEM for at least 4 donors. (Right) The fold increase in infection was calculated by comparing transduced cells to MDDC Ctrl. ***, P < 0.001.
These experiments show that the low levels of CXCR4 modulate fusion by an X4 strain. However, the sensitivity of the cells to productive infection remains low, suggesting that further blocks may restrict later steps of NL4-3 replication. In contrast, endogenous CCR5 levels are sufficient for fusion and infection by an R5 strain, which are not further enhanced when the coreceptor is overexpressed.
Increasing CD4 levels in intracellular compartments does not enhance HIV-1 infection or fusion.
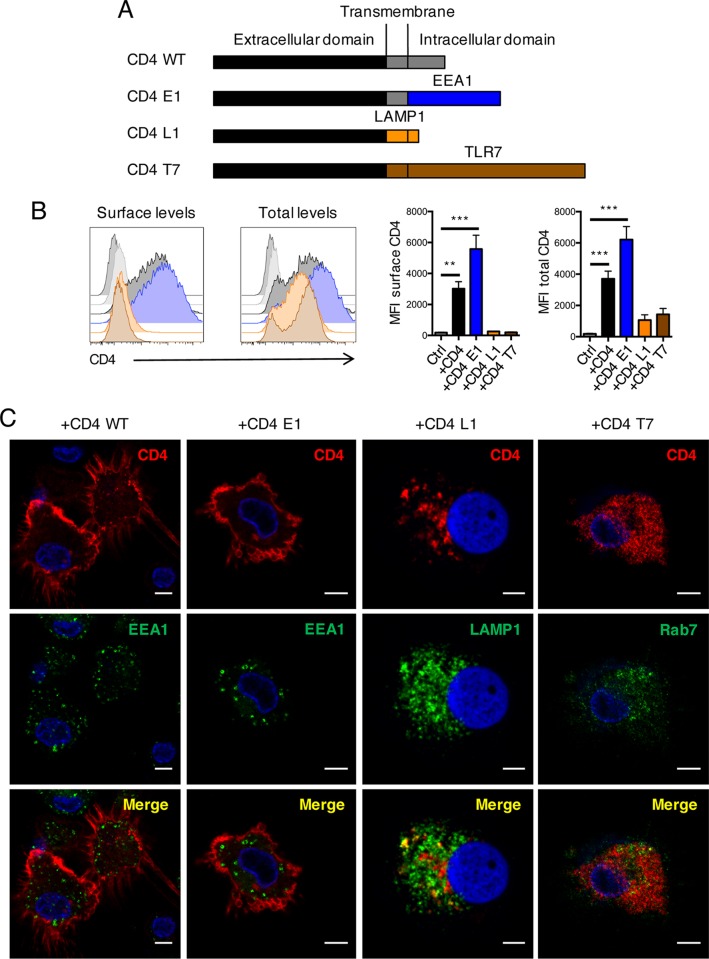
We next asked whether CD4 present in endosomes might promote infection from within the compartment. We engineered chimeras composed of the extracellular domain of CD4 and the transmembrane and cytoplasmic domains of three different endosomal proteins (Fig. 5A). The cytoplasmic tails of proteins contain trafficking signals routing the proteins to selective intracellular environments. For instance, relocalization of CD4 to late endosomes/lysosomes has been previously performed by adding the LAMP1 cytoplasmic tail to the extracellular domain of CD4 (48, 49). To redirect CD4 to early endosomes, we fused CD4 with the intracellular domain of EEA1 (early endosome antigen 1) (CD4 E1). To redirect CD4 to late endosomes or lysosomes, we created chimeras with the transmembrane and cytoplasmic domains of the lysosomal protein LAMP1 (CD4 L1) or the endosomal/lysosomal protein Toll-like receptor 7 (TLR7) (50–53) (CD4 T7). These chimeras were used to transduce MDDCs, yielding MDDC plus CD4 E1, MDDC plus CD4 L1, and MDDC plus CD4 T7. Their localization was first assessed by flow cytometry. Surface levels were measured by staining the cells in the absence of permeabilization, whereas total levels (surface and intracellular) were quantified after permeabilization (Fig. 5B). CD4 WT was detected at the surface, and permeabilization did not enhance the staining. This was also the case for CD4 E1, indicating that the molecule unexpectedly did not accumulate in an early endosomal compartment. EEA1 is a soluble protein, and its localization signal is a complex zinc finger-containing domain. Adding the localization domain of EEA1 to a transmembrane protein might have disrupted its conformation, rendering it nonfunctional. We therefor used the mutant as an additional control for overexpression of CD4 at the cell surface. In contrast, the CD4 L1 and CD4 T7 molecules were not detected at the plasma membrane. However, the chimeras were readily detected after cell permeabilization. We confirmed these findings by costaining the cells with CD4 and early endosomal (EEA1), late endosomal (Rab7), or lysosomal (LAMP1) markers (Fig. 5C). As expected, CD4 WT and CD4 E1 were mostly localized at the plasma membrane and poorly colocalized with EEA1. CD4 L1 and CD4 T7 were barely detected at the cell surface. CD4 L1 displayed clustered intracellular staining that partly colocalized with LAMP1 (Fig. 5C). CD4 T7 showed a more diffuse pattern, with no obvious costaining with LAMP1 (not shown) and partial colocalization with Rab7 (Fig. 5C).
FIG 5.
Generation and characterization of CD4 chimeras. (A) Schematic representation of CD4 WT and a chimera containing the transmembrane and intracellular domains of the indicated proteins. (B) MDDCs were transduced with lentiviral vectors encoding CD4 WT (+CD4 WT), CD4 E1 (+CD4 E1), CD4 L1 (+CD4 L1), and CD4 T7 (+CD4 T7) proteins. CD4 levels were assessed by flow cytometry after fixation and staining without permeabilization (surface levels) or with permeabilization with 0.05% saponin (total levels). One representative donor out of 4 is shown in the two left panels, and MFI is shown in the two right panels as means and SEM for 4 donors. **, P < 0.01; ***, P < 0.001. (C) Transduced cells were seeded on coverslips, fixed, and permeabilized before costaining with antibodies against CD4 (red) and the indicated endosomal markers (green). The merged images (bottom row) highlight the colocalization events (yellow). Representative images from 4 independent donors are shown. Scale bars, 5 μm.
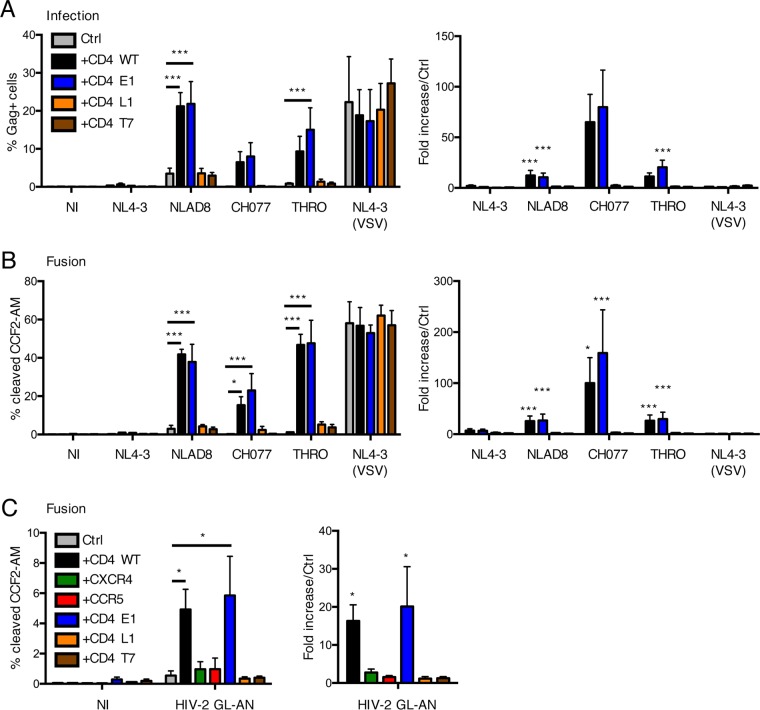
We then assessed the abilities of the different CD4 chimeras to enhance HIV-1 replication. To this end, transduced cells were exposed to several HIV-1 isolates, and viral infection (Fig. 6A) and fusion (Fig. 6B) were measured as described above. CD4 WT and CD4 E1 both strongly enhanced infection and fusion. In sharp contrast, CD4 L1 and CD4 T7 did not improve viral replication and access to the cytoplasm.
FIG 6.
Impact of CD4 chimeras on HIV fusion and infection in MDDCs. MDDCs were transduced with the CD4 chimeras shown in Fig. 5. (A) Effect of the CD4 chimeras on HIV-1 infection. Cells were infected with the indicated strains of HIV-1. After 3 days, productive infection was monitored by measuring the proportion of Gag-positive cells by flow cytometry. (Left) The results are means and SEM for at least 4 donors. (Right) The fold increase in infection was calculated by comparing transduced cells to MDDC Ctrl. (B) Effect of CD4 chimeras on HIV-1 fusion. The transduced cells were used for a fusion assay. (Left) Results are means and SEM for at least 4 donors. (Right) The fold increase in fusion was calculated by comparing transduced cells to MDDC Ctrl. (C) Effect of the CD4 chimeras on HIV-2 fusion. The transduced cells were used for a fusion assay, using the HIV-2 strain GL-AN. The fold increase in fusion was calculated by comparing transduced cells to MDDC Ctrl. The results are means and SEM for at least 3 donors. *, P < 0.05; ***, P < 0.001.
We recently reported that HIV-2 also poorly infects MDDCs when viral particles are not pseudotyped with VSV-G, due to a fusion defect (20). We thus examined whether HIV-2 fusion can be enhanced by the overexpression of CD4. MDDCs transduced with WT or chimeric CD4 molecules were exposed to HIV-2 GL-AN (20), and a fusion assay was performed. As with HIV-1, HIV-2 GL-AN fusion was increased by 15-fold with CD4 WT and CD4 E1 molecules, whereas CD4 L1 and T7 did not enhance fusion (Fig. 6C).
Therefore, the presence of CD4 at the cell surface, and not in intracellular compartments, promotes fusion of various HIV-1 and HIV-2 strains with MDDCs.
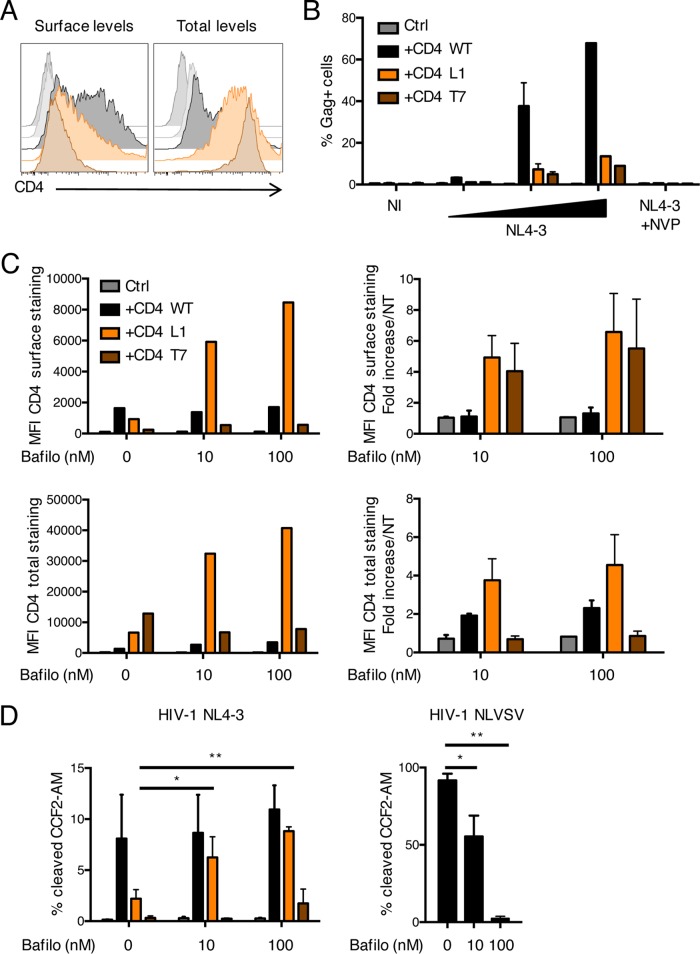
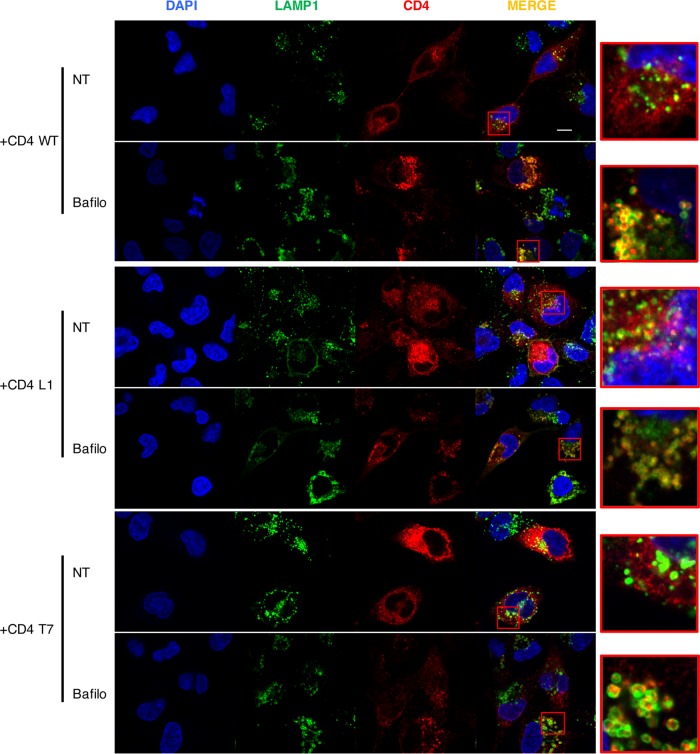
We then examined the behavior of these CD4 chimeras in CHME cells. This human microglial cell line was selected because it lacks endogenous CD4 expression (54). We transduced the cells with lentiviral vectors expressing CD4 WT, CD4 L1, or CD4 T7 and used them for infection and fusion assays. CD4 WT was present at the cell surface, whereas CD4 L1 and CD4 T7 were mostly found in the cell interior, with low but detectable levels at the surface (Fig. 7A). CD4 WT allowed HIV-1 infection, and both CD4 L1 and CD4 T7 permitted a modest increase in HIV-1 infection. This strongly suggests that the CD4 chimeras can bind gp120 and allow infection when present at the cell surface. We then asked whether bafilomycin A1, an inhibitor of vesicular acidification, and degradation by pH-sensitive proteases (55) may modify the steady-state levels of the CD4 chimeras. Bafilomycin A1 did not significantly impact CD4 WT or CD4 T7 but strongly increased the surface levels of CD4 L1 (Fig. 7C), suggesting that the molecule might be degraded when it reaches the endosomal compartment. We then performed fusion assays in CHME cells (Fig. 7D). In the absence of bafilomycin A1, CD4 WT and, to a lesser extent, CD4 L1 and CD4 T7 molecules allowed HIV-1 fusion. The addition of bafilomycin A1 had no or minor positive effect on fusion mediated by CD4 WT or CD4 T7, respectively. In contrast, bafilomycin A1 restored viral fusion mediated by CD4 L1, reflecting the enhancement of surface expression of the molecule. As a positive control, we verified that bafilomycin A1 inhibited fusion of HIV particles pseudotyped with VSV-G, which requires vesicular acidification for entry (Fig. 7D). We next performed confocal microscopy analysis to analyze the effect of bafilomycin A1 on the localization of the various chimeras in LAMP1+ endosomes/lysosomes (Fig. 8). For CD4 WT, CD4 L1, and CD4 T7, the inhibitor increased colocalization with LAMP1.
FIG 7.
Impact of CD4 chimeras on HIV fusion and infection in CHME cells. CHME cells were transduced with the CD4 chimeras described in the legend to Fig. 5. (A) CD4 levels were assessed in cells by flow cytometry after fixation and staining without permeabilization (surface levels) or with permeabilization with 0.05% saponin (total levels). One representative staining is shown. (B) Cells were infected with HIV-1 NL4-3. After 3 days, productive infection was monitored by measuring the proportion of Gag-positive cells by flow cytometry. The results are means and SEM for 3 independent experiments. (C and D) CHME cells were treated with the indicated doses of bafilomycin A1 for 24 h. (C) CD4 levels were assessed by flow cytometry as for panel A. (Left) One representative experiment. (Right) Means and SEM for 3 experiments. (D) Cells were then used for a fusion assay with the indicated viruses. The data are means and SEM for 3 independent experiments. *, P < 0.05; **, P < 0.01.
FIG 8.
Localization of CD4 chimeras in CHME cells. CHME cells transduced with the CD4 chimeras were treated or not with bafilomycin A1 (100 nM) (Bafilo). After 24 h, the cells were costained with CD4 (red) and the lysosomal marker LAMP1 (green). One representative image per condition from 3 independent experiments is shown. The red squares indicate the zone that has been magnified on the right. Scale bar, 10 μm.
Altogether, these experiments strongly suggest that the CD4 chimeras have the ability to bind gp120 and allow infection. CD4 L1 is probably rapidly degraded in an endosomal compartment and triggers fusion when present at the cell surface. CD4 T7 is present in endosomal compartments in the presence of bafilomycin A1, but the low surface levels of the molecules do not allow efficient HIV-1 entry.
DISCUSSION
DCs are poorly sensitive to productive HIV infection, in large part because viral reverse transcription is impaired by SAMHD1. Earlier steps of the viral life cycle are also suboptimal, and it has been observed that HIV-1 and HIV-2 fusion may be limited in MDDCs (20, 56). Here, we further investigated the sensitivity of MDDCs to HIV fusion. We studied the importance of receptor and coreceptor levels and examined the cellular localization of viral fusion events. We report that HIV-1 fusion mainly takes place at the plasma membrane in MDDCs. This process is inefficient because of the low surface levels of CD4. Rerouting CD4 to intracellular compartments does not further increase viral entry and replication in these cells.
We first used a TAS protocol (27, 35), as well as inhibition of macropinocytosis, to show that HIV fusion mainly occurs at the plasma membrane and probably not after viral particle internalization. DCs display intracellular invaginations connected to the cell surface and lacking markers of endosomes, lysosomes, or antigen-processing vesicles, in which captured viral particles may accumulate before transfer to CD4+ T cells (57–59). In DCs, viral capture is mainly due to virion binding to lectins, such as DC-SIGN and Siglec-1 (7–11, 60). Env binding to DC-SIGN may prevent fusion by impairing interaction with CD4 (61). This suggests that viral fusion at the plasma membrane and in these surface-connected intracellular compartments may be regulated by the relative amounts and competition between Env-binding receptors that allow or do not allow productive infection.
DCs express low levels of CD4 and CXCR4, whereas CCR5 levels are higher than in lymphocytes (32, 33, 62, 63). DC maturation is associated with modulation of the expression of a large array of cellular proteins. HIV fusion with DCs declines as cells mature and lose CCR5 (56). To study the role of CD4 and coreceptor levels in viral fusion, we transduced immature MDDCs with lentiviral vectors encoding these molecules. Lentiviral transduction as assessed with a control vector induced partial maturation of DCs with moderate upregulation of CD83 and CD86 (not shown) and downregulation of DC-SIGN but did not affect endogenous levels of CD4, CCR5, or CXCR4. However, viral fusion occurred similarly in nontransduced cells and in cells transduced with the control vector. We show that the overexpression of CD4 enhances HIV-1 fusion and infection, strongly suggesting that the low endogenous levels of the receptor limit viral infection. Alternatively, and not exclusively, it is possible that a restriction factor limits fusion or that a cellular protein facilitating entry is lacking or is suboptimally expressed in MDDCs. Overexpressing CD4 may compensate for these limitations. Increasing CXCR4 levels enhanced fusion but not productive infection by an X4 strain, confirming the existence of additional postfusion blocks (45). In contrast, CCR5 levels are naturally elevated in MDDCs, and overexpressing the molecule did not further improve infection.
Recent unbiased single-cell RNA sequencing and mass cytometry (cytometry by time of flight [CyTOF]) analysis of human blood cells identified at least four monocyte and six DC subsets, including novel pre-DC and pDC populations (5, 6). These high-dimensional techniques revealed that the DC compartment is more complex than initially thought. A recent study also demonstrated that CD141+ DCs display innate resistance to infection by a broad range of enveloped viruses, including HIV, whereas CD1c+ cells are susceptible to infection (26). The ability of CD141+ DCs to resist infection is conferred by Rab15, a vesicle-trafficking protein (26). It will be of interest to determine the levels and roles of molecules such as Rab15, CD4, and coreceptors and sensitivity to HIV-1 fusion and infection across the spectrum of DC subsets.
We also designed CD4 chimeras to redirect the receptor to various endosomal compartments. This strategy was only partly successful. Addition of the cytoplasmic domain of the early endosomal marker transferrin receptor (not shown) or EEA1 did not redistribute CD4 from the plasma membrane. This might be due to the constant recycling of early endosomal membrane components to the surface. However, addition of the transmembrane and cytoplasmic domains of the LAMP1 lysosomal or TLR7 endosomal/lysosomal proteins prevented surface expression of the chimeras, which were detected intracellularly. These two proteins partially costained with late endosomal/lysosomal markers. However, the intracellular CD4 molecules did not enhance HIV fusion and productive infection. This strongly suggests that the presence of CD4 in late endosomal/lysosomal compartments does not allow efficient access of incoming HIV particles to the cytoplasm. It does not rule out the possibility that fusion might occur in an earlier endosomal compartment. It is possible that virions reaching endosomes or lysosomes are rapidly degraded, preventing further fusion (64, 65). This is in line with a previous report indicating that although HIV-1 enters MDDCs predominantly through endocytosis, the endocytosed virions cannot initiate productive infection (34). Another nonexclusive explanation is that most of the viral particles are captured upon binding to lectins and then reach the nonlysosomal, nonacidic compartment that is connected to the cell surface. It will be of interest to examine whether this intracellular compartment, containing CD81 and other tetraspanins (7–11), may be a site of viral fusion. Of note, we previously reported that HIV-2 fusion is low in MDDCs (20). We further show here that, as for HIV-1, the poor access of incoming HIV-2 to the cytoplasm is due to low CD4 levels at the plasma membrane.
The route of viral entry may modulate innate sensing and antigen presentation by DCs (1, 38, 53, 66–68). As expected, infection of MDDCs overexpressing wild-type CD4 resulted in enhanced expression of the interferon-stimulated MxA gene (not shown), indicating that the increased viral infection augmented innate sensing. In contrast, this was not the case with the CD4 L1 or CD4 T7 chimera (not shown). It is tempting to speculate that low viral accumulation and/or fusion within an endosomal/lysosomal compartment may limit viral sensing by MDDCs. Whether antigen cross-presentation may be modulated by the intracellular localization of CD4 deserves future study.
Interestingly, infection by HIV-1 BaL was not enhanced in MDDCs overexpressing CD4. HIV-1 BaL was selected in macrophage cultures and has the ability to use low levels of CD4 for fusion. However, adaptation to infect low-level CD4-expressing cells may widen HIV-1 tropism but is associated with slower kinetics of entry and severely impacts envelope functionality (69). Interestingly, the transmitted/founder strains that most likely first encounter DCs at the site of infection require high levels of CD4 for fusion, and their infection was enhanced in MDDCs overexpressing the receptor.
In summary, our results indicate that multiple barriers prevent productive infection of MDDCs by various HIV-1 and HIV-2 strains, the earliest of which is due to low CD4 surface levels that limit viral fusion.
MATERIALS AND METHODS
Cells and reagents.
PBMCs were isolated from the blood of healthy donors by Ficoll centrifugation. The blood was provided by the EFS (Etablissement Francais du Sang, the official French blood bank). CD4+ T lymphocytes and CD14+ monocytes were isolated from PBMCs by positive selection using magnetic beads (CD4 and CD14 microbeads; Miltenyi Biotech). Primary CD4+ T lymphocytes were activated using phytohemagglutinin (PHA) (1 μg ml−1) and grown in RPMI medium complemented with 10% heat-inactivated fetal calf serum (FCS) and interleukin 2 (IL-2) for 3 days before staining. MDDCs were generated as described previously (20) by culturing monocytes with 50 ng ml−1 IL-4 and 10 ng ml−1 granulocyte-macrophage colony-stimulating factor (GM-CSF) for 5 days. CHME3 microglial cells (termed CHME cells here) have been described previously (54). The fusion inhibitors MVC and T-20 were from the NIH AIDS reagent program.
Viruses and virus-like particles.
HIV-1 strains were produced by calcium-phosphate transfection of HEK-293T cells. HIV-1 NLAD8 is a chimera of HIV-1 NL4-3 with the AD8 CCR5-tropic envelope. HIV-1 THRO and CH077 are CCR5-tropic transmitted/founder viruses from the NIH AIDS reagent program. HIV-1 BaL was obtained from culture supernatant of chronically infected MOLT cells (70). The HIV-2 strain GL-AN was described previously(20). VSV-G-pseudotyped viruses were obtained by cotransfection of HEK-293T cells with the corresponding proviruses and a VSV-G expression plasmid. For fusion assays, these viruses were produced as described above in the presence of a plasmid encoding the Vpr–β-lactamase fusion protein (42). For HIV-2, the plasmid encoding β-lactamase fused to HIV-2 Vpr was a kind gift from Matthias Dittmar (71). VLPs containing Vpx were produced using SIV-3+ WT plasmids as described previously (13, 14). The CD4 mutants (CD4 E1, CD4 L1, and CD4 T7) were constructed by gene synthesis and inserted in a pTrip CD4 WT vector (72). The vectors encoding CD4 WT, the various CD4 mutants, CXCR4, and CCR5 were produced by cotransfection of HEK-293T cells with the corresponding pTrip plasmid, the pR8.2 packaging construct, and a VSV-G expression plasmid.
Transduction of MDDCs and CHME cells.
Monocytes were treated immediately after isolation with Vpx-containing SIV VLPs in RPMI medium complemented with 10% FCS, 50 ng ml−1 IL-4, 10 ng ml−1 GM-CSF, and 10 mM HEPES. After 2 h, the cells were suspended at 2 × 106 cells ml−1 in the same medium and transduced with the indicated lentiviral vectors at 75 ng p24 ml−1 in 2.5 ml. The monocytes were then differentiated into MDDCs and used at day 5 postdifferentiation. CHME cells were transduced as described previously (54).
Infection and fusion assays.
MDDCs were seeded in 96-well plates at 1 × 105 to 2 × 105 cells per well. Infections were performed using the indicated viruses (at 100 to 300 ng ml−1 p24 in 100 to 200 μl) in the presence of 10 mM HEPES and 2 μg ml−1 DEAE dextran. For viral replication assays, cells were pretreated with Vpx-containing VLPs 2 h before viral exposure. The infection was monitored 3 days later by flow cytometry. As expected, we did not detect productive infection of MDDCS in the absence of Vpx-containing VLPs (not shown). Viral fusion was assessed as described previously (42). Briefly, MDDCs were exposed to ultracentrifuged viruses containing the Vpr–β-lactamase fusion protein. After 2 h, the cells were washed in cold CO2-independent medium (Invitrogen) without FCS. The cells were then resuspended in CO2-independent medium supplemented with 10% FCS and incubated with the CCF2-AM substrate (CCF2-AM kit; Invitrogen) in the presence of 1.8 mM probenecid (Sigma) for 2 h at room temperature. After 3 washes in cold CO2-independent medium, the cells were either fixed in 4% paraformaldehyde (PFA) for 10 min or surface stained with CD4-allophycocyanin (APC) antibody for 30 min at 4°C before fixing. The cells were then resuspended in phosphate-buffered saline (PBS)-1% bovine serum albumin (BSA)-1.8 mM probenecid. The cleaved CCF2-AM fluorescence (excitation at 405 nm; emission at 450 nm) was measured by flow cytometry using the DAPI (4′,6-diamidino-2-phenylindole) channel on a FACSCanto II (BD). In some experiments, the same DC samples were used to assess both viral fusion and replication. We verified that the preincubation of MDDCs with Vpx-containing VLPs did not impact viral fusion (not shown). Moreover, omitting DEAE dextran decreased the efficacy of viral fusion, but overexpressing CD4 had the same impact on HIV fusion with or without DEAE dextran (not shown). DMA was from Sigma. MDDCs were treated with increasing doses of the drug for 45 min before addition of the virus or of 40-kDa dextran-fluorescein as a control. For fusion assays in CHME cells, cells were seeded in 24-well plates at 1 × 105 cells per well 1 day before the experiment. The cells were then left untreated or treated overnight with bafilomycin A1 at 10 or 100 nM. The cells were washed twice and then used either for the Vpr-Blam assay or for immunofluorescence analysis.
Binding and uptake quantification by SIMOA p24 assay.
MDDCs were seeded in 96-well plates at 1 × 105 to 2 × 105 cells per well. Infections were performed for 2 h using the indicated viruses (at 100 to 300 ng ml−1 p24 in 100 to 200 μl). The cells were then washed and either processed for immunofluorescence or lysed to measure cell-associated p24 levels by ultrasensitive digital enzyme-linked immunosorbent assay (ELISA) (Simoa) (43).
Flow cytometry.
Cell surface staining was performed for 30 min at 4°C with the following antibodies: CD4-phycoerythrin (PE) (Miltenyi), CD4-APC (Beckman Coulter), and uncoupled CXCR4 and CCR5 (12G5 and clone 2D7 antibodies, respectively, from the NIH AIDS reagent program), DC-SIGN–PE (Beckman Coulter), Lineage Cocktail 1 fluorescein isothiocyanate (FITC) (BD), CD11c-PE (Miltenyi), CD83-APC (Becton Dickinson), CD86-PE (Beckman Coulter), and goat anti-mouse IgG2a A647 (Life Technologies). For surface or intracellular staining, cells were fixed in 4% PFA for 10 min and incubated with the antibodies in PBS-1% BSA with or without 0.05% saponin. For Gag staining, cells were fixed in 4% PFA for 10 min and incubated with the KC57-PE monoclonal antibody (Beckman Coulter) in PBS-1% BSA-0.05% saponin for 30 min at 4°C. Samples were analyzed on a FACSCanto II (BD).
Immunofluorescence.
Cells were seeded on poly-l-lysine-coated coverslips and fixed in 4% PFA for 10 min. The cells were then stained as described previously (61) in PBS-1% BSA-0.05% saponin using the following antibodies: CD4-biotin (Miltenyi), CD4 (AbCam), EEA1 (Cell Signaling), LAMP1 (Santa Cruz), Rab7 (Cell Signaling), mannose receptor (BD Pharmingen), streptavidin-Cy5 (Jackson), anti-rabbit A488 (Life Technologies), and goat anti-mouse IgG1 Cy3 (Jackson). Samples were analyzed on a confocal microscope (Leica LSM 700 upright).
Statistical analyses.
Statistical analyses were performed using two-way analysis of variance (ANOVA), followed by a Dunnett multiple-comparison test or (Fig. 1F, 2D, and 4B) one-way ANOVA followed by Dunn's multiple-comparison test using GraphPad Prism software.
ACKNOWLEDGMENTS
We thank all the members of the Virus and Immunity Unit for helpful discussions. We thank the EFS and the NIH AIDS Research and Reference Reagent Program for providing reagents.
The work was supported by grants from the CHIKV-Viro-Immuno (ANR-14-CE14-0015-01) and TIMTAMDEN (ANR-14-CE14-0029) projects, the Labex IBEID program (ANR-10-IHUB-0002), the Vaccine Research Institute (ANR-10-LABX-77-01), the Gilead HIV Cure program, and Institut Pasteur.
REFERENCES
- 1.Buseyne F, Le Gall S, Boccaccio C, Abastado JP, Lifson JD, Arthur LO, Rivière Y, Heard JM, Schwartz O. 2001. MHC-I-restricted presentation of HIV-1 virion antigens without viral replication. Nat Med 7:344–349. doi: 10.1038/85493. [DOI] [PubMed] [Google Scholar]
- 2.Alloatti A, Kotsias F, Magalhaes JG, Amigorena S. 2016. Dendritic cell maturation and cross-presentation: timing matters! Immunol Rev 272:97–108. doi: 10.1111/imr.12432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guilliams M, Ginhoux F, Jakubzick C, Naik SH, Onai N, Schraml BU, Segura E, Tussiwand R, Yona S. 2014. Dendritic cells, monocytes and macrophages: a unified nomenclature based on ontogeny. Nat Rev Immunol 14:571–578. doi: 10.1038/nri3712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Segura E, Amigorena S. 2015. Cross-presentation in mouse and human dendritic cells. Adv Immunol 127:1–31. doi: 10.1016/bs.ai.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Villani A-CC, Satija R, Reynolds G, Sarkizova S, Shekhar K, Fletcher J, Griesbeck M, Butler A, Zheng S, Lazo S, Jardine L, Dixon D, Stephenson E, Nilsson E, Grundberg I, McDonald D, Filby A, Li W, De Jager PL, Rozenblatt-Rosen O, Lane AA, Haniffa M, Regev A, Hacohen N. 2017. Single-cell RNA-seq reveals new types of human blood dendritic cells, monocytes, and progenitors. Science 356:eaah4573. doi: 10.1126/science.aah4573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.See P, Dutertre C-AA, Chen J, Günther P, McGovern N, Irac SE, Gunawan M, Beyer M, Händler K, Duan K, Sumatoh HRB, Ruffin N, Jouve M, Gea-Mallorquí E, Hennekam RCM, Lim T, Yip CC, Wen M, Malleret B, Low I, Shadan NB, Fen CFS, Tay A, Lum J, Zolezzi F, Larbi A, Poidinger M, Chan JKY, Chen Q, Rénia L, Haniffa M, Benaroch P, Schlitzer A, Schultze JL, Newell EW, Ginhoux F. 2017. Mapping the human DC lineage through the integration of high-dimensional techniques. Science 356:eaag3009. doi: 10.1126/science.aag3009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmed Z, Kawamura T, Shimada S, Piguet V. 2015. The role of human dendritic cells in HIV-1 infection. J Investig Dermatol 135:1225–1233. doi: 10.1038/jid.2014.490. [DOI] [PubMed] [Google Scholar]
- 8.Piguet V, Steinman RM. 2007. The interaction of HIV with dendritic cells: outcomes and pathways. Trends Immunol 28:503–510. doi: 10.1016/j.it.2007.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu L, KewalRamani VN. 2006. Dendritic-cell interactions with HIV: infection and viral dissemination. Nat Rev Immunol 6:859–868. doi: 10.1038/nri1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Izquierdo-Useros N, Lorizate M, McLaren PJ, Telenti A, Krausslich HG, Martinez-Picado J. 2014. HIV-1 capture and transmission by dendritic cells: the role of viral glycolipids and the cellular receptor Siglec-1. PLoS Pathog 10:e1004146. doi: 10.1371/journal.ppat.1004146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Puryear WB, Akiyama H, Geer SD, Ramirez NP, Yu X, Reinhard BMM, Gummuluru S. 2013. Interferon-inducible mechanism of dendritic cell-mediated HIV-1 dissemination is dependent on Siglec-1/CD169. PLoS Pathog 9:e1003291. doi: 10.1371/journal.ppat.1003291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lahouassa H, Daddacha W, Hofmann H, Ayinde D, Logue EC, Dragin L, Bloch N, Maudet C, Bertrand M, Gramberg T, Pancino G, Priet S, Canard B, Laguette N, Benkirane M, Transy C, Landau NR, Kim B, Margottin-Goguet F. 2012. SAMHD1 restricts the replication of human immunodeficiency virus type 1 by depleting the intracellular pool of deoxynucleoside triphosphates. Nat Immunol 13:223–228. doi: 10.1038/ni.2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goujon C, Jarrosson-Wuilleme L, Bernaud J, Rigal D, Darlix JL, Cimarelli A. 2006. With a little help from a friend: increasing HIV transduction of monocyte-derived dendritic cells with virion-like particles of SIV(MAC). Gene Ther 13:991–994. doi: 10.1038/sj.gt.3302753. [DOI] [PubMed] [Google Scholar]
- 14.Laguette N, Sobhian B, Casartelli N, Ringeard M, Chable-Bessia C, Segeral E, Yatim A, Emiliani S, Schwartz O, Benkirane M. 2011. SAMHD1 is the dendritic- and myeloid-cell-specific HIV-1 restriction factor counteracted by Vpx. Nature 474:654–657. doi: 10.1038/nature10117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hrecka K, Hao C, Gierszewska M, Swanson SK, Kesik-Brodacka M, Srivastava S, Florens L, Washburn MP, Skowronski J. 2011. Vpx relieves inhibition of HIV-1 infection of macrophages mediated by the SAMHD1 protein. Nature 474:658–661. doi: 10.1038/nature10195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McIlroy D, Autran B, Cheynier R, Wain-Hobson S, Clauvel JP, Oksenhendler E, Debré P, Hosmalin A. 1995. Infection frequency of dendritic cells and CD4+ T lymphocytes in spleens of human immunodeficiency virus-positive patients. J Virol 69:4737–4745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Donaghy H, Gazzard B, Gotch F, Patterson S. 2003. Dysfunction and infection of freshly isolated blood myeloid and plasmacytoid dendritic cells in patients infected with HIV-1. Blood 101:4505–4511. doi: 10.1182/blood-2002-10-3189. [DOI] [PubMed] [Google Scholar]
- 18.Calantone N, Wu F, Klase Z, Deleage C, Perkins M, Matsuda K, Thompson EA, Ortiz AM, Vinton CL, Ourmanov I, Lore K, Douek DC, Estes JD, Hirsch VM, Brenchley JM. 2014. Tissue myeloid cells in SIV-infected primates acquire viral DNA through phagocytosis of infected T cells. Immunity 41:493–502. doi: 10.1016/j.immuni.2014.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shingai M, Welbourn S, Brenchley JM, Acharya P, Miyagi E, Plishka RJ, Buckler-White A, Kwong PD, Nishimura Y, Strebel K, Martin MA. 2015. The expression of functional Vpx during pathogenic SIVmac infections of rhesus macaques suppresses SAMHD1 in CD4+ memory T cells. PLoS Pathog 11:e1004928. doi: 10.1371/journal.ppat.1004928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chauveau L, Puigdomenech I, Ayinde D, Roesch F, Porrot F, Bruni D, Visseaux B, Descamps D, Schwartz O. 2015. HIV-2 infects resting CD4+ T cells but not monocyte-derived dendritic cells. Retrovirology 12:2. doi: 10.1186/s12977-014-0131-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smed-Sorensen A, Lore K, Vasudevan J, Louder MK, Andersson J, Mascola JR, Spetz AL, Koup RA. 2005. Differential susceptibility to human immunodeficiency virus type 1 infection of myeloid and plasmacytoid dendritic cells. J Virol 79:8861–8869. doi: 10.1128/JVI.79.14.8861-8869.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Granelli-Piperno A, Shimeliovich I, Pack M, Trumpfheller C, Steinman RM. 2006. HIV-1 selectively infects a subset of nonmaturing BDCA1-positive dendritic cells in human blood. J Immunol 176:991–998. doi: 10.4049/jimmunol.176.2.991. [DOI] [PubMed] [Google Scholar]
- 23.Duvall MG, Lore K, Blaak H, Ambrozak DA, Adams WC, Santos K, Geldmacher C, Mascola JR, McMichael AJ, Jaye A, Whittle HC, Rowland-Jones SL, Koup RA. 2007. Dendritic cells are less susceptible to human immunodeficiency virus type 2 (HIV-2) infection than to HIV-1 infection. J Virol 81:13486–13498. doi: 10.1128/JVI.00976-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lahaye X, Satoh T, Gentili M, Cerboni S, Conrad C, Hurbain I, El Marjou A, Lacabaratz C, Lelievre JD, Manel N. 2013. The capsids of HIV-1 and HIV-2 determine immune detection of the viral cDNA by the innate sensor cGAS in dendritic cells. Immunity 39:1132–1142. doi: 10.1016/j.immuni.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 25.Manel N, Hogstad B, Wang Y, Levy DE, Unutmaz D, Littman DR. 2010. A cryptic sensor for HIV-1 activates antiviral innate immunity in dendritic cells. Nature 467:214–217. doi: 10.1038/nature09337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Silvin A, Yu CI, Lahaye X, Imperatore F, Brault J-B, Cardinaud S, Becker C, Kwan W-H, Conrad C, Maurin M, Goudot C, Marques-Ladeira S, Wang Y, Pascual V, Anguiano E, Albrecht RA, Iannacone M, García-Sastre A, Goud B, Dalod M, Moris A, Merad M, Palucka AK, Manel N. 2017. Constitutive resistance to viral infection in human CD141+ dendritic cells. Sci Immunol 2:eaai8071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Herold N, Anders-Osswein M, Glass B, Eckhardt M, Muller B, Krausslich HG. 2014. HIV-1 entry in SupT1-R5, CEM-ss, and primary CD4+ T cells occurs at the plasma membrane and does not require endocytosis. J Virol 88:13956–13970. doi: 10.1128/JVI.01543-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marin M, Melikyan GB. 2015. Can HIV-1 entry sites be deduced by comparing bulk endocytosis to functional readouts for viral fusion? J Virol 89:2985. doi: 10.1128/JVI.03352-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sattentau QJ. 2010. Cell-to-cell spread of retroviruses. Viruses 2:1306–1321. doi: 10.3390/v2061306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Miyauchi K, Kim Y, Latinovic O, Morozov V, Melikyan GB. 2009. HIV enters cells via endocytosis and dynamin-dependent fusion with endosomes. Cell 137:433–444. doi: 10.1016/j.cell.2009.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.de la Vega M, Marin M, Kondo N, Miyauchi K, Kim Y, Epand RF, Epand RM, Melikyan GB. 2011. Inhibition of HIV-1 endocytosis allows lipid mixing at the plasma membrane, but not complete fusion. Retrovirology 8:99. doi: 10.1186/1742-4690-8-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee B, Sharron M, Montaner LJ, Weissman D, Doms RW. 1999. Quantification of CD4, CCR5, and CXCR4 levels on lymphocyte subsets, dendritic cells, and differentially conditioned monocyte-derived macrophages. Proc Natl Acad Sci U S A 96:5215–5220. doi: 10.1073/pnas.96.9.5215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patterson S, Gross J, English N, Stackpoole A, Bedford P, Knight SC. 1995. CD4 expression on dendritic cells and their infection by human immunodeficiency virus. J Gen Virol 76:1155–1163. doi: 10.1099/0022-1317-76-5-1155. [DOI] [PubMed] [Google Scholar]
- 34.Janas AM, Dong C, Wang J-HH, Wu L. 2008. Productive infection of human immunodeficiency virus type 1 in dendritic cells requires fusion-mediated viral entry. Virology 375:442–451. doi: 10.1016/j.virol.2008.01.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Melikyan GB, Markosyan RM, Hemmati H, Delmedico MK, Lambert DM, Cohen FS. 2000. Evidence that the transition of HIV-1 gp41 into a six-helix bundle, not the bundle configuration, induces membrane fusion. J Cell Biol 151:413–423. doi: 10.1083/jcb.151.2.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang J-HH, Wells C, Wu L. 2008. Macropinocytosis and cytoskeleton contribute to dendritic cell-mediated HIV-1 transmission to CD4+ T cells. Virology 381:143–154. doi: 10.1016/j.virol.2008.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ménager MMM, Littman DR. 2016. Actin dynamics regulates dendritic cell-mediated transfer of HIV-1 to T cells. Cell 164:695–709. doi: 10.1016/j.cell.2015.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moris A, Nobile C, Buseyne F, Porrot F, Abastado JP, Schwartz O. 2004. DC-SIGN promotes exogenous MHC-I-restricted HIV-1 antigen presentation. Blood 103:2648–2654. doi: 10.1182/blood-2003-07-2532. [DOI] [PubMed] [Google Scholar]
- 39.Luban J. 2012. Innate immune sensing of HIV-1 by dendritic cells. Cell Host Microbe 12:408–418. doi: 10.1016/j.chom.2012.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Veiga S, Henriques S, Santos NC, Castanho M. 2004. Putative role of membranes in the HIV fusion inhibitor enfuvirtide mode of action at the molecular level. Biochem J 377:107–110. doi: 10.1042/bj20031350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lazzarin A. 2005. Enfuvirtide: the first HIV fusion inhibitor. Expert Opin Pharmacother 6:453–464. doi: 10.1517/14656566.6.3.453. [DOI] [PubMed] [Google Scholar]
- 42.Cavrois M, De Noronha C, Greene WC. 2002. A sensitive and specific enzyme-based assay detecting HIV-1 virion fusion in primary T lymphocytes. Nat Biotechnol 20:1151–1154. doi: 10.1038/nbt745. [DOI] [PubMed] [Google Scholar]
- 43.Passaes CP, Bruel T, Decalf J, David A, Angin M, Monceaux V, Muller-Trutwin M, Noel N, Bourdic K, Lambotte O, Albert ML, Duffy D, Schwartz O, Saez-Cirion A, ANRS RHIVIERA Consortium. 2017. Ultrasensitive HIV-1 p24 assay detects single infected cells and differences in reservoir induction by latency reversal agents. J Virol 91:e02296-16. doi: 10.1128/JVI.02296-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Aggarwal A, Hitchen TL, Ootes L, McAllery S, Wong A, Nguyen K, McCluskey A, Robinson PJ, Turville SG. 2017. HIV infection is influenced by dynamin at 3 independent points in the viral life cycle. Traffic 18:392–410. doi: 10.1111/tra.12481. [DOI] [PubMed] [Google Scholar]
- 45.Pion M, Arrighi JF, Jiang J, Lundquist CA, Hartley O, Aiken C, Piguet V. 2007. Analysis of HIV-1-X4 fusion with immature dendritic cells identifies a specific restriction that is independent of CXCR4 levels. J Investig Dermatol 127:319–323. doi: 10.1038/sj.jid.5700518. [DOI] [PubMed] [Google Scholar]
- 46.Dong C, Janas AM, Wang JH, Olson WJ, Wu L. 2007. Characterization of human immunodeficiency virus type 1 replication in immature and mature dendritic cells reveals dissociable cis- and trans-infection. J Virol 81:11352–11362. doi: 10.1128/JVI.01081-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Joseph SB, Arrildt KT, Swanstrom AE, Schnell G, Lee B, Hoxie JA, Swanstrom R. 2014. Quantification of entry phenotypes of macrophage-tropic HIV-1 across a wide range of CD4 densities. J Virol 88:1858–1869. doi: 10.1128/JVI.02477-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rowell JF, Ruff AL, Guarnieri FG, Staveley-O'Carroll K, Lin X, Tang J, August JT, Siliciano RF. 1995. Lysosome-associated membrane protein-1-mediated targeting of the HIV-1 envelope protein to an endosomal/lysosomal compartment enhances its presentation to MHC class II-restricted T cells. J Immunol 155:1818–1828. [PubMed] [Google Scholar]
- 49.O'Brien M, Manches O, Wilen C, Gopal R, Huq R, Wu V, Sunseri N, Bhardwaj N. 2016. CD4 receptor is a key determinant of divergent HIV-1 sensing by plasmacytoid dendritic cells. PLoS Pathog 12:e1005553. doi: 10.1371/journal.ppat.1005553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Eskelinen E-LL. 2006. Roles of LAMP-1 and LAMP-2 in lysosome biogenesis and autophagy. Mol Aspects Med 27:495–502. doi: 10.1016/j.mam.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 51.Ewald SE, Barton GM. 2011. Nucleic acid sensing Toll-like receptors in autoimmunity. Curr Opin Immunol 23:3–9. doi: 10.1016/j.coi.2010.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gay NJ, Symmons MF, Gangloff M, Bryant CE. 2014. Assembly and localization of Toll-like receptor signalling complexes. Nat Rev Immunol 14:546–558. doi: 10.1038/nri3713. [DOI] [PubMed] [Google Scholar]
- 53.Gleeson PA. 2014. The role of endosomes in innate and adaptive immunity. Semin Cell Dev Biol 31:64–72. doi: 10.1016/j.semcdb.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 54.Donahue DA, Amraoui S, di Nunzio F, Kieffer C, Porrot F, Opp S, Diaz-Griffero F, Casartelli N, Schwartz O. 2016. SUN2 overexpression deforms nuclear shape and inhibits HIV. J Virol 90:4199–4214. doi: 10.1128/JVI.03202-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Maréchal V, Clavel F, Heard JM, Schwartz O. 1998. Cytosolic Gag p24 as an index of productive entry of human immunodeficiency virus type 1. J Virol 72:2208–2212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cavrois M, Neidleman J, Kreisberg JF, Fenard D, Callebaut C, Greene WC. 2006. Human immunodeficiency virus fusion to dendritic cells declines as cells mature. J Virol 80:1992–1999. doi: 10.1128/JVI.80.4.1992-1999.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yu HJ, Reuter MA, McDonald D. 2008. HIV traffics through a specialized, surface-accessible intracellular compartment during trans-infection of T cells by mature dendritic cells. PLoS Pathog 4:e1000134. doi: 10.1371/journal.ppat.1000134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Garcia E, Pion M, Pelchen-Matthews A, Collinson L, Arrighi J-FF, Blot G, Leuba F, Escola J-MM, Demaurex N, Marsh M, Piguet V. 2005. HIV-1 trafficking to the dendritic cell-T-cell infectious synapse uses a pathway of tetraspanin sorting to the immunological synapse. Traffic 6:488–501. doi: 10.1111/j.1600-0854.2005.00293.x. [DOI] [PubMed] [Google Scholar]
- 59.Izquierdo-Useros N, Naranjo-Gomez M, Archer J, Hatch SC, Erkizia I, Blanco J, Borras FE, Puertas MC, Connor JH, Fernandez-Figueras MT, Moore L, Clotet B, Gummuluru S, Martinez-Picado J. 2009. Capture and transfer of HIV-1 particles by mature dendritic cells converges with the exosome-dissemination pathway. Blood 113:2732–2741. doi: 10.1182/blood-2008-05-158642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gummuluru S, Ramirez GN, Akiyama H. 2014. CD169-dependent cell-associated HIV-1 transmission: a driver of virus dissemination. J Infect Dis 210(Suppl 3):S641–S647. doi: 10.1093/infdis/jiu442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nobile C, Moris A, Porrot F, Sol-Foulon N, Schwartz O. 2003. Inhibition of human immunodeficiency virus type 1 Env-mediated fusion by DC-SIGN. J Virol 77:5313–5323. doi: 10.1128/JVI.77.9.5313-5323.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Granelli-Piperno A, Moser B, Pope M, Chen D, Wei Y, Isdell F, O'Doherty U, Paxton W, Koup R, Mojsov S, Bhardwaj N, Clark-Lewis I, Baggiolini M, Steinman RM. 1996. Efficient interaction of HIV-1 with purified dendritic cells via multiple chemokine coreceptors. J Exp Med 184:2433–2438. doi: 10.1084/jem.184.6.2433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rubbert A, Combadiere C, Ostrowski M, Arthos J, Dybul M, Machado E, Cohn MA, Hoxie JA, Murphy PM, Fauci AS, Weissman D. 1998. Dendritic cells express multiple chemokine receptors used as coreceptors for HIV entry. J Immunol 160:3933–3941. [PubMed] [Google Scholar]
- 64.Nobile C, Petit C, Moris A, Skrabal K, Abastado JP, Mammano F, Schwartz O. 2005. Covert human immunodeficiency virus replication in dendritic cells and in DC-SIGN-expressing cells promotes long-term transmission to lymphocytes. J Virol 79:5386–5399. doi: 10.1128/JVI.79.9.5386-5399.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Turville SG, Santos JJ, Frank I, Cameron PU, Wilkinson J, Miranda-Saksena M, Dable J, Stossel H, Romani N, Piatak M Jr, Lifson JD, Pope M, Cunningham AL. 2004. Immunodeficiency virus uptake, turnover, and 2-phase transfer in human dendritic cells. Blood 103:2170–2179. doi: 10.1182/blood-2003-09-3129. [DOI] [PubMed] [Google Scholar]
- 66.Moris A, Pajot A, Blanchet F, Guivel-Benhassine F, Salcedo M, Schwartz O. 2006. Dendritic cells and HIV-specific CD4+ T cells: HIV antigen presentation, T cell activation, viral transfer. Blood 108:1643–1651. doi: 10.1182/blood-2006-02-006361. [DOI] [PubMed] [Google Scholar]
- 67.Iwasaki A. 2012. Innate immune recognition of HIV-1. Immunity 37:389–398. doi: 10.1016/j.immuni.2012.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bruni D, Chazal M, Sinigaglia L, Chauveau L, Schwartz O, Despres P, Jouvenet N. 2015. Viral entry route determines how human plasmacytoid dendritic cells produce type I interferons. Sci Signal 8:ra25. doi: 10.1126/scisignal.aaa1552. [DOI] [PubMed] [Google Scholar]
- 69.Beauparlant D, Rusert P, Magnus C, Kadelka C, Weber J, Uhr T, Zagordi O, Oberle C, Duenas-Decamp MJ, Clapham PR, Metzner KJ, Günthard HF, Trkola A. 2017. Delineating CD4 dependency of HIV-1: adaptation to infect low level CD4 expressing target cells widens cellular tropism but severely impacts on envelope functionality. PLoS Pathog 13:e1006255. doi: 10.1371/journal.ppat.1006255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Massanella M, Puigdomènech I, Cabrera C, Fernandez-Figueras MT, Aucher A, Gaibelet G, Hudrisier D, García E, Bofill M, Clotet B, Blanco J. 2009. Antigp41 antibodies fail to block early events of virological synapses but inhibit HIV spread between T cells. AIDS 23:183–188. doi: 10.1097/QAD.0b013e32831ef1a3. [DOI] [PubMed] [Google Scholar]
- 71.Reuter S, Kaumanns P, Buschhorn SB, Dittmar MT. 2005. Role of HIV-2 envelope in Lv2-mediated restriction. Virology 332:347–358. doi: 10.1016/j.virol.2004.11.025. [DOI] [PubMed] [Google Scholar]
- 72.Sol-Foulon N, Esnault C, Percherancier Y, Porrot F, Metais-Cunha P, Bachelerie F, Schwartz O. 2004. The effects of HIV-1 Nef on CD4 surface expression and viral infectivity in lymphoid cells are independent of rafts. J Biol Chem 279:31398–31408. doi: 10.1074/jbc.M401621200. [DOI] [PubMed] [Google Scholar]