Abstract
Exosomes are defined as submicron (30–150 nm), lipid bilayer-enclosed extracellular vesicles (EVs), specifically generated by the late endosomal compartment through fusion of multivesicular bodies with the plasma membrane. Produced by almost all cells, exosomes were originally considered to represent just a mechanism for jettisoning unwanted cellular moieties. Although this may be a major function in most cells, evolution has recruited the endosomal membrane-sorting pathway to duties beyond mere garbage disposal, one of the most notable examples being its cooption by retroviruses for the generation of Trojan virions. It is, therefore, tempting to speculate that certain cell types have evolved an exosome subclass active in intracellular communication. We term this EV subclass “signalosomes” and define them as exosomes that are produced by the “signaling” cells upon specific physiological or environmental cues and harbor cargo capable of modulating the programming of recipient cells. Our recent studies have established that signalosomes released by mesenchymal stem/stromal cells (MSCs) represent the main vector of MSC immunomodulation and therapeutic action in animal models of lung disease. The efficacy of MSC-exosome treatments in a number of preclinical models of cardiovascular and pulmonary disease supports the promise of application of exosome-based therapeutics across a wide range of pathologies within the near future. However, the full realization of exosome therapeutic potential has been hampered by the absence of standardization in EV isolation, and procedures for purification of signalosomes from the main exosome population. This is mainly due to immature methodologies for exosome isolation and characterization and our incomplete understanding of the specific characteristics and molecular composition of signalosomes. In addition, difficulties in defining metrics for potency of exosome preparations and the challenges of industrial scale-up and good manufacturing practice compliance have complicated smooth and timely transition to clinical development. In this manuscript, we focus on cell culture conditions, exosome harvesting, dosage, and exosome potency, providing some empirical guidance and perspectives on the challenges in bringing exosome-based therapies to clinic.
Keywords: exosomes, extracellular vesicles, exosome-based therapeutics, mesenchymal stem cells, preclinical
Introduction
The intracellular transfer of diverse moieties via extracellular vesicles (EVs) has been proposed to be a widespread process. Cells release diverse EVs that include exosomes, microvesicles (MVs) and apoptotic bodies (1, 2). The classification of such EV subtypes is mainly based on their biogenesis and resultant biophysical properties, such as size, density, and predominant protein markers. Originally, the class of EVs generated through the endosomal pathway (exosomes) was assumed to represent a mere mechanism for the cell to jettison unwanted moieties (3, 4). We now understand that exosome biogenesis is a process governed by the endosomal-sorting complex machinery and involves the formation of intraluminal vesicles within multivesicular bodies (MVBs). Mature MVBs fuse with the plasma membrane and subsequently secrete the enclosed exosomes into the extracellular environment. During their biogenesis, exosomes associate with an array of bioactive cargo from their parental cell. Such cargo has been reported to include genetic information in the form of small noncoding RNAs, free fatty acids, surface receptors, and proteins (Figure 1) (5, 6). It is considered that the biophysical properties of EVs, including their cargo, reflect the stimulus triggering their formation (7), implying specific packaging of “message” prior to export from the parent cell. In turn, the secretion of these biologically loaded signaling vectors to the extracellular environment represents an important method of cell-to-cell communication, dubbed the “new endocrinology”.
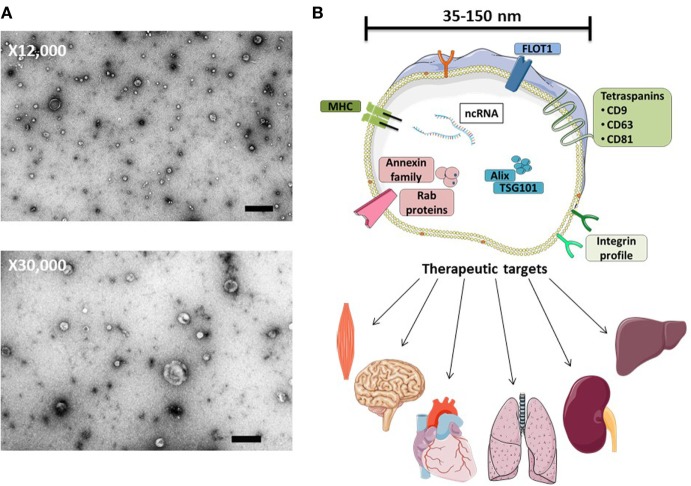
Figure 1.
MSC-exosome morphology and composition. (A) Transmission electron microscopy (TEM) images of human bone marrow-derived MSC-exosomes (low magnification, 12,000×, scale bar = 500 nm, and high magnification, 30,000×, scale bar = 100 nm) representative TEM images adapted from Ref. (8). (B) MSC-exosomes are surrounded by a phospholipid bilayer and may contain proteins, such as annexins (these are important for transport); tetraspanins such as CD9, CD81, and CD63; and other proteins, such as Alix and TSG101, that are involved in exosomal biogenesis from endosomes. MSC-exosome therapy has shown beneficial effects in numerous preclinical models, demonstrating histological and functional benefits in multiple organs. Abbreviations: FLOT1, flotillin-1; MHC, major histocompatibility complex; TSG101, tumor susceptibility gene 101.
Exosomes have been shown to play important roles in a broad range of pathological conditions, such as cancer (9), liver and kidney disease (10), neurodegenerative disorders (11), and numerous cardiopulmonary disorders (12, 13). More recently, in addition to their prognostic and diagnostic value, exosomes have also been reported to represent novel therapeutic reagents across multiple disciplines.
Exosome-Based Therapeutics
The therapeutic capacity of exosomes generated by mesenchymal stem/stromal cells (MSCs) that have been derived from different organs, such as bone marrow, umbilical cord, adipose tissue, or placenta has been tested in various disease models. In the cases where cells and their respective exosomes were studied in parallel, exosome treatment has demonstrated a similar or even superior therapeutic capacity to MSC treatment (14). MSC-exosomes have provided beneficial effects in numerous disease models promoting functional recovery and neurovascular plasticity following traumatic brain injury (15), reducing myocardial infarction size (16, 17), ameliorating hypoxia-induced pulmonary hypertension (18), aiding repair of kidney injury (19, 20), and orchestrating neurological protection by the transfer of microRNA (21, 22). MSC-exosome-based approaches for the treatment of different disease models are highlighted in Table 1.
Table 1.
Summary of MSC-exosome-based approaches for the treatment of different disease models.
| Disease model | MSC-product “nomenclature” | Isolation method | Dose assessment | Dose | Reference |
|---|---|---|---|---|---|
| Respiratory | |||||
| Bronchopulmonary dysplasia | Exosomes | Density Cushion | Cell equivalent | 0.5 × 106 | Willis et al. (8) |
| Pulmonary hypertension | Exosomes | SEC | Protein | 0.1–10 μg | Lee et al. (18) |
| Pulmonary hypertension | Exosomes | UC (100K × g) | Protein | 25 μg | Aliotta et al. (23) |
| Acute lung injury | Microvesicles (MVs) | UC (100K × g) | Cell equivalent | 1.5 × 106 | Zhu et al. (24) |
| Silicosis | Exosomes | Sucrose gradient | Protein | 40 μg | Phinney et al. (25) |
| Pneumonia | MVs | UC (100K × g) | Cell equivalent | 9 × 106 | Monsel et al. (26) |
| Cardiovascular | |||||
| Myocardial infarction | Exosomes | ExoQuick | Cell equivalent | 4 × 106 | Yu et al. (27) |
| Myocardial infarction | Extracellular vesicles (EVs) | UC (100K × g) | Protein | 80 μg | Bian et al. (28) |
| Myocardial infarction | Exosomes | ExoQuick | Protein | 80 μg | Teng et al. (29) |
| Ischemia/reperfusion | Exosomes | HPLC | Protein | 0.4 μg | Lai et al. (16) |
| Ischemia/reperfusion | Exosomes | HPLC | Protein | 0.4–0.8 μg | Arslan et al. (17) |
| Neurological | |||||
| Traumatic brain injury | EVs | Anion exchange chromatograph | Protein | 30 μg | Kim et al. (30) |
| Laser-induced retinal injury | Exosomes | UC (110K × g) | Protein | 10 μg | Yu et al. (31) |
| Optical nerve crush | Exosomes | UC (100K × g) | ExoELISA | 3 × 109 | Mead and Tomarev (32) |
| Stroke | EVs | UC (110K × g) | Cell equivalent | 2 × 106 | Doeppner et al. (33) |
| Stroke | Exosomes | UC (100K × g) | Protein | 100 μg | Xin et al. (34) |
| Musculoskeletal | |||||
| Cardiotoxin injury | EVs | UC (100K × g) | Protein | 5 μg | Lo Sicco et al. (35) |
| Hepatic | |||||
| Drug-induced liver injury | Exosomes | UC (100K × g) | Protein | 0.4 μg | Tan et al. (36) |
| Liver fibrosis | Exosomes | UC (100K × g) | Protein | 250 μg | Li et al. (37) |
| Gastrointestinal | |||||
| Colitis | EVs | UC (100K × g) | Protein | 50–200 μg | Yang et al. (38); Fang et al. (39) |
| Dermatological | |||||
| Wound healing | Exosomes | UC (100K × g) | Protein | 160 μg | Zhang et al. (40) |
| Wound healing | Exosomes | UC (120K × g) | Protein | 100 μg | Fang et al. (39) |
| Renal | |||||
| Ischemia/reperfusion | MVs | UC (100K × g) | Protein | 100 μg | Zou et al. (41) |
| Acute kidney injury | MVs | UC (100K × g) | Protein | 100 μg | Bruno et al. (42) |
Ultracentrifugation (UC): 100,000–120,000 × g (100K–120K × g). Size-exclusion chromatography (SEC). ExoQuick and ExoELISA refer to a commercially available exosome isolation kit and CD63 capture (exosome) ELISA, respectively (Systems Biosciences, CA, USA).
While the functional roles of exosomes have been extensively reported [reviewed in Ref. (43–46)], few reviews have addressed the challenges underlying the transition of exosome-based therapies from animal models to clinical development. Furthermore, the full realization of their therapeutic potential has been hampered by a lack of standardization in exosome isolation and characterization. Herein, we will focus on the therapeutic application of MSC-exosomes and outline topics relevant to the facilitation of their development as a pharmaceutical preparation, focusing on exosome harvesting, dosing and potency, and providing guidance on the current challenges in bringing exosome-based therapies to clinic.
Mesenchymal Stem/Stromal Cell Origin: Where are the Exosomes Coming From?
A comprehensive characterization of the tissue/cellular source of exosomes is imperative for exosome-based therapeutics. Detailed methods for obtaining human MSCs from several tissues, including bone marrow (BMSCs), Wharton’s jelly (WJMSCs), umbilical cord blood, and adipose tissue are well reported (47, 48). By definition, MSCs must adhere to plastic, demonstrate a baseline differentiation potential to osteocytes, chondrocytes, and adipocytes in vitro, and express the presence of widely accepted surface markers (Table 2) (49). However, donor-to-donor variability remains a prominent challenge. Studies have found that BMSCs obtained from older donors have slower proliferation and reduced differentiation potential in vitro. Furthermore, discrepancies in the differentiation capacity and transcriptome profiles are reported to be tissue and species dependent (50–52). To what extent do these uncertainties affect the therapeutic capacity of MSCs and their resultant exosomes remains unclear. Thus, in addition to validated MSC isolation procedures, investigators should adhere to carefully selected donor eligibility criteria in accordance with the appropriate ethical and regulatory approval, employing strict control measures to prevent risk of relevant communicable disease agents or diseases (RCDADs), such as human immunodeficiency virus (HIV), hepatitis C virus, and cytomegalovirus. Moreover, donor screening should include a comprehensive medical record review, physical assessment, and medical history interview, with records documented in compliance with appropriate regulatory frame. The International Society of Extracellular Vesicles (ISEV), the Food and drug Administration (FDA), the International Council for Harmonization (ICH) of Technical Requirements for Pharmaceuticals for Human Use, and the European Medicines Agency (EMA) provide extensive guidance for the development and generation of novel biological medicines with regard to donor/patient care, product safety, and quality (53–56). The demonstration that exosomes generated by MSCs isolated from WJMSCs are as effective as BMSC-exosomes in treating rodent disease models (8) may facilitate standardization and consistency of MSC lines for exosome harvesting. Moreover, the umbilical cord may possess several advantages over bone marrow. First, the umbilical cord represents a more readily available source than bone marrow. Second, it is often viewed as discarded medical waste that does not require any invasive procedures or cadaver procurement.
Table 2.
Minimal criteria for defining MSCs, as put forth by The International Society for Cellular Therapy.
| Characterization of mesenchymal stem/stromal cells (MSCs) |
|---|
|
Human leukocyte antigen–antigen D related (HLA-DR). Adapted from Dominici et al. (49).
“Physioxia” Considerations in Establishing MSC Culture Conditions for Exosome Production
Previous studies have reported that the protein and RNA profile of exosomes reflect the cell culture conditions and microenvironmental stimuli that triggered their release. With this in mind, it begs to question can “stimulating” and/or preconditioning cells be used as a means to generate a more homogenous or efficacious exosome population? Interestingly, in an experimental model of hyperoxia-induced bronchopulmonary dysplasia (BPD), Waszak and coworkers found that the conditioned media (CM) derived from hyperoxia-preconditioned rat BMSCs (95% O2, for 24 h) provided greater protection in vivo compared to CM collected from cells grown under control conditions (57). Clearly, in the absence of further characterization, one can only speculate where the observed augmentation of activity resides. Other studies have found that MSCs cultured in hypoxia conditions (<5% O2) exhibited an altered protein expression pattern compared to MSCs cultured in the so-called “normoxia” (58). Furthermore, in a murine hind limb ischemia model, they showed that intra-arterial injection of MSCs cultured in both “normoxic” or hypoxic conditions enhanced revascularization compared with saline controls; however, the functional recovery of mice that received hypoxia preconditioned MSCs was faster (59). These reports suggest that preconditioning MSCs in different oxygen environments may improve their tissue regenerative potential.
Indeed, “hypoxia” (1% O2) has been shown to increase exosome production in numerous cell types in vitro. Previous studies have shown that the hypoxia-induced elevation in exosome secretion is chiefly governed by hypoxia-inducible factor-1 alpha (HIF-1α) and is independent of apoptosis (60). Often, laboratory cell culture conditions are at atmospheric oxygen levels (21% O2, corresponding to a PO2 of ~159 mmHg); following adjustment to 5% CO2, this equates to ~19.95% O2 (~150 mmHg). Although, it is challenging to accurately measure tissue oxygen concentrations in vivo, it is well recognized that most of the human body tissue is normally exposed to much lower O2 levels. This can range from 160 to 100 mmHg in the alveoli, >35 mmHg in the brain, and ~25 mmHg in skeletal muscle (61–63). Notably, in the bone marrow, arguably the most common origin of MSCs, the PO2 is reported to be ~40 mmHg, while the umbilical cord vasculature PO2 is reported to be between 10 and 30 mmHg (63). Organ oxygen levels have been extensively reviewed (63). However, it is important to remember that the different techniques used to measure oxygen concentration in vivo are subject to their own advantages and limitations.
In vivo, the oxygen concentration of an organ is an indication of its physiological state and reflects the balance between oxygen delivery and its metabolic consumption. Consequently, in a physiological condition, organs are subject their own unique “physioxia” status. On balance, the routine laboratory cell culture conditions expose MSCs to oxygen levels higher than those in their physiologic niches, and this departure from “physioxia” may precipitate a “perceived hyperoxia” response. Thus, it is important to recognize this factor when interpreting results of experiments performed in atmospheric “normoxia,” and also to realize that the impact of this factor may vary, depending on the particular study and the metrics assessed.
In turn, several questions remain unanswered. The optimal oxygen concentration for in vitro MSC culture and the effect that it may have on subsequent exosome production remains undefined at this point. Existing reports indicate that optimization is likely to be both MSC origin and disease model specific. Thus, additional studies assessing the effect of oxygen levels on MSCs and their resultant exosomes are much needed.
Exosome Heterogeneity
Cells generate three major EV classes: apoptotic bodies, MVs, and exosomes. Arguably, it is often assumed each subtype represents a homogenous vesicle population that can be distinguished based on biophysical properties such as size or density. However, it has become obvious that even within such subtypes, there is heterogeneity (2, 64). Although, the field lacks tools to distinguish vesicles from different routes of biogenesis, recent evidence has demonstrated that MSCs release distinct EV subpopulations that differ in biophysical, proteomic, and RNA repertoires. Specifically, Kowal and coworkers found that large-, medium-, and small-sized EVs can be isolated by sequential low-, intermediate-, and high-speed centrifugation, respectively. Among the small-EVs (exosomes), four subcategories were defined by their degree of enrichment in CD63, CD9, and/or CD81 tetraspanins (64). In accordance, Lai et al. found that MSCs secrete many distinct subtypes of vesicles, which differ in RNA and protein composition (65). It is relevant to note that the study involved an immortalized, iPS-derived MSC cell line that will likely secrete a more restricted range of exosome subtypes than those generated by primary cells.
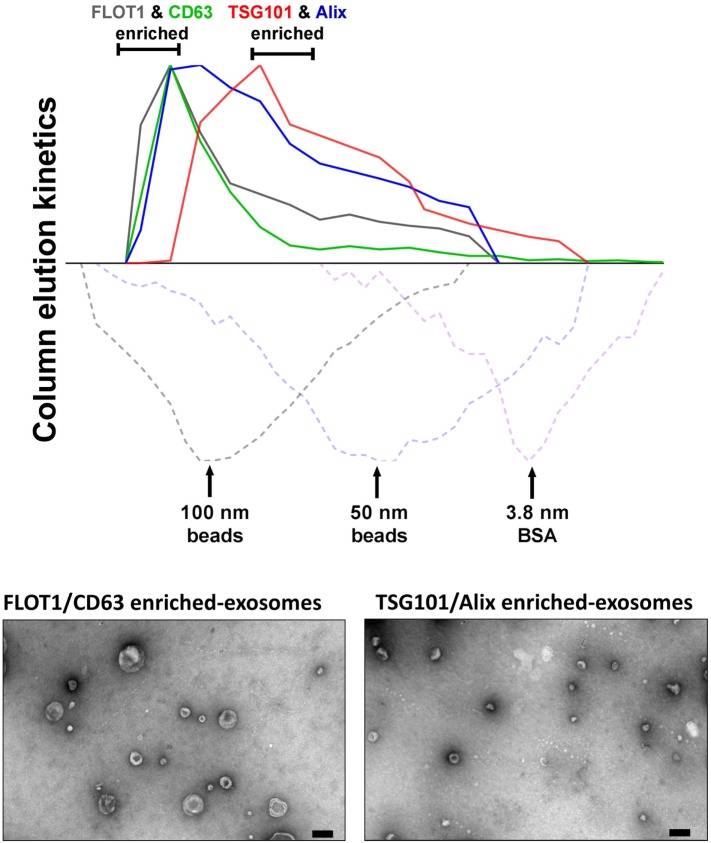
In our hands, ongoing studies aim to address the relationships between MSC-exosome subtypes and therapeutic efficacy and to explore the hypothesis that a discrete subtype is responsible for the therapeutic activity in our established experimental models of BPD, a chronic lung disorder of infants (8). Here, we isolated exosomes from either human BMSCs or WJMSCs by differential centrifugation, followed by tangential flow filtration and iodixanol density floatation before separating exosome subtypes by size-exclusion chromatography (SEC) (described in Figure 2). This approach separates MSC-exosome subtypes based on their size, and in accordance with previous reports, we demonstrate a shift in protein markers associated with different exosome subtypes. Specifically, we found that CD63 and flotillin-1 (FLOT1) is associated with “large”-exosomes (>80 nm), while Alix and TSG101 is enriched in “small”-exosomes (<80 nm). Few studies assess the ratio of such markers; however, further investigation is warranted as it may provide a tool for distinguishing exosome subtypes. Ongoing in vivo studies are testing whether the different MSC-exosome subtypes exhibit differential therapeutic efficacy in a number of animal models currently utilized by our group and collaborators.
Figure 2.
Isolation of MSC-exosomes subtypes by size-exclusion chromatography (SEC). Briefly, exosomes were isolated directly from cell culture supernatants following a 36 h harvest period in serum-free-media. Cell culture media were subjected to differential centrifugation, 300 × g for 10 min, followed by 3,000 × g for 10 min, and 13,000 × g for 30 min to remove any cells, cell debris, and large apoptotic bodies in suspension, respectively. Conditioned media (CM) was concentrated 50-fold by tangential flow filtration (TFF) and the exosomes were purified using OptiPrep™ (iodixanol) cushion density flotation (3.5 h at 100,000 × g, 4°C), as previously described (8). Heterogeneous exosomes were further purified by size using size-exclusion chromatography (SEC). Here, sepharose CL-2B (80 mL) was washed with 1 × SSPE buffer [containing 1 mM EDTA and 149 mM NaCl in 0.20 mM phosphate buffer (pH 7.4)]. The column was packed with washed sepharose CL-2B to create a column with an internal diameter of 1.6 cm and height of 40 cm. Exosomes (1 ml, corresponding to 60 × 106 MSC equivalents) were added to column with a flow rate of 1 ml/min. Fractions (1 ml) were collected and assessed by dot plots and electron microscopy. The elution kinetics of 100 nm, 50 nm, and bovine serum albumin (BSA) were used to estimate exosome elution kinetics. TSG101, Alix, CD63, and FLOT1 levels were assessed by dot plots and are reported as relative intensity. Here, we identify two distinct MSC-exosome subtypes. The larger exosomes (>80 nm) have a greater flotillin-1 (FLOT1) and CD63 enrichment, while smaller exosomes (<80 nm) have a greater TSG101 and Alix ratio.
Regulatory frameworks often require a mechanism-of-action that details the identity, quantification, and characterization of such bioactive substances responsible for the therapeutic effect(s). Moreover, disclosure of non-active components (“excipients”) in drug preparations should be acknowledged (56, 66). Knowing exosome subtypes harbor different protein and genetic cargo, it is fair to speculate that they likely mediate different effects on targets cells. Thus, improved separation techniques that distinguish between “non-active” and therapeutic exosome subtypes may help focus the search for the bioactive substance(s) responsible for such beneficial effects. The “one size fits all” hypothesis may not work for exosome-based therapeutics. Although a specific exosome subset may induce beneficial therapeutic effects in a specific disease model, it is important to recognize that a different exosome subpopulation may afford the beneficial effects in a different disease model.
Emerging Themes in Exosome Isolation
Isolation methods impact exosome integrity, in vivo biodistribution and metabolic fate (56). Exosome isolation techniques from various biological fluids and cell culture medium have been extensively reviewed (67–69). It is well established that widely applied exosome isolation techniques, such as differential ultracentrifugation (UC), promote vesicle aggregation and often co-isolate soluble factors and protein (70). Thus, a consensus in the field has shifted toward more “gentle” isolation techniques to ultimately reduce contaminants (non-EV material), maintain integrity, and isolate “bioactive” vesicles from heterogeneous EV populations. To date, popular avenues of investigation include gradient density isolation and SEC, with the latter being more suited to enclosed tissues culture systems. Variations of such approaches have been shown to effectively separate exosomes from proteins and soluble factors in different biological fluids (71, 72). However, layered density-based procedures may achieve enrichment rather than true exosome isolation, where the influence of UC parameters coupled with high-sucrose concentrations may change the osmotic environment (69). Furthermore, UC methods are impracticable for large-scale bioprocessing.
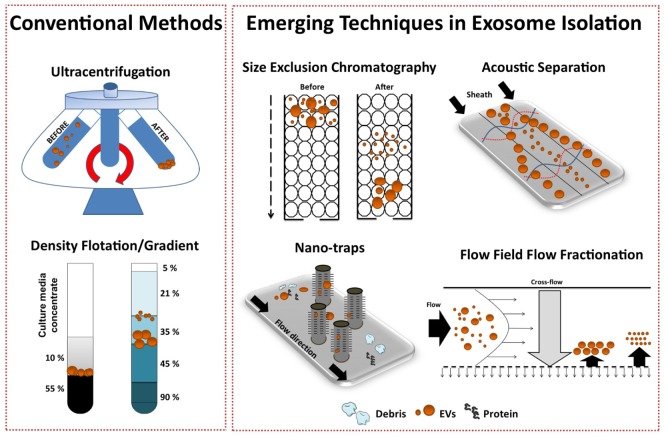
Several emerging technology platforms have shown promise in isolating exosomes from various sample matrices, with each method exploiting a particular biophysical trait of exosomes such as their size, density, shape, or surface receptors (Figure 3) (72). The final goal is an isolation method that is label free, distinguishes between exosome subtypes and interfering components, and can facilitate a large-scale production of exosomes.
Figure 3.
Conventional and emerging exosome isolation techniques. Ultracentrifugation (UC) is the most common exosome isolation method. Here, sedimentation of solutes including vesicles is governed by their size/density. Variations of UC such as layered or cushion based-density gradient UC are also widely employed. New methods are required to facilitate large-scale, high-yield production of exosomes for clinical applications. Several emerging technology platforms have shown promise in isolating exosomes from various sample matrices. Techniques, such as size-exclusion chromatography, ciliated micropillars nano-traps, acoustic wave separation technology, and flow field-flow fraction (F4), exploit unique biophysical traits of exosomes.
Recently, Lee and colleagues employed a label-free acoustic nano-filter system to isolate exosomes based on their size (73). Specifically, using ultrasound standing waves exert differential acoustic force, they isolated exosomes from both cell culture media and stored red blood cell products. They effectively separated exosomes (149 nm) and MVs (410 nm). Although, its application for high-throughput exosome preparations is yet to be established, previous studies have used label-free acoustic wave systems to isolate circulating tumor cells (74).
Exosomes can also be separated by size with 10 nm accuracy using variations of flow field-flow fractionation (F4) (75). Asymmetrical F4 (AF4) is a one-phase chromatography method that uses parabolic-flow to drive exosomes across a flow channel. A crossflow intercepts the parabolic-flow perpendicular to the channel and distributes particulate components against the flow chamber wall. Subsequently, exosomes are separated based on differences in diffusivity. Smaller particles diffuse further from the accumulation wall and are eluted earlier than larger ones. Successful attempts have been made using AF4 to isolate exosomes from human neural stem cell culture (76) and melanoma cell lines (77). AF4 approaches provide promise for “label-free” isolation of large-scale exosome production.
To effectively utilize the size difference between exosomes, other EV subtypes and cellular debris, Wang and colleagues fabricated a porous silicon nanowire-on-micropillar “nano-trap” made from ciliated micropillars (78). This fabricated microfluidic device preferentially traps exosomes with a diameter of 40–100 nm, while filtering out proteins, larger EVs, and cellular debris. Moreover, trapped exosomes can be recovered by dissolving the porous silicon nanowires in PBS buffer. However, in this proof-of-concept study, the authors noted poor vesicle retention (~60%) and only assessed small sample volume (30 μl), thus scalability is yet to be demonstrated.
Overall, to support the development of exosome-based therapeutics, research efforts should focus on the development of “label-free” exosome isolation techniques that can support high-throughput systems/scale-up requirements and are capable of distinguishing exosome subtypes. Although a number of highly sophisticated technologies for EV isolation have emerged recently, their application is mainly in the biomarker field, as tools for exosome-based diagnostics. Although such emerging technologies hold great promise, the large-scale preparation of isolated exosome subtypes to be used as the basis of exosome-based pharmaceutical products will probably depend, at least in the near future, on modifications of classic industrial processes such as SEC.
Dose Evaluation
Currently, investigators use several different methods to quantify exosome dosage, making inter-study comparison troublesome. Common quantitative practices include reporting cell equivalents, protein concentration, and/or specialized quantitative analytical measurements by instruments, such as tunable resistive pulse sensing (TRPS) and nanoparticle tracking analysis (NTA), with each method harboring its own advantages and limitations [for recent reviews (79–82)]. The need to standardize exosome dosing is imperative. Of interest, methods such as TRPS are currently used to verify particle size and characterization for liposome-encapsulated forms of doxorubicin and are accepted within the definition of bioequivalence as set forth by the FDA and EMA. Although enumeration of analytical criteria is beyond the scope of this review, we acknowledge that the field is limited by current technology and lacks the ability to accurately assess exosomes at a single vesicle level. Thus, to aid inter-study comparison, we recommend that in addition to providing extensive detail of standardized cell culture conditions and pre-analytical protocols, investigators should measure exosome concentration using multiple quantification tools, where possible. A summary of the advantages and limitations of common methods used to determine exosome dose are highlighted in Table 3. Establishing an exosome potency assay is a novel approach which holds great promise in standardizing exosome dosing.
Table 3.
A summary of the advantages and limitations of common methods used to determine exosome dose.
| Exosome dosing method | Information acquired | Advantages | Limitations | ||
|---|---|---|---|---|---|
| Protein | Total protein amount | Fast | May not reflect bioactive ingredient. May measure non-exosomal-associated protein. Does not reflect particle concentration/size/distribution | ||
| Low cost | |||||
| Nanoparticle tracking analysis (NTA) | Particle concentration, size, and distribution (range 10 nm–2 μm) | Fluorescent-NTA available | Difficulties in determining vesicle aggregates and size heterogeneity in biological samples | ||
| Provides absolute EV concentration, size and distribution | |||||
| Tunable resistive pulse sensing (TRPS) | Particle concentration, size and distribution (size range <40 nm–10 μm) | Provides absolute EV concentration, size and distribution. Can also measure particle surface charge | Different pore sizes are needed to assess biological samples that contain both exosomes (for example, <150 nm) and larger EVs (>150 nm) | ||
| Can detect non-exosome material within size range | |||||
| ELISA | Specific concentration of EV marker (for example, CD9 or CD63) | Specific to “exosome” protein | May not reflect bioactive exosome population. Time consuming. Provides non-specific information about exosome size/distribution | ||
| Dynamic light scattering (DLS) | Particle concentration and size (range <1 nm–10 μm) | Fast | Difficulties in measuring heterogeneous samples | ||
| Small volume required | |||||
| Flow cytometry | Particles concentration and size (size range ~>150 nm) | Non-specialized (typical) laboratory equipment | Detection limit (~<150 nm) (cytometer dependent) | ||
| Fluorescently labeled EVs | |||||
| Cell equivalents | Cell number | Low cost | Requires standardized tissue culture procedures. Does not reflect particle concentration/size/distribution | ||
| Fast | |||||
| Emerging tools for estimating exosome dose | Description | ||||
| “Fingerprinting assays” | Quantifies surrogate markers (for example levels/ratios of exosome markers such as CD63, CD9, and CD81) as an indication of potency and/or dose | ||||
| Exosome potency assays | Quantifies the ability of an exosome preparation to elicit the desired biologic/therapeutic action or surrogate activity in vitro and/or in vivo | ||||
NTA and DLS size ranges were obtained from http://malvern.com. TRPS detection range was obtained from http://izon.com.
Developing an Exosome Potency Assay
The definition of the bioactive substance(s) will remain a crucial question in the preclinical development of exosome-based therapeutics. With an orchestra of bioactive cargo and diverse physiological effects (Figure 1B), identification of “one” bioactive substance or a singular mechanism-of-action appears improbable. By FDA standards, potency is defined as the products specific ability or capacity to affect a given result (66). With no “gold-standard” technique for their quantification, assessment of exosome potency would be a valuable tool in overcoming the inconsistencies in preparations and batch-to-batch variation. For example, exosomes obtained from two separate donors may be normalized via a given quantitative method; however, the “bioactive” load may differ, subsequently the potency and degree of efficacy will not be the same. Thus, investigators should consider employing a unique exosome potency unit (EPU) to standardize practices and minimize variation between different samples. Presently, attempts to define an exosome potency metric utilized the immunomodulatory properties of MSC-exosomes. For example, Jiao et al. described an in vitro potency assay for MSC-exosomes based on the release of IL-10 from mononuclear cells following incubation with exosome preparations, and other studies have shown that T-cell proliferation assays may be modified to provide the basis for assays on exosome immunomodulatory potency (29, 83). Growing evidence also suggests that MSC-exosomes can modulate macrophage phenotypes (8, 35). Macrophages play a pivotal part in regulating immune responses. They assume both phagocytic “defensive” roles and exhibit regulatory “anti-inflammatory” actions, facilitating both the initiation and the resolution of inflammation (84). With this consideration in mind, our ongoing studies are exploring an in vitro macrophage polarization assay as a means of assessing MSC-exosome potency. Briefly, the potency assay involves adding MSC-exosomes to murine bone marrow-derived macrophages (BMDMs) that are polarized to the classically activated (proinflammatory) M1-phenotype. The functional endpoint is the capacity of MSC-exosomes to suppress the mRNA induction of TNFα. The half maximal effective concentration (EC50 value, 50% inhibition in TNFα mRNA levels, relative to M1 control) is transformed to an arbitrary EPU (described in Figure 4) (8). In turn, an EPU could potentially be applied to standardize dosing between different exosome preparations. In all cases, potency assays need to be disease specific, fit-for-purpose, and employ relevant functional end-points.
Figure 4.
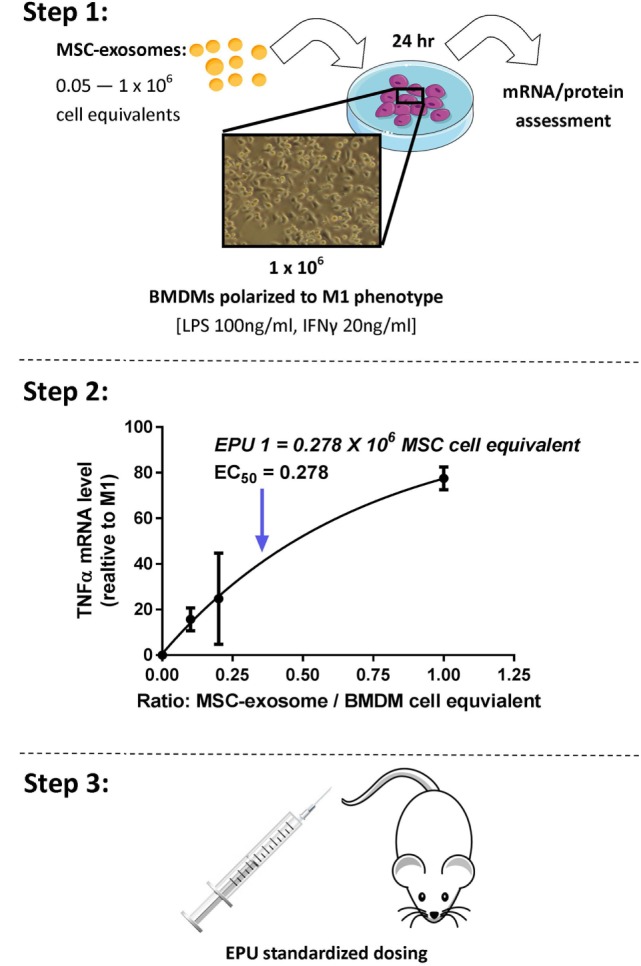
Stepwise approach to developing an MSC-exosome potency assay. Considering limitations in current exosome quantification techniques, assessment of exosome potency would be a valuable tool to standardize exosome dosing. Step 1: primary murine bone marrow-derived macrophages (BMDMs) were obtained by flushing the femur and tibia of 6- to 8-week-old FVB mice. M1 polarization was initiated by lipopolysaccharide (LPS) 100 ng/ml and interferon-γ (IFNγ) 20 ng/ml stimulation. Macrophage polarization (1 × 106 BMDMs) was initiated with/without the presence of MSC-exosome preparations (0.05–1 × 106 cell equivalents), providing several ratios of MSC-exosome cell equivalents-to-BMDMs. After 24 h, total RNA was isolated and TNFα mRNA levels were assessed by RT-qPCR. The functional endpoint is the capacity of MSC-exosomes to suppress the mRNA induction of TNFα. Step 2: an EC50 value (50% reduction in TNFα mRNA, relative to M1 control) is transformed to an arbitrary exosome potency unit (EPU). Data were adapted from our recent work (8), where we demonstrated purified human umbilical cord MSC-exosomes, dose dependently suppressed mRNA levels of TNFα in alveolar macrophages in vitro. Step 3: an EPU can be applied to standardize dosing between different exosome preparations or as a means of correlating potency to exosome quantity.
Manufacturing and Scale-Up
In 2002, Lamparski et al. described a method for the production and characterization of clinical grade exosomes derived from dendritic cells for their application in cancer vaccine clinical trials (85). Using ultrafiltration coupled with a sucrose/deuterium oxide UC cushion, they isolated vesicles (50–90 nm in diameter) containing major histocompatibility complex (MHC) class-I, -II, and CD1, and tetraspanin molecules (CD9, CD63, and CD81) In addition, in 2005, Navabi and coworkers detailed the development of a method for the preparation and characterization of good manufacturing practice (GMP)-grade exosomes from the ascites fluid of ovarian cancer patients (86). Since then our understanding of exosome biology has improved and the development of specialized isolation and characterization methods has allowed investigators to more accurately isolate and characterize exosome populations.
Considering the development of exosome-based therapeutics, lessons could be learned from cell therapy. The in vitro expansion of cells (such as MSCs) is required to deliver an effective therapeutic dose, with the absence of having a detrimental impact on the quality of the cell. Upon scaling-up, process analytical technology (PAT), a system proposed by the FDA, may be implemented to monitor the manufacturing process through continuous measurement of cell parameters (87, 88). Monitoring bioprocess parameters, such as population doubling time, temperature, metabolite concentrations, pH, pO2 and pCO2, may help ensure optimal exosome quality and quantity, as previous reports have shown that subtle acidic pH shifts may impair exosome aggregation inhibiting forces and, in turn, promote aggregation and reduce functionality (56).
Recently, the inevitable shift to using tissue culture bioreactors has been used to generate large-scale EV preparations. Indeed, Watson and colleagues demonstrated that hollow-fiber bioreactors promotes enhanced exosome production (~40-fold greater EVs/ml of CM) when compared to conventional 2D tissue culture preparations (89). However, it remains unclear if such methods enhance generalized EV production or simply reflect a reduction in exosome re-uptake. Under the considerations discussed above, relating to EV diversity and the possibility that only specific exosome subtypes may represent the therapeutic agent, it is premature to assume that production of higher EV numbers will necessarily yield a higher efficacy final product. Optimization of MSC culture conditions will, therefore, require the parallel development of a dependable and easily adoptable potency assay.
“Off-The-Shelf” Exosomes
With evidence to suggest that exosomes can be stored at −20°C for up to 6 months with no loss to their biochemical activity, “off-the-shelf” exosome-based products represent an attractive pharmaceutical formulation (56, 66, 90). Although standardized storage procedures remain to be defined, current storage protocols use isotonic buffers to prevent pH shifts during storage, avoid freeze–thaw cycles and are absent of dimethyl sulfoxide (DMSO) and glycerol as previous reports have shown these agents may impact exosome integrity (91). With a lack of data addressing the impact of storage time and excipients on exosome structural stability and functional efficacy, more studies are warranted to help define a provisional “shelf-life” for exosome-based products and facilitate the manufacturing and distribution process.
EV-Based Therapy in Clinical Trials
Promising preclinical data that demonstrated dendritic cell-derived EVs containing MHC–peptide complexes could alter tumor growth in immune competent mice led to a phase I anti-melanoma clinical trial conducted in France (92) and a phase I anti-non-small cell lung cancer clinical trial in the United States (93) (clinical trial applications highlighted in Table 4). Both clinical trials administered autologous dendritic cell-derived EVs that met their respective current GMP standards. Such clinical trials to date are important for their demonstration of both the feasibility and the short-term safety of autologous EV administration, but safety considerations for therapies based on exogenous exosome-based products will arguably be more stringent. Nevertheless, it is very encouraging to note that preclinical studies have established immunomodulation as the main therapeutic mechanism of MSC-exosomes action. Immunomodulation is clearly involved in the autologous exosome clinical trials mentioned above, and this may provide guidelines and precedent for clinical trials using exogenous exosomes. In this context, a recent clinical case involving treatment of a steroid-refractory graft-vs-host disease patient with MSC-EVs derived from unrelated bone marrow donors produced encouraging results (94).
Table 4.
Exosome-based therapy: clinical trials.
| Disease | Phase | Vesicle cellular source | Route of administration | Isolation method | Modified (Y/N) | Status | Reference |
|---|---|---|---|---|---|---|---|
| Melanoma | I—open label | Autologous monocyte-derived dendritic cells | SC | UF/UC sucrose cushion | Y | Complete | Escudier et al. (92) |
| Non-small cell lung cancer | I—open label | Autologous monocyte-derived dendritic cells | SC and intradermal | UF/UC sucrose cushion | Y | Complete | Morse et al. (93) |
| Colon cancer | I—open label | Autologous ascites | SC | UC sucrose cushion | N | Complete | Dai et al. (95) |
| Colon cancer | I—open label | Plant based | – | Not declared | Y | Ongoing | NCT01294072 |
| Type I diabetes | I—open label | Umbilical cord blood (allogeneic) MSC | – | Not declared | N | Ongoing | NCT02138331 |
| Non-small cell lung cancer | II—open label | Tumor cell | Pleural or peritoneal cavity | Not declared | Y | Complete | Besse et al. (96) |
| Wound healing (Ulcer) | I—open label | Plasma (autologous) | – | Not declared | N | Enrolling | NCT02565264 |
MSC, mesenchymal stem/stromal cells; SC, subcutaneous; UF, ultrafiltration; UC, ultracentrifugation.
Adapted from Lener et al. (56).
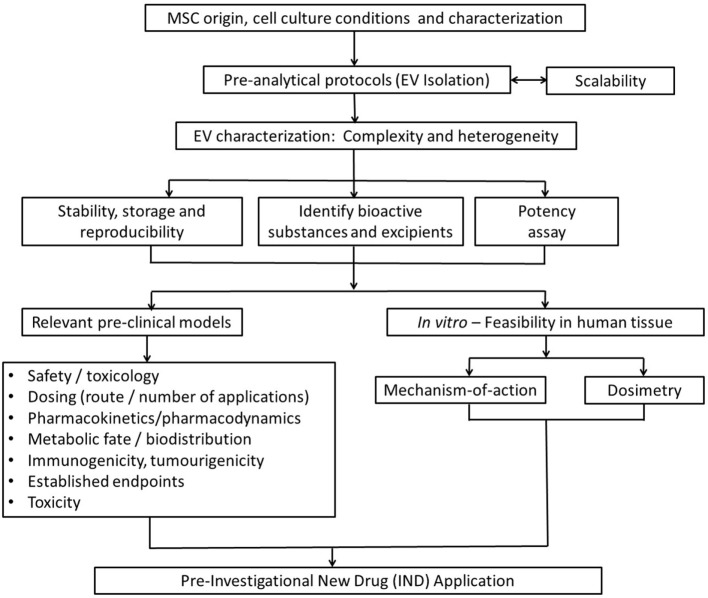
Ultimately, issues raised in this review aim to provide a basic guidance for investigators on key issues to consider for the smooth transition of exosome-based therapies from the preclinical model into clinical development (Figure 5). Among them, determining the optimal dose, the appropriate time window for exosome administration, the number of doses, and route of administration that achieves maximal efficacy without adverse effects are the most important issues to resolve. Such issues will be disease/model specific and clearly beyond the scope of this work.
Figure 5.
Strategic flowchart for the preclinical testing of exosome-based therapeutics. EV, extracellular vesicle. Adapted from Ref. (97).
Summary
Exosome-based therapeutics represent a most promising next generation approach for treating a diverse number of diseases, particularly diseases the pathogenesis of which involves a primary (or major) inflammatory component. The efficacy of MSC-exosome treatments has been robustly established in numerous preclinical models, but development of large-scale GMP-grade exosome-based pharmaceuticals and subsequent clinical trials demand the resolution of several technological and mechanistic issues, reflecting the cautious navigation in unknown seas for this relatively novel field. Among the major issues to be resolved are the definition of an EPU, the standardization of MSC culture conditions and protocols for exosome harvest and storage. Although safety considerations need also to be addressed, it is expected that safety concerns for cell-free, exosome-based clinical trials will be arguably milder than those relevant to live cell MSC trials currently in progress, as mutagenicity and oncogenicity concerns will be null.
Author Contributions
GW participated in data collection, analysis, and manuscript writing. SK and SAM contributed to final article editing and approval.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Funding. This work was supported in part by NIH grants RO1 HL085446 and RO1 HL055454 (SK) and a United Therapeutics Corp. Sponsored Research Grant (SK and SAM).
References
- 1.Gould SJ, Raposo G. As we wait: coping with an imperfect nomenclature for extracellular vesicles. J Extracell Vesicles (2013) 2:20389. 10.3402/jev.v2i0.20389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Willms E, Johansson HJ, Mäger I, Lee Y, Blomberg KEM, Sadik M, et al. Cells release subpopulations of exosomes with distinct molecular and biological properties. Sci Rep (2016) 6:22519. 10.1038/srep22519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnstone RM, Adam M, Hammond JR, Orr L, Turbide C. Vesicle formation during reticulocyte maturation. Association of plasma membrane activities with released vesicles (exosomes). J Biol Chem (1987) 262:9412–20. [PubMed] [Google Scholar]
- 4.Théry C. Exosomes: secreted vesicles and intercellular communications. F1000 Biol Rep (2011) 3:15. 10.3410/B3-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van der Pol E, Böing AN, Harrison P, Sturk A, Nieuwland R. Classification, functions, and clinical relevance of extracellular vesicles. Pharmacol Rev (2012) 64:676–705. 10.1124/pr.112.005983 [DOI] [PubMed] [Google Scholar]
- 6.Kowal J, Tkach M, Théry C. Biogenesis and secretion of exosomes. Curr Opin Cell Biol (2014) 29:116–25. 10.1016/j.ceb.2014.05.004 [DOI] [PubMed] [Google Scholar]
- 7.de Jong OG, Verhaar MC, Chen Y, Vader P, Gremmels H, Posthuma G, et al. Cellular stress conditions are reflected in the protein and RNA content of endothelial cell-derived exosomes. J Extracell Vesicles (2012) 1:18396. 10.3402/jev.v1i0.18396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Willis GR, Fernandez-Gonzalez A, Anastas J, Vitali SH, Liu X, Ericsson M, et al. Mesenchymal stromal cell exosomes ameliorate experimental bronchopulmonary dysplasia and restore lung function through macrophage immunomodulation. Am J Respir Crit Care Med (2017). 10.1164/rccm.201705-0925OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azmi AS, Bao B, Sarkar FH. Exosomes in cancer development, metastasis and drug resistance: a comprehensive review. Cancer Metastasis Rev (2013) 32:623–42. 10.1007/s10555-10013-19441-10559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krause M, Samoylenko A, Vainio SJ. Exosomes as renal inductive signals in health and disease, and their application as diagnostic markers and therapeutic agents. Front Cell Dev Biol (2015) 3:65. 10.3389/fcell.2015.00065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Howitt J, Hill AF. Exosomes in the pathology of neurodegenerative diseases. J Biol Chem (2016) 23:26589–97. 10.1074/jbc.R116.757955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hugel B, Martínez MC, Kunzelmann C, Freyssinet J-M. Membrane microparticles: two sides of the coin. Physiology (2005) 20:22. 10.1152/physiol.00029.2004 [DOI] [PubMed] [Google Scholar]
- 13.Ailawadi S, Wang X, Gu H, Fan G-C. Pathologic function and therapeutic potential of exosomes in cardiovascular disease. Biochim Biophys Acta (2015) 1852:1–11. 10.1016/j.bbadis.2014.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aslam M, Baveja R, Liang OD, Fernandez-Gonzalez A, Lee C, Mitsialis SA, et al. Bone marrow stromal cells attenuate lung injury in a murine model of neonatal chronic lung disease. Am J Respir Crit Care Med (2009) 180:1122–30. 10.1164/rccm.200902-0242OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang Y, Chopp M, Meng Y, Katakowski M, Xin H, Mahmood A, et al. Effect of exosomes derived from multipluripotent mesenchymal stromal cells on functional recovery and neurovascular plasticity in rats after traumatic brain injury. J Neurosurg (2015) 122:856–67. 10.3171/2014.11.JNS14770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lai RC, Arslan F, Lee MM, Sze NSK, Choo A, Chen TS, et al. Exosome secreted by MSC reduces myocardial ischemia/reperfusion injury. Stem Cell Res (2010) 4:214–22. 10.1016/j.scr.2009.12.003 [DOI] [PubMed] [Google Scholar]
- 17.Arslan F, Lai RC, Smeets MB, Akeroyd L, Choo A, Aguor ENE, et al. Mesenchymal stem cell-derived exosomes increase ATP levels, decrease oxidative stress and activate PI3K/Akt pathway to enhance myocardial viability and prevent adverse remodeling after myocardial ischemia/reperfusion injury. Stem Cell Res (2013) 10:301–12. 10.1016/j.scr.2013.01.002 [DOI] [PubMed] [Google Scholar]
- 18.Lee C, Mitsialis SA, Aslam M, Vitali SH, Vergadi E, Konstantinou G, et al. Exosomes mediate the cytoprotective action of mesenchymal stromal cells on hypoxia-induced pulmonary hypertension. Circulation (2012) 126:2601–11. 10.1161/CIRCULATIONAHA.112.114173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dorronsoro A, Robbins PD. Regenerating the injured kidney with human umbilical cord mesenchymal stem cell-derived exosomes. Stem Cell Res Ther (2013) 4:39–39. 10.1186/scrt187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang G, Wang D, Miao S, Zou X, Liu G, Zhu Y. Extracellular vesicles derived from mesenchymal stromal cells may possess increased therapeutic potential for acute kidney injury compared with conditioned medium in rodent models: a meta-analysis. Exp Ther Med (2016) 11:1519–25. 10.3892/etm.2016.3076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xin H, Li Y, Buller B, Katakowski M, Zhang Y, Wang X, et al. Exosome-mediated transfer of mir-133b from multipotent mesenchymal stromal cells to neural cells contributes to neurite outgrowth. Stem Cells (2012) 30:1556–64. 10.1002/stem.1129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kalani A, Tyagi N. Exosomes in neurological disease, neuroprotection, repair and therapeutics: problems and perspectives. Neural Regen Res (2015) 10:1565–7. 10.4103/1673-5374.165305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aliotta JM, Pereira M, Wen S, Dooner MS, Del Tatto M, Papa E, et al. Exosomes induce and reverse monocrotaline-induced pulmonary hypertension in mice. Cardiovasc Res (2016) 110:319–30. 10.1093/cvr/cvw054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhu Y-G, Feng X-M, Abbott J, Fang X-H, Hao Q, Monsel A, et al. Human mesenchymal stem cell microvesicles for treatment of E. coli endotoxin-induced acute lung injury in mice. Stem Cells (2014) 32:116–25. 10.1002/stem.1504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Phinney DG, Di Giuseppe M, Njah J, Sala E, Shiva S, St Croix CM, et al. Mesenchymal stem cells use extracellular vesicles to outsource mitophagy and shuttle microRNAs. Nat Commun (2015) 6:8472. 10.1038/ncomms9472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Monsel A, Zhu Y-G, Gennai S, Hao Q, Hu S, Rouby J-J, et al. Therapeutic effects of human mesenchymal stem cell-derived microvesicles in severe pneumonia in mice. Am J Respir Crit Care Med (2015) 192:324–36. 10.1164/rccm.201410-1765OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yu B, Kim HW, Gong M, Wang J, Millard RW, Wang Y, et al. Exosomes secreted from GATA-4 overexpressing mesenchymal stem cells serve as a reservoir of anti-apoptotic microRNAs for cardioprotection. Int J Cardiol (2015) 182:349–60. 10.1016/j.ijcard.2014.12.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bian S, Zhang L, Duan L, Wang X, Min Y, Yu H. Extracellular vesicles derived from human bone marrow mesenchymal stem cells promote angiogenesis in a rat myocardial infarction model. J Mol Med (2014) 92:387–97. 10.1007/s00109-013-1110-5 [DOI] [PubMed] [Google Scholar]
- 29.Teng X, Chen L, Chen W, Yang J, Yang Z, Shen Z. Mesenchymal stem cell-derived exosomes improve the microenvironment of infarcted myocardium contributing to angiogenesis and anti-inflammation. Cell Physiol Biochem (2015) 37:2415–24. 10.1159/000438594 [DOI] [PubMed] [Google Scholar]
- 30.Kim D-K, Nishida H, An SY, Shetty AK, Bartosh TJ, Prockop DJ. Chromatographically isolated CD63+CD81+ extracellular vesicles from mesenchymal stromal cells rescue cognitive impairments after TBI. Proc Natl Acad Sci U S A (2016) 113:170–5. 10.1073/pnas.1522297113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yu B, Shao H, Su C, Jiang Y, Chen X, Bai L, et al. Exosomes derived from MSCs ameliorate retinal laser injury partially by inhibition of MCP-1. Sci Rep (2016) 6:34562. 10.1038/srep34562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mead B, Tomarev S. BMSC-derived exosomes promote survival of retinal ganglion cells through miRNA-dependent mechanisms. Stem Cells Transl Med (2017) 6:1273–85. 10.1002/sctm.16-0428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Doeppner TR, Herz J, Görgens A, Schlechter J, Ludwig A-K, Radtke S, et al. Extracellular vesicles improve post-stroke neuroregeneration and prevent postischemic immunosuppression. Stem Cells Transl Med (2015) 4:1131–43. 10.5966/sctm.2015-0078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xin H, Li Y, Cui Y, Yang JJ, Zhang ZG, Chopp M. Systemic administration of exosomes released from mesenchymal stromal cells promote functional recovery and neurovascular plasticity after stroke in rats. J Cereb Blood Flow Metab (2013) 33:1711–5. 10.1038/jcbfm.2013.152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lo Sicco C, Reverberi D, Balbi C, Ulivi V, Principi E, Pascucci L, et al. Mesenchymal stem cell-derived extracellular vesicles as mediators of anti-inflammatory effects: endorsement of macrophage polarization. Stem Cells Transl Med (2017) 6:1018–28. 10.1002/sctm.16-0363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tan CY, Lai RC, Wong W, Dan YY, Lim S-K, Ho HK. Mesenchymal stem cell-derived exosomes promote hepatic regeneration in drug-induced liver injury models. Stem Cell Res Ther (2014) 5:76. 10.1186/scrt465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li T, Yan Y, Wang B, Qian H, Zhang X, Shen L, et al. Exosomes derived from human umbilical cord mesenchymal stem cells alleviate liver fibrosis. Stem Cells Dev (2013) 22:845–54. 10.1089/scd.2012.0395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yang J, Liu X-X, Fan H, Tang Q, Shou Z-X, Zuo D-M, et al. Extracellular vesicles derived from bone marrow mesenchymal stem cells protect against experimental colitis via attenuating colon inflammation, oxidative stress and apoptosis. PLoS One (2015) 10:e0140551. 10.1371/journal.pone.0140551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fang S, Xu C, Zhang Y, Xue C, Yang C, Bi H, et al. Umbilical cord-derived mesenchymal stem cell-derived exosomal micrornas suppress myofibroblast differentiation by inhibiting the transforming growth factor-β/SMAD2 pathway during wound healing. Stem Cells Transl Med (2016) 5:1425–39. 10.5966/sctm.2015-0367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang J, Guan J, Niu X, Hu G, Guo S, Li Q, et al. Exosomes released from human induced pluripotent stem cells-derived MSCs facilitate cutaneous wound healing by promoting collagen synthesis and angiogenesis. J Transl Med (2015) 13:49. 10.1186/s12967-015-0417-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zou X, Zhang G, Cheng Z, Yin D, Du T, Ju G, et al. Microvesicles derived from human Wharton’s Jelly mesenchymal stromal cells ameliorate renal ischemia-reperfusion injury in rats by suppressing CX3CL1. Stem Cell Res Ther (2014) 5:40. 10.1186/scrt428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bruno S, Grange C, Collino F, Deregibus MC, Cantaluppi V, Biancone L, et al. Microvesicles derived from mesenchymal stem cells enhance survival in a lethal model of acute kidney injury. PLoS One (2012) 7:e33115. 10.1371/journal.pone.0033115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lai RC, Chen TS, Lim SK. Mesenchymal stem cell exosome: a novel stem cell-based therapy for cardiovascular disease. Regen Med (2011) 6:481–92. 10.2217/rme.11.35 [DOI] [PubMed] [Google Scholar]
- 44.Kourembanas S. Stem cell-based therapy for newborn lung and brain injury: feasible, safe, and the next therapeutic breakthrough? J Pediatr (2014) 164:954–6. 10.1016/j.jpeds.2014.01.064 [DOI] [PubMed] [Google Scholar]
- 45.Mitsialis SA, Kourembanas S. Stem cell-based therapies for the newborn lung and brain: possibilities and challenges. Semin Perinatol (2016) 40:138–51. 10.1053/j.semperi.2015.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Phinney DG, Pittenger MF. Concise review: MSC-derived exosomes for cell-free therapy. Stem Cells (2017) 35:851–8. 10.1002/stem.2575 [DOI] [PubMed] [Google Scholar]
- 47.Romanov YA, Darevskaya AN, Merzlikina NV, Buravkova LB. Mesenchymal stem cells from human bone marrow and adipose tissue: isolation, characterization, and differentiation potentialities. Bull Exp Biol Med (2005) 140:138–43. 10.1007/s10517-005-0430-z [DOI] [PubMed] [Google Scholar]
- 48.Hendijani F. Explant culture: an advantageous method for isolation of mesenchymal stem cells from human tissues. Cell Prolif (2017) 50:e12334. 10.1111/cpr.12334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini FC, Krause DS, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy (2006) 8:315–7. 10.1080/14653240600855905 [DOI] [PubMed] [Google Scholar]
- 50.Choudhery MS, Khan M, Mahmood R, Mehmood A, Khan SN, Riazuddin S. Bone marrow derived mesenchymal stem cells from aged mice have reduced wound healing, angiogenesis, proliferation and anti-apoptosis capabilities. Cell Biol Int (2012) 36:747–53. 10.1042/CBI20110183 [DOI] [PubMed] [Google Scholar]
- 51.Choudhery MS, Badowski M, Muise A, Harris DT. Comparison of human adipose and cord tissue derived mesenchymal stem cells. Cytotherapy (2013) 15:330–43. 10.1016/j.jcyt.2012.11.010 [DOI] [PubMed] [Google Scholar]
- 52.Choudhery MS, Badowski M, Muise A, Pierce J, Harris DT. Donor age negatively impacts adipose tissue-derived mesenchymal stem cell expansion and differentiation. J Transl Med (2014) 12:8. 10.1186/1479-5876-12-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Halme DG, Kessler DA. FDA regulation of stem-cell–based therapies. N Engl J Med (2006) 355:1730–5. 10.1056/NEJMhpr063086 [DOI] [PubMed] [Google Scholar]
- 54.Harron DWG. Technical requirements for registration of pharmaceuticals for human use: the ICH process. In: Griffin JP, editor. The Textbook of Pharmaceutical Medicine. Oxford: Blackwell Publishing Ltd; (2007). p. 552–64. [Google Scholar]
- 55.Ancans J. Cell therapy medicinal product regulatory framework in Europe and its application for MSC-based therapy development. Front Immunol (2012) 3:253. 10.3389/fimmu.2012.00253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lener T, Gimona M, Aigner L, Börger V, Buzas E, Camussi G, et al. Applying extracellular vesicles based therapeutics in clinical trials – an ISEV position paper. J Extracell Vesicles (2015) 4:30087. 10.3402/jev.v4.30087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Waszak P, Alphonse R, Vadivel A, Ionescu L, Eaton F, Thebaud B. Preconditioning enhances the paracrine effect of mesenchymal stem cells in preventing oxygen-induced neonatal lung injury in rats. Stem Cells Dev (2012) 21:2789–97. 10.1089/scd.2010.0566 [DOI] [PubMed] [Google Scholar]
- 58.Riis S, Stensballe A, Emmersen J, Pennisi CP, Birkelund S, Zachar V, et al. Mass spectrometry analysis of adipose-derived stem cells reveals a significant effect of hypoxia on pathways regulating extracellular matrix. Stem Cell Res Ther (2016) 7:52. 10.1186/s13287-016-0310-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rosová I, Dao M, Capoccia B, Link D, Nolta JA. Hypoxic preconditioning results in increased motility and improved therapeutic potential of human mesenchymal stem cells. Stem Cells (2008) 26:2173–82. 10.1634/stemcells.2007-1104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Burnley-Hall N, Willis G, Davis J, Rees DA, James PE. Nitrite-derived nitric oxide reduces hypoxia-inducible factor 1α-mediated extracellular vesicle production by endothelial cells. Nitric Oxide (2017) 63:1–12. 10.1016/j.niox.2016.12.005 [DOI] [PubMed] [Google Scholar]
- 61.Boekstegers P, Riessen R, Seyde W. Oxygen partial pressure distribution within skeletal muscle: indicator of whole body oxygen delivery in patients? Adv Exp Med Biol (1990) 277:507–14. 10.1007/978-1-4684-8181-5_57 [DOI] [PubMed] [Google Scholar]
- 62.Le Q-T, Chen E, Salim A, Cao H, Kong CS, Whyte R, et al. An Evaluation of tumor oxygenation and gene expression in patients with early stage non–small cell lung cancers. Clin Cancer Res (2006) 12:1507–14. 10.1158/1078-0432.CCR-05-2049 [DOI] [PubMed] [Google Scholar]
- 63.Carreau A, Hafny-Rahbi BE, Matejuk A, Grillon C, Kieda C. Why is the partial oxygen pressure of human tissues a crucial parameter? Small molecules and hypoxia. J Cell Mol Med (2011) 15:1239–53. 10.1111/j.1582-4934.2011.01258.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kowal J, Arras G, Colombo M, Jouve M, Morath JP, Primdal-Bengtson B, et al. Proteomic comparison defines novel markers to characterize heterogeneous populations of extracellular vesicle subtypes. Proc Natl Acad Sci U S A (2016) 113:E968–77. 10.1073/pnas.1521230113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lai RC, Tan SS, Yeo RWY, Choo ABH, Reiner AT, Su Y, et al. MSC secretes at least 3 EV types each with a unique permutation of membrane lipid, protein and RNA. J Extracell Vesicles (2016) 5:29828. 10.3402/jev.v5.29828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Batrakova EV, Kim MS. Development and regulation of exosome-based therapy products. Wiley Interdiscip Rev Nanomed Nanobiotechnol (2016) 8:744–57. 10.1002/wnan.1395 [DOI] [PubMed] [Google Scholar]
- 67.Théry C, Amigorena S, Raposo G, Clayton A. Chapter 3: Isolation and characterization of exosomes from cell culture supernatants and biological fluids. Current Protocols in Cell Biology. John Wiley & Sons, Inc; (2006). Unit 3.22 p. 10.1002/0471143030.cb0322s30 [DOI] [PubMed] [Google Scholar]
- 68.Momen-Heravi F, Balaj L, Alian S, Mantel P-Y, Halleck Allison E, Trachtenberg Alexander J, et al. Current methods for the isolation of extracellular vesicles. Biol Chem (2013) 394:1253–6. 10.1515/hsz-2013-0141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Witwer KW, Buzás EI, Bemis LT, Bora A, Lässer C, Lötvall J, et al. Standardization of sample collection, isolation and analysis methods in extracellular vesicle research. J Extracell Vesicles (2013) 2:20360. 10.3402/jev.v2i0.20360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Linares R, Tan S, Gounou C, Arraud N, Brisson AR. High-speed centrifugation induces aggregation of extracellular vesicles. J Extracell Vesicles (2015) 4:29509. 10.3402/jev.v4.29509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Böing AN, Van Der Pol E, Grootemaat AE, Coumans FAW, Sturk A, Nieuwland R. Single-step isolation of extracellular vesicles by size-exclusion chromatography. J Extracell Vesicles (2014) 3:23430. 10.3402/jev.v3.23430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Li P, Kaslan M, Lee SH, Yao J, Gao Z. Progress in exosome isolation techniques. Theranostics (2017) 7:789–804. 10.7150/thno.18133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lee K, Shao H, Weissleder R, Lee H. Acoustic purification of extracellular microvesicles. ACS Nano (2015) 9:2321–7. 10.1021/nn506538f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Li P, Mao Z, Peng Z, Zhou L, Chen Y, Huang P-H, et al. Acoustic separation of circulating tumor cells. Proc Natl Acad Sci U S A (2015) 112:4970–5. 10.1073/pnas.1504484112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sitar S, Kejžar A, Pahovnik D, Kogej K, Tušek-Žnidarič M, Lenassi M, et al. Size characterization and quantification of exosomes by asymmetrical-flow field-flow fractionation. Anal Chem (2015) 87:9225–33. 10.1021/acs.analchem.5b01636 [DOI] [PubMed] [Google Scholar]
- 76.Kang D, Oh S, Ahn S-M, Lee B-H, Moon MH. Proteomic analysis of exosomes from human neural stem cells by flow field-flow fractionation and nanoflow liquid chromatography−tandem mass spectrometry. J Proteome Res (2008) 7:3475–80. 10.1021/pr800225z [DOI] [PubMed] [Google Scholar]
- 77.Petersen KE, Manangon E, Hood JL, Wickline SA, Fernandez DP, Johnson WP, et al. A review of exosome separation techniques and characterization of B16-F10 mouse melanoma exosomes with AF4-UV-MALS-DLS-TEM. Anal Bioanal Chem (2014) 406:7855–66. 10.1007/s00216-014-8040-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wang Z, Wu H-J, Fine D, Schmulen J, Hu Y, Godin B, et al. Ciliated micropillars for the microfluidic-based isolation of nanoscale lipid vesicles. Lab Chip (2013) 13:2879–82. 10.1039/c3lc41343h [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Akers JC, Ramakrishnan V, Nolan JP, Duggan E, Fu C-C, Hochberg FH, et al. Comparative analysis of technologies for quantifying extracellular vesicles (evs) in clinical cerebrospinal fluids (CSF). PLoS One (2016) 11:e0149866. 10.1371/journal.pone.0149866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chia BS, Low YP, Wang Q, Li P, Gao Z. Advances in exosome quantification techniques. Trends Anal Chem (2017) 86:93–106. 10.1016/j.trac.2016.10.012 [DOI] [Google Scholar]
- 81.Koritzinsky EH, Street JM, Star RA, Yuen PST. Quantification of exosomes. J Cell Physiol (2017) 232:1587–90. 10.1002/jcp.25387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rupert DLM, Claudio V, Lässer C, Bally M. Methods for the physical characterization and quantification of extracellular vesicles in biological samples. Biochim Biophys Acta (2017) 1861:3164–79. 10.1016/j.bbagen.2016.07.028 [DOI] [PubMed] [Google Scholar]
- 83.Jiao J, Milwid JM, Yarmush ML, Parekkadan B. A mesenchymal stem cell potency assay. Methods Mol Biol (2011) 677:221–31. 10.1007/978-1-60761-869-0_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wynn TA, Vannella KM. Macrophages in tissue repair, regeneration, and fibrosis. Immunity (2016) 44:450–62. 10.1016/j.immuni.2016.02.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lamparski HG, Metha-Damani A, Yao J-Y, Patel S, Hsu D-H, Ruegg C, et al. Production and characterization of clinical grade exosomes derived from dendritic cells. J Immunol Methods (2002) 270:211–26. 10.1016/S0022-1759(02)00330-7 [DOI] [PubMed] [Google Scholar]
- 86.Navabi H, Croston D, Hobot J, Clayton A, Zitvogel L, Jasani B, et al. Preparation of human ovarian cancer ascites-derived exosomes for a clinical trial. Blood Cells Mol Dis (2005) 35:149–52. 10.1016/j.bcmd.2005.06.008 [DOI] [PubMed] [Google Scholar]
- 87.Placzek MR, Chung I-M, Macedo HM, Ismail S, Mortera Blanco T, Lim M, et al. Stem cell bioprocessing: fundamentals and principles. J R Soc Interface (2009) 6:209–32. 10.1098/rsif.2008.0442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Heathman TRJ, Nienow AW, Mccall MJ, Coopman K, Kara B, Hewitt CJ. The translation of cell-based therapies: clinical landscape and manufacturing challenges. Regen Med (2015) 10:49–64. 10.2217/rme.14.73 [DOI] [PubMed] [Google Scholar]
- 89.Watson DC, Bayik D, Srivatsan A, Bergamaschi C, Valentin A, Niu G, et al. Efficient production and enhanced tumor delivery of engineered extracellular vesicles. Biomaterials (2016) 105:195–205. 10.1016/j.biomaterials.2016.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Vishnubhatla I, Corteling R, Stevanato L, Hicks C, Sinden J. The development of stem cell-derived exosomes as a cell-free regenerative medicine. J Circ Biomark (2016) 3:2. 10.5772/58597 [DOI] [Google Scholar]
- 91.Lőrincz ÁM, Timár CI, Marosvári KA, Veres DS, Otrokocsi L, Kittel Á, et al. Effect of storage on physical and functional properties of extracellular vesicles derived from neutrophilic granulocytes. J Extracell Vesicles (2014) 3:25465. 10.3402/jev.v3.25465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Escudier B, Dorval T, Chaput N, André F, Caby M-P, Novault S, et al. Vaccination of metastatic melanoma patients with autologous dendritic cell (DC) derived-exosomes: results of the first phase I clinical trial. J Transl Med (2005) 3:10–10. 10.1186/1479-5876-3-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Morse MA, Garst J, Osada T, Khan S, Hobeika A, Clay TM, et al. A phase I study of exosome immunotherapy in patients with advanced non-small cell lung cancer. J Transl Med (2005) 3:9. 10.1186/1479-5876-3-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kordelas L, Rebmann V, Ludwig AK, Radtke S, Ruesing J, Doeppner TR, et al. MSC-derived exosomes: a novel tool to treat therapy-refractory graft-versus-host disease. Leukemia (2014) 28:970–3. 10.1038/leu.2014.41 [DOI] [PubMed] [Google Scholar]
- 95.Dai S, Wei D, Wu Z, Zhou X, Wei X, Huang H, et al. Phase I clinical trial of autologous ascites-derived exosomes combined with GM-CSF for colorectal cancer. Mol Ther (2008) 16:782–90. 10.1038/mt.2008.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Besse B, Charrier M, Lapierre V, Dansin E, Lantz O, Planchard D, et al. Dendritic cell-derived exosomes as maintenance immunotherapy after first line chemotherapy in NSCLC. Oncoimmunology (2016) 5:e1071008. 10.1080/2162402X.2015.1071008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Willis GR, Kourembanas S, Mitsialis SA. Therapeutic applications of extracellular vesicles: perspectives from newborn medicine. Methods Mol Biol (2017) 1660:409–32. 10.1007/978-1-4939-7253-1_34 [DOI] [PubMed] [Google Scholar]