Abstract
Previous research has utilized the approach avoidance task (AAT) to measure approach and avoidance action tendencies in socially anxious individuals. “Neutral” social stimuli may be perceived as ambiguous and hence threatening to socially anxious individuals, however it is unclear whether this results in difficulty approaching ambiguous (“neutral”) versus unambiguous threat (e.g., disgust) faces (i.e., intolerance of ambiguity). Thirty participants with Social Anxiety Disorder (SADs) and 29 non-anxious controls completed an implicit AAT in which they were instructed to approach or avoid neutral and disgust faces (i.e., pull or push a joystick) based on color of the picture border. Results indicated that SADs demonstrated greater difficulty approaching neutral relative to disgust faces. Moreover, intolerance for approach of ambiguity predicted social anxiety severity while controlling for the effects of trait anxiety and depression. Our results provide further support for the role of intolerance of ambiguity in SAD.
Keywords: approach avoidance task, automatic action tendencies, intolerance of ambiguity, social anxiety disorder
A substantial body of research demonstrates that individuals with Social Anxiety Disorder (SAD) demonstrate selective information processing biases for threat-related information (for a review see Kuckertz & Amir, 2014). These threat biases are assumed to contribute to the etiology and maintenance of the disorder. For example, diagnostic criteria for SAD specify fear of rejection (American Psychiatric Association, 2013), suggesting that disgust faces might be particularly threatening for those with social anxiety (Rozin, Lowery, & Ebert, 1994). Indeed, socially anxious individuals demonstrate an attentional bias for disgust faces compared to neutral faces (Pishyar, Harris, & Menzies, 2004), and modification of attentional bias for disgust faces has been associated with reduced social anxiety symptoms (Amir et al., 2009), diagnostic remission (Schmidt et al., 2009), and improved performance on a speech task (Amir et al., 2008).
Despite the relevance of non-ambiguously negative facial expressions (i.e., disgust) in social anxiety, research also suggests that “neutral” facial expressions convey ambiguity, and are often negatively valenced for individuals with social anxiety (e.g., Lange, Allart, Keijsers, Rinck, & Becker, 2012; Yoon & Zinbarg, 2008). Indeed, individuals with SAD tend to interpret ambiguous information as threatening (for a review see Kuckertz & Amir, 2014), and thus neutral faces may be associated with more threatening interpretations by individuals with SAD relative to interpretations made by non-anxious controls (NACs). Similarly, neutral facial expressions convey uncertainty regarding the person’s thoughts, feelings, or intent, which may be perceived as threatening by individuals with SAD given that SAD is characterized by intolerance of uncertainty (Boelen & Reijntjes, 2009).
Neutral faces may be perceived as particularly threatening by socially anxious individuals when assessed via implicit tasks. For example, Lange and colleagues (2012) found that individuals with a diagnosis of SAD, compared to NACs, rated Chinese idiographs more negatively when followed by a neutral, subliminally presented face prime. In contrast, SAD and NAC groups did not differ in their ratings of Chinese idiographs following presented of angry, subliminally presented face primes.
Thus, extant literature suggests that both non-ambiguously negative faces (i.e., disgust faces) and ambiguous faces (i.e., neutral faces) may be considered threating to individuals with social anxiety. However, the role that interpretation of neutral versus non-ambiguously negative faces has in the clinical manifestation of SAD is unclear. Diagnostic criteria for SAD include avoidance of feared social situations (American Psychiatric Association, 2013). Consistent with the notion of avoidance as a primary clinical target in SAD, psychosocial treatment of SAD has long included emphasis on exposure therapy (e.g., Feske & Chambless, 1995), which focuses on increasing approach and reducing avoidance of feared social situations. Therefore an important, clinically informative question pertains to the extent to which SAD is characterized by relative avoidance of neutral versus non-ambiguously negative social stimuli. Such an understanding may inform the features of exposure exercises in the context of treatment for SAD.
While findings by Lange and colleagues (2012) suggest that stimuli may be rated more negatively when implicitly primed by a neutral rather than non-ambiguously negative face, such findings do not directly speak to the extent to which individuals approach or avoid neutral versus non-ambiguously negative social stimuli. Fortunately, action tendencies to approach or avoid disorder-relevant stimuli may be assessed at an implicit level via the Approach Avoidance Task (AAT) (Phaf, Mohr, Rotteveel, & Wicherts, 2014; Roefs et al., 2011). According to the reflective impulsive model of behavior (Strack & Deutsch, 2004), stimuli from the environment elicit automatic evaluations that activate affectively congruent behavioral schemas of approach and avoidance. One way to assess these behavioral schemas implicitly is to use speed of arm flexion (i.e., approach) and speed of arm extension (i.e., avoidance) in response to disorder-relevant stimuli using the AAT.
The AAT has been used to study implicit action tendencies in highly socially anxious individuals (HSAs). Voncken, Rinck, Deckers, and Lange (2012) presented HSAs and NACs with pictures of neutral faces and computer monitors and asked participants to pull or push a joystick in response to an emotion-irrelevant feature of the picture, resulting in the visual impression of approach (i.e., face or computer monitor turned towards participant) or avoidance (i.e., face or computer monitor turned away from participant). Voncken et al. calculated approach and avoidance bias scores using a calculation method proposed by Najmi and colleagues (2010). According to this conceptualization, approach and avoidance may represent different aspects of automatic behavior systems in the presence of emotional stimuli, rather than opposite ends of the same continuum (Najmi et al., 2010). Voncken et al. (2012) found that HSAs but not NACs were slower to pull neutral faces towards themselves in comparison to pulling pictures of computer monitors. No group differences were found for pushing the joystick in response to neutral faces versus computer monitors. While these findings suggest that HSAs experienced relative difficulty approaching, but not increased avoidance of neutral faces, the authors did not compare action tendencies for multiple facial expressions, therefore it is unclear whether their findings are due to the effect of neutral expressions specifically or facial stimuli in general.
Several other studies have also used the AAT in the context of social anxiety. For example Roelofs and colleagues (2010) asked HSA and NAC participants to pull or push pictures of angry, happy, or neutral faces based on picture color. However, the authors compared response times for pushing and pulling the joystick within each valence, thus their analyses did not allow for differentiation between biased approach tendencies and biased avoidance tendencies. Similarly, Heuer, Rinck, and Becker (2007) instructed HSAs and NACs to push or pull a joystick in response to angry, neutral, or smiling faces displayed on a computer screen. These researchers used puzzle pictures as non-emotional control stimuli. Like Roelofs and colleagues, these authors did not calculate separate indices for approach and avoidance. Moreover, participants were instructed to respond to the picture content rather than a content-irrelevant feature of the picture, which is arguably not an implicit task (Roefs et al., 2011).
In summary, previous research suggests that the AAT may be a useful task for assessing approach and avoidance action tendencies in individuals with high levels of social anxiety. However, only one study to date has differentiated approach from avoidance tendencies (Voncken et al., 2012). Moreover, that study did not compare relative difficulties of approaching neutral faces to unambiguously threatening faces, thus it is not clear to what extent individuals with social anxiety display difficulty approaching neutral (i.e., ambiguous) versus unambiguous threat faces (i.e., intolerance of ambiguity).
In the current study we addressed three issues in the literature. First, we compared approach and avoidance tendencies for neutral faces versus unambiguously negative (disgust) emotional faces. Our goal was to elucidate relative difficulties with these two stimuli types in social anxiety disorder, or intolerance for ambiguity. Second, we examined the validity of the AAT in a clinically diagnosed population with SAD. Finally, we examined the utility of the AAT in predicting social anxiety symptom severity, when controlling for the effect of trait anxiety and depression.
Method
Participants
Participants were individuals with SAD and NACs. Individuals with SAD (n = 30) met DSM-IV criteria for SAD as determined by the Structural Clinical Interview for DSM-IV (SCID; First, Spitzer, Gibbon, & Williams, 2002) and scored above 50 on the Liebowitz Social Anxiety Scale – Clinician rated version (LSAS-CR; Liebowitz, 1987). Participants were recruited from two clinical trials conducted at the Center for Understanding and Treating Anxiety at San Diego State University (see Amir et al., 2009; Amir & Taylor, 2012 for full inclusion/exclusion criteria and additional sample characteristics); all individuals with SAD completed the task prior to beginning treatment. The average participant age was 38.89 years (SD = 9.98) and the SAD group comprised 54% females.
The non-anxious controls (NACs, n = 26) did not meet diagnostic criteria for any past or present Axis I disorder based on a SCID interview. NACs were recruited from the community and scored 29 or lower on the self-report version LSAS (LSAS-SR). The average participant age was 25.28 years (SD = 13.15) and the NAC group comprised 56% females. All participants were paid $20 for their participation.
Three participants (two SADs and one NAC) were excluded due to less than chance accuracy (< 50%) on the AAT task. Therefore, our final sample comprised 53 participants (SAD, n = 28; NAC, n = 25).
Self-report measures
Beck Depression Inventory-II (BDI-II)
The BDI-II (Beck, Steer, & Brown, 1996) is a self-report inventory to assess depression symptoms. It consists of 21 items on a 0–3 point scale, and a total score is calculated by summing up all responses. Psychometric properties of the BDI-II are good among both clinical and non-clinical samples. Internal consistency in the current sample was excellent (Cronbach’s alpha = .96).
Spielberger State-Trait Anxiety Inventory (STAI-S/T)
The STAI (Spielberger, Gorsuch, Lushene, Vagg, and Jacobs, 1983) is a 40-item questionnaire assessing the intensity of feelings of anxiety, distinguishing between state anxiety (i.e., how participants feel right now) and trait anxiety (i.e., how participants feel generally). Answers are given on a 1–4 point scale and a total score is calculated by summing up all responses. Internal consistency in the current sample was excellent (Cronbach’s alpha = .97).
Liebowitz Social Anxiety Scale (LSAS, Clinician-Rated and Self-Report versions)
The LSAS (Liebowitz, 1987) measures symptoms of social anxiety. It consists of 24 social situations, and participants are asked to rate their level of fear and avoidance for each situation on a 0–3 point scale. The LSAS can be clinician-rated (LSAS-CR) in which the LSAS is administered during a clinical interview or self-report (LSAS-SR). Both versions are psychometrically sound, and scales can be used interchangeably (Fresco, et al., 2001). The LSAS-CR was administered to the clinical socially anxious sample during the interview; the LSAS-SR was administered to the non-anxious group. Internal consistency in the current sample was excellent for the LSAS-CR (Cronbach’s alpha = .93) and LSAS-SR (Cronbach’s alpha = .91).
The approach-avoidance task
The stimuli for the AAT assessment comprised eight pictures of faces: four with disgust expressions and four with neutral expressions. Actors comprised two Caucasian adult males and two Caucasian adult females. These pictures were selected from a well-validated set of emotional facial expressions (Matsumoto & Ekman, 1988) and have been used in previous research examining information-processing biases in SAD (Amir et al., 2009; Schmidt et al., 2009). We selected disgust faces as our non-ambiguous negative facial expression due to previous research utilizing disgust faces in AAT for anxiety disorders (Kuckertz, Carmona, Chang, Piacentini,& Amir, 2015) as well as in other information processing tasks in socially anxious individuals (Amir et al., 2008; Amir et al., 2009; Pishyar, Harris, & Menzies, 2004; Schmidt et al., 2009). The pictures were surrounded by a green or a blue border. Participants were instructed to pull the joystick if the border was green and to push the joystick if the border was blue. To remain consistent with previous research (Amir, Kuckertz, & Najmi, 2013), we included filler trials in which pictures were framed by a beige border designating movement to the right side, however these trials were not included in analysis.
Participants were seated in front of a computer screen, with a joystick situated on the desk. Pulling the joystick resulted in an increasingly larger picture while pushing the joystick resulted in a smaller picture, simulating approach and avoidance, respectively. The picture would disappear if the joystick was pushed or pulled 30° into either direction, regardless of response accuracy. The next trial would start if the participant moved the joystick back into the central position and pushed the button on the joystick. Response latencies were measured from the appearance until the disappearance of the picture.
Prior to the assessment participants completed a practice. During the practice participants completed thirteen trials with a different set of disgust and neutral pictures than the pictures used in the experimental task. The assessment phase comprised 192 trials [4 Actors × 2 Facial expressions (Disgust, Neutral) × 3 Border color (Green, Blue, Beige) × 8 Repetitions]. Trials were presented in a different random order for each participant.
Procedure
Participants signed the informed consent form and provided demographic information. Next, participants completed the BDI-II, STAI-S/T, and either LSAS-SR (NACs) or the LSAS-CR (SADs). A trained (masters or doctoral level) interviewer administered the SCID. Participants then completed the AAT. This procedure was approved by the Institutional Review Board at San Diego State University.
Results
Demographics and Baseline Data
The final groups comprising 28 individuals with SAD and 25 NACs did not differ significantly in age [t(51) = 1.00, p = .322, d = 0.27],1 education [t(50) = 0.32, p = .750, d= 0.09], or gender ratio [χ2(1) = 0.03, p = .859]. As expected, individuals with SAD had higher scores than NACs on symptoms of social anxiety [t(51) = 17.33, p < .001, d = 4.76], state anxiety [t(50) = 8.02, p < .001, d = 2.23], trait anxiety [t(50) = 10.82, p< .001, d = 3.01], and depressive symptoms [t(50) = 8.20, p < .001, d = 2.28]. See Table 1 for demographic and self-report data.
Table 1.
Demographics, Symptom, and AAT Response Latency Data
| Group | ||
|---|---|---|
| Variable | SAD (n = 28) | NAC (n = 25) |
| % Female | 53.57a | 56.00a |
| Age | 38.89 (9.98)a | 35.28 (13.15)a |
| Education | 14.96 (2.18)a | 14.76 (2.39)a |
| LSAS/LSAS-SR | 87.29 (21.73)a | 7.84 (7.68)b |
| STAI-T | 59.21 (10.29)a | 29.88 (9.07)b |
| STAI-S | 52.29 (11.88)a | 28.21 (9.37)b |
| BDI-II | 24.64 (12.92)a | 2.38 (3.37)b |
| Disgust Pull | 1026 (132)a | 974 (166)a |
| Neutral Pull | 1209 (176)a | 1081 (195)b |
| Disgust Push | 1031 (159)a | 960 (158)a |
| Neutral Push | 1195 (214)a | 1095 (180)a |
Note. Mean response latencies presented in milliseconds with standard deviations presented in parentheses. LSAS = Liebowitz Social Anxiety Scale (Liebowitz, 1987); LSAS-SR = Liebowitz Social Anxiety Scale Self-Report (Liebowitz, 1987); STAI-T = Spielberger State-Trait Anxiety Inventory – Trait; STAI-S = Spielberger State-Trait Anxiety Inventory – State (Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983); BDI-II = Beck Depression Inventory-II (Beck, Steer, & Brown, 1996); means with different subscript differ significantly.
Approach-Avoidance Task (AAT)
Data Preparation
We removed incorrect trials and the highest and lowest 1% of response latencies from the AAT. We also removed response latencies deviating more than two SD from the mean response latency for each participant's own overall response latency (Kuckertz et al., 2015).
Group Differences in Approach and Avoidance
Response latencies were analyzed separately for the two response directions (i.e., pull and push; Najmi et al., 2010). Table 1 presents overall mean response latencies for each response direction and face type.
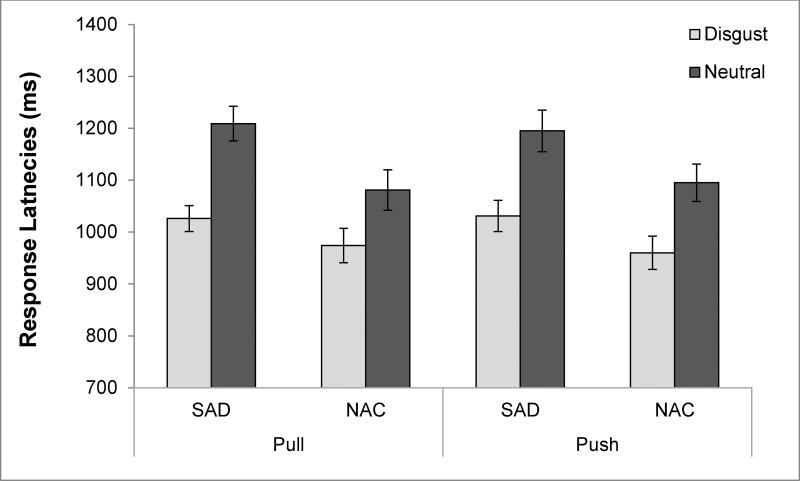
For the push response direction, we submitted the mean response latencies to a 2 (Group: SAD, NAC) × 2 (Valence: Disgust Face, Neutral Face) repeated measures ANOVA (see Figure 1). This analysis revealed a significant main effect of Valence [F(1,51) = 121.18, p < .001, η2 = .70] such that all participants pushed disgust faces more quickly than neutral faces. The main effect of Group [F(1,51) = 3.21, p = .079, η2 = .06] was marginally significant with SADs slower in pushing faces in general than NACs. The Valence × Group interaction was not significant [F(1,51) = 1.16, p = .520, η2 = .02].
Figure 1.
Mean response latencies (with standard error bars) as a function of Group (SAD, NAC), Picture Type (Disgust, Neutral), and Response Direction (Pull, Push).
Similarly, we submitted the mean response latencies for the pull responses to a 2 (Group: SAD, NAC) × 2 (Valence: Disgust Face, Neutral Face) repeated measures ANOVA. Both the main effects of Valence [F(1,51) = 133.11, p < .001, η2 = .72] and Group [F(1,51) = 4.04, p = .050, η2 = .07] were significant. These main effects were qualified by an interaction of Group × Valence [F(1,51) = 8.97, p = .004, η2 = .15]. Follow-up simple effects analyses revealed that SADs were slower in pulling neutral faces compared to NACs[t(51) = 2.50, p = .016, d = 0.69]; however groups did not differ in speed of pulling disgust pictures [t(51) = 1.25, p = .216, d = 0.34]. Moreover, both SADs [t(27) = −8.84, p < .001, d = 1.18] and NACs [t(24) = −7.98, p < .001, d = 0.59] were slower in pulling neutral faces compared to disgust faces. Similar to past research (e.g., Najmi et al., 2010; Voncken et al., 2012) we also computed an approach bias (difference between response latencies in pulling disgust faces compared to response latencies for pulling neutral faces). This intolerance for approach of ambiguity index would be negative when there is a greater difficulty approaching neutral faces relative to nonambiguous disgust faces. This bias was more negative for SADs (Mdifference = −183, SDdifference= 110) than for NACs (Mdifference = −107, SDdifference = 67), t(51) = −3.00, p = .004, d = 0.82.
Relationship between AAT Biases and Social Anxiety Symptoms
To elucidate the relationship between the approach response system and social anxiety symptoms, we correlated separate measures of approach for disgust and neutral faces, as well as the intolerance for approach of ambiguity index with LSAS scores. LSAS scores were correlated with approaching of neutral faces (r =.38, p = .005) such that higher levels of social anxiety were associated with slower response latencies in approaching neutral faces. The correlation between social anxiety and approach of disgust faces was not significant (r = .21, p = .131). Moreover, the intolerance for approach of ambiguity index was correlated with LSAS such that greater intolerance for approach of ambiguity (i.e., increasingly negative bias scores indicating longer response times to approach neutral faces compared to disgust faces) was associated with higher levels of social anxiety symptoms (r = −.42, p = .002).
Because our correlational analyses suggested that the intolerance for approach of ambiguity score was significantly associated with social anxiety symptoms, these results suggest that both neutral and disgust-related approach responses may contribute valuable information when combined into a single intolerance for approach of ambiguity index.
To assess the predictive utility of the intolerance for approach of ambiguity bias when accounting for trait anxiety (STAI-T) and depression (BDI-II), we also conducted a simultaneous multiple regression to predict LSAS scores with intolerance for approach of ambiguity bias, BDI and STAI-T as predictors. The intolerance for approach of ambiguity bias (β = −.19, t = −2.87, p = .006), trait anxiety (β = .52, t = 4.46, p < .001), and depression (β = .35, t = 3.03, p = .004) were all unique predictors of social anxiety symptoms, such that greater intolerance for approach of ambiguity (i.e., greater difficulty approaching neutral relative to nonambiguous disgust), higher levels of depression, and higher levels of trait anxiety, were all associated with higher levels of social anxiety.
Discussion
In the present study we found that individuals with SAD and NACs did not differ in implicit avoidance in response to neutral versus nonambiguous disgust facial expressions. When examining approach responses we found that the SAD group showed greater intolerance for approach of ambiguity compared to NACs. That is, individuals with SAD demonstrated greater difficulty approaching neutral faces relative to nonambiguous disgust faces. Moreover, the results of our regression analyses suggest that intolerance for approach of ambiguity predicted severity of social anxiety symptoms while controlling for the effects of trait anxiety and depression. Our findings are consistent with research (e.g., Najmi et al., 2010) showing that individuals with obsessive compulsive symptoms are characterized by greater difficulty approaching disorder-relevant stimuli in comparison to non-disorder relevant stimuli when compared to NACs. Together, these studies highlight the role of approach (pulling) but not avoidance (pushing) action tendencies for anxiety disorders and suggest that the pull AAT response may help elucidate the etiology and/or maintenance of such disorders. Such cross-diagnostic comparisons are particularly relevant to the National Institute of Mental Health Research Domain Criteria (RDoC) initiative (Insel et al., 2010) that seeks to identify constructs representative of mechanisms of psychopathology across diagnostic categories. For example, difficulties with implicit approach of disorder-relevant stimuli may be a useful construct for RDoC (e.g., see Approach Motivation construct (http://www.nimh.nih.gov/research-priorities/rdoc/positive-valence-systems-workshop-proceedings.shtml).
Our results provide further evidence that individuals with SAD may interpret “neutral” faces as ambiguous and therefore threatening (Lange et al., 2012; Yoon & Zinbarg, 2008). Previous research has shown that individuals with SAD rate non-valenced, non-facial stimuli as more threatening when primed by a neutral facial expression compared to when primed by a nonambiguous angry facial expression in an implicit task (Lange et al., 2012). Similarly, in the present study individuals with SAD displayed greater intolerance for ambiguity compared to NACs in the context of contrasting neutral facial expressions to nonambiguous disgust expressions assessed via an implicit AAT.
Moreover, related findings have been demonstrated in other studies examining interpretation of non-facial ambiguous information in SAD assessed via an implicit, or automatic, task. For example, Amir, Prouvost, and Kuckertz (2012) found that individuals with SAD were significantly slower to endorse benign (including neutral and positive) interpretations of ambiguous sentences compared to NACs, suggesting that SAD is characterized by difficulty in making benign interpretations in an automatic context. The authors did not find parallel findings for negative interpretations. Thus, individuals with SAD may demonstrate interpretation biases for multiple types (e.g., faces, sentences) of ambiguous stimuli (see Kuckertz & Amir, 2014 for a review).
Results from our study add to a growing body of literature suggesting that individuals with SAD may find neutral, or ambiguous, information to be threatening. Such findings have clinical implications for treatment of SAD. For example, exposure exercises may be best designed to maximize tolerance for ambiguous social situations. Therefore, such exercises may include approaching situations in which the outcome is ambiguous (i.e., patient is unsure how speech will be received by audience) rather than non-ambiguous rejection or disgust (i.e., patient is giving speech to an audience knowing that they will disagree with content). Treatment for SAD may also emphasize cognitive restructuring related to ambiguous situations (e.g., intolerance of uncertainty; Boelen & Reijntjes, 2009). We note that further research in this area will provide greater confidence in the clinical utility of these findings.
Our study has limitations. Our task included only neutral and nonambiguous disgust faces. However, inclusion of other types of nonambiguous threat faces (e.g., angry) as well as positive faces would allow us to further differentiate the role of intolerance for approach of ambiguity compared to multiple types of nonambiguous emotional expressions. Further, future studies should include explicit face ratings for all AAT facial stimuli in order to compare implicit versus explicit reactions to included stimuli. Such data would help elucidate the difference in responses in SAD to ambiguity when assessed across different levels of awareness.
Despite its limitations, the current study provides further support for the role of intolerance of ambiguity in SAD. Moreover, our results further highlight the importance of differentiating between approach and avoidance tendencies in the context of AATs (see Najmi et al., 2010), and suggest that in particular, implicit approach tendencies may be biased for disorder-relevant stimuli, thus representing a potential target for cross-diagnostic research initiatives and delineation of related constructs across various forms of psychopathology.
Acknowledgments
This project was supported by National Institutes of Health Grants R34MH077129, R34MH073004, and R01MH087623 awarded to Dr. Amir.
We wish to thank Marije van Essen for her assistance with an earlier version of this manuscript.
Footnotes
Effect sizes for t tests were calculated as follows: d = mean difference/pooled standard deviation.
Disclosure: Dr. Amir is part owner of a company that markets anxiety relief products.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Amir N, Beard C, Taylor CT, Klumpp H, Elias J, Burns M, Chen X. Attention training in individuals with generalized social phobia: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2009;77:961–973. doi: 10.1037/a0016685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amir N, Kuckertz JM, Najmi S. The effect of modifying automatic avoidance tendencies on overt avoidance behaviors. Emotion. 2013;13:478–484. doi: 10.1037/a0030443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amir N, Najmi S, Bomyea J, Burns M. Disgust and anger in social anxiety. International Journal of Cognitive Therapy. 2010;3:3–10. doi: 10.1521/ijct.2010.3.1.3. [DOI] [Google Scholar]
- Amir N, Prouvost C, Kuckertz JM. Lack of a benign interpretation bias in social anxiety disorder. Cognitive BehaviourTherapy. 2012;41:119–129. doi: 10.1080/16506073.2012.662655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amir N, Taylor CT. Interpretation training in individuals with generalized social anxiety disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2012;80:497–511. doi: 10.1037/a0026928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amir N, Weber G, Beard C, Bomyea J, Taylor CT. The effect of a single-session attention modification program on response to a public-speaking challenge in socially anxious individuals. Journal of Abnormal Psychology. 2008;117:860–868. doi: 10.1037/a0013445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck depression inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Baumeister RF, Vohs KD, Funder DC. Psychology as the science of self-reports and finger movements: Whatever happened to actual behavior? Perspectives on Psychological Science. 2007;2:396–403. doi: 10.1111/j.1745-6916.2007.00051.x. [DOI] [PubMed] [Google Scholar]
- Boelen PA, Reijntjes A. Intolerance of uncertainty and social anxiety. Journal of Anxiety Disorders. 2009;23:130–135. doi: 10.1016/j.janxdis.2008.04.007. [DOI] [PubMed] [Google Scholar]
- Feske U, Chambless DL. Cognitive behavioral versus exposure only treatment for social phobia: A meta-analysis. Behavior Therapy. 1995;4:695–720. doi: 10.1016/S0005-7894(05)80040-1. [DOI] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P) New York, NY: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Fresco DM, Coles ME, Heimberg RG, Liebowitz MR, Hami S, Stein MB, Goetz D. The Liebowitz Social Anxiety Scale: A comparison of the psychometric properties of self-report and clinician-administered formats. Psychological Medicine. 2001;31:1025–1035. doi: 10.1017/S0033291701004056. [DOI] [PubMed] [Google Scholar]
- Heuer K, Rinck M, Becker ES. Avoidance of emotional facial expressions in social anxiety: The Approach–Avoidance Task. BehaviourResearch and Therapy. 2007;45:2990–3001. doi: 10.1016/j.brat.2007.08.010. [DOI] [PubMed] [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Wang P. Research domain criteria (RDoC): Toward a new classification framework for research on mental disorders. American Journal of Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Kuckertz JM, Amir N. Cognitive biases in social anxiety disorder. In: Hofmann SG, DiBartolo PM, editors. Social Anxiety: Clinical, Developmental, and Social Perspectives. 3. San Diego, CA: Elsevier Academic Press; 2014. [Google Scholar]
- Kuckertz JM, Carmona AR, Chang SW, Piacentini J, Amir N. Factors predicting youth anxiety severity: Preliminary support for a standardized behavioral assessment of parental and youth avoidance behaviors. Journal of Cognitive Psychotherapy. 2015;29:212–229. doi: 10.1891/0889-8391.29.3.212. [DOI] [PubMed] [Google Scholar]
- Lange WG, Allart E, Keijsers GP, Rinck M, Becker ES. A neutral face is not neutral even if you have not seen it: Social anxiety disorder and affective priming with facial expressions. Cognitive BehaviourTherapy. 2012;41:108–118. doi: 10.1080/16506073.2012.666563. [DOI] [PubMed] [Google Scholar]
- Lange WG, Keijsers G, Becker ES, Rinck M. Social anxiety and evaluation of social crowds: Explicit and implicit measures. Behaviour Research and Therapy. 2008;46:932–943. doi: 10.1016/j.brat.2008.04.008. [DOI] [PubMed] [Google Scholar]
- Liebowitz MR. Social phobia. Modern Problems of Pharmacopsychiatry. 1987;22:141–173. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- Matsumoto D, Ekman P. Japanese and Caucasian facial expressions of emotion and neutral faces. Motivation and Emotion. 1988;13:143–157. doi: 10.1007/BF00992959. [DOI] [Google Scholar]
- Najmi S, Kuckertz JM, Amir N. Automatic avoidance tendencies in individuals with contamination-related obsessive-compulsive symptoms. BehaviourResearch and Therapy. 2010;48:1058–1062. doi: 10.1016/j.brat.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pishyar R, Harris LM, Menzies RG. Attentional bias for words and faces in social anxiety. Anxiety, Stress & Coping: An International Journal. 2004;17:23–36. doi: 10.1080/10615800310001601458. [DOI] [Google Scholar]
- Phaf RH, Mohr SE, Rotteveel M, Wicherts JM. Approach, avoidance, and affect: A meta-analysis of approach-avoidance tendencies in manual reaction time tasks. Frontiers in Psychology. 2014;5 doi: 10.3389/fpsyg.2014.00378. Article 378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roefs A, Huijding J, Smulders FT, MacLeod CM, de Jong PJ, Wiers RW, Jansen A. Implicit measures of association in psychopathology research. Psychological Bulletin. 2011;137:149. doi: 10.1037/a0021729. [DOI] [PubMed] [Google Scholar]
- Roelofs K, Putman P, Schouten S, Lange WG, Volman I, Rinck M. Gaze direction differentially affects avoidance tendencies to happy and angry faces in socially anxious individuals. BehaviourResearch and Therapy. 2010;48:290–294. doi: 10.1016/j.brat.2009.11.008. [DOI] [PubMed] [Google Scholar]
- Rozin P, Lowery L, Ebert R. Varieties of disgust faces and the structure of disgust. Journal of Personality and Social Psychology. 1994;66:870–881. doi: 10.1037/0022-3514.66.5.870. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Richey JA, Buckner JD, Timpano KR. Attention training for generalized social anxiety disorder. Journal of Abnormal Psychology. 2009;118:5–14. doi: 10.1037/a0013643. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press; Palo Alto, CA: 1983. [Google Scholar]
- Strack F, Deutsch R. Reflective and impulsive determinants of social behavior. Personality and Social Psychology Review. 2004;8:220–247. doi: 10.1207/s15327957pspr0803_1. [DOI] [PubMed] [Google Scholar]
- Voncken MJ, Rinck M, Deckers A, Lange WG. Anticipation of social interaction changes implicit approach-avoidance behavior of socially anxious individuals. Cognitive Therapy and Research. 2012;36:740–749. doi: 10.1007/s10608-011-9408-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon KL, Zinbarg RE. Interpreting neutral faces as threatening is a default mode for socially anxious individuals. Journal of Abnormal Psychology. 2008;117:680–685. doi: 10.1037/0021-843X.117.3.680. [DOI] [PubMed] [Google Scholar]