Abstract
Background
Acute stroke (AS) rates in patients over 90 years of age (very elderly) with atrial fibrillation (AF) in the United States (US) are not known. We assessed trends in hospitalizations for AS among very elderly with AF in the US from 2005 to 2014.
Methods
We used the nationwide inpatient sample (NIS) from the USA; 2005–2014. AF and AS diagnoses were abstracted using international classification of diseases, 9th Revision, clinical modification (ICD-9-CM) codes.
Results
From 2005 to 2014, 3,606,073 hospitalizations of very elderly with AF were reported. Of these, 188,948 hospitalizations (141,822 hospitalizations in women and 47,126 hospitalizations in men) had AS as the primary diagnosis. Age adjusted AS hospitalizations increased in the total cohort (3217/million in 2005 to 3871/million in 2014), in women (3540/million in 2005 to 4487/million in 2014) and in men (2490/million in 2005 to 3173/million in 2014) (P < 0.001). Anticoagulation rates increased in women (8% in 2005 to 19.9% in 2014) and in men (8.9% in 2005 to 21.6% in 2014). AS rates, though numerically lower than the total cohort, showed an increasing trend in anticoagulated patients as well (all anticoagulated patients: 212/million in 2005 to 513/million in 2014; anticoagulated women: 224/million in 2005 to 529/million in 2014, anticoagulated men: 184/million in 2005 to 518/million in 2014).
Conclusions
There is an increasing trend in AS hospitalizations among nonagenarians with AF in the US despite improving utilization of anticoagulants in this patient population. The etiologies driving this alarming trend are unclear and require further study.
Keywords: Anticoagulation, Atrial fibrillation, Nonagenarian, Stroke
1. Introduction
With improved healthcare and increasing longevity in the United States (US), the proportion of people surviving to > 90 years of age (very elderly) is steadily increasing.[1] Though accounting for only 0.02% of the US population, it is estimated that there will be over one million very elderly individuals in the USA by the end of this decade.[2] However, the US health care system may be suboptimally equipped to manage this vulnerable population because evidence based outcomes data with regards to chronic diseases such as non-valvular atrial fibrillation (AF) is rather scanty in this subgroup.
Stroke is a major complication of AF and is associated with enormous economic burden to the society. In the last decade, important changes have been proposed with regards to acute stroke (AS) prevention in patients with AF.[3] In order to enhance anticoagulation utilization in the elderly population, two points were allocated for age > 75 years in the currently recommended risk assessment—the CHA2DS2-VASc score.[4] Further, the use of direct oral anticoagulants has been recommended in appropriately selected elderly patients because of their favorable efficacy and safety profile compared to warfarin.[5] However, it is unclear if these recommendations are appropriately utilized in the real-world clinical care of the very elderly.
In this study, we analyzed the temporal trends in AS hospitalizations in very elderly patients with AF in the years 2005–2014. This information may help with assessing the current state of AS prevention outcomes and will potentially guide future efforts to reduce incidence of AS in this patient population.
2. Methods
We used the nationwide inpatient sample (NIS) for this analysis. NIS has been described in detail in other publications.[6],[7] In brief, the NIS is a nationally representative, largest, all-payer database of inpatient hospitalizations in the USA that is maintained by the Agency for Health Care Quality and Research (AHRQ). NIS comprises random 20% sample of all inpatient hospitalizations from 46 states in the USA from 1998 to 2014. Each observation in the NIS represents an individual hospitalization with a primary diagnosis, up to 24 secondary diagnoses, and up to 15 procedure codes. All discharge diagnoses and procedures were coded using the International Classification of Disease–9th clinical modification (ICD-9CM) codes.
Two different sampling strategies were followed in the assembly of the NIS data: (1) prior to 2012, the NIS included all discharges from a random sample of 20% of acute care hospitals in the USA, stratified by bed size, region and location; and (2) starting in 2012, the NIS included a random sample of 20% of discharges from all acute care hospitals in the USA. By this effort, the margin of error was reduced by 50% and national estimates decreased by 4.3%.[8] From 1998 to 2011, discharge weights are provided by the AHRQ after a validation process which are used to calculate national estimates. As recommended by the AHRQ,[9] in order to account for the differences in sampling strategy from 2012–2014, compared to before 2012, revised discharge weights termed “trend weights” are used for 2011 and all preceding years while computing national estimates in order to ensure comparability across years and to facilitate trends analysis from 1998–2014.[9]
2.1. Study population
University of Texas Health Science Center at Houston, Texas, USA reviewed the study protocol and the study was exempt from human subject research as it includes only de-identified, publically available data. For our analysis, we only used NIS data from 2005 to 2014. Similar to prior studies,[6],[10] ICD-9CM code 427.31 was used to identify hospitalizations involving patients with AF from the NIS database. Hospitalizations involving very elderly patients (age ≥ 90 years) with ICD-9CM code 427.31 in the primary or any secondary discharge diagnoses from 2005 to 2014 formed the study cohort. From the study cohort, we abstracted demographic data, payment type and comorbid diseases. It is to be noted that between 2012 and 2014, the NIS stopped reporting the exact age at the time of hospitalization for patients over 90 years of age. All hospitalizations of patients over 90 years were reported as a single value ‘90’. Hence, calculation of mean age in this time window 2012–2014 was not possible. We assessed stroke risk using CHA2DS2-VASc algorithm.[4] Charlson's comorbidity index (CCI) was calculated to quantify the comorbid disease burden of the study cohort.[11] ICD-9CM code V58.6; represents long term and current use of anticoagulants was used to identify hospitalizations involving anticoagulated patients with AF.
2.2. Outcomes assessed
The study outcome of interest was AS hospitalizations, defined as those hospitalizations involving the study cohort that were due to AS as the primary diagnosis and AF mentioned in any of the secondary diagnoses. Similar to prior investigations,[6],[10] ICD-9CM codes 433.xx, 434.xx and 436.xx were used to abstract AS hospitalizations from the study cohort. AS hospitalizations were expressed as hospitalization rates/million population, calculated by dividing total estimated number of AS hospitalizations of very elderly (aged > 90 years) for a specific year (numerator), by the US census population estimate of those older than 90 years for that year (denominator).[12] This multiplied by 1 million gives the AS hospitalization rates/million population. Similarly, we calculated from 2005–2014, AS hospitalizations/million population of anticoagulated patients with AF.
2.3. Statistical analysis
As per the recommendations of the AHRQ, we used survey analysis methods to account for clustering and stratification of patients for all continuous and categorical variables. We used Stata IC 13.0 (Stata-Corp, College Station, TX) and SAS 9.0 (SAS Institute Inc, Cary, North Carolina) software to perform statistical analysis. We used sampling weights to estimate trends and national estimates in order to account for the change in sampling design as recommended by the AHRQ.[9] Specifically, in order to account for the differences in sampling strategy from 2012–2014, compared to before 2012, revised discharge weights termed “trend weights” are used for 2011 and all preceding years while computing national estimates in order to ensure comparability across years and to facilitate trend analysis.[9] Similar to prior analyses[6],[7] trends in patient demographics, comorbid diseases, AS hospitalizations/million population, and AS hospitalizations involving anticoagulated patients with AF/million population were evaluated using the Cochrane Armitage test for categorical variables[13] and the Cuzick test for continuous variables.[14] Further, patient demographics, comorbid diseases and AS hospitalizations within each year for men and women were compared using student t test or Wilcoxon Rank sum test as appropriate for continuous variables and Chi-square test for categorical variables after adjusting for survey weights. P < 0.05 was considered statistically significant.
3. Results
From 2005 to 2014, 3,606,073 hospitalizations of the very elderly with AF were reported in the NIS. Table 1 details the trends in patient demographics, payment type, comorbid diseases, CHA2DS2-VASc score, CCI score and anticoagulation rates. Proportion of hospitalizations involving women were more than those involving men. Medicare/Medicaid paid for nearly 95% of hospitalizations 2005–2014. Proportion with hypertension, diabetes, coronary artery disease, prior stroke, peripheral vascular disease, renal failure, dementia and cancer increased; 2005–2014 (Table 1). Anticoagulation rates increased in women (8% in 2005 to 19.9% in 2014) as well as in men (8.9% in 2005 to 21.6% in 2014).
Table 1. Baseline characteristics of patients with AF with hospitalizations from 2005–2014.
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | P trend | |
| Total hospitalizations | 310,440 | 314,943 | 316,735 | 332044 | 337,476 | 358,266 | 413,589 | 397,760 | 408,250 | 416,570 | < 0.001 |
| Mean age, yrs | 92.5 | 92.6 | 92.6 | 92.6 | 92.7 | 92.6 | 92.6 | 90* | 90* | 90* | - |
| Female, % | 69.7% | 68.8% | 68.7% | 68.7% | 68.2% | 67.5% | 67.4% | 66.3% | 65.5% | 64.6% | < 0.001 |
| Race, % | |||||||||||
| White | 90.0% | 87.6% | 88.2% | 88.3% | 88.1% | 88.2% | 88.5% | 88.0% | 87.8% | 87.6% | < 0.001 |
| Black | 3.8% | 5.0% | 4.6% | 4.2% | 4.1% | 4.9% | 4.8% | 4.5% | 4.6% | 4.7% | 0.030 |
| Other | 6.2% | 7.4% | 7.2% | 7.5% | 7.8% | 6.9% | 6.6% | 7.5% | 7.6% | 7.7% | 0.001 |
| Payment type, % | |||||||||||
| Medicare/Medicaid | 95.7% | 95.8% | 94.4% | 93.9% | 94.2% | 94.5% | 95.2% | 95.7% | 95.2% | 95.1% | < 0.001 |
| Private insurance | 3.5% | 3.4% | 4.6% | 4.9% | 4.7% | 4.4% | 3.8% | 3.3% | 3.6% | 3.8% | < 0.001 |
| Self-pay/other | 0.8% | 0.8% | 1.0% | 1.2% | 1.1% | 1.1% | 1.0% | 1.0% | 1.2% | 1.1% | < 0.001 |
| AHRQ comorbidity measures (%) | |||||||||||
| Prior CHF | 41.5% | 40.6% | 40.4% | 38.1% | 37.9% | 38.1% | 38.5% | 39.2% | 39.6% | 39.7% | < 0.001 |
| Hypertension | 58.0% | 61.6% | 46.0% | 47.4% | 69.7% | 71.6% | 72.0% | 76.9% | 77.6% | 79.2% | < 0.001 |
| Diabetes mellitus | 14.7% | 15.4% | 16.7% | 17.9% | 18.2% | 19.0% | 19.4% | 21.2% | 21.5% | 22.4% | < 0.001 |
| Peripheral vascular disease | 5.5% | 5.9% | 6.1% | 6.7% | 6.9% | 7.0% | 7.5% | 9.0% | 9.4% | 9.7% | < 0.001 |
| Prior CAD | 32.5% | 32.8% | 34.2% | 35.4% | 35.7% | 35.8% | 36.5% | 40.0% | 39.4% | 40.1% | < 0.001 |
| Prior stroke | 7.6% | 7.8% | 7.9% | 8.5% | 8.6% | 8.5% | 8.5% | 8.9% | 9.2% | 9.3% | < 0.001 |
| Chronic lung disease | 22.5% | 22.7% | 22.8% | 21.3% | 21.8% | 21.8% | 21.7% | 23.5% | 22.1% | 22.4% | 0.177 |
| Renal failure | 5.1% | 12.3% | 20.6% | 20.9% | 24.0% | 24.0% | 27.6% | 31.1% | 31.1% | 31.4% | < 0.001 |
| Dementia | 4.4% | 4.0% | 3.5% | 3.9% | 3.7% | 3.3% | 3.1% | 3.0% | 3.3% | 3.7% | < 0.001 |
| Cancer | 4.1% | 4.0% | 4.2% | 4.2% | 4.2% | 3.6% | 4.2% | 4.3% | 4.3% | 4.6% | < 0.001 |
| Disease severity indices | |||||||||||
| CHA2DS2VASC score | 2.7 | 2.7 | 2.5 | 2.6 | 2.8 | 2.8 | 2.8 | 2.6 | 2.8 | 2.8 | < 0.001 |
| CCI ≥ 2 | 41.8 | 45.3 | 49.8 | 49.9 | 52.3 | 51.8 | 54.4 | 57.2 | 58.1 | 58.8 | < 0.001 |
| Anticoagulation rates | |||||||||||
| Women | 8.0 | 9.1 | 11.1 | 11.9 | 14.7 | 16.2 | 17.2 | 17.7 | 18.5 | 19.9 | < 0.001 |
| Men | 8.9 | 9.7 | 11.7 | 12.4 | 15.4 | 17.5 | 18.9 | 19.2 | 19.9 | 21.6 | < 0.001 |
*The database stopped mentioning specific age from 2012 to 2014. AF: atrial fibrillation; AHRQ: Agency for Health Care Quality and Research; CAD: cardiovascular diseases; CCI: Charlson's comorbidity index; CHF: congestive heart failure.
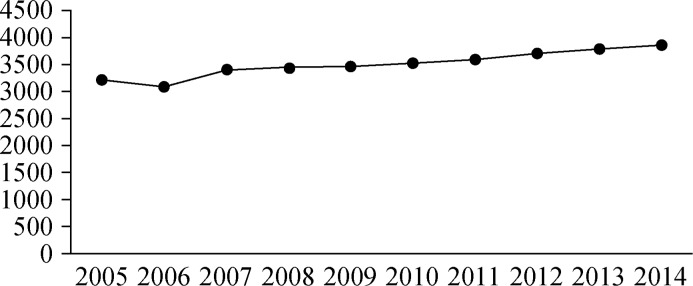
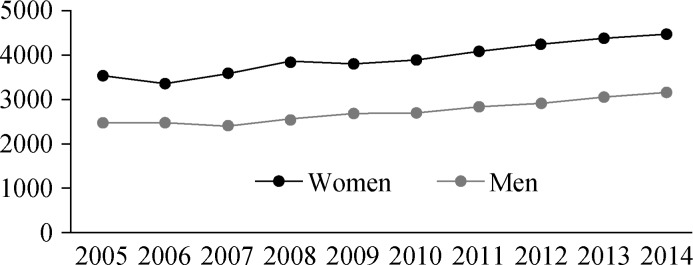
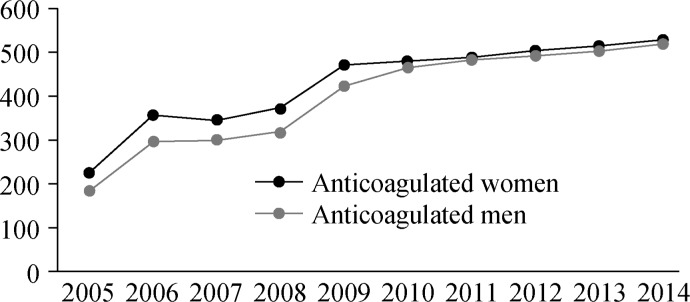
Table 2 details the national estimated numbers of AS hospitalizations. Table 3 details AS hospitalization rates/million population. In total, 188,948 hospitalizations (141,822 hospitalizations in women and 47,126 hospitalizations in men) had AS as the primary diagnosis. AS hospitalizations increased in the total cohort (3217/million in 2005 to 3871/million in 2014), in women (3540/million in 2005 to 4487/million in 2014) and in men (2490/million in 2005 to 3173/million in 2014) (P < 0.001) in the total cohort (Figure 1 & 2). AS rates in the anticoagulated patients, though numerically lower than the total cohort, showed an increasing trend as well (all anticoagulated patients: 212/million in 2005 to 513/million in 2014; anticoagulated women: 224/million in 2005 to 529/million in 2014, anticoagulated men: 184/million in 2005 to 518/million in 2014; Table 3, Figure 3).
Table 2. National estimates of stroke hospitalizations from 2005–2014.
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | P trend | |
| Total cohort | 15,100 | 15,084 | 15,550 | 17,897 | 17,991 | 19,477 | 21,523 | 21,699 | 21,788 | 22,839 | < 0.001 |
| Anticoagulated | 996 | 1,638 | 1,552 | 1,835 | 2,368 | 2,591 | 3,335 | 2,950 | 3,150 | 4,245 | < 0.001 |
| Women cohort | 11,504 | 11,315 | 12,399 | 13,631 | 13,498 | 14,567 | 16,207 | 16,154 | 15,938 | 16,609 | < 0.001 |
| Anticoagulated women | 730 | 1190 | 1266 | 1310 | 1,665 | 1,750 | 2,325 | 1,985 | 2,135 | 2,560 | < 0.001 |
| Men cohort | 3,596 | 3,769 | 3,875 | 4,266 | 4,493 | 4,910 | 5,316 | 5,545 | 5,850 | 6,230 | < 0.001 |
| Anticoagulated men | 266 | 448 | 510 | 525 | 703 | 841 | 1,010 | 965 | 1,015 | 1,665 | < 0.001 |
Table 3. Stroke hospitalizations/million population, 2005 – 2014.
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | P trend | |
| Total cohort | 3,217 | 3,099 | 3,400 | 3444 | 3,462 | 3,520 | 3,601 | 3,712 | 3,796 | 3,871 | < 0.001 |
| Anticoagulated | 212 | 336 | 307 | 353 | 455 | 468 | 477 | 489 | 496 | 513 | < 0.001 |
| Women cohort | 3,540 | 3,380 | 3,597 | 3,858 | 3,820 | 3,909 | 4,100 | 4,257 | 4,399 | 4,487 | < 0.001 |
| Anticoagulated women | 224 | 355 | 345 | 370 | 471 | 477 | 489 | 501 | 514 | 529 | < 0.001 |
| Men cohort | 2,490 | 2,482 | 2,432 | 2,565 | 2,702 | 2,716 | 2,855 | 2,930 | 3,079 | 3,173 | < 0.001 |
| Anticoagulated men | 184 | 295 | 300 | 315 | 422 | 465 | 481 | 490 | 503 | 518 | < 0.001 |
Figure 1. Acute stroke in the total cohort.
Figure 2. Sex specific stroke rates.
Figure 3. Sex specific stroke rates in anticoagulated patients.
A distinct sex gap was noted in the AS rates with women experiencing higher rates of AS compared to men in the total cohort (Figure 2). However, in anticoagulated patients (Figure 3) this sex gap in AS risk, though persisted 2005–2009, significantly attenuated from 2010–2014.
4. Discussion
In our large sample, nationally representative analysis using the NIS database we found an increasing trend in AS hospitalizations of the very elderly with AF. This was true in men as well as in women. Although, anticoagulation rates consistently increased in both sexes 2005–2014, AS hospitalizations increased in the anticoagulated patients as well in this 10 year period.
Data on AS trends in the very elderly are limited. Although prior analyses have assessed AS trends in patients with AF in the USA,[15],[16] data specific to the very elderly; aged > 90 years were not mentioned in these reports. To the best of our knowledge, the present study appears to be the first to specifically address this age group. The reasons for increasing rate of hospitalizations for AS observed in our analysis are unclear. One of the potential explanations could be growing prevalence of comorbidities such as hypertension, diabetes, coronary artery disease, prior stroke, peripheral vascular disease, and renal failure in the recent years (Table 1). All of them are well-recognized risk factors for stroke in AF patients. With advancement of care, progressively sicker patients are able to survive to more advanced ages.
Although the use of anticoagulants has steadily increased over the years, the rates still remain sub-optimal (19.9% in women and 21.6% in men in 2014). Inadequate anticoagulation is a problem in all age groups with AF. In a recent analysis of 94,474 AF patients with a history of AS, 83.6% were not receiving anticoagulation.[17] In another small retrospective cohort analysis from the US, Marti, et al.,[18] reported that none of 39 very elderly (age > 90 years) AF patients with a prior history of AS were receiving anticoagulation. Our study shows that the utilization rate of anticoagulation therapy in the very elderly AF patients remains relatively low. One of the most commonly cited reasons for such poor adherence to the AF anticoagulation guidelines is physician perceived fear of hemorrhagic complications in this age group.[19],[20] However, risk benefit analysis has shown that, in appropriately selected very elderly patients, AS risk reduction conferred by anticoagulation may potentially outweigh the hemorrhagic risk.[19],[21]
The increase in AS rates over the recent years despite better utilization of anticoagulation observed in our study appears to be counterintuitive. However, the NIS database does not provide data about stroke etiology and severity as well as quality and type of anticoagulation at the time of AS hospitalizations. Thus, our data do not allow drawing a firm conclusion about efficacy of anticoagulation in the very elderly patient population. Although AS rates in anticoagulated AF patients were numerically lower than those in the total cohort (3871/million in the total cohort and 513/million in the anticoagulated patients in 2014) suggesting protective effect of anticoagulation in this age group, the trend analysis used in our study does not allow a formal statistical comparison between these two distinctive cohorts.
Further, we noted a sex gap in AS rates; women experienced higher rates of AS compared to men in the total cohort. A higher risk of AF related AS in women comparing to men has been previously reported.[22]–[24] This has been attributed to increased systemic inflammation and pro-coagulants,[25] as well as larger left atrial volume and lower left atrial mechanics[26] in women (particularly in older women) with AF. Differential anticoagulation rates between sexes have also been reported as a potential reason for higher risk of stroke in female AF patients. Bhave, et al.,[27] and Hsu, et al.,[28] showed that females receive lower rates of anticoagulation compared to their male counterparts. In our study, we noted slightly higher utilization of anticoagulation in men compared to women (Table 1).
4.1. Limitations
Although the NIS database is large and nationally representative, it lacks granularity with regards to AF type, quality of anticoagulation, as well as type and severity of stroke. In addition, this database does not provide information on readmissions and recurrent strokes. ICD-9CM code based data abstract is prone to coding errors. Finally, patient level data were not available. This limited our ability to assess the effect of patient level variables on AS outcomes.
4.2. Conclusions
There is an increasing trend in AS hospitalizations among nonagenarians with AF in the US in the recent years despite improving utilization of anticoagulants in this patient population. The reasons driving this alarming trend are unclear and require further study.
Footnotes
This article is part of a Special Issue “Arrhythmia management in elderly patients”.
Guest Editors: Evgeny N Mikhaylov, Tamas Szili-Torok and Dmitry S Lebedev
References
- 1.Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, et al. Inequalities in life expectancy among us counties, 1980 to 2014: temporal trends and key drivers. JAMA Intern Med. Published Online First: May 2017. DOI: 10.1001/jamainternmed.2017.0918. [DOI] [PMC free article] [PubMed]
- 2.Kincel B. The centenarian population: 2007–2011. [accessed June 21, 2016]. https://www.census.gov/prod/2014pubs/acsbr12-18.pdf.
- 3.January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association task force on practice guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64:E1–E76. doi: 10.1016/j.jacc.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 4.Lip GY, Nieuwlaat R, Pisters R, et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137:263–272. doi: 10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- 5.Nielsen PB, Skjøth F, Søgaard M, et al. Effectiveness and safety of reduced dose non-vitamin K antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ. 2017;356:j510. doi: 10.1136/bmj.j510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel NJ, Deshmukh A, Pant S, et al. Contemporary trends of hospitalization for atrial fibrillation in the United States, 2000 through 2010: implications for healthcare planning. Circulation. 2014;129:2371–2379. doi: 10.1161/CIRCULATIONAHA.114.008201. [DOI] [PubMed] [Google Scholar]
- 7.Khera R, Cram P, Lu X, et al. Trends in the use of percutaneous ventricular assist devices: analysis of national inpatient sample data, 2007 through 2012. JAMA Intern Med. 2015;175:941–950. doi: 10.1001/jamainternmed.2014.7856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Houchens RLRD, Elixhauser A, Jiang J. [accessed April 20, 2017]. Https://www.hcupus.ahrq.gov/db/nation/nis/reports/NISRedesignFinalReport040914.pdf.
- 9.Houchens RL, Ross D, Elixhauser A. Using the HCUP national inpatient sample to estimate trends. 2015. [accessed April 20, 2017]. HCUP Methods Series Report # 2006-05. http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp.
- 10.Freeman JV, Wang Y, Akar J, et al. National Trends in Atrial Fibrillation Hospitalization, Readmission, and Mortality for Medicare Beneficiaries, 1999–2013. Circulation. 2017;135:1227–1239. doi: 10.1161/CIRCULATIONAHA.116.022388. [DOI] [PubMed] [Google Scholar]
- 11.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 12.Annual estimates of the resident population by sex and selected age groups for the United States: April 1, 2000 to July 1, 2015 (nc-est2009-02) [accessed April 20, 2017]. Http://www.census.gov/popest/national/asrh/NC-EST2009-sa.html.
- 13.Armitage P. Tests for linear trends in proportions and frequencies. Biometrics. 1995;11:375–386. [Google Scholar]
- 14.Cuzick J. A wilcoxon-type test for trend. Stat Med. 1985;4:87–90. doi: 10.1002/sim.4780040112. [DOI] [PubMed] [Google Scholar]
- 15.Shroff GR, Solid CA, Herzog CA. Atrial fibrillation, stroke, and anticoagulation in medicare beneficiaries: trends by age, sex, and race, 1992–2010. J Am Heart Assoc. 2014;3:e000756. doi: 10.1161/JAHA.113.000756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chamberlain AM, Brown RD, Jr, Alonso A, et al. No decline in the risk of stroke following incident atrial fibrillation since 2000 in the community: a concerning trend. J Am Heart Assoc. 2016:e003408. doi: 10.1161/JAHA.116.003408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xian Y, O'Brien EC, Liang L, et al. Association of preceding antithrombotic treatment with acute ischemic stroke severity and in-hospital outcomes among patients with atrial fibrillation. JAMA. 2017;317:1057–1067. doi: 10.1001/jama.2017.1371. [DOI] [PubMed] [Google Scholar]
- 18.Marti J, Anton E. Stroke in the very elderly. Stroke. 2005;36:705–706. doi: 10.1161/01.str.0000157947.89347.d8. [DOI] [PubMed] [Google Scholar]
- 19.Lepor NE. Changing the guard in long-term anticoagulation: clinical and economic implications. Rev Cardiovasc Med. 2004;5:S22–S29. [PubMed] [Google Scholar]
- 20.Rahimi AR, Wrights B, Akhondi H, et al. Clinical correlation between effective anticoagulants and risk of stroke: are we using evidence-based strategies? South Med J. 2004;97:924–931. doi: 10.1097/01.SMJ.0000129930.40928.3F. [DOI] [PubMed] [Google Scholar]
- 21.George E, Leon F. Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation. Analysis of pooled data from five randomized controlled trials. Arch Intern Med. 1994;154:1449–1457. [PubMed] [Google Scholar]
- 22.Friberg L, Benson L, Rosenqvist M, et al. Assessment of female sex as a risk factor in atrial fibrillation in Sweden: nationwide retrospective cohort study. BMJ. 2012;344:e3522. doi: 10.1136/bmj.e3522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Avgil Tsadok M, Jackevicius CA, et al. Sex differences in stroke risk among older patients with recently diagnosed atrial fibrillation. JAMA. 2012;307:1952–1958. doi: 10.1001/jama.2012.3490. [DOI] [PubMed] [Google Scholar]
- 24.Fang MC, Singer DE, Chang Y, et al. Gender differences in the risk of ischemic stroke and peripheral embolism in atrial fibrillation: the Anticoagulation and Risk factors In Atrial fibrillation (ATRIA) study. Circulation. 2005;112:1687–1691. doi: 10.1161/CIRCULATIONAHA.105.553438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cove CL, Albert CM, Andreotti F, et al. Female sex as an independent risk factor for stroke in atrial fibrillation: possible mechanisms. Thromb Haemost. 2014;111:385–391. doi: 10.1160/TH13-04-0347. [DOI] [PubMed] [Google Scholar]
- 26.Yoshida K, Obokata M, Kurosawa K, et al. Effect of sex differences on the association between stroke risk and left atrial anatomy or mechanics in patients with atrial fibrillation. Circ Cardiovasc Imaging. 2016;9:e004999. doi: 10.1161/CIRCIMAGING.116.004999. [DOI] [PubMed] [Google Scholar]
- 27.Bhave PD, Lu X, Girotra S, et al. Race and sex-related differences in care for patients newly diagnosed with atrial fibrillation. Heart Rhythm. 2015;12:1406–1412. doi: 10.1016/j.hrthm.2015.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hsu JC, Maddox TM, Kennedy K, et al. Aspirin instead of oral anticoagulant prescription in atrial fibrillation patients at risk for stroke. J Am Coll Cardiol. 2016;67:2913–2923. doi: 10.1016/j.jacc.2016.03.581. [DOI] [PubMed] [Google Scholar]
- 29.Poli D, Antonucci E, Grifoni E, et al. Gender differences in stroke risk of atrial fibrillation patients on oral anticoagulant treatment. Thromb Haemost. 2009;101:938–942. [PubMed] [Google Scholar]