Abstract
Objective
To assess the impact of the upper gastrointestinal ‘Be Clear on Cancer’ campaign launched by Public Health England between January and February 2015 on open-access gastroscopy referrals, incidence of target diagnoses (oesophagogastric cancer and Barrett’s oesophagus), cancer staging at presentation, 1-year survival and cost per additional diagnosis.
Design
We performed a retrospective study of patients referred for 2-week-wait (2WW), open-access endoscopy 3 months following the campaign with diagnoses, endoscopic findings, staging and 12-month survival compared with data from corresponding months in 2014.
Setting
Three adjacent National Health Service trusts in the West Midlands with a combined population of 1.34 million in 2015.
Results
2WW open-access referrals increased by 48% (95% CI 1.35 to 1.61, p<0.001). The proportion of target diagnoses fell from 6.7% to 6.1% (p=0.62). There were no significant overall increases in target diagnoses (OR 1.35, 95% CI 0.95 to 1.92, p=0.11) or cancer (OR 1.30, 95% CI 0.80 to 2.07, p=0.36). There was no change in tumour, node, metastasis (TNM) staging for oesophageal or gastric cancer. Overall 1-year survival did not alter significantly (HR 1.10, 95% CI 0.56 to 2.19, p=0.76).
Discussion
The ‘Be Clear on Cancer’ campaign led to a 48% increase in demand for 2WW gastroscopies but did not significantly affect the incidence of target diagnoses, cancer staging or 1-year survival.
Keywords: be clear on cancer, screening, upper gastrointestinal cancer, barrett’s oesophagus
Introduction
The upper gastrointestinal (GI) ‘Be Clear on Cancer’ (BCOC) campaign was launched by Public Health England (PHE) to raise awareness of gastro-oesophageal cancers, and ran for 4 weeks from 26 January to 22 February 2015.1
The key messages advertised on television, radio and press were ‘Having heartburn, most days, for 3 weeks or more, could be a sign of cancer – tell your doctor’ and ‘Food sticking when you swallow could be a sign of cancer – tell your doctor’.1 The campaign was designed to raise awareness of warning symptoms of gastro-oesophageal cancer, that is, dyspepsia and dysphagia. The aim of the campaign was to promote symptom awareness, diagnose cancers at an earlier stage, and to ultimately improve cancer survival in line with European counterparts.2 The campaign estimated that out of 10 200 deaths from oesophagogastric cancers in England annually, 950 deaths could be avoided if survival rates were to match the best in Europe, and early diagnosis was felt to be critically important in achieving better survival.2
A previous regional pilot study undertaken between February and March of 2014 within the North England Strategic Clinical Network showed a significant uplift in spontaneous awareness of cancer symptoms.2 There had been a 52% increase in urgent general practitioner referrals for suspected upper GI cancer, compared with 17% in the control area, and a 29% increase in the proportion of upper GI cancers diagnosed via a 2-week-wait (2WW) pathway in the 60–69 age group.2 Results from seven local pilots involving 25 primary care trusts (PCTs) in England in 2012 showed a 26% increase in 2WW referrals and a 20% increase in oesophageal cancers diagnosed following a 2WW referral, compared with 3% in control areas (all other PCTs in England).3 We have now carried out a detailed analysis of the BCOC campaign outcomes in three geographically adjacent large acute trusts.
Aims and objectives
We assessed the impact of the 2015 BCOC campaign on the following outcomes in the 3-month period after the campaign: (1) 2WW open-access gastroscopy referrals, (2) incidence of target diagnoses (oesophagogastric cancer and Barrett’s oesophagus), (3) cancer stage at diagnosis and (4) 12-month survival. An additional exploratory analysis of costs was performed.
Methods
We performed a retrospective study using pooled data from three National Health Service (NHS) trusts from the West Midlands. The trusts included the Royal Wolverhampton NHS Trust, Dudley Group Hospitals NHS Foundation Trust, and Sandwell and West Birmingham, with a combined population of 1.22 million in 2014 and 1.34 million in 2015 (following expansion of Royal Wolverhampton NHS Trust to include part of the mid-Staffs catchment population). Patients referred for 2WW open-access endoscopy for 3 months following the start of the campaign (1 February to 30 April 2015) and for the same period in the preceding year (2014) were identified from cancer services databases. Secondary-care gastroscopy referrals and patients with known pre-existing diagnoses were excluded from the study. All relevant endoscopy reports were reviewed. Target diagnoses included oesophageal and gastric cancers, and Barrett’s oesophagus owing to its premalignant potential. Cases of Barrett’s oesophagus were identified based on endoscopic diagnoses and confirmation of intestinal metaplasia (International Statistical Classification of Diseases (ICD-10) code of K22.7), whereas oesophageal and gastric cancers were identified from ICD-10 codes of C15 and C16, respectively. Barrett’s dysplasia was graded based on opinions from two expert histopathologists following multidisciplinary team discussion. Pathology reports were reviewed and, for confirmed cancer cases, staging information from CT and endoscopic ultrasound investigations was recorded. Mortality data were retrieved from individual cancer services department via the Somerset Cancer Register.
Endoscopic and histological findings, cancer staging and 12-month survival in cancer cases were then compared with data from corresponding months in 2014. We selected the same period from 2014 as our comparison group in order to minimise the effect of any seasonal variation in referral rates. Adjustments for the higher population in 2015 were made by extrapolating total numbers from 2014 upwards to match the total population in 2015. ORs of 2WW referrals and target diagnoses were obtained from incidence rate comparisons (per 100 000 population per year). Analyses were performed using SPSS V.23. Pearson’s χ2 test was used for incidence rate comparisons, Fisher’s exact for comparisons between groups and Mann-Whitney U test for age comparisons. Kaplan-Meier analyses were performed to study survival, with HRs estimated using the log-rank method. Two-tailed p values were considered significant if <0.05. Cost estimates were based on the 2014/2015 NHS tariffs.4
Results
2WW open-access referrals
1266 2WW open-access referrals were received between February and April 2015, compared with 777 referrals in the same period in 2014. After population adjustment, the numbers of gastroscopy performed per population rose by 48% (95% CI 1.35 to 1.62, p<0.001) (figure 1).
Figure 1.

Impact of the campaign on 2-week-wait open-access referrals across the three trusts compared with the same period in the preceding year.
Target diagnoses
We compared the incidence of oesophagogastric cancer and Barrett’s oesophagus in each of the NHS trusts (figure 2). There were no significant increases in incidence within each trust. Overall, the incidence of oesophagogastric cancer and Barrett’s oesophagus increased by 30% (95% CI 0.80 to 2.07, p=0.36) and 42% (95% CI 0.84 to 2.40, p=0.23), respectively. Although the incidence of combined target diagnoses increased by 35%, this was also not statistically significant (95% CI 0.95 to 1.92, p=0.11) (table 1). Only one case of Barrett’s oesophagus with high-grade dysplasia was detected within the 2015 cohort, which harboured intramucosal adenocarcinoma in the resection specimen. Overall, the incidence of target diagnoses as a proportion of 2WW referrals did not increase (6.1% in 2015 vs 6.9% in 2014; OR 0.9, 95% CI 0.63 to 1.31, p=0.62). The median age (and IQR) at cancer diagnosis in 2014 and 2015 were 75.0 (13.5) and 73.9 (11.0), respectively (p=0.41).
Figure 2.
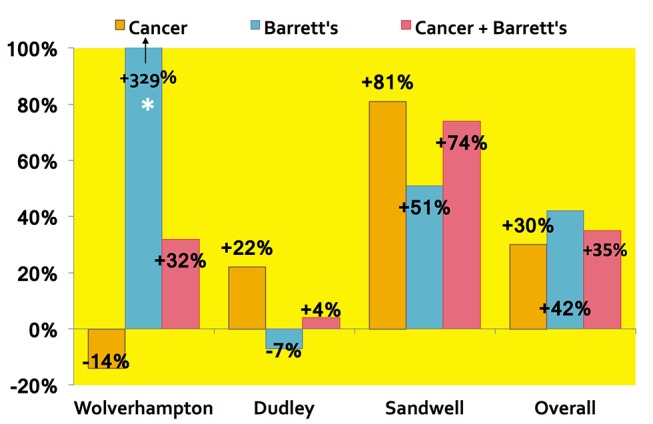
Graph showing changes in incidence of Barrett’s oesophagus (BO) and gastro-oesophageal cancer diagnoses in the three trusts and the overall result for 2015 compared with 2014.
Table 1.
Comparisons of referrals and target diagnoses before and after the Be Clear on Cancer campaign
| Population | 2014 | 2015 | OR* (p value) | 95% CI | |
| 1 224 000 | 1 345 000 | ||||
| Referrals | 777 | 1260 | 1.48 (p<0.001) | 1.35 to 1.61 | |
| Barrett’s oesophagus | N (% of referrals) | 23 (3.0%) | 36 (2.9%) | ||
| Incidence (per 100 000/year) | 7.5 | 10.7 | 1.42 (p=0.23) | 0.84 to 2.40 | |
| Cancers | N (% of referrals) | 29 (3.7%) | 41 (3.3%) | ||
| Incidence (per 100 000/year) | 9.5 | 12.2 | 1.30 (p=0.36) | 0.80 to 2.07 | |
| Target diagnoses | N (% of referrals) | 52 (6.7%) | 77 (6.1%) | ||
| Incidence (per 100 000/year) | 17.0 | 22.9 | 1.35 (p=0.11) | 0.95 to 1.92 | |
*ORs refer to incidence rates in 2015 versus 2014.
Cancer staging
We assessed whether the campaign had an impact on earlier presentation of oesophagogastric cancer by arbitrarily characterising early presentation based on tumour bulk (≤T2 disease vs >T2) and tumour localisation based on the absence of nodal/metastatic involvement (N0/M0 vs >N0/M0). Three patients in 2014 and four in 2015 were excluded due to inadequate staging information. One patient in 2014 had T staging but had inconclusive N/M staging (T4NxMx). Following the campaign, there were no significant differences in the stage of presentation of oesophageal or gastric tumour (table 2). As shown in table 2, patients with gastric cancer appeared to present at a more advanced stage—all patients had presented with >T2 disease, with only one patient in both years presenting with localised disease. Four of 29 patients (13.8%) underwent curative resection in 2014 compared with 9/41 (22.0%) in 2015 (OR 1.76, 95% CI 0.48 to 6.38, p=0.53).
Table 2.
Comparison of oesophageal and gastric cancer staging at presentation in 2014 and 2015
| ≤T2 disease | >T2 disease | |||
| Oesophageal | Gastric | Oesophageal | Gastric | |
| 2014 | 4 | 0 | 15 | 8 |
| 2015 | 8 | 0 | 19 | 10 |
| OR (≤T2 oesophageal cancer): 1.58, 95% CI 0.40 to 6.26, p=0.73 OR (≤T2 gastric cancer): N/A, p=1.00 | ||||
| N0/M0 | >N0/M0 | |||
| Oesophageal | Gastric | Oesophageal | Gastric | |
| 2014 | 4 | 1 | 14 | 7 |
| 2015 | 10 | 1 | 17 | 9 |
| OR (localised oesophageal cancer): 2.06, 95% CI 0.53 to 8.01, p=0.34 OR (localised gastric cancer): 0.78, 95% CI 0.04 to 14.75, p=1.00 | ||||
N/A, not applicable.
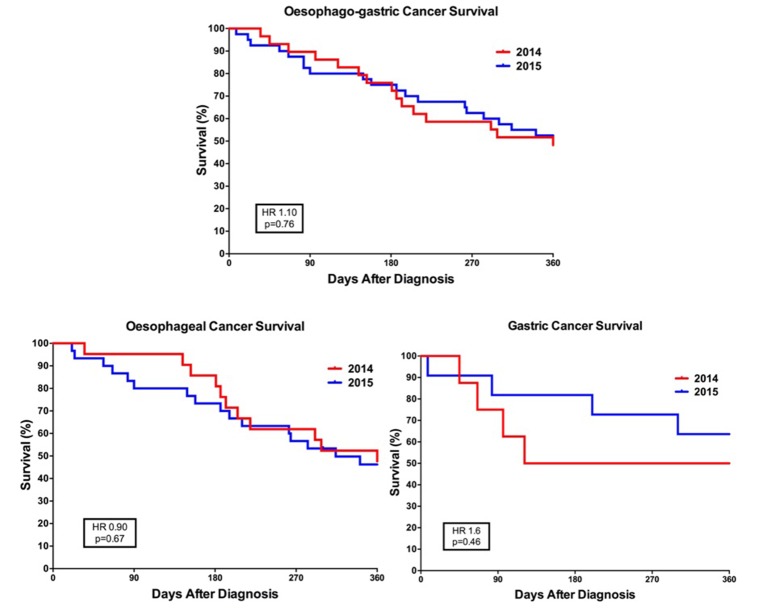
Cancer survival
Kaplan-Meier survival curves following cancer diagnoses are shown in figure 3. Overall 12-month survival rates were 48.3% (14/29) in 2014 and 53.6% (22/41) in 2015, with an absolute difference of 5.3% (HR 1.10; 95% CI 0.56 to 2.19, p=0.76). When stratified by disease location, 12-month survival for oesophageal cancer was 46.2% (13/30) in 2015 vs 47.6% (10/21) in 2014. For gastric cancer, the corresponding figures were 63.6% (7/11) vs 50.0% (4/8), respectively. There were no statistically significant differences observed.
Figure 3.
Kaplan-Meier curves illustrating 1-year survival of oesophagogastric cancers, gastric cancer and oesophageal cancer in 2014 and 2015 cohorts.
Cost per additional diagnosis
Four hundred and eighty-three additional gastroscopies were performed in the study period between 2014 and 2015. With an estimated cost of £344 per gastroscopy,4 this amounted to £166K in additional endoscopy costs (approximately £12K per 100K population). Based on 25 additional target diagnoses (12 cancers and 13 cases of Barrett’s oesophagus), the costs for an additional cancer diagnosis and target diagnosis were £13 800 and £6645 per case, respectively. These figures do not include the costs of the campaign, consultation costs in primary or secondary care, or administrative costs (eg, biopsies).
Discussion
The BCOC campaign has been successful in raising awareness of gastro-oesophageal cancer symptoms, which was reflected by the uplift in demand for open-access endoscopy by 48% across the West Midlands. This is important as oesophagogastric cancer has not been well-publicised compared with other cancer campaigns.5 A regional study in 2010 showed that only 10% of the public had appreciated dysphagia as a possible symptom of oesophagogastric cancer.5 In contrast, 71% of patients would seek medical advice after discovering a breast lump.5 Data from a previous BCOC pilot had shown an increase in oesophagogastric cancer symptom awareness.3 However, the three trusts investigated in our study are located in the top 6 regions with the highest indices of deprivation in England,6 and as such it remains unclear whether the results from our region would be reproducible on a national scale.
Despite this, we have not demonstrated a statistically significant effect of the campaign on increasing either the incidence rate of Barrett’s oesophagus, oesophagogastric cancer or the combination of the two. Diagnosis of Barrett’s oesophagus was included as an outcome measure in view of its premalignant potential and the recognition of an increased diagnosis rate from previous pilots.3 Detection of high-grade dysplasia or intramucosal adenocarcinoma in the context of Barrett’s oesophagus is important as these lesions may be amenable to curative endoscopic resection and ablation.7 However, only one case of intramucosal adenocarcinoma was detected in the 2015 cohort, which was not amenable to endotherapy.
In terms of cancer detection, there was a signal suggesting that the campaign had led to an increase in detection of smaller oesophageal tumours (OR 1.58), non-disseminated oesophageal cancer (OR 2.06) and more patients receiving curative surgery (OR 1.76), although this was not significant. There was also a marginal and non-significant increase in 12-month survival after the campaign (53.6% vs 48.3%). Our results appear to be more favourable in comparison with national 12-month survival data for oesophageal (41.9%) and gastric cancer (41.8%).8 9 This may have been due to the exclusion of emergency presentations, which tend to be associated with poorer outcomes. If our 12-month survival figures had been significant, then based on an estimated annual incidence of 12 900 cases of oesophagogastric cancers in England, the absolute survival difference of 5.3% would reflect an increase in 12-month survival of 683 cases per year, which would still fall short of the campaign’s intended benchmark of 950 fewer deaths per year in England, even if the BCOC’s campaign impact was sustainable. However, further follow-up will be necessary to identify whether any differences in longer term survival become apparent.
Our study does have limitations. First, we did not perform detailed stratification of our 2WW referral cohort, for instance, with age and sex. Second, target diagnoses within individual trusts were small, which may have accounted for the heterogeneity in numbers between sites, especially with diagnoses of Barrett’s oesophagus. Although ORs for studied outcomes did suggest an effect from the campaign, our study may not have been sufficiently powered to reach statistical significance, whereas a larger study may be helpful to validate our findings. Third, we acknowledge that our cost estimates are crude and not a cost-effectiveness analysis. Fourth, we assumed that the campaign would have a degree of durability; we had selected 3 months for postcampaign follow-up, based on data from a pilot site (Dudley Group Hospitals NHS Trust) of 2WW endoscopy referral rates reverting back to baseline between April and May 2015. However, owing to PHE intervention in pockets of the North of England, the choice of baseline months in 2014 may not have denoted the lowest levels of awareness. Furthermore, it is unknown whether or how it would be possible to sustain the increased public awareness of upper GI malignancy that was evident during the relatively brief but intense campaign period.
Other authors have examined the impact of the same campaign in their own catchment populations, although methodology and comparison populations have differed between the studies and all have analysed smaller target populations than our own.10–12 In line with our findings, these studies have shown significant increases in demand for 2WW endoscopy referrals (36.5%–88.6%), without an increase in cancer diagnoses.10 11 While our limitations are likely to be addressed in the nationwide data from PHE, we welcome additional analyses including the effects of the campaign on outpatient referrals, trends in 2016, demographic and geographical differences in uptake and diagnoses, and longer term and multivariate survival analyses, in addition to formal cost-effectiveness projections. Identifying the regions and patient characteristics that may benefit most from such an intervention may aid the design and population targeting of future public health campaigns.
In conclusion, the upper gastrointestinal BCOC campaign increased endoscopy demand by 48% over a 3-month period in our catchment population, but without a significant increase in the overall incidence of Barrett’s and oesophagogastric cancer. Although the ORs appear promising for earlier cancer staging at presentation and 12-month survival, this was not statistically significant. Nationwide results from the campaign are eagerly anticipated.
Significant of this study.
What is already known on this topic?
The Be Clear on Cancer (BCOC) is a series of public health campaigns aimed to increase awareness of cancer diagnoses.
Previous pilot studies have shown increases in 2-week-wait (2WW) endoscopy referrals, but its impact on diagnoses is unclear.
What this study adds?
The upper gastrointestinal BCOC campaign increased regional 2WW endoscopy referrals by 48%.
There were no significant increases in target diagnoses (Barrett’s oesophagus or upper gastrointestinal cancer), cancer staging or 12-month survival.
The costs per additional cancer diagnosis and target diagnosis were £13 800 and £6645, respectively.
How might it impact on clinical practice in the foreseeable future?
Different strategies may need to be sought in order to detect oesophagogastric cancer at earlier stages.
Acknowledgments
We would like to thank James Hodson from the Institute of Translational Medicine, University Hospitals Birmingham, for his help with validating statistical outputs.
Footnotes
Contributors: All authors contributed equally.
Competing interests: None declared.
Patient consent: No specific use of patients.
Provenance and peer review: Not commissioned; externally peer reviewed.
Correction notice: This article has been corrected since it published Online First. The results in the abstract has been corrected.
References
- 1.Cancer Research UK. Oesophago-gastric cancers campaign: overview. http://www.cancerresearchuk.org/health-professional/early-diagnosis-activities/be-clear-on-cancer/oesophago-gastric-cancers-campaign/campaign-overview (accessed 24 Oct 2016).
- 2.Cancer Research UK. Oesophago-gastric Campaign: information to help you prepare. https://www.cancerresearchuk.org/sites/default/files/cruk_bcoc_ogover_final.pdf (accessed 24 Oct 2016).
- 3.Cancer Research UK. Improving the early diagnosis of oesophago-gastric cancers; findings from seven local be clear on Cancer pilots. http://www.cancerresearchuk.org/sites/default/files/poster_og.pdf (accessed 24 Oct 2016).
- 4.Monitor and NHS England. The NHS payment system: documents and guidance - NHS national tariff payment system for 2014/15. https://www.gov.uk/government/consultations/nhs-national-tariff-payment-system-for-2014-to-2015 (accessed 24 Oct 2016).
- 5.Tentzeris V, Lake B, Cherian T, et al. Poor awareness of symptoms of oesophageal Cancer. Interact Cardiovasc Thorac Surg 2011;12:32–4. doi:10.1510/icvts.2010.247213 [DOI] [PubMed] [Google Scholar]
- 6.Department for Communities and Local Government. English indices of deprivation. 2015. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/465791/English_Indices_of_Deprivation_2015_-_Statistical_Release.pdf (accessed 26 Oct 2016).
- 7.Fitzgerald RC, di Pietro M, Ragunath K, et al. British society of Gastroenterology guidelines on the diagnosis and management of Barrett’s oesophagus. Gut 2014;63:7–42. doi:10.1136/gutjnl-2013-305372 [DOI] [PubMed] [Google Scholar]
- 8.Cancer Research UK. Oesophageal cancer survival statistics. http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/oesophageal-cancer/survival (accessed 26 Oct 2016).
- 9.Cancer Research UK. Stomach cancer survival statistics. http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/stomach-cancer/survival (accessed 26 Oct 2016).
- 10.Koo S, Awadelkarim B, Choudhary S, et al. PTU-159 The Clinical and Service Impact of The National Oesophago-Gastric Cancer Awareness Campaign: A Locality Analysis from County Durham. Gut 2016;65:A135.2–A136. doi:10.1136/gutjnl-2016-312388.244 [Google Scholar]
- 11.Kabir M, Khoo D. PWE-141 Impact of The ‘Be Clear On Cancer’ National Oesophago-Gastric Cancer Awareness Campaign on Endoscopy Services and Cancer Diagnosis Rates and Outcomes. Gut 2016;65:A207.3–A208. doi:10.1136/gutjnl-2016-312388.386 [Google Scholar]
- 12.Alam MA, Sajjad A, Dixon A, et al. PTH-150 Improving Early Diagnosis of Oesophago-Gastric Cancers; A DGH Experience Pre and Post ‘Be Clear On Cancer’ Campaign. Gut 2016;65:A293.1–A293. doi:10.1136/gutjnl-2016-312388.553 [Google Scholar]