Abstract
Objective
Guidelines for the assessment of non-alcoholic fatty liver disease (NAFLD) have been published in 2016 by National Institute for Health and Care Excellence and European Associations for the study of the Liver–European Association for the study of Diabetes–European Association for the study of Obesity. Prior to publication of these guidelines, we performed a cross-sectional survey of gastroenterologists and hepatologists regarding NAFLD diagnosis and management.
Design
An online survey was circulated to members of British Association for the Study of the Liver and British Society of Gastroenterology between February 2016 and May 2016.
Results
175 gastroenterologists/hepatologists responded, 116 completing the survey, representing 84 UK centres. 22% had local NAFLD guidelines. 45% received >300 referrals per year from primary care for investigation of abnormal liver function tests (LFTs). Clinical assessment tended to be performed in secondary rather than primary care including body mass index (82% vs 26%) and non-invasive liver screen (86% vs 32%) and ultrasound (81% vs 37%). Widely used tools for non-invasive fibrosis risk stratification were aspartate transaminase (AST)/alanine transaminase (ALT) ratio (53%), Fibroscan (50%) and NAFLD fibrosis score (41%). 78% considered liver biopsy in selected cases. 50% recommended 10% weight loss target as first-line treatment. Delivery of lifestyle interventions was mostly handed back to primary care (56%). A minority have direct access to community weight management services (22%). Follow-up was favoured by F3/4 fibrosis (72.9%), and high-risk non-invasive fibrosis tests (51%). Discharge was favoured by simple steatosis at biopsy (30%), and low-risk non-invasive scores (25%).
Conclusions
The survey highlights areas for improvement of service provision for NAFLD assessment including improved recognition of non-alcoholic steatohepatitis in people with type 2 diabetes, streamlining abnormal LFT referral pathways, defining non-invasive liver fibrosis assessment tools, use of liver biopsy, managing metabolic syndrome features and improved access to lifestyle interventions.
Keywords: LIVER BIOPSY, LIVER FUNCTION TEST, NONALCOHOLIC STEATOHEPATITIS, FATTY LIVER
Introduction
Non-alcoholic fatty liver disease (NAFLD) is highly prevalent, affecting ∼25% of the population and is likely to increase further due to the obesity epidemic.1 NAFLD occurs due to accumulation of liver fat (steatosis) in the context of obesity and insulin resistance leading to generation of lipotoxic intermediates, and a cycle of liver cell stress, inflammation and fibrosis. This can progress ultimately to decompensated cirrhosis and/or hepatocellular carcinoma (HCC).2
NAFLD is typically asymptomatic and therefore the majority of patients remain undiagnosed. However, other associated features of metabolic syndrome including obesity, insulin resistance, type 2 diabetes, hyperlipidaemia and hypertension may frequently come to medical attention, and also affect prognosis, increasing risk of cardiovascular mortality in this group of patients.3 Thus, the typical patient with NAFLD crosses many of the boundaries between primary and secondary care and between traditional clinical specialties.
The first-line intervention to treat NAFLD is lifestyle changes to lose weight, although many patients with NAFLD find support for lifestyle interventions difficult to access or achieve.4
Although there are currently no licensed drug therapies to treat non-alcoholic steatohepatitis (NASH), several agents are in phase II and III clinical trials. Therefore, the major priorities of healthcare providers at present are to identify those at risk of NAFLD, establish a definite diagnosis, initiate lifestyle interventions, identify those with advanced disease for HCC surveillance and identify those with earlier fibrosis but potentially progressive NASH who may benefit from new treatments in the future.
In 2016, two clinical guidelines for the assessment and treatment of NAFLD have been published: National Institute for Health and Care Excellence (NICE) clinical guideline 495 and the joint European Associations for the study of the Liver (EASL), European Association for the study of Diabetes (EASD) and the European Association for the study of Obesity (EASO).6 The publication of both these guidelines represents an important landmark in NAFLD clinical practice and research. It also highlights the many challenges and uncertainties in the existing evidence base posed by this important clinical problem.
The aim of the present survey was to understand the degree to which practice varies across the UK in identifying patients with NAFLD, diagnosis, risk stratification and treatment. Additionally, these data provide a context for the subsequent recommendations of NICE and EASL-EASD-EASO guidelines for assessment and treatment of NAFLD. We have used the survey findings to recommend an ‘action plan’ to improve NAFLD management.
Method
Survey questions were agreed by the UK-NAFLD group. A 10-question online survey was circulated to members of the British Association for the Study of the Liver (BASL) (859 members) and British Society of Gastroenterology (BSG) Liver Section (561 members) between February 2016 and May 2016. This was prior to the publication of NICE guideline 49 and contemporary to the EASL-EASD-EASO guideline release. The full list of questions included in the survey is provided in the online supplementary appendix.
flgastro-2017-100806supp001.pdf (73.1KB, pdf)
Results
Respondents sample of opinion
One hundred and seventy-five gastroenterologists/hepatologists responded to the survey. One hundred and sixteen respondents provided complete responses, and there were 59 incomplete questionnaires. Eighty-four separate NHS organisations across England, Scotland, Wales and Northern Ireland responded (see online supplementary appendix). Thirty (17%) considered themselves district general hospital (DGH) gastroenterologists, 50 (29%) were DGH gastroenterologists with a hepatology interest, 67 (38%) were hepatologists in a specialist liver unit and 28 (16%) in a liver transplant centre. There was no significant variance in completion rates by type of centre (table 1).
Table 1.
Responses by centre type for NAFLD guidelines and liver fibrosis assessment modalities
| All centres | DGH gastroenterology (%) | DGH hepatology interest (%) |
Specialist hepatology (%) | Liver transplant units (%) | |
|---|---|---|---|---|---|
| Response | |||||
| Completed | 116 (66) | 19 (63) | 34 (68) | 48 (72) | 15 (54) |
| Incomplete | 59 (34) | 11 (37) | 16 (32) | 19 (28) | 13 (46) |
| Local NAFLD guidelines | |||||
| Yes | 38 (22) | 1 (3) | 4 (8) | 23 (34) | 10 (35) |
| No* | 137 (78) | 29 (97) | 46 (92) | 44 (66) | 18 (65) |
| NAFLD fibrosis score | |||||
| Performed in all | 48 (41) | 4 (21) | 14 (41) | 22 (46) | 8 (53) |
| Selected cases | 29 (25) | 4 (21) | 12 (35) | 10 (21) | 3 (20) |
| Not routine* | 39 (34) | 11 (58) | 8 (24) | 16 (33) | 4 (27) |
| APRI score | |||||
| Performed in all | 8 (6) | 0 (0) | 3 (9) | 2 (4) | 3 (20) |
| Selected cases | 18 (16) | 1 (5) | 6 (18) | 10 (21) | 1 (7) |
| Not routine* | 90 (78) | 18 (95) | 25 (73) | 36 (75) | 11 (73) |
| FIB-4 | |||||
| Performed in all | 19 (16) | 1 (5) | 3 (9) | 9 (19) | 6 (40) |
| Selected cases | 15 (13) | 1 (5) | 2 (6) | 10 (21) | 2 (13) |
| Not routine* | 82 (71) | 17 (90) | 29 (85) | 29 (60) | 7 (47) |
| Fibroscan | |||||
| Performed in all | 58 (50) | 3 (16) | 11 (32) | 34 (71) | 10 (67) |
| Selected cases | 46 (40) | 12 (63) | 17 (50) | 12 (25) | 5 (33) |
| Not routine* | 12 (10) | 4 (21) | 6 (18) | 2 (4) | 0 (0) |
| AST/ALT ratio | |||||
| Performed in all | 62 (53) | 9 (47) | 16 (47) | 28 (58) | 9 (60) |
| Selected cases | 24 (21) | 4 (21) | 8 (24) | 10 (21) | 2 (13) |
| Not routine* | 30 (26) | 6 (32) | 10 (29) | 10 (21) | 4 (27) |
| Liver biopsy | |||||
| Performed in all | 7 (6) | 3 (16) | 0 (0) | 2 (4) | 2 (13) |
| Selected cases | 90 (78) | 12 (63) | 22 (65) | 43 (90) | 13 (87) |
| Not routine* | 19 (16) | 4 (21) | 12 (35) | 3 (6) | 0 (0) |
| ELF test | |||||
| Performed in all | 6 (5) | 0 (0) | 1 (3) | 0 (0) | 5 (33) |
| Selected cases | 10 (9) | 2 (11) | 1 (3) | 4 (8) | 3 (20) |
| Not routine* | 100 (86) | 17 (89) | 32 (94) | 44 (92) | 7 (47) |
*Missing responses in completed questionnaires counted as ‘not routine’.
APRI, AST to Platelet Ratio Index; DGH, district general hospital; ELF, Enhanced Liver Fibrosis; NAFLD, non-alcoholic fatty liver disease.
flgastro-2017-100806supp002.pdf (295.6KB, pdf)
38/175 respondents (22%) stated that their centre had local guidelines for NAFLD management. All the respondents that stated they had local NAFLD guidelines completed the survey. More respondents from specialist hepatology units (34%) and liver transplant centres (35%) stated they had local NAFLD guidelines than those in DGH gastroenterology (3%) or DGH with hepatology interest (8%) (table 1).
NAFLD assessment
The majority of new diagnoses of NAFLD are made following investigation of abnormal liver function tests (LFTs), which have typically been performed in primary care for some indication other than suspected NAFLD.7 The UK NAFLD survey data indicate a high demand for secondary care services to investigate abnormal LFTs with 49/110 (45%) of respondents reporting >300 referrals per year from primary care for investigation of abnormal LFTs.
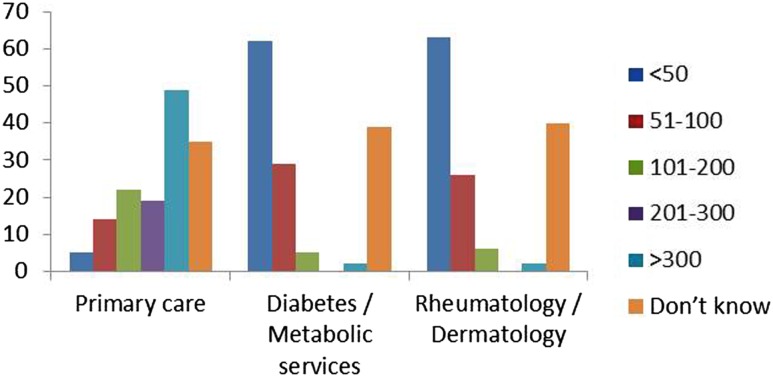
Referrals from diabetes/metabolic services for investigation of abnormal LFTs are fewer than from primary care, with 63/99 (64%) of respondents reporting <50 referrals per year from these services. This supports the perception that NAFLD is under-recognised in this high-risk population with type 2 diabetes (figure 1).
Figure 1.
UK non-alcoholic fatty liver disease survey data estimated number of referrals to gastroenterology and hepatology with abnormal liver function tests (number of respondents).
A positive diagnosis of NAFLD is made on the basis of imaging evidence of hepatic steatosis, and exclusion of other causes of liver disease including alcohol-related liver disease, viral hepatitis, autoimmune liver disease and haemochromatosis. NAFLD diagnosis therefore requires an initial clinical assessment for features of the metabolic syndrome, an alcohol history and a negative ‘non-invasive liver screen’ and abdominal ultrasound scan.8 The UK NAFLD survey questions sought to understand where in the diagnostic pathway an assessment for body mass index (BMI), alcohol consumption and waist circumference is being made. BMI (82.6%) and alcohol history (79.1%) are usually performed in secondary care rather than in primary care, but waist circumference is not routinely performed in most units (56.5%) (see online supplementary figure 1A). For diagnosis of NAFLD, the Fatty Liver Index score (an algorithm based on BMI, waist circumference, gamma-glutamyl transferase (GGT) and fasting triglycerides) is not routinely performed in 89.3% of respondents, although had been suggested by NICE as useful for NAFLD diagnosis.
flgastro-2017-100806supp003.pdf (230.5KB, pdf)
The survey data indicate that the non-invasive liver screen including ferritin (87.7%), hepatitis B and C serology (86%), liver autoantibodies (91.2%), immunoglobulins (91.2%) and liver ultrasound (80.9%) are performed in the majority of cases by secondary rather than primary care (see online supplementary figure 1B).
Assessment of liver fibrosis
Various scoring systems/tools are available for the non-invasive assessment of liver fibrosis. Many require measurement of the AST, whereas others include transient elastography (Fibroscan) and serum fibrosis tests including serum Enhanced Liver Fibrosis (ELF) test. NICE recommends offering testing for advanced liver fibrosis to people with NAFLD using the ELF test.5
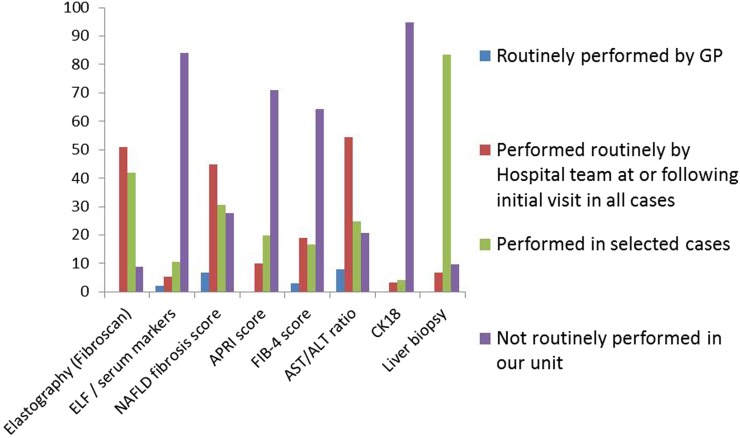
The UK NAFLD survey attempted to capture data on which tools are currently most widely used for non-invasive fibrosis assessment (figure 2). The survey found that the AST is routinely performed by the hospital team in 71.4% of cases, and in 33.9% of primary care cases. The survey indicates that primary care do not routinely perform any assessment of liver fibrosis, with only 7.9% routinely performing AST/ALT ratio in primary care. The tools most commonly used routinely in secondary care are as follows: AST/ALT ratio (53%), transient elastography (Fibroscan) (50%), NAFLD fibrosis score (41%), FIB-4 score (16%), APRI score (6%) and ELF test or other serum fibrosis markers (5%). There was variation in modalities used for liver fibrosis assessment according to type of centre, notably Fibroscan more likely to be performed in specialist hepatology centres (71%) and transplant units (67%) than DGH gastroenterology (16%) or DGH hepatology interest (32%) centres (table 1).
Figure 2.
Modalities performed to assess for liver fibrosis (% of respondents). ELF, Enhanced Liver Fibrosis; NAFLD, non-alcoholic fatty liver disease.
Liver biopsy
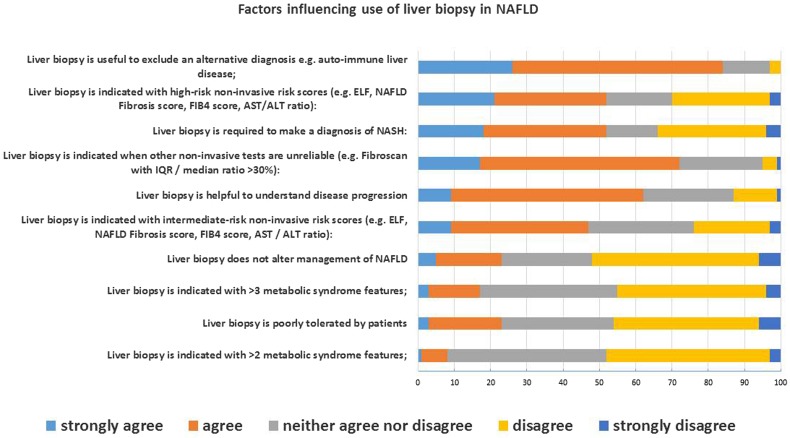
Liver biopsy is an important tool for NAFLD assessment to establish a diagnosis of NASH by histological features of steatosis, hepatocyte ballooning and inflammation, and to stage degree of liver fibrosis. Neither the NICE nor EASL-EASD-EASO guidelines make specific recommendations regarding when to use liver biopsy in NAFLD assessment, although the EASL-EASD-EASO guidance advocates the approach of applying non-invasive methods first, to avoid biopsy in low-risk cases.6 In the UK NAFLD survey, 78% of respondents said they would consider liver biopsy in selected cases. The strength of agreement with a series of statements regarding use of liver biopsy in NAFLD was asked to attempt to understand the boundaries and indications for liver biopsy. The hierarchy of factors for which respondents agreed or strongly agreed with is shown in figure 3. There was general agreement that liver biopsy is indicated when an alternative diagnosis is in the differential, and/or where there are high non-invasive scores of fibrosis. There was also general disagreement that liver biopsy is poorly tolerated by patients. There does not appear to be a consensus of views regarding the utility of liver biopsy in those with escalating features of the metabolic syndrome and in those with intermediate non-invasive risk scores.
Figure 3.
Factors influencing use of liver biopsy in non-alcoholic fatty liver disease (NAFLD) assessment. ELF, Enhanced Liver Fibrosis; NASH, non-alcoholic steatohepatitis.
Extrahepatic conditions
Extraheptic conditions are relevant to holistic care in patients with NAFLD. NICE guidance highlights awareness that NAFLD is a risk factor for type 2 diabetes, hypertension and chronic kidney disease. Furthermore, there should be awareness that in people with type 2 diabetes, NAFLD is a risk factor for atrial fibrillation, myocardial infarction, ischaemic stroke and death from cardiovascular causes.5 The survey sought to understand who manages features of the metabolic syndrome in patients with NAFLD. The survey data indicate that only in a minority does secondary care take ownership of these extrahepatic conditions, the majority either providing advice to general practitioner (GP) or leaving extrahepatic conditions entirely for the GP to manage (see online supplmentary figure 2).
Alcohol
NICE guidelines state that people with NAFLD should stay within the national recommended limits for alcohol consumption. Most respondents of the survey are providing advice consistent with this, advising on both <14 units per week in those without advanced fibrosis (70.6%) and the calorific nature of alcohol (63%) should be moderated to help lose weight.
Lifestyle modification
Currently, lifestyle intervention to lose weight by diet and exercise is the first-line treatment for NAFLD.9 The survey sought to identify whether services can provide access to effective lifestyle interventions. The majority of respondents relied on referral by GP to community weight management services (56.3%) to facilitate delivery of lifestyle interventions. A minority of respondents in secondary care had direct access to either a multidisciplinary clinic with dieticians and physiotherapists (20.9%) input or tier 2 (26%), tier 3 (23%) and/or tier 4 (26%) community weight management services. The survey indicates that most respondents give general advice on diet (93%) and exercise (94%), but fewer set specific weight loss targets of >5% or >10% (see online supplementary figure 3).
Pharmacotherapy
In the absence of any licensed drugs for NASH, most respondents never prescribe any specific pharmaco-interventions including vitamin E, insulin sensitisers, omega 3 supplements or probiotics. Fifty-five per cent occasionally give advice on specific lipid-lowering therapy (see online supplementary figure 4).
Follow-up decision making
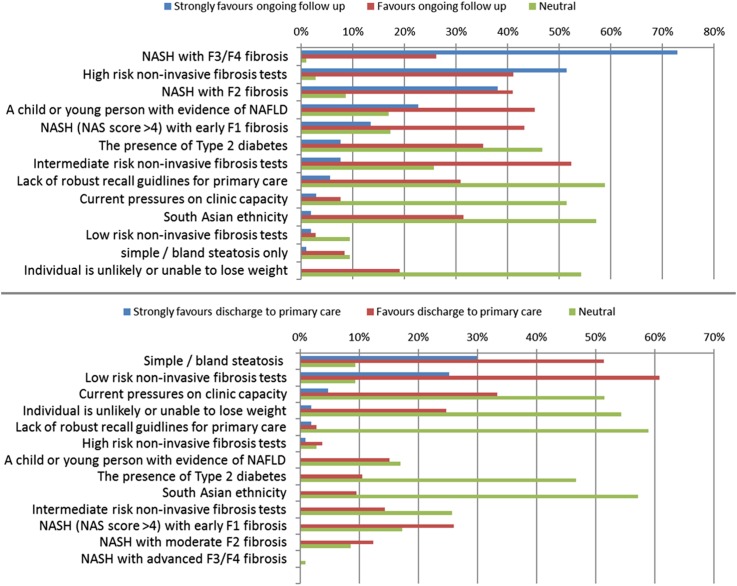
The survey sought to capture data of factors that influence decisions in secondary care to follow up a case of NAFLD, or discharge back to primary care. Those factors most strongly favouring secondary care follow-up were as follows: NASH with F3/F4 fibrosis, high-risk non-invasive fibrosis test scores, NASH with F2 fibrosis and a child or young person with evidence of NAFLD (figure 4A). Factors favouring discharge included simple bland steatosis at liver biopsy, low-risk non-invasive fibrosis tests, current pressures on clinic capacity and individual unlikely or unable to lose weight (figure 4B).
Figure 4.
(A, top panel) Factors favouring follow-up in secondary care. (B, bottom panel) Factors favouring discharge from secondary care. NAFLD, non-alcoholic fatty liver disease; NASH, non-alcoholic steatohepatitis.
Discussion
The publication of clinical practice guidelines for assessment and treatment of NAFLD from NICE and EASL-EASD-EASO provides an impetus to improve care and service provision for patients with NAFLD. Prior to publication of these guidelines, the responses indicate that only a minority of centres had local recommendations for NAFLD assessment, particularly district general hospitals (3%–8%), although only 34% of respondents from specialist liver units and 35% from liver transplant centres had local NAFLD guidelines.
This is the first national cross-sectional survey which attempted to provide some context for implementation of the recent NICE guidelines. In light of the survey findings, we have summarised recommendations to implement changes in practice locally that will help move from the position described by this survey to improved services for patients with NAFLD (table 2).
Table 2.
UK NAFLD Group Recommendations for implementation
| Guideline domain | Proposed actions for implementation | Impact | Research priorities |
|---|---|---|---|
| Identification of NAFLD in high-risk groups | Screening primary care populations with known type 2 diabetes for significant NAFLD with liver fibrosis as part of the existing diabetes QOF | Increased NAFLD diagnosis in high-risk patients with type 2 diabetes | Does earlier diagnosis of NASH with liver fibrosis alter outcomes in patients with T2DM? |
| Diagnosis | Review and streamline referral pathways for assessment of abnormal LFTs. Perform routine diagnostic investigations to establish NAFLD diagnosis, including abdominal ultrasound and non-invasive liver screen blood tests (hepatitis B and C serology), ALT, AST, ferritin, autoantibody profile and immunoglobulins) in primary care | Streamline referral pathways to decrease number of hospital outpatient appointments | Evaluation of community-based programmes for NAFLD diagnosis and risk stratification |
| Staging for advanced disease | Perform a non-invasive test with high negative predictive value to exclude advanced liver fibrosis in primary care, or at point of referral for assessment to secondary care. Fib 4, NFS, ELF and transient elastography all suitable depending on local availability | Facilitates discharge of low-risk cases, and decision to biopsy and follow-up intermediate and high-risk cases | Evaluate the diagnostic performance and cost-effectiveness of non-invasive fibrosis risk scores versus ELF versus transient elastography |
| Liver biopsy | Offer liver biopsy to those with intermediate and high-risk scores to diagnose NASH with fibrosis, or reclassify as low risk, and reporting using standardised criteria | Definitive NASH diagnosis, access to clinical trials and those that may benefit for future licensed therapies | Evaluation of biomarkers and imaging as an alternative to biopsy for NASH diagnosis and staging |
| Extrahepatic conditions | Proactive management of features of the metabolic syndrome by both primary and secondary care | Improved cardiovascular risk reduction | Specific evidence base on which insulin sensitisers, lipid-lowering therapies and antihypertensive are best in NAFLD cases |
| Lifestyle intervention | Set target of 10% weight loss by diet and exercise as first-line treatment for all cases of NAFLD. Increase access to tier 2 and 3 weight management services to deliver weight loss as first-line NAFLD treatment |
Improved efficacy of lifestyle intervention to treat NASH. Define lifestyle non-responders who may benefit from trials and future therapies |
What factors influence response/non-response to lifestyle intervention? |
| Trials | Individuals with NASH and ≥F2 fibrosis should be offered access to clinical trials, and long-term follow-up in secondary care to assess fibrosis progression | Evidence base for NASH specific therapies | What interventions have greatest efficacy, in which populations? Factors that determine response and non-response |
ELF, Enhanced Liver Fibrosis; NAFLD, non-alcoholic fatty liver disease; NASH, non-alcoholic steatohepatitis; NFS, NAFLD Fibrosis Score; QOF, Quality Outcomes Framework; T2DM, type 2 diabetes mellitus.
The major demand to assess probable NAFLD in secondary care is coming from primary care referral to investigate abnormal LFTs. The evidence from this survey suggests a likely under-recognition of NAFLD in high-risk individuals, such as those attending diabetes clinics. A significant proportion of asymptomatic patients attending type 2 diabetes clinics have undiagnosed NAFLD and advanced liver fibrosis10 and therefore diabetic clinics may be an appropriate setting for case finding.
Simple steps can be implemented into most local referral guidelines and pathways to improve standards. These include improved simple clinical assessment including alcohol history, measurement of BMI and waist circumference in all cases.
Abnormal LFT pathways can be streamlined, recognising that NAFLD is the most common reason for referral from primary care for investigation of abnormal LFTs.7 NAFLD diagnosis can be made in primary care, by exclusion of other causes of liver disease. Thus, an alcohol history, non-invasive liver screen and ultrasound scan to exclude biliary pathology and confirm hepatic steatosis are mandatory. Streamlined abnormal LFT referral pathways between primary and secondary care should be developed in all localities to prevent unnecessary follow-up appointments. The focus of secondary care assessment of NAFLD should be on staging, managing the metabolic syndrome and delivering lifestyle interventions.
Following NAFLD diagnosis, non-invasive assessment of liver fibrosis is required. NICE advocates the use of ELF testing which could be performed exclusively in primary care. However, the survey indicates that only 5% of respondents were routinely using ELF. The assessment of fibrosis is generally perceived as an added value exercise of a secondary care referral and the most widely used tools identified from the survey were transient elastography (Fibroscan), AST/ALT ratio, NFS and Fib-4 scores. All of these modalities have an evidence base for having good (>90%) negative predictive values to ‘rule-out’ advanced fibrosis in those with low scores, but poor positive predictive values to ‘rule-in’ NASH with fibrosis in those with higher scores in secondary care cohorts.11
Current NICE and EASL-EASD-EASO guidelines do not specify when liver biopsy should be undertaken, but histology is required to diagnose NASH with fibrosis. Most survey respondents indicated that there is a role for liver biopsy, which was most strongly favoured when an alternative diagnosis was being considered, and in those with high-risk non-invasive scores. Liver biopsy has an important role in defining eligibility to clinical trials and should be reported according to an agreed framework.12 13
The survey indicates variation in delivery of lifestyle intervention and specific management of features of the metabolic syndrome. In many instances, respondents indicated that secondary care gastroenterologists and hepatologists consider this the responsibility for primary care to deliver. We advocate that secondary care gastroenterologists and hepatologists assessing patients with NAFLD should prescribe a target of 10% weight loss over 12 weeks by diet and exercise as first-line treatment for NAFLD, and re-assess response. This can be facilitated in most districts by closer working and referral pathways to tier 2 and 3 community weight management services, in line with the NICE obesity guidance.14 Furthermore, the survey highlights variation in ownership of management of features of the metabolic syndrome. We advocate a more holistic approach to managing the metabolic syndrome by all physicians assessing patients with NAFLD.
The strengths of this survey are that it is representative of opinion of membership of BSG and BASL gastroenterologists and hepatologists in secondary care. The study is limited by not including representation from primary care, and the data remain qualitative and subjective. It is the intention of the UK NAFLD group to repeat the survey, a year after publication of NICE guidelines to determine if management of patients with NAFLD is improving.
In conclusion, the survey has highlighted priorities for service development to adopt recent guidance for NAFLD management, including improved recognition of NAFLD in type 2 diabetes, streamlining abnormal LFT referral pathways, defining non-invasive fibrosis assessment, when to perform liver biopsy, increasing ownership of managing metabolic syndrome and improving access and delivery of lifestyle interventions.
Significant of this study.
What is already known on this topic
New clinical guidelines for non-alcoholic fatty liver disease (NAFLD) assessment, diagnosis and treatment were published in 2016 from National Institute for Health and Care Excellence and European Associations for the study of the Liver.
What this study adds
This national cross-sectional survey captured opinion on the state of NAFLD assessment in the UK, before guideline publication.
How might it impact on clinical practice in the foreseeable future
The survey has identified priority areas for service improvement and implementation of recent guidelines.
Footnotes
Contributors: DAS designed the survey, collated responses, performed data analysis and wrote first draft of the manuscript. GA, WA, MA, QA, JC, SK, AF, SM, PNN, JO, JT and ET contributed to the design of the survey, interpretation of data and revised the manuscript.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Younossi ZM, Koenig AB, Abdelatif D, et al. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016;64:73–84. doi:10.1002/hep.28431 [DOI] [PubMed] [Google Scholar]
- 2.Machado MV, Diehl AM. Pathogenesis of nonalcoholic steatohepatitis. Gastroenterology 2016;150:1769–77. doi:10.1053/j.gastro.2016.02.066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol 2015;62:S47–64. doi:10.1016/j.jhep.2014.12.012 [DOI] [PubMed] [Google Scholar]
- 4.Dudekula A, Rachakonda V, Shaik B, et al. Weight loss in nonalcoholic Fatty liver disease patients in an ambulatory care setting is largely unsuccessful but correlates with frequency of clinic visits. PLoS ONE 2014;9:e111808 doi:10.1371/journal.pone.0111808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.NICE guideline 49. Non-alcoholic fatty liver disease: assessment and management. non-alcoholic fatty liver disease: assessment and management. London, 2016. https://www.nice.org.uk/guidance/ng49 [Google Scholar]
- 6.European Association for the Study of the Liver. Electronic address eee, European Association for the Study of D, European Association for the Study of O. EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol 2016;64:1388–402. doi:10.1016/j.jhep.2015.11.004 [DOI] [PubMed] [Google Scholar]
- 7.Armstrong MJ, Houlihan DD, Bentham L, et al. Presence and severity of non-alcoholic fatty liver disease in a large prospective primary care cohort. J Hepatol 2012;56:234–40. doi:10.1016/j.jhep.2011.03.020 [DOI] [PubMed] [Google Scholar]
- 8.Dyson JK, Anstee QM, McPherson S. Non-alcoholic fatty liver disease: a practical approach to diagnosis and staging. Frontline Gastroenterol 2014;5:211–18. doi:10.1136/flgastro-2013-100403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dyson JK, Anstee QM, McPherson S. Non-alcoholic fatty liver disease: a practical approach to treatment. Frontline Gastroenterol 2014;5:277–86. doi:10.1136/flgastro-2013-100404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Armstrong MJ, Hazlehurst JM, Parker R, et al. Severe asymptomatic non-alcoholic fatty liver disease in routine diabetes care; a multi-disciplinary team approach to diagnosis and management. QJM 2014;107:33–41. doi:10.1093/qjmed/hct198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McPherson S, Stewart SF, Henderson E, et al. Simple non-invasive fibrosis scoring systems can reliably exclude advanced fibrosis in patients with non-alcoholic fatty liver disease. Gut 2010;59:1265–9. doi:10.1136/gut.2010.216077 [DOI] [PubMed] [Google Scholar]
- 12.Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 2005;41:1313–21. doi:10.1002/hep.20701 [DOI] [PubMed] [Google Scholar]
- 13.Bedossa P, Consortium FP. Utility and appropriateness of the fatty liver inhibition of progression (FLIP) algorithm and steatosis, activity, and fibrosis (SAF) score in the evaluation of biopsies of nonalcoholic fatty liver disease. Hepatology 2014;60:565–75. doi:10.1002/hep.27173 [DOI] [PubMed] [Google Scholar]
- 14.NICE guideline 43. Obesity: identification, assessment and management of overweight and obesity in children, young people and adults: partial update of CG43. Obesity: identification, assessment and management of overweight and obesity in children, young people and adults: partial update of CG43. London, 2014. https://www.nice.org.uk/guidance/cg189 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
flgastro-2017-100806supp001.pdf (73.1KB, pdf)
flgastro-2017-100806supp002.pdf (295.6KB, pdf)
flgastro-2017-100806supp003.pdf (230.5KB, pdf)