Abstract
Objectives: The use of effective contraception can decrease the incidence of unplanned pregnancy among adolescents. This study aims to examine the effectiveness of an iPad-based application (app) on improving adolescent girls’ sexual health knowledge and on its ability to influence their intentions to use effective contraception. Study Design: This was a prospective study of girls aged 12 to 18 years recruited from 3 school-based health centers in California. Results: A total of 120 racially/ethnically diverse participants used the iPad app; 54% were sexually active, with only 26% using effective contraception at baseline. The average score on baseline sexual health knowledge assessment was 58%. After using the app, 68% of the sexually active participants reported intention to use effective contraception in the future, and sexual health knowledge improved significantly to 79% (P < .001). Conclusions: This iPad-based app is a promising intervention to educate adolescents about sexual health and support them in selecting an effective contraception method.
Keywords: computer-based intervention, adolescent contraceptive use, sexual health knowledge, school-based health center, iPad, LARC
Introduction
Despite national declines, the teen birth rate in the United States is higher than in any other developed country.1,2 Compared with adults, teen parents and their offspring are at greater risk for poor economic and psychosocial outcomes, and children of teen parents are more likely to experience preterm birth, low birth weight, behavior problems, and an increased risk of becoming teen parents themselves compared with children of older parents.3,4 Although there are a number of primary prevention efforts that delay the onset of sexual activity,5 many adolescents are still at risk of having an unintended pregnancy.6 Nearly half of all 17-year-olds report having had sex,7 and their knowledge and use of effective contraceptives is poor—especially for highly effective contraceptive methods.8 Thus, interventions to improve adolescents’ access to comprehensive, confidential contraceptive information and services are essential.9
Long-acting reversible contraceptives (LARCs), such as intrauterine devices (IUDs) and hormonal implants, are now recommended as first-line contraceptives for adolescents10,11 because they are highly effective, safe, have few side effects, and do not require maintenance after insertion. Despite these recommendations, less than 5% of teens currently using contraceptives are using a LARC method.12 Many adolescents are not aware of LARCs, and providers often lack the time, comfort, and knowledge to provide accurate and effective LARC counseling to adolescents.8,13-17 There is emerging research on interventions that can improve adolescents’ attitudes and uptake of LARCs. For instance, the Contraceptive CHOICE study found that when adolescents are offered appropriate counseling and cost is removed as a barrier, 61% to 69% chose a LARC method.18 Another recent randomized control study found that patient-centered, efficacy-based counseling results in increased uptake of highly effective methods including LARCs.19 There is also some encouraging evidence that brief educational interventions can improve adolescents’ attitudes toward IUDs.20 In addition, one study found, that at least among adult women, a computer-based intervention was effective in promoting the uptake of effective contraceptives such as LARCs.21
Computer-based interventions are a preferred modality for sexual health education and risk assessment among adolescents.22,23 However, few studies have explored the use of computerized interventions to improve contraceptive knowledge and uptake among adolescents.24,25 The purpose of this study is to examine the extent to which use of an interactive, iPad-based mobile health application (app) can improve adolescent girls’ knowledge of contraception and their intent to use more effective contraception methods, including LARCs.
Methods
App Development
Health-E-You, an interactive, individually tailored mobile health app was developed to educate adolescents about contraceptive methods and to assist them in selecting a contraceptive method that meets their individual needs. It was designed to be used in conjunction with a clinical encounter to prime both the patient and provider prior to the face-to-face visit. The app was designed in close collaboration with clinicians and adolescents and based on principles of social cognitive theory. According to this theory, self-efficacy and goal setting influence behavior, and behavior is often shaped by forethought about the future, identification of desired outcomes, and through the use of information that can be acquired via vicarious learning experiences.26 Accordingly, Health-E-You presents information while simultaneously providing an individualized assessment of users’ heath risks, expectations, and preferences to facilitate a sense of agency and self-efficacy around contraceptive choice. Users are encouraged to choose contraception options based on their own timeline for childbearing. They review pros and cons of each contraceptive method according to their own lifestyle preferences and needs and are provided with vicarious learning experiences through YouTube style videos (used with permission from Bedsider.org) featuring diverse young women discussing their experiences with various contraceptive methods. The clinician receives feedback from the app to further support and reinforce the adolescent in selecting an effective and appropriate method.
Focus groups, interviews, and iterative usability testing sessions with adolescents and providers were conducted to ensure that the content and messaging was relevant, engaging, and youth friendly and that it would facilitate an individualized counseling approach appropriate for adolescents. We conducted a series of 8 focus groups with approximately 6 to 8 adolescent girls (15-18 years old) per group (6 with Latina youth and 2 with multiple ethnicities). Youth expressed enthusiastic interest in using touch-screen tablet computers or iPads to explore information about contraceptive options over traditional health education formats such as brochures. They expressed a great deal of interest in using the app because they felt it was private and they could explore topics on their own time without feeling like they were “being judged” by a health professional. Youth provided input on common misconceptions about sexual health and contraception and suggested using a “myth-busters” style game to assess if common misconceptions about sexual health were a myth or fact. Youth reviewed existing computer-based contraception education tools on several leading websites and reported that these sites seemed more suited for adult women with more education and experience. Youth also felt that the number of contraceptive options presented on websites was overwhelming and suggested presenting methods in a time-line format based on duration of action. Furthermore, they felt that they would not seek out these websites on their own and expressed a preference for being able to use a tablet computer confidentially, in a school-based health center (SBHC) or clinic setting. Adolescent medicine specialists and clinicians from each of the three SBHCs were also interviewed during the development of Health-E-You. They indicated that they wanted the app to offload as much of the contraceptive health education and risk assessment as possible and wanted the information captured in the app to be shared with them prior to the face-to-face encounter to improve the efficiency and effectiveness of the visit. Paper prototypes were developed and revised through iterative input from clinicians and adolescents.
Description of Health-E You
The Health-E-You programming framework contains a number of features, including customized, individually tailored patient education content, consisting of complex individual pathways and real-time dynamic decision trees as well as secure communication strategies that allow patient and clinician to share information confidentially.27 It presents audio and visual components in a touch screen, interactive format on an iPad. The app also enables real-time, secure data capture for remote data analyses.
First, the app provides a brief description of the module and consents the user to participate. It then assesses sexual health knowledge using an interactive truth versus myth game (see Table 1 for the list of knowledge assessment items). Correct answers to the truth versus myth statements are then presented to the user as short, easy-to-read explanations. Next, the app assesses the user’s individual contraceptive needs and use. It then presents a visual continuum of effective contraceptive options based on duration of action and efficacy and the user can select each method to get basic information about the method, its use, and pros and cons (Figure 1). The user also answers a brief series of questions about acceptability of common side effects and is screened for possible contraindications (via CDC medical eligibility criteria). The user can also select different video vignettes featuring young women discussing their experiences with a particular method.28 Throughout the module, the user is given individually tailored messages. For instance, if she indicates that she is using an ineffective contraceptive method (e.g. withdrawal or the rhythm method), she is warned that many women become pregnant with this method and is directed to explore more effective contraceptive methods. The app also emphasizes dual use of contraception and condoms to protect against unplanned pregnancy and sexually transmitted infections (STIs) and provides information about emergency contraception. At the completion of the module, sexual health knowledge is reassessed using a true/false format, and the user is asked to select the contraceptive method she would like to use in the future. The module concludes with a brief, 5-question app acceptability survey with questions such as, “I found this program easy to use” and “I felt comfortable answering questions on a computer like this,” and a few basic demographic questions. Information about contraceptive choice is then shared with the user’s provider via secure e-mail so that she may be offered her preferred method during a clinical visit.
Table 1.
Knoweldge Assessment Items (Myth vs Fact).
| 1. Myth or Fact? Birth control pills can reduce risk of getting a sexually transmitted disease (STD). |
| 2. Myth or Fact? A woman cannot get pregnant if the male partner pulls out before he ejaculates (cums). |
| 3. Myth or Fact? Weight gain is a common side effect of most birth control methods, especially for the Intra-Uterine Device (IUD) [Mirena]. |
| 4. Myth or Fact? Birth control pills start working as soon as you begin the method. |
| 5. Myth or Fact? Decreased menstrual bleeding from using IUDs [Mirena] does not cause health problems later on. |
| 6. Myth or Fact? Contraception methods, like the IUD [Mirena] and implant, can make it more difficult to become pregnant in the future. |
| 7. Myth or Fact? The IUD [Mirena] is easy for a doctor to insert and remove. |
Figure 1.
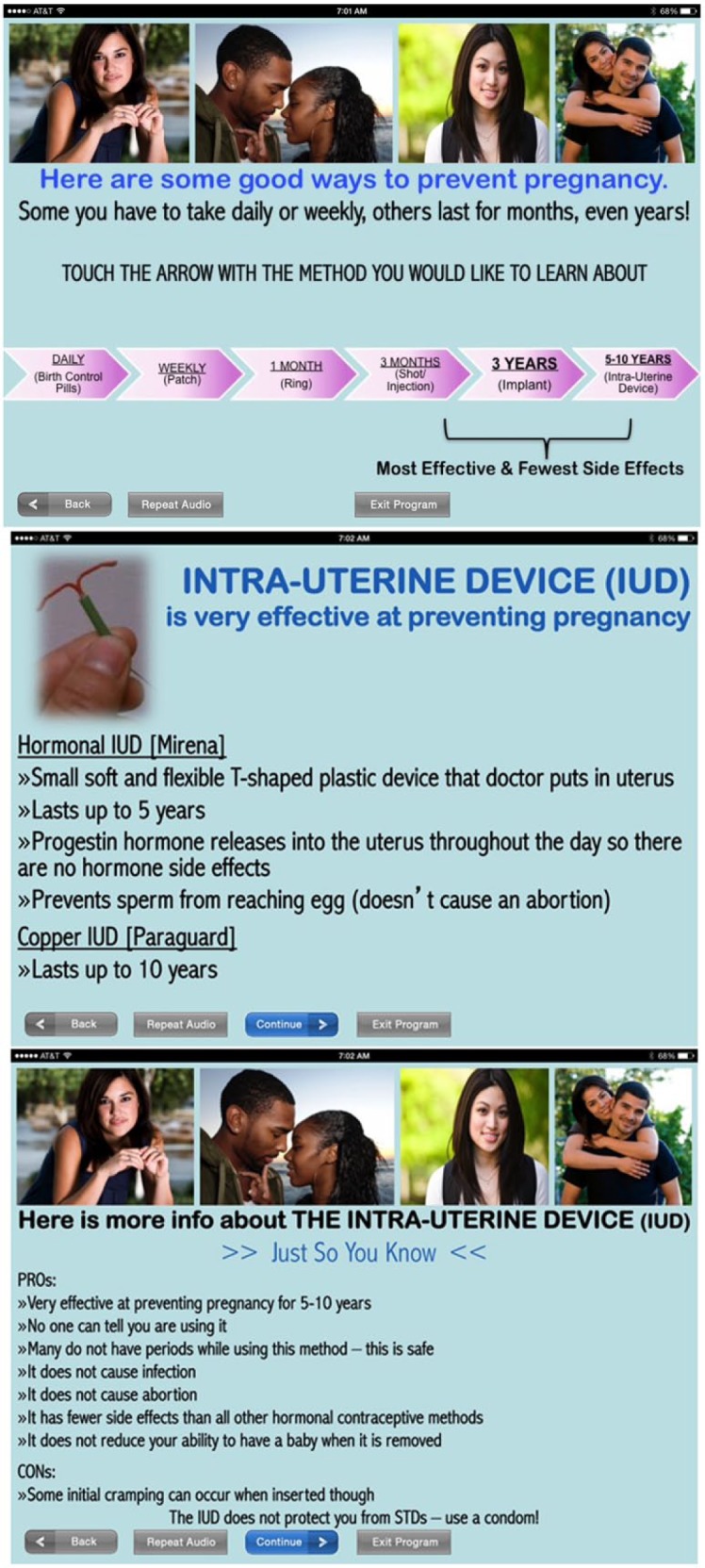
Contraceptive Options.
Procedures
This study examined the impact of Health-E-You on contraceptive knowledge and on its ability to promote use of effective contraception among adolescent girls at 3 SBHCs in urban settings in northern and southern California.
English-speaking girls who presented for care at the SBHCs used the app prior to their clinical encounter. Data were collected in real time and stored in a back-end database with no patient identifiers. Waivers of parental consent were obtained to protect adolescent confidentiality. Informed consent for adolescent participants was obtained via the app. The study was approved by the internal review board at the University of California, San Francisco.
Results
A total of 120 girls used the Health-E-You app between April and September 2014.
Demographic and Background Information About Participants
The sample was ethnically diverse (see Table 2). The mean age of participants was 16.4 years (range 12-18 years). More than half of the participants (54%) reported currently being sexually active. Of those sexually active participants, 68% were using no contraception (Table 3). Among those who reported they were using contraception, 22% were using condoms alone, 3% were using birth control pills, 1.5% were using a hormonal injection, 1.5% were the using calendar method, and 1.5% reported using withdrawal. The remaining 1.5% did not specify the method they were using.
Table 2.
Demographics (n = 120).a
| n | Percentage | |
|---|---|---|
| Mean age (years) ± SD (range) | 16.4 | ±2.3 (12-18) |
| Currently sexually active | 65 | (54) |
| Race/Ethnicity | ||
| Latina/Hispanic | 38 | (32) |
| African American/Black | 28 | (23) |
| Asian American | 10 | (8) |
| Caucasian/White | 10 | (8) |
| Multiple | 9 | (7) |
| Other | 5 | (4) |
| Not provided | 20 | (17) |
Given as n (%) unless otherwise specified.
Table 3.
Baseline Birth Control Use Patterns Among Sexually Active Participants (n = 65).
| n | Percentage | |
|---|---|---|
| None | 44 | (68.0) |
| Condoms alone | 14 | (22.0) |
| Birth control pills | 2 | (3.0) |
| Hormonal injection | 1 | (1.5) |
| Calendar method | 1 | (1.5) |
| Withdrawal | 1 | (1.5) |
| No response | 2 | (3.0) |
Sexual Health Knowledge, Contraceptive Use, and Intentions
There were significant improvements in pre-post sexual health knowledge assessed at the beginning of the app and at the end of the app. The mean proportion of correct answers at baseline was 58% (range = 14%-86%; SD = 0.3), which improved significantly at posttest to 79% (range = 29%-85%; SD = 0.3; p ≤ .001).
Among the sexually active participants, only 26% (n = 17) reported use of an effective contraceptive method at baseline. Of those, the majority (n = 14) reported only using condoms. After using the app, 66% (n = 43) reported intentions to use an effective method of contraception (p < .001), and 25% indicated that they would use dual contraception (ie, a hormonal method or LARC plus a condom) (Table 4).
Table 4.
Baseline Birth Control Use Versus Intention for Future Use After Using Health-E-You Among Sexually Active Participants (n = 65).
| Method | Baseline Use, n (%) | Intentions for Future Use, n (%) |
|---|---|---|
| Implant total | 0 (0) | 6 (9.0) |
| Implant alone | 0 | 5 |
| Implant + Condom | 0 | 1 |
| IUD total | 0 (0) | 6 (9.0) |
| IUD alone | 0 | 5 |
| IUD + Condom | 0 | 1 |
| Shot total | 1 (1.5) | 1 (1.5) |
| Shot alone | 1 | 0 |
| Shot + Condom | 0 | 1 |
| Ring total | 0 (0) | 4 (6.0) |
| Ring alone | 0 | 2 |
| Ring + Condom | 0 | 2 |
| Patch total | 0 (0) | 1 (1.5) |
| Patch alone | 0 | 1 |
| Patch + Condom | 0 | 0 |
| Pill total | 2 (3.0) | 15 (23.0) |
| Pill alone | 2 | 4 |
| Pill + Condom | 0 | 11 |
| Condoms alone | 14 (21.0) | 9 (14.0) |
| Calendar method | 1 (1.5) | 1 (1.5) |
| Withdrawal | 1 (1.5) | 1 (1.5) |
| No response | 2 (3.0) | 19 (29.0) |
| More than 2 methods | 0 (0) | 1 (1.5) |
| None | 44 (68) | 1 (1.5) |
Abbreviation: IUD, intrauterine device.
The most popular method was the birth control pill, with 23% of participants indicating future intention to use this method. The pill was followed by condoms (14%), the IUD and implant (each at 9%), vaginal ring (6%), patch (2%), and shot (2%). None indicated intention to use emergency contraception; 3 participants indicated that they would use an ineffective method such as withdrawal or rhythm method; and 1 participant indicated that she would use more than 2 methods (pill, patch, ring, condoms).
Of the 44 participants who reported that they were sexually active and not using any contraception prior to using the app, 28 (64%) reported that they would use an effective method after using the app. The participants (both sexually active and non-sexually active) who expressed intent to use a LARC method in the future were only slightly older on average than the overall study sample (mean age 16.6 vs 16.4 years); the majority where white, all were sexually active, and 33% were using some form of contraception prior to using the app (Table 5).
Table 5.
Characteristics of All Participants Who Indicated Intention to Use LARC (n = 12) Versus Non-LARC Methods (n = 37).
| LARC | Non-LARC | |||
|---|---|---|---|---|
| Mean age, years ± SD (range) | 16.6 ± 0.8 (16-18) | 15.9 ± 1.5 (12-18) | ||
| Average score on initial knowledge assessment, percentage ± SD (range) | 69 ± 0.17 (29%-86%) | 68 ± 0.25 (14%-100%) | ||
| n | Percentage | n | Percentage | |
| Race/Ethnicity | ||||
| Caucasian/White | 4 | (33%) | 6 | (16%) |
| African American/Black | 3 | (25%) | 7 | (19%) |
| Latina/Hispanic | 3 | (25%) | 13 | (35%) |
| Asian | 1 | (8%) | 6 | (16%) |
| Multiple/Other | 1 | (8%) | 7 | (19%) |
| Currently sexually active | 12 | (100%) | 34 | (92%) |
| Currently using a method to prevent pregnancy | 4 | (33%) | 10 | (27%) |
| Condom | 3 | 8 | ||
| Ineffective method | 1 | 1 | ||
| Birth control pill | 0 | 1 | ||
Discussion
This study explored the ability of an interactive, individually tailored app, Health-E You, to improve contraceptive knowledge and influence contraceptive use among a diverse group of adolescent girls presenting for care at 3 California SBHCs. Despite the safety, acceptability, and effectiveness of LARC methods for use among adolescents, uptake has been slow29 and many lack access to LARCs30. This app is designed to be used in conjunction with a patient-centered clincial encounter that supports adolescents’ access to the full range of contraceptive options and facilitates contraceptive choice which is free of coersion.
This app increased sexual health knowledge and influenced adolescents’ intentions to use an effective or more effective method of contraception. Baseline contraceptive knowledge assessment revealed that, on average, users answered 4 out of 7 questions correctly prior to using the app, indicating important gaps in contraceptive knowledge among the study participants. After using the app, the mean correct scores increased significantly, suggesting that Health-E-You is an effective educational tool for this population. In addition, more than half of the participants in this study reported being sexually active, and most of them (68%) were using no contraception prior to using the app. After using the app, the majority of sexually active participants indicated intention to use an effective contraceptive method in the future, and many indicated intention to use a dual method. Although the birth control pill remained the most popular method, several participants indicated intentions to use LARC methods. These data suggest that Health-E-You is effective at promoting the use of effective contraceptive methods, including LARCs, and dual method use among adolescents.
There are a number of limitations to this study. This study included a relatively small sample of 120 participants, of whom 65 were sexually active. Because of this, our analysis focused on sexually active participants who were at greatest risk for pregnancy. This study was not able to assess the influence of Health-E-You on contraceptive use intentions among not-yet-sexually active youth because only 5 of the non–sexually active participants provided information on their intentions to use contraception in the future. In addition, this study was a pilot study, and as such, it did not utilize a comparison group to evaluate the efficacy of the app versus standard counseling materials or assess knowledge and actual contraceptive use and adherence over time. Furthermore, because of the small sample, we were not able to assess variations in intentions by demographic factors or factors associated with their visit (eg, reason for visit, satisfaction with clinic/clinic staff).
Health-E-You is a promising intervention that is acceptable to adolescents and clinic staff/providers, feasible to implement, and an effective contraceptive counseling tool for adolescent patients when used in conjunction with a clinical visit. This study indicates that future research is warranted to more rigorously evaluate the effectiveness of Health-E-You. Specifically, a randomized-controlled trial could be used to determine its effect on improvements in the use of effective contraception, adherence to effective contraception over time, and knowledge retention over time. Although more research is needed, this study shows that Health-E-You helps adolescents understand their options and encourages the use of effective contraceptive methods, including LARCs.
Author Contributions
KPT conceptulalized study design, development of the app, and data collection methods. VVM was the lead author in writing the manuscript. KPT and VVM both contributed to the conceptualization of this manuscript, conducted data analyses, and provided approval of the final manuscript.
Acknowledgments
We would like to thank the participating School Based Health/Wellness Centers in the Los Angeles and Vallejo Unified School Districts and Kimberly Uyeda, MD, MPH Director, Student Medical Services at LAUSD. Special thanks to our partners who were instrumental in pilot testing the app: Maryjane Puffer, BSN, MPA, and Sang Leng Trieu, DrPH, from the Los Angeles Trust for Children’s Health, and Rebecca Dudovitz, MD, MSHS, from UCLA; and our colleagues Loris Hwang, MD, Claire Brindis, DrPH, Lauren Hartman, MD, and Felicia Rodriquez who provided input on the development of the app.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was partially funded through a PCORI Reducing Disparities Award No. AD-1502-27481, the Hellman Fellowship Fund, and Grant T71MC00003 from the Maternal and Child Health Bureau, Health Resources and Services Administration, US Department of Health and Human Services.
References
- 1. World Bank Group. World Development Indicators 2014. http://elibrary.worldbank.org/doi/book/10.1596/978-1-4648-0163-1. Accessed January 10, 2017.
- 2. Martin JA, Hamilton BE, Osterman MJ, Curtin SC, Matthews TJ. Births: final data for 2013. Natl Vital Stat Rep. 2015;64:1-68. [PubMed] [Google Scholar]
- 3. Jaffee S, Caspi A, Moffitt TE, Belsky J, Silva P. Why are children born to teen mothers at risk for adverse outcomes in young adulthood? Results from a 20-year longitudinal study. Dev Psychopathol. 2001;13:377-397. [DOI] [PubMed] [Google Scholar]
- 4. Olausson PO, Haglund B, Weitoft GR, Cnattingius S. Teenage childbearing and long-term socioeconomic consequences: a case study in Sweden. Fam Plan Perspect. 2001;33:70-74. [PubMed] [Google Scholar]
- 5. US Department of Health & Human Services, Office of Adolescent Health, Teen Pregnancy Prevention Resource Center. Evidence-based programs. http://www.hhs.gov/ash/oah/oah-initiatives/teen_pregnancy/db/tpp-searchable.html. Accessed January 10, 2017.
- 6. Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84:478-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Finer LB, Philbin JM. Sexual initiation, contraceptive use, and pregnancy among young adolescents. Pediatrics. 2013;131:886-891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Teal SB, Romer SE. Awareness of long-acting reversible contraception among teens and young adults. J Adolesc Health. 2013;52:S35-S39. [DOI] [PubMed] [Google Scholar]
- 9. Society for Adolescent Health and Medicine; Burke PJ, Coles MS, Di Meglio G, et al. Sexual and reproductive health care: a position paper of the Society for Adolescent Health and Medicine. J Adolesc Health. 2014;54:491-496. [DOI] [PubMed] [Google Scholar]
- 10. Committee on Practice Bulletins—Gynecology. Long-acting reversible contraception: implants and intrauterine devices. Obstet Gynecol. 2011;118:184. ACOG Practice Bulletin No. 121. [DOI] [PubMed] [Google Scholar]
- 11. Committee on Adolescence. American Academy of Pediatrics Policy Statement: Contraception for adolescents. Pediatrics. 2014;134:e1244-e1256.25266430 [Google Scholar]
- 12. Kavanaugh ML, Jerman J, Finer LB. Changes in use of long-acting reversible contraceptive methods among U.S. women, 2009-2012. Obstet Gynecol. 2015;126:917-927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tyler CP, Whiteman MK, Zapata LB, Curtis KM, Hillis SD, Marchbanks PA. Health care provider attitudes and practices related to intrauterine devices for nulliparous women. Obstet Gynecol. 2012;119:762-771. [DOI] [PubMed] [Google Scholar]
- 14. Russo JA, Miller E, Gold MA. Myths and misconceptions about long-acting reversible contraception (LARC). J Adolesc Health. 2013;52(4, suppl):S14-S21. [DOI] [PubMed] [Google Scholar]
- 15. Kavanaugh ML, Frohwirth L, Jerman J, Popkin R, Ethier K. Long-acting reversible contraception for adolescents and young adults: patient and provider perspectives. J Pediatr Adolesc Gynecol. 2013;26:86-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fleming KL, Sokoloff A, Raine TR. Attitudes and beliefs about the intrauterine device among teenagers and young women. Contraception. 2010;82:178-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Carr S, Espey E. Intrauterine devices and pelvic inflammatory disease among adolescents. J Adolesc Health. 2013;52(4, suppl):S22-S28. [DOI] [PubMed] [Google Scholar]
- 18. Mestad R, Secura G, Allsworth JE, Madden T, Zhao Q, Peipert JF. Acceptance of long-acting reversible contraceptive methods by adolescent participants in the Contraceptive CHOICE Project. Contraception. 2011;84:493-498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Harper C., Rocca C, Thompson K, Morphesis J, Goodman S, Darney P, Westhoff C, Speidel J. Reductions in pregnancy rates in the USA with long-acting reversible contraception: a cluster randomised trial. The Lancet. 2015;386 (9993):562-568. [DOI] [PubMed] [Google Scholar]
- 20. Whitaker AK, Terplan M, Gold MA, Johnson LM, Creinin MD, Harwood B. Effect of a brief educational intervention on the attitudes of young women toward the intrauterine device. J Pediatr Adolesc Gynecol. 2010;23:116-120. [DOI] [PubMed] [Google Scholar]
- 21. Garbers S, Meserve A, Kottke M, Hatcher R, Ventura A, Chiasson MA. Randomized controlled trial of a computer-based module to improve contraceptive method choice. Contraception. 2012;86:383-390. [DOI] [PubMed] [Google Scholar]
- 22. Paperny DM. Computerized health assessment and education for adolescent HIV and STD prevention in health care settings and schools. Health Educ Behav. 1997;24:54-70. [DOI] [PubMed] [Google Scholar]
- 23. Tebb KP, Gonzalez R, Nelson C, Sansone R, Shafer MA. Acceptability and feasibility of an interactive computer assisted intervention to increase chlamydia screening during urgent care visits. J Adolesc Health. 2010;46(Supp.1):S79. [Google Scholar]
- 24. Brown KE, Abraham C, Joshi P, Wallace LM. Sexual health professionals’ evaluations of a prototype computer-based contraceptive planning intervention for adolescents: implications for practice. Sex Health. 2012;9:341-348. [DOI] [PubMed] [Google Scholar]
- 25. Roberto AJ, Zimmerman RS, Carlyle KE, Abner EL, Cupp PK, Hansen GL. The effects of a computer-based pregnancy, STD, and HIV prevention intervention: a nine-school trial. Health Commun. 2007;21:115-124. [DOI] [PubMed] [Google Scholar]
- 26. Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31:143-164. [DOI] [PubMed] [Google Scholar]
- 27. Suarez L, Jorgenson J, Manley T, Yen M, Simeonov I. The Open mHealth Mobile Framework: Supporting Evidence-Based Medicine on Mobile Devices for Patient Care. San Francisco, CA: mHealth Group, University of California San Francisco; 2011. [Google Scholar]
- 28. Bedsider. Real stories. http://bedsider.org/features/17. Accessed January 10, 2017.
- 29. Pazol K, Daniels K, Romero L, Warner L, Barfield W. Trends in Long-Acting Reversible Contraception Use in Adolescents and Young Adults: New Estimates Accounting for Sexual Experience. J Adolesc Health. 2016;59(4):438-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pritt NM, Norris AH, Berlan ED. Barriers and Facilitators to Adolescents’ Use of Long-Acting Reversible Contraceptives. J Pediatr Adolesc Gynecol. 2016. [DOI] [PubMed] [Google Scholar]


