Abstract
Purpose of review
Half the world’s population has access to Internet and technologies, and utilization is near-ubiquitous among providers and key populations. Despite being so well connected; identifying, reaching and linking vulnerable populations to HIV clinical services remains a global challenge. This review highlights the emerging online-to-offline (O2O) models, their potential in scaling-up services, and evaluating impact, and implications for future research.
Recent findings
Globally, four major types of O2O models have been implemented, primarily in the West and Asia, especially among men who have sex with men (MSM) and transgender women (TG). These models have varying levels of impact in terms of reach, engagement, participation, linkage, and ability to track and monitor participants, and assess outcomes. Those integrated with offline sites enable seamless transition, dramatically reduce the O2O linkage time and demonstrate high linkage success (>73%). O2O models are ideal for at-risk, stigmatized, criminalized populations and for scaling-up biomedical prevention interventions such as pre- and post-exposure prophylaxis.
Summary
O2O models represent novel and powerful solutions to reverse the pandemic, and could help fill significant programmatic gaps in tracking individuals through HIV cascades. Providers, especially in resource-limited settings could choose between a variety of current approaches highlighted in this review, and employ no-cost or cost-effective technologies to transform their traditional models and leverage O2O models.
Keywords: O2O models, ICT, service delivery models, key populations, HIV testing, PrEP scale-up
INTRODUCTION
Despite remarkable advances in prevention sciences and compelling evidence that biomedical interventions significantly prevent HIV [1–7], and reduce new HIV infections and AIDS-related mortality [8–11], HIV transmission rates remain common among key populations namely men who have sex with men (MSM), transgender women (TG), people who inject drugs (PWIDs) and sex workers [12]. HIV testing is the first critical entry point into HIV prevention and treatment cascades, however testing uptake remains suboptimal. Almost half of all people living with HIV are unaware of their status [13]. UNAIDS calls for harnessing innovative technologies for expanded prevention uptake to fast-track the response to end AIDS [12]. However, despite exponential proliferation of technologies and near-ubiquitous Internet access among vulnerable populations and healthcare providers [14–17], HIV service delivery for the most part remains traditional. To reverse the pandemic, technology-based service delivery models are urgently needed.
Online-to-Offline (O2O) models integrating emerging technologies in HIV service delivery are a burgeoning area of interest. O2O models represent powerful resources and opportunities to tailor online outreach, identify and engage key populations, and enable seamless transition to HIV clinical services. Understanding how O2O models integrate and harness technologies could help enable rapid and massive scale-up of clinical services globally.
In this review article we describe the types of O2O models implemented among key populations, their impact in bridging the gaps and scaling-up clinical services, and potential for tracking individuals. We then discuss their role in increasing biomedical HIV prevention intervention uptake. In our final section, we argue on the need for implementing such models for other key populations, and in resource-limited settings, and conclude by foregrounding the review’s implications for practice, and directions for future research.
ONLINE-TO-OFFLINE (O2O) MODELS
Simply put, O2O models in HIV service delivery means the linkage between online service utilization and subsequent offline clinical service uptake, i.e., providers reaching out or approached online, identifying vulnerable populations and using a variety of strategies and approaches to encourage, motivate and link people to relevant clinical services.
Although, there are a plethora of online studies targeting populations vulnerable to HIV, compelling studies with the central theme and goal of reaching, identifying and engaging online key populations, optimizing O2O linkages and demonstrating offline service uptake remain limited. We conducted a literature review to identify recent online studies for the scale-up of critical HIV clinical services (HIV prevention, treatment and care) among key populations. We searched PubMed with key terms for Internet, online, social media, eCounseling, technology in combination with HIV testing, prevention, pre-exposure prophylaxis (PrEP), post-exposure prophylaxis (PEP), antiretroviral treatment (ART), treatment, care and these populations. This search was extended to abstracts from the International AIDS Conference. We also searched online for key interventions designed to scale-up services and surveillance data from UNAIDS, WHO, CDC and country-specific sources to identify relevant reports and case studies.
Of 72 unique publications identified in our original search, 14 studies [18–19, 20*, 21*, 22*, 23*, 24*, 25*, 26*, 27*, 28*, 29, 30**, 31**,32*] met the inclusion criteria and were published between April 2015 and March 2017 (Table 1). Inclusion criteria included articles in English that reported data on impact of online interventions in increasing access to HIV and sexually transmitted infections (STIs) related information, reaching and engaging online key populations in HIV/STIs awareness and/or demonstrating testing and prevention services uptake. Authors carefully examined the study design, methods, technology platforms, study location and population, key themes, aims and guiding theories, and outcomes, and placed them in a framework of four major types of O2O models based on previous literature [28, 33–37]. We base our O2O models mainly on the information seeking models of Choo and Marchionini [33–35], Platt’s social media “engagement spectrum” framework [36] and novel PrEP scale-up model proposed by Anand and colleagues [28, 37], that provided us with novel insights into four approaches that could facilitate online to offline linkages, including one-way information provision and information-seeking and use behavior, promotions and advertisements for engagement, bi-directional communication and support to stimulate participation through fostering interactions (multi-way engagement), and lastly an integrated approach incorporating previous approaches together with direct online bookings to receive services at collaborated offline sites. We describe the studies found highlighting the four O2O models, as well as the models impact to facilitate linkages, and then provide some context regarding strengths and issues with measurement and linkages outcomes.
Table 1.
Summary of studies describing the types of Online-to-Offline (O2O) models implemented globally and their impact to scale up HIV clinical services
| Lead author, country | O2O platform | Intervention | Objectives | Target population / Inclusion criteria | Impact of intervention |
|---|---|---|---|---|---|
| Information O2O | |||||
| Eurosurveillance editorial team, 28 European Union (EU) member States [18] | Mobile-optimized, HIV Testing Site Finder, an online tool listing HIV testing clinics across EU states | Enabled online health seeking populations to search for a nearby (geo-location based) HIV testing site by country, town and area code | To increase HIV status awareness and communicate benefits of HIV testing to reduce late diagnosis in Europe | MSM, TG and other key populations | Approximately 40,000 people visited the test finder, and viewed 74,000 testing sites in close proximity |
| Stephan, Tanzania [19] | PMTCT website hosting regularly updated PMTCT-related news, resources and publications | Engaged website visitors in comprehensive information and resources on PMTCT | To increase access to information about prevention among healthcare workers and PMTCT stakeholders in Tanzania | PMTCT healthcare workers and stakeholders in Tanzania | Website received 28,400 visits, with 66,463 page views, over 2 years; 30 % of visits were from returning visitors. The majority of visitors from Tanzania (50 %) and from other African countries (16 %) |
| Promotion O2O | |||||
| Wilkinson, Australia [20*] | Drama Downunder (DDU) social marketing campaign with digital media advertisement i.e. banners on dating website, promotions via outdoor, and print gay media, supported by a range of campaign material | Established an online, open recruitment cohort of MSM and surveyed at approximate 12-month intervals | To promote HIV/STI testing among men who have sex with men (MSM), and evaluate the impact of DDU on HIV, syphilis, gonorrhea, and chlamydia testing | 18 years and above gay and other MSM in Victoria, Australia | High campaign awareness among 242 MSM completing 726 prospective surveys. Post-DDU, gonorrhea test rates increased significantly among HIV-negative MSM. |
| Solorio, USA [21*] | Social marketing campaign, including radio announcements, a website, zip-code based HIV testing locator, social media outreach, a reminder system using mobile technology, print materials, and a toll-free hotline | A cohort of 50 young Latino immigrant MSM were recruited, exposed to campaign and followed over time | To increase HIV testing among young Latino MSM | Latino immigrant, non-self identified MSM, ages 18–30 years old | Increased HIV testing rates at the mid-campaign follow-up (OR 1.7, 95 % CI0.9–3.4, P= 0.1). Campaign received 68,300 impressions from Facebook viewers. A total of 409 interactions with 324 unique followers/fans were recorded. |
| Tang, China [22*] | Crowdsourced video and health marketing video to promote first-time HIV testing | Participants recruited online were screened for eligibility, enrolled, and were randomly assigned to either watch the crowdsourced video or the health marketing video | To compare first-time HIV testing rates among MSM and TG individuals who received a crowdsourced or a health marketing HIV test promotion video | MSM and TG | In the crowdsourced intervention arm, 114 of 307 (37%) reported testing for HIV compared with 111 of 317 (35%) in the health marketing arm. |
| eCounseling O2O | |||||
| Anand, Thailand [23*] | Web-based communications strategy, including website, targeted marketing and promotions, social media and web message boards for online counseling and referrals, and an online tool ‘Testing Site Near You’ to choose nearest available MSM friendly testing site | MSM recruited online through promotions registered on real-time support platforms. Intervention staff assessed risks, shared HIV-related information, offered individualized counseling, and encouraged MSM to undergo HIV screening and provided referrals | Scale-up early HIV testing and counseling (HTC) and linkage to treatment among MSM | MSM | An estimated 11,120 gay men and other MSM received eCounseling; 8,288 MSM were referred to HTC services; 1,223 to STI testing services; 1,112 MSM living with HIV were advised regarding HIV treatment and 278 MSM were advised on PEP and PrEP. The website engaged 1.69 million viewers, and gained more than 8 million page views. |
| Rhodes, USA [24*] | Offer social support in informal, interactions within 4 geographically focused social media sites: Adam4Adam, BlackGayChat, Craigslist, and Gay.com | A repeated cross-sectional matched-pair randomized trial design with 2 intervention and 2 comparison communities to test whether HIV testing changed after 12 months of intervention implementation | To promote and increase HIV testing among MSM and TG who use existing social media designed for social and sexual networking | MSM and TG | At posttest, 63.7% of intervention participants reported HIV testing compared with 42.0% of comparison participants, an almost three times (2.9) higher odds of testing (95% confidence interval, 1.8–4.7). |
| Lampkin, USA [25*] | Passive outreach for delivering STD/HIV prevention services to MSM on Grindr, an all male social networking platform | Educators provided health education and information about available STD/HIV testing, and used a variety of methods to encourage and facilitate users in actualizing referrals | Evaluate outcomes related to online outreach through use of a social networking platform with geolocation features, and impact on STD/HIV prevention and linkage-to care services | MSM | A 14-fold increase in (a 5-year period) the number of MSM reached for counseling and education. 35% of engaged users received some combination of counseling, referrals, testing, treatment, and/or follow-up. |
| Smith, USA [26*] | Proactive outreach on sexual partner-seeking websites (bathhouses, bookstores, sex parties, Craigslist, and anonymous online hookups) | MSM advertising for bareback sex were contacted by trained black gay man for chats and received HIV testing information, risk reduction strategies, and linkage to HIV/STD testing services | Increase HIV awareness, correct risk perceptions and engagement in HIV testing | African American and other minority MSM, age 18 years above | Of 400 contacts advertising for bareback sex and contacted for chats, 30% received a referral to an STD test, and 43.5% received an HIV test as a result of the BARRE program. 89% felt comfortable with proactive outreach. |
| Mashru, Canada [27*] | Telemedicine-videoconferencing technology based infectious disease consultation service to remote communities | Telemedicine-based infectious disease consultation service to remote communities suffering with a heavy burden of infectious disease | To address needs for care in infectious diseases in northwestern Ontario, where important gaps in service to First Nations’ communities continue to exist | Remote/First Nations’ communities | 191 teleconsultations occurred in one year: 76 initial consultations, 82 follow-up appointments and 33 case conferences. |
| Integrated O2O | |||||
| Anand, Thailand [28*] | HIV educational and counseling website, tailored social media PrEP promotions, real-time PrEP eCounseling, free online booking system, auto-generated site- and service-specific e-tickets and Quick Response (QR) codes, collaboration with four private, public and CBOs sites | MSM and TG received eCounseling, counsellors conducted risk assessment, introduced them to PrEP and HIV testing services. Participants prioritized their preferred site/service, completed bookings, and received an e-ticket with a QR code. Participants checked-in at the clinic site and staff scanned the QR code | To increase HIV testing and PrEP uptake among high-risk MSM and TG | MSM and TG | Reached 272,568 people online via the PrEP O2O promotions. 425 MSM and TG received eCounseling and e-tickets. 325 (76.5%) MSM and TG checked-in at clinics and received HIV testing. Nine (2.8%) were diagnosed HIV-positive. Of 316 HIV-negative MSM and TG, 168 (53.2%) started PrEP. |
| Gilbert, Canada [29, 30**] | GetCheckedOnline (GCO), a comprehensive web-based testing service integrated with six sexual health sites for chlamydia, gonorrhea, syphilis, HIV, and HCV testing | Online visitors to the website created an account, completed risk assessment, created and printed a laboratory form, submited specimens, and received results | To increase testing for sexually transmitted and blood-borne infections (STBBIs), reach high-prevalence populations facing testing barriers, and increase clinical STI service capacity | MSM, youth and rural populations | 868 created accounts, 590 (68%) completed risk assessments, and 434 (50%) printed and received lab forms. Of those who printed lab forms, 318 (73.2%) submitted specimens. 96 (30.2%) tested more than once and 10 (3.1%) had a positive STI diagnosis |
| Polilli, Italy [31**] | A Web-based tool with a region wide deployment, information on STIs (HIV, hepatitis B and C, and syphilis), a structured questionnaire called “risk calculator” to assess one’s own risk behaviors and direct booking of their test at one of six sites throughout the region | Users were invited to assess risk behaviors using “risk calculator”, users scoring a moderate or high risk) were encouraged to anonymously (using nickname or fantasy name) make booking for free testing at any of the six linked sites | To recruit persons at high risk of HIV and other STIs and increase HIV/STI screening and linkage to care | High-risk MSM, PWIDs, female, male | About 6,000 users visited the website; >5,000 went through the “risk calculator” and nearly 3,500 booked their testing. Among them, 3,046 (87%) individuals presented for their testing. An overall 7% of unaware STIs, including 0.92% of HIV infections, were diagnosed. |
| Anand, Thailand [32*] | Electronic health record system (EHR) system to enable online consent, knowledge assessment, appointment scheduling, e-counselling, secure access to laboratory results, automated appointment reminders and personalised messaging, and fast-track access to HIV treatment providers (via online registration code) | Participants were enrolled online based on their preference into one of three EHR-supported arms: (1) private clinic-based HIV testing and counselling (HTC); (2) online pretest counselling and private clinic-based HIV testing (hybrid); and (3) online supervised HIV self-testing and counselling (eHTC) | To engage high-risk MSM and TG in online HIV prevention and treatment cascades | MSM and TG | A total of 489 MSM and TG were assessed for their risk, of whom 186 (38%) enrolled into the study. Of the enrolled participants, 89, 72 and 25 chose to join the HTC, hybrid and eHTC arms. HIV prevalence was highest among participants in the eHTC arm (16% vs 1.4% vs 2.2%, P=0.01). |
MSM, men who have sex with men; TG, transgender women; PWIDs, people who inject drugs; FSWs, female sex workers; HIV, human immunodeficiency virus; HCV, hepatitis C virus; STDs, sexually transmitted diseases; STIs, sexually transmitted infections; PMTCT, prevention of mother-to-child transmission of HIV; HTC, HIV testing and counseling; CBOs, community-based organizations; PrEP, pre-exposure prophylaxis; PEP, post-exposure prophylaxis.
TYPES OF O2O MODELS IN HIV SERVICE DELIVERY
We shed light on the four major types of O2O models (Figure 1) based on the key methodologies used, touch points (point of interaction between provider and key populations) optimized and describe them in an ascending order of their potential to track and monitor participants and evaluate impact.
Figure 1. Online-to-Offline (O2O) models in HIV service delivery.
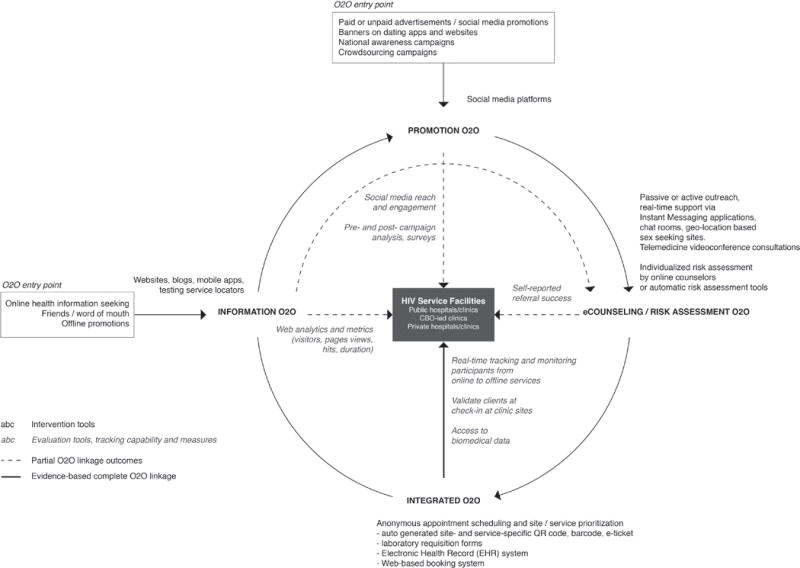
Information and Promotion O2O are the primary entry points into an O2O ecosystem. Information, Promotion and eCounseling O2O rely on participant/self-reported or clinic-reported measures to evaluate linkage success. The Integrated O2O model fosters collaboration between online intervention and offline HIV service delivery site teams to enable seamless O2O transition, and leverages real-time tracking and monitoring technologies to validate participants and demonstrate O2O linkages.
Information O2O
Despite awareness efforts, not knowing the benefits of HIV testing and early antiretroviral treatment (ART) and location of the clinic sites, remain some of the factors behind late testing and diagnosis of HIV, as well as delayed HIV care and ART initiation [38–42]. The Internet has emerged as a preferred and safe haven for at-risk and stigmatized groups, who greatly benefit from guidance in navigating through such resources [43–45]. Sexual minority youth, in fact, are more likely than their heterosexual peers to seek out sexual health information online, and take action (i.e. seek medical care) [17]. The Informational O2O model aims to increase access to credible HIV-related information including locations/details of clinic sites, via traditional desktop and mobile websites, applications and blogs, and testing/care service locators [18] and for this new access to information to subsequently result in increased uptake of testing and prevention services. About 40,000 people visited the European HIV Test Finder, an online tool supporting people to find HIV-testing sites across Europe, and viewed 74,000 testing sites in close proximity [18]. A national website to increase access to information about prevention of mother-to-child transmission of HIV (PMTCT) among healthcare workers and PMTCT stakeholders in Tanzania received a total of 28,400 visits, with 66,463 page views, over 2 years [19].
However, there are noticeable gaps in this model. High level of knowledge does not always translate into service uptake [46]. Although, web metrics provide some insight, evaluating impact remains a challenge. For example, although 40,000 people visited the European HIV Test Finder, and viewed 74,000 testing sites in close proximity [18, 47], less is known on actual numbers receiving testing. Lastly, Information O2O models are passive approaches, as they largely rely on the online health-seeking behaviors of key populations [33, 34], who prioritize information based on site/app credibility and evaluation judgments [48], and are likely to not prefer governmental websites [49] or venture beyond the first page of search engine results [50].
Given, the rise in embedded functionalities and social media integration in the web platforms, stand-alone Information O2O models are continually shifting to Promotion O2O [19].
Promotion O2O
The potential of social networking sites goes beyond just being a cost-effective tool for recruiting ‘hard-to-reach’ populations into online research studies and in randomized control trials (RCTs) [51]. Promotion O2O models harness their proliferation, and embrace this unprecedented resource to proactively reach and engage vulnerable populations for HIV/sexually transmitted infection (STI) testing scale-up [52]. Large-scale, time-based and hyperlocal social media based advertising, and crowdsourcing campaigns are such an example. Increasing HIV/STI testing trends among MSM pre- and post- a social marketing campaign have been reported in Australia [20*]. The 16-week ‘Tu Amigo Pepe’ campaign led to a significant and immediate impact on HIV testing rates among young Latino immigrant MSM [21*]. National HIV testing campaigns in the US have also proven effective in reaching groups disproportionately affected by HIV (black men, MSM and transgender persons), and note a significant increase in new HIV-positive diagnoses during the campaign week (p<0.001) [53]. In Indonesia and Malaysia, culturally-sensitive campaigns have shown great promise [52, 54]. Crowdsourcing campaigns harnessing the power of community engagement also represent powerful, cost-effective tools to promote clinical services, especially in large-population settings. In China, a RCT crowdsourced HIV testing campaign has been largely successful in promoting first-time HIV testing among MSM and TG as compared with a health marketing campaign [22*].
Although Promotion O2O models achieve high reach and engagement, tracking, monitoring and measuring impact remains a challenge as results often coincide with other plausible drivers of testing. Most studies rely on pre and post campaign evaluations through self-reported surveys or overall changes in number of people attending clinic. Efforts are therefore needed to fill evidence gaps in measuring O2O linkages by leveraging innovative technologies with tracking and monitoring features and strengthen evaluation rigour for long-term impact evaluations by paying greater attention to evaluation design, and strengthening outcome indicators [55, 56].
eCounseling O2O (online counseling, risk assessment and referral)
With the rapid proliferation of smartphones, Instant Messaging (IM) apps (WhatsApp, WeChat, Messenger, LINE), popular and free alternatives to SMS/phone calls, geosocial sexual networking apps (Grindr, Jack’d, etc.), and real-time videoconferencing technologies have become increasingly dominant [57–61]. Such rapid technological advancements and exponential rise in usage has profoundly impacted the way people communicate, resulting in a growing need for ‘instant gratification’ [62, 63]. Online groups expect seamless, omnichannel service experience [64] and real-time responses to their inquiries [43, 44]. Drawing on these developments, an eCounseling O2O model, adopts a proactive approach to establish bidirectional communication and foster relationships, address inaccurate perceptions of risk, and facilitate timely referrals to relevant services [23*].
Two parallel approaches have commonly been adopted, often also incorporating components from the former two models [23*]. The former is an unobtrusive approach, designed to be congruent to key populations, where providers or community-based organizations (CBOs)/peer educators don’t ‘target’ or ‘intervene upon’ users, but initiate communication after an interested person approaches. Providers make themselves accessible online to deliver prompt messages/responses, often during business hours in West [24*] and flexible days/hours in Asia [44], conduct risk assessment, encourage and facilitate referrals (send maps to sites, reminders for testing and/or treatment, motivational IM chats, etc.). An eCounseling O2O model in Thailand, offering real-time support to MSM and TG has helped achieve motivational aims, increase perceptions of risk and facilitate >17,000 referrals (in 5-years) to relevant sites/services [23*]. In a RCT of an intervention designed to increase HIV testing among MSM and TG by offering social support (spontaneous interactions delivered by health educators) within 4 geographically focused social media sites, Rhodes and colleagues report a significant increase in self-reported past 12-month HIV testing within intervention communities as compared to control arm (63.7% vs. 42.0%) [24*]. In a suburban California county, passive outreach on Grindr led to a 14-fold increase in MSM reached (in 5-years) for counseling, and 35% (197/562) of engaged users received testing/treatment referrals [25*]. Real-time telemedicine services adopting an unobtrusive approach, where online users contact providers and schedule appointment for a videoconferencing consultation session, are increasingly popular. In San Francisco, face-to-face videoconferencing with medical experts has brought HIV specialty services to patients (which includes HIV testing, treatment, and PrEP, counseling and mental health services). Majority (79%) of the program’s patients stated that they prefer a telemedicine appointment to an in-person visit [65].
The second approach, using online outreach, has also proven effective in engaging key populations in one-on-one, anonymous risk reduction conversations, and successful referrals to testing services (73.5% lead to HIV/STI testing) [26*]. In remote settings or correctional facilities, the nurses or officials perform telemedicine appointments for patients, and physicians/specialists reach out to patients with telehealth. In Ontario, telemedicine-based infectious disease consultation service successfully delivered 191 videoconference consultations to remote communities in one year and high patient satisfaction was reported [27*]. Some studies report high acceptability rates (>60%) with both unobtrusive and outreach approaches [25, 26, 66].
The model helps address inaccurate/low HIV risk perceptions, a critical factor behind late diagnosis [51, 67, 68]. Although, highly responsive to WHO’s global call for demand creation [69], the model is resource intensive on the supply side. Chatbots are increasingly popular [70, 71], although studies comparing effectiveness of automated support with different intensities of individual support are needed.
Integrated O2O
Despite dedicated eCounseling initiatives, and timely referrals to services, fear of disclosing one’s sexual identity, risk behavior and service preference to unknown providers, fragmented experiences [43, 72] and structural barriers [73, 74] act as impediments to testing [75] and early linkage to care [43]. An Integrated O2O model aims to optimize linkages by delivering seamless and fully integrated online and offline services. In addition to incorporating components of the previous three models, the Integrated O2O model fosters collaboration between online intervention teams and offline sites (public/private hospitals and clinics, CBOs or laboratories) enabling key populations to prioritize their preferred site (linked with the program) for receiving services, complete bookings anonymously, schedule testing appointment (via online booking system) and receive booking confirmation (for example, auto-generated site- and service-specific e-tickets, QR codes, barcodes, lab forms). The model leverages technologies with real-time tracking and monitoring features and enables offline clinic site team to validate participants during their visit.
In Thailand, an integrated O2O model demonstrated that a majority (76.4%) of MSM and TG completing online bookings and receiving e-tickets, actually check-in to receive HIV clinical services. Use of QR codes and a free application with real-time monitoring features helped track, validate participants and identify participants’ choice of service. The median (IQR) time between receiving e-ticket and check-in was only 3 (0–7) days [28*]. Interestingly, these results are consistent with an O2O model in Canada comprising of a comprehensive web-based testing service integrated with six sexual health sites integrated with existing sexual health services for scaling STI testing among MSM. Online clients created an account, completed risk assessment, viewed test recommendations and then printed their laboratory test requisition with a unique client code. Clients presented with the laboratory form to one of six designated sites in Vancouver where specimens were collected. Majority 73% of those who printed the lab forms actually submitted specimens [29, 30**]. The requirement to print a laboratory requisition was noted as a major barrier to service uptake and the study recommended barcode scanning from client’s smartphone as future alternative, similar to the strategy used in Thailand [28*]. Impressively, in Italy, implementation of an Integrated O2O model comprising of web-based tool with region wide deployment, ‘risk calculator’ and online booking system for direct booking of test at one of six linked Infectious Diseases Units, resulted in nearly 3,500 users completing online bookings, and 3,046 individuals (87%) presented for offline testing (HIV/STI, hepatitis B virus (HBV) and hepatitis C virus (HCV) testing) in over 15 months [31**]. The model adds to previous three models by explicitly reducing barriers and has demonstrated remarkable online to offline linkage success. Service uptake in this model is high and measurable, many of those who complete risk assessment, receive e-tickets or laboratory requisitions receive offline services.
THE WAY FORWARD
O2O models have largely been implemented in the West and Asia, and evaluated primarily among MSM (and few TG). To reverse the pandemic, it is critical to untap their potential to scale-up biomedical HIV prevention interventions and clinical services among other vulnerable populations in resource-limited settings.
O2O models for biomedical HIV prevention intervention scale-up
Globally, almost 2 million new HIV infections occur each year [76]. Suboptimal control of the epidemic is partially due to vulnerable populations’ insufficient uptake of proven and effective biomedical HIV prevention interventions such as PEP and PrEP [1, 4–7, 77, 78]. To address the scale-up challenges [79, 80] O2O models are being implemented. A novel O2O model piloted by Anand and colleagues, has demonstrated remarkable potential in reducing barriers and scaling PrEP among high-risk, closeted MSM and TG individuals [28*]. Of 316 HIV-negative participants linked to sites, the majority (53.2%) started PrEP as compared to HIV testing alone. In the US, an O2O model piloting comprehensive prevention app has resulted in 9% (8/86) of PrEP-eligible men starting PrEP [81].
PEP must be started within 72 hours after a recent possible exposure to HIV (preferably within 24 hours) [7]. The potential of O2O models to identify recently exposed populations, deliver prompt, real-time responses [23, 44*] and dramatically reduce the linkage time, makes them an incredible PEP service delivery solution. An eCounseling O2O has proven effective in linking recently exposed individuals to PEP services, and those diagnosed early with acute HIV infection to early ART [23, 82].
There is sufficient evidence on the need for and potential of technologies in improving retention in HIV care and PrEP studies, and sustaining ART/PrEP adherence [43, 83–86]. However, delayed linkage into HIV care and late initiation of ART remains a persistent challenge confronting HIV treatment programmes [87]. Innovative technology-based approaches to facilitate online linkage to ART are therefore urgently needed. Online Test and Treat, an implementation science research study using secure Electronic Health Record (EHR) technology to enable online linkage to treatment sites and fast-track access to ART for newly diagnosed participants (performing online HIV self-testing) is currently underway in Thailand [32*, 88].
Other key populations and risk behaviors (female sex workers and people who inject drugs)
One in 3 female sex workers (FSWs) are living with HIV in an estimated 26 countries [89]. Given, FSW’s increasing use of technologies for health information seeking [90, 91], refining and tailoring O2O models is of urgent priority to address substantial gaps in optimal HIV prevention uptake [92, 93].
There is some controversy in terms of the technology utilization among PWIDs, a population most severely affected by HIV and HCV worldwide [94–96]. Although some studies suggest usage is lower than the general population [97], rise in Internet use and digital peer pressure is rapidly fuelling drug use [98, 99]. Given, criminalization of drug use, and stigma against PWIDs prevent their access to services [94], O2O models could be effective to scale-up HIV/HCV/STI testing/treatment and PrEP/PEP services. An integrated O2O model in Canada has successfully engaged 41 (8.1%) PWIDs in testing [30**]. In Italy, 2% (58/3046) of subjects completing online bookings and linked to sites were diagnosed with HCV [31**]. Importantly, tailoring of O2O models is crucial to engage older and/or homeless PWIDs or those with low or no income [100].
Leveraging Integrated O2O model: Implications for practise
Online groups expect a unified experience to enable seamless transition between online and offline services [64, 101]. Omnichannel and seamless experiences as those offered by the Integrated O2O model are therefore key to service delivery in today’s digital age. Although all four types of O2O models summarized in this review represent potential in scaling-up clinical services, we particularly stress on the need for and recommend implementing and deploying Integrated O2O model (an emerging model with studies published recently in 2017), given its potential to address linkage barriers, fill significant programmatic gaps and demonstrate O2O linkage success [28*, 30**, 31**]. We summarize our findings on how providers in low and resource-limited countries could easily implement an Integrated O2O model (Box 1).
Box 1. Leveraging Integrated O2O model.
Recommendations to implement an Integrated O2O model to maximize linkage outcomes.
LEVERAGING INTEGRATED O2O MODEL
Establish “Integrated O2O network” by harnessing collaborations between the online intervention teams and offline providers (public/private healthcare and community centres) to ensure timely O2O transition and seamless linkages
Extend tailored social media promotions and outreach through multiple social media networks of community-based sites staff and popular online platforms used for seeking sex or substance to successfully reach a large number of high-risk groups
Deliver real-time eCounseling and instant text/video support (as compared to time-delayed responses) through instant messaging platforms or applications linked and integrated in one platform to deliver one seamless, cross-channel journey experience
Enable clients to make online bookings anonymously and schedule appointments for their offline clinic visits, issue auto-generated site- and service-specific e-tickets and Quick Response (QR) codes to enable monitoring and check-in by offline site staff
Deploy technologies with real-time tracking and monitoring features to validate participants, collect and track check-in data in real time and monitor live check-in statistics to document linkages (with out relying on participants self-reported data)
CONCLUSION
Although, O2O models are dynamic and will constantly evolve with emerging technologies and varying population needs, this review sheds light on a variety of current models to keep risk populations wedded into O2O ecosystem and boost linkages to clinical services. Going forward, providers would be needed to keep pace with digital trends and experience greater obligation to leverage such models. CBOs will play a vital role in capitalizing on the online service delivery component and could spur linkages. Linkage, retention, monitoring and evaluation outcomes will depend on the types of O2O models deployed. Key populations utilizing services provided within the same O2O ecosystem would enable providers to have a better understanding of their behaviors and outcomes through data analytics, and would be vital to longer-term retention in services. Future research should highlight critical factors to consider while tailoring O2O models for other key populations (especially TG, FSWs and PWIDs), as well as share implementation challenges and successes in resource-limited settings.
KEY POINTS.
Online-to-Offline (O2O) models help identify and seamlessly transition key populations from virtual to critical offline HIV clinical services.
Providers and CBOs (especially in resource limited settings) could harness widely available (low or no cost) technologies to transition their traditional models and leverage O2O models to tailor outreach, optimize experiences and spur linkages.
Evidence suggests that Integrated O2O models dramatically reduce the online to offline linkage time and demonstrate phenomenal linkage success (>73%).
O2O models present innovative monitoring solutions to help fill significant programmatic gaps in tracking individuals through HIV cascades.
The potential of O2O models in delivering prompt real-time responses to key populations and dramatically reducing the online to offline linkage time, makes them a viable service delivery solution for scaling-up biomedical interventions such as PrEP and PEP.
Acknowledgments
T.A. and C.N. were supported by grants from MAC AIDS Fund, ViiV Healthcare and amfAR through a grant from the US National Institutes of Health’s National Institute of Allergy and Infectious Diseases, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Cancer Institute, National Institute of Mental Health, and National Institute on Drug Abuse as part of the International Epidemiology Databases to Evaluate AIDS (IeDEA; U01AI069907). The content is solely the responsibility of the authors and does not necessarily reflect the views or policies of MAC AIDS Fund, ViiV Healthcare or amfAR.
Financial support and sponsorship
None declared.
Footnotes
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cardo DM, Culver DH, Ciesielski CA, et al. A case-control study of HIV seroconversion in health care workers after percutaneous exposure. Centers for Disease Control and Prevention Needlestick Surveillance Group. N Engl J Med. 1997;337:1485–90. doi: 10.1056/NEJM199711203372101. [DOI] [PubMed] [Google Scholar]
- 2.Hosek S, Rudy B, Landovitz R, et al. An HIV pre-exposure prophylaxis demonstration project and safety study for young men who have sex with men in the United States (ATN 110) J Int AIDS Soc. 2015;18:48. [Google Scholar]
- 3.Molina JM, Capitant C, Spire B, et al. On demand PrEP with oral TDF-FTC in MSM: results of the ANRS Ipergay trial; Conference on Retroviruses and Opportunistic Infections (CROI); Seattle, WA. 2015. p. 23LB. [Google Scholar]
- 4.Grant RM, Anderson PL, McMahan V, et al. Results of the iPrEx open-label extension (iPrEx OLE) in men and transgender women who have sex with men: PrEP uptake, sexual practices, and HIV incidence; 20th International AIDS Conference; Melbourne, Australia. 2014. TUAC0105LB. [Google Scholar]
- 5.Grant RM, Anderson PL, McMahan V, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect Dis. 2014;14:820–9. doi: 10.1016/S1473-3099(14)70847-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grant RM, Lama JR, Anderson P, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363:2587–99. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization (WHO) Post-exposure prophylaxis to prevent HIV infection: joint WHO/ILO guidelines on post-exposure prophylaxis (PEP) to prevent HIV infection. Geneva: World Health Organization Department of HIV/AIDS; 2007. [Google Scholar]
- 8.INSIGHT START Study Group. Lundgren JD, Babiker AG, et al. Initiation of Antiretroviral Therapy in Early Asymptomatic HIV Infection. N Engl J Med. 2015;373:795–807. doi: 10.1056/NEJMoa1506816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.TEMPRANO ANRS 12136 Study Group. Danel C, Moh R, et al. A trial of early antiretrovirals and isoniazid preventive therapy in Africa. N Engl J Med. 2015;373:808–22. doi: 10.1056/NEJMoa1507198. [DOI] [PubMed] [Google Scholar]
- 10.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jia Z, Mao Y, Zhang F, et al. Antiretroviral therapy to prevent HIV transmission in serodiscordant couples in China (2003-11): a national observational cohort study. Lancet. 2013;382:1195–203. doi: 10.1016/S0140-6736(12)61898-4. [DOI] [PubMed] [Google Scholar]
- 12.UNAIDS. On the Fast-Track to end AIDS. Geneva: UNAIDS; 2016. [Google Scholar]
- 13.United Nations. On the fast-track to ending the AIDS epidemic: report of the United Nations Secretary-General for the high-level meeting on ending AIDS. United Nations: 2016. [Google Scholar]
- 14.Gould G, Nilforooshan R. WhatsApp Doc? BMJ Innov. 2016;2:109–10. doi: 10.1136/bmjinnov-2016-000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mobasheri MH, King D, Johnston M, et al. The ownership and clinical use of smartphones by doctors and nurses in the UK: a multicentre survey study. BMJ Innov. 2015;1:174–81. [Google Scholar]
- 16.Boonnoon J. ‘Third gender’ users spend most time on the net: survey Bangkok, Thailand: The Nation. http://www.nationmultimedia.com/business/Third-gender-users-spend-most-time-on-the-Net-surv-30240411.html. [Accessed 12 March 2017]
- 17.Mitchell KJ, Ybarra ML, Korchmaros JD, Kosciw JG. Accessing sexual health information online: use, motivations and consequences for youth with different sexual orientations. Health Educ Res. 2014;29:147–57. doi: 10.1093/her/cyt071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eurosurveillance editorial team. New European HIV Test Finder launched during European HIV-Hepatitis Testing Week. Euro Surveill. 2015;20(47) doi: 10.2807/1560-7917.ES.2015.20.47.30072. [DOI] [PubMed] [Google Scholar]
- 19.Stephan G, Hoyt MJ, Storm DS, et al. Development and promotion of a national website to improve dissemination of information related to the prevention of mother-to-child HIV transmission (PMTCT) in Tanzania. BMC Public Health. 2015;15:1077. doi: 10.1186/s12889-015-2422-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *20.Wilkinson AL, Pedrana AE, El-Hayek C, et al. The impact of a social marketing campaign on HIV and sexually transmissible infection testing among men who have sex with men in Australia. Sex Transm Dis. 2016;43:49–56. doi: 10.1097/OLQ.0000000000000380. This study highlights the impact of a social marketing campaign in changing HIV/STI testing rates in an online cohort of MSM pre- and post-campaign. [DOI] [PubMed] [Google Scholar]
- *21.Solorio R, Norton-Shelpuk P, Forehand M, et al. Tu amigo pepe: evaluation of a multi-media marketing campaign that targets young Latino immigrant MSM with HIV testing messages. AIDS Behav. 2016;20:1973–88. doi: 10.1007/s10461-015-1277-6. An interesting study highlighting that HIV testing campaign is a promising approach to increase HIV testing rates among young non-gay identified Latino immigrant MSM. [DOI] [PubMed] [Google Scholar]
- *22.Tang W, Han L, Best J, et al. Crowdsourcing HIV test promotion videos: a noninferiority randomized controlled trial in China. Clin Infect Dis. 2016;62:1436–42. doi: 10.1093/cid/ciw171. This study demonstrates the impact of crowdsourced HIV testing campaign in promoting first-time HIV testing among MSM and TG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *23.Anand T, Nitpolprasert C, Ananworanich J, et al. Innovative strategies using communications technologies to engage gay men and other men who have sex with men into early HIV testing and treatment in Thailand. J Virus Erad. 2015;1:111–5. doi: 10.1016/S2055-6640(20)30483-0. This study highlights that real-time eCounseling helps reduce the time lag in service delivery and represents powerful solution for linking recently exposed populations to PEP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *24.Rhodes SD, McCoy TP, Tanner AE, et al. Using social media to increase HIV testing among gay and bisexual men, other men who have sex with men, and transgender persons: outcomes from a randomized community trial. Clin Infect Dis. 2016;62:1450–3. doi: 10.1093/cid/ciw127. An interesting study highlighting that offering social support within existing, commonly used and geographically focused social media sites helps increase HIV testing. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *25.Lampkin D, Crawley A, Lopez TP, et al. Reaching suburban men who have sex with men for STD and HIV services through online social networking outreach: a public health approach. J Acquir Immune Defic Syndr. 2016;72:73–8. doi: 10.1097/QAI.0000000000000930. This study highlights that passive outreach on Grindr for STD/HIV prevention and linkage-to care leads to a dramatic increase in MSM reached for counseling and, referrals to testing and treatment. [DOI] [PubMed] [Google Scholar]
- *26.Smith C, White M, Ross MW. Experience of online outreach for black MSM populations at high risk for HIV transmission. J Assoc Nurses AIDS Care. 2017;28:25–6. doi: 10.1016/j.jana.2016.09.009. This interesting study illustrates the success of using active outreach strategies (on partner-seeking websites) to engage high-risk MSM in risk reduction conversations and referrals to HIV/STI testing. [DOI] [PubMed] [Google Scholar]
- *27.Mashru J, Kirlew M, Saginur R, Schreiber YS. Management of infectious diseases in remote northwestern Ontario with telemedicine videoconference consultations. J Telemed Telecare. 2017;23:83–7. doi: 10.1177/1357633X15625136. This interesting study highlights the success of telemedicine-videoconferencing technology based infectious disease consultation service in addressing the needs of remote communities. [DOI] [PubMed] [Google Scholar]
- *28.Anand T, Nitpolprasert C, Trachunthong D, et al. A novel Online-to-Offline (O2O) model for pre-exposure prophylaxis and HIV testing scale up. J Int AIDS Soc. 2017;20:1–11. doi: 10.7448/IAS.20.1.21326. This study is one of the first to demonstrate that integrated O2O models optimize linkage to and scale-up PrEP among high-risk MSM and TG, and presents innovative solutions to fill significant programmatic gaps in tracking and monitoring participants along HIV cascades. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gilbert M, Haag D, Hottes TS, et al. Get Checked… Where? The Development of a Comprehensive, Integrated Internet-Based Testing Program for Sexually Transmitted and Blood-Borne Infections in British Columbia, Canada. JMIR Res Protoc. 2016;5:e186. doi: 10.2196/resprot.6293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **30.Gilbert M, Salway T, Haag D, et al. Use of GetCheckedOnline, a Comprehensive Web-based Testing Service for Sexually Transmitted and Blood-Borne Infections. J Med Internet Res. 2017;19:e81. doi: 10.2196/jmir.7097. This study demonstrates that web-based testing services linked with laboratories for specimens’ collection are acceptable and feasible approaches to engage high-risk Canadian MSM in STBBIs testing. The study highlights that most who print the online laboratory form present to receive offline-testing services. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **31.Polilli E, Sozio F, Di Stefano P, et al. Web-based HIV testing in Abruzzo, Italy: analysis of 15-month activity results. AIDS Patient Care STDS. 2016;30:471–5. doi: 10.1089/apc.2016.0082. A very interesting study highlighting that web-based tools enabling online risk assessment and anonymous bookings for free testing at linked Infectious Diseases Units helps reach and diagnose previously unaware HIV/STI infected populations. [DOI] [PubMed] [Google Scholar]
- *32.Anand T, Nitpolprasert C, Kerr SJ, et al. Implementation of an online HIV prevention and treatment cascade in Thai men who have sex with men and transgender women using Adam’s Love Electronic Health Record system. J Virus Erad. 2017;3:15–23. doi: 10.1016/S2055-6640(20)30293-4. This study highlights the potential of Electronic Health Record (EHR) system to engage first time testers in online supervised HIV self-testing, and trends towards better reaching HIV-positive MSM and TG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Choo CW, Detlor B, Turnbull D. Information seeking on the web: an integrated model of browsing and searching. First Monday. 2000;5 [Google Scholar]
- 34.Marchionini GM. Information seeking in electronic environments. Cambridge: Cambridge University Press; 1995. [Google Scholar]
- 35.Hung PW, Johnson SB, Kaufman DR, Mendonça EA. A multi-level model of information seeking in the clinical domain. J Biomed Inform. 2008;41:357–70. doi: 10.1016/j.jbi.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Platt T, Platt J, Thiel DB, Kardia SL. Facebook advertising across an engagement spectrum: a case example for public health communication. JMIR Public Health Surveill. 2016;2:e27. doi: 10.2196/publichealth.5623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Anand T, Nitpolprasert C, Trachunthong D, et al. A novel Online-To-Offline (O2O) model for PrEP and HIV testing scale-up. Vol. 2016. Durban, South Africa: (AIDS 2016). LBPE035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang L, Xiao Y, Lu R, et al. Predictors of HIV testing among men who have sex with men in a large Chinese city. Sex Transm Dis. 2013;40:235–40. doi: 10.1097/OLQ.0b013e31827ca6b9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Evans C, Turner K, Suggs LS, et al. Developing a mHealth intervention to promote uptake of HIV testing among African communities in the UK: a qualitative study. BMC Public Health. 2016;16:656. doi: 10.1186/s12889-016-3278-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Katz IT, Essien T, Marinda ET, et al. Antiretroviral therapy refusal among newly diagnosed HIV-infected adults. AIDS. 2011;25:2177–81. doi: 10.1097/QAD.0b013e32834b6464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gamble T, McCauley M, Talley J, et al. Acceptance of ART in the delay arm after notification of interim study results: data from HPTN 052; 20th Conference on Retroviruses and Opportunistic Infections (CROI); Atlanta, GA. 2013. [Google Scholar]
- 42.Jenness SM, Myers JE, Neaigus A, et al. Delayed entry into HIV medical care after HIV diagnosis: risk factors and research methods. AIDS Care. 2012;24:1240–8. doi: 10.1080/09540121.2012.656569. [DOI] [PubMed] [Google Scholar]
- 43.Anand T, Nitpolprasert C, Kerr SJ, et al. A qualitative study of Thai HIV-positive young men who have sex with men and transgender women demonstrates the need for eHealth interventions to optimize the HIV care continuum. AIDS Care. 2017;7:1–6. doi: 10.1080/09540121.2017.1286288. [DOI] [PubMed] [Google Scholar]
- 44.Anand T, Nitpolprasert C, Ananworanich J, et al. Characteristics of HIV risks among Thai young men who have sex with men and transgender youth using an eCounseling platform. Vol. 2016. Durban, South Africa: (AIDS 2016). TUPEC229. [Google Scholar]
- 45.Oppong Asante K. HIV/AIDS knowledge and uptake of HIV counselling and testing among undergraduate private university students in Accra, Ghana. Reprod Health. 2013;10:17. doi: 10.1186/1742-4755-10-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tsereteli N, Chikovani I, Chkhaidze N, et al. HIV testing uptake among female sex workers and men who have sex with men in Tbilisi, Georgia. HIV Medicine. 2013;14:29–32. doi: 10.1111/hiv.12065. [DOI] [PubMed] [Google Scholar]
- 47.Frellick M. Apps and Social Media Can Reach High-Risk HIV Populations. HIV Drug Therapy. 2016 http://www.medscape.com/viewarticle/871137. [Accessed 12 March 2017]
- 48.Allam A, Schulz PJ, Nakamoto K. The impact of search engine selection and sorting criteria on vaccination beliefs and attitudes: two experiments manipulating Google output. J Med Internet Res. 2014;16:e100. doi: 10.2196/jmir.2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wilkerson JM, Smolenski DJ, Horvath KJ, et al. Online and offline sexual health-seeking patterns of HIV-negative men who have sex with men. AIDS Behav. 2010;14:1362–70. doi: 10.1007/s10461-010-9794-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Eysenbach G, Köhler C. How do consumers search for and appraise health information on the world wide web? Qualitative study using focus groups, usability tests, and in-depth interviews. BMJ. 2002;324:573–7. doi: 10.1136/bmj.324.7337.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vial AC, Starks TJ, Parsons JT. Relative efficiency of field and online strategies in the recruitment of HIV-positive men who have sex with men. AIDS Educ Prev. 2016;27:103–11. doi: 10.1521/aeap.2015.27.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Anand T, Nitpolprasert C, Sohn AH, et al. Temanteman.org, an integrated public-private sector communication strategy to scale up early and routine HIV testing among most-at-risk populations (MARPs) in Indonesia. Vol. 2014. Melbourne, Australia: (AIDS 2014). TUPE174. [Google Scholar]
- 53.Lecher SL, Hollis N, Lehmann C, et al. Evaluation of the impact of national HIV testing day - United States, 2011-2014. MMWR Morb Mortal Wkly Rep. 2016;65:613–8. doi: 10.15585/mmwr.mm6524a2. [DOI] [PubMed] [Google Scholar]
- 54.Tey K. Website to raise awareness on AIDS The Star Online. http://www.thestar.com.my/news/community/2014/12/01/website-to-raise-awareness-on-aids-online-resource-centre-launched-to-provide-relevantinformation-a/. [Accessed 12 March 2017]
- 55.Bates I. Designing and measuring the progress and impact of health research capacity strengthening initiatives. BMC Proc. 2015;9:S9. doi: 10.1186/1753-6561-9-S10-S9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Maleka EN. Monitoring and evaluation of sport-based HIV/AIDS awareness programmes: strengthening outcome indicators. SAHARA J. 2016;14:1–21. doi: 10.1080/17290376.2016.1266506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Alpeyev P, Nakamura Y, Leung A. Has Japan’s most popular messaging app peaked? Bloomberg. 2016 https://www.bloomberg.com/graphics/2016-line-ipo/. [Accessed 12 March 2017]
- 58.Munroe I. Messaging app wars take new turn with Line IPO. 2016 http://www.aljazeera.com/news/2016/07/messaging-app-wars-turn-line-ipo-160713112038045.html. [Accessed 12 March 2017]
- 59.Kang CR, Bang JH, Cho SI, et al. Patients presenting with advanced human immunodeficiency virus disease: epidemiological features by age group. J Korean Med Sci. 2016;31(2):178–82. doi: 10.3346/jkms.2016.31.2.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Statista. Most popular mobile messaging apps. 2017 https://www.statista.com/statistics/258749/most-popular-global-mobile-messenger-apps/. [Accessed 12 March 2017]
- 61.Pew Research Center. Mobile Fact Sheet. 2017 http://www.pewinternet.org/fact-sheet/mobile/. [Accessed 12 March 2017]
- 62.Meena PS, Mittal PK, Solanki RK. Problematic use of social networking sites among urban school going teenagers. Ind Psychiatry J. 2012;21:94–7. doi: 10.4103/0972-6748.119589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schilhab T. Adaptive smart technology use: the need for meta-self-regulation. Front Psychol. 2017;8:298. doi: 10.3389/fpsyg.2017.00298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Juaneda-Ayensa E, Mosquera A, Sierra Murillo Y. Omnichannel customer behavior: key drivers of technology acceptance and use and their effects on purchase intention. Front Psychol. 2016;7:1117. doi: 10.3389/fpsyg.2016.01117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.UCSF 360 Wellness Center. Urban HIV Telemedicine Program San Francisco, USA. 2016 http://360.ucsf.edu/content/urban-hiv-telemedicine-program. [Accessed 21 May 2017]
- 66.Sun CJ, Stowers J, Miller C, et al. Acceptability and feasibility of using established geosocial and sexual networking mobile applications to promote HIV and STD testing among men who have sex with men. AIDS Behav. 2015;19:543–52. doi: 10.1007/s10461-014-0942-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ganju D, Ramesh S, Saggurti N. Factors associated with HIV testing among male injecting drug users: findings from a cross-sectional behavioural and biological survey in Manipur and Nagaland, India. Harm Reduct J. 2016;13:21. doi: 10.1186/s12954-016-0110-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Runhua Li, Xiaohong Pan, Qiaoqin Ma, et al. Prevalence of prior HIV testing and associated factors among MSM in Zhejiang Province, China: a cross-sectional study. BMC Public Health. 2016;16:1152. doi: 10.1186/s12889-016-3806-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.World Health Organization (WHO) Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations – 2016 update. Geneva: WHO; 2016. [PubMed] [Google Scholar]
- 70.Lotz B. Facebook Messenger chatbot aims to prevent mother to child HIV transmission. 2016 http://www.htxt.co.za/2016/07/19/momconnect-aims-to-prevent-mother-to-child-hiv-transmission-with-a-facebook-messenger-bot/. [Accessed 12 March 2017]
- 71.Kruk ME, Kujawski S, Moyer CA, et al. Next generation maternal health: external shocks and health-system innovations. Lancet. 2016;388:2296–306. doi: 10.1016/S0140-6736(16)31395-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bajunirwe F, Tumwebaze F, Abongomera G, et al. Identification of gaps for implementation science in the HIV prevention, care and treatment cascade; a qualitative study in 19 districts in Uganda. BMC Res Notes. 2016;9:217. doi: 10.1186/s13104-016-2024-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Beattie TS, Bhattacharjee P, Suresh M, et al. Personal, interpersonal and structural challenges to accessing HIV testing, treatment and care services among female sex workers, men who have sex with men and transgenders in Karnataka state, South India. J Epidemiol Community Health. 2012;66:ii42–8. doi: 10.1136/jech-2011-200475. [DOI] [PubMed] [Google Scholar]
- 74.Woodford MR, Chakrapani V, Newman PA, Shunmugam M. Barriers and facilitators to voluntary HIV testing uptake among communities at high risk of HIV exposure in Chennai, India. Glob Public Health. 2015:1–17. doi: 10.1080/17441692.2015.1057757. [DOI] [PubMed] [Google Scholar]
- 75.Underhill K, Morrow KM, Colleran C, et al. A qualitative study of medical mistrust, perceived discrimination, and risk behavior disclosure to clinicians by U.S. male sex workers and other men who have sex with men: implications for biomedical HIV prevention. J Urban Health. 2015;92(4):667–86. doi: 10.1007/s11524-015-9961-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fact sheet November 2016. Geneva: UNAIDS; 2016. [Google Scholar]
- 77.Krakower DS, Jain S, Mayer KH. Antiretrovirals for primary HIV prevention: the current status of pre- and post-exposure prophylaxis. Curr HIV/AIDS Rep. 2015;12:127–38. doi: 10.1007/s11904-014-0253-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.World Health Organization (WHO) Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. Geneva: WHO; 2015. [PubMed] [Google Scholar]
- 79.Cáceres CF, Bekker LG, Godfrey-Faussett P. No one left behind: how are we doing in the roll-out of PrEP as part of combination HIV prevention? J Int AIDS Soc. 2016;19:1–3. doi: 10.7448/IAS.19.7.21364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zablotska I, Grulich AE, Phanuphak N, et al. PrEP implementation in the Asia-Pacific region: opportunities, implementation and barriers. J Int AIDS Soc. 2016;19:21119. doi: 10.7448/IAS.19.7.21119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sullivan PS, Driggers R, Stekler JD, et al. Usability and Acceptability of a Mobile Comprehensive HIV Prevention App for Men Who Have Sex With Men: A Pilot Study. JMIR Mhealth Uhealth. 2017;5:e26. doi: 10.2196/mhealth.7199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ananworanich J. HIV DNA set point is rapidly established in acute HIV infection and dramatically reduced by early ART. EBioMedicine. 2016;11:68–72. doi: 10.1016/j.ebiom.2016.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kanters S, Park JJH, Chan K, et al. Interventions to improve adherence to antiretroviral therapy: a systematic review and network meta-analysis. Lancet HIV. 2016;4(1):e31–e40. doi: 10.1016/S2352-3018(16)30206-5. [DOI] [PubMed] [Google Scholar]
- 84.Ware NC, Pisarski EE, Tam M, et al. The Meanings in the messages: how SMS reminders and real-time adherence monitoring improve antiretroviral therapy adherence in rural Uganda. AIDS. 2016;30:1287–94. doi: 10.1097/QAD.0000000000001035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Montaner J, Rojo P, Anand T, Rockstroh J. Highlights of the International Congress on Drug Therapy in HIV Infection, 23–26 October 2016, Glasgow, UK. J Virus Erad. 2017;3:97–100. doi: 10.1016/S2055-6640(20)30290-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Haberer JE, Musiimenta A, Atukunda EC, et al. Short message service (SMS) reminders and real-time adherence monitoring improve antiretroviral therapy adherence in rural Uganda. AIDS. 2016;30:1295–300. doi: 10.1097/QAD.0000000000001021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mugglin C, Estill J, Wandeler G, et al. Loss to programme between HIV diagnosis and initiation of antiretroviral therapy in sub-Saharan Africa: Systematic review and meta-analysis. Trop Med Int Health. 2012;17:1509–20. doi: 10.1111/j.1365-3156.2012.03089.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Anand T, Nitpolprasert C, Kerr SJ, et al. Factors influencing and associated with the decision to join in Thailand’s first online supervised HIV self-testing and counselling initiative. J Int AIDS Soc. 2016;19:228. [Google Scholar]
- 89.Baral S, Beyrer C, Muessig K, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:538–49. doi: 10.1016/S1473-3099(12)70066-X. [DOI] [PubMed] [Google Scholar]
- 90.Brody C, Tatomir B, Sovannary T, et al. Mobile phone use among female entertainment workers in Cambodia: an observation study. Mhealth. 2017;3:3. doi: 10.21037/mhealth.2017.01.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hong Y, Li X, Fang X, et al. Internet use among female sex workers in China: implications for HIV/STI prevention. AIDS Behav. 2011;15:273–82. doi: 10.1007/s10461-010-9846-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Shokoohi M, Karamouzian M, Khajekazemi R, et al. Correlates of HIV testing among female sex workers in Iran: findings of a national bio-behavioural surveillance survey. PLoS ONE. 2016;11:e0147587. doi: 10.1371/journal.pone.0147587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Xu J, Brown K, Ding G, et al. Factors associated with HIV testing history and HIV-test result follow-up among female sex workers in two cities in Yunnan, China. Sex Transm Dis. 2011;38:89–95. doi: 10.1097/OLQ.0b013e3181f0bc5e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.UNAIDS. Do no harm: health, human rights and people who use drugs. Geneva: UNAIDS; 2016. [Google Scholar]
- 95.Thein HH, Yi Q, Dore GJ, Krahn MD. Natural history of hepatitis C virus infection in HIV-infected individuals and the impact of HIV in the era of highly active antiretroviral therapy: a meta-analysis. AIDS. 2008;22:1979–91. doi: 10.1097/QAD.0b013e32830e6d51. [DOI] [PubMed] [Google Scholar]
- 96.UNAIDS. Global AIDS Update. Geneva: UNAIDS; 2016. [Google Scholar]
- 97.Genz A, Kirk G, Piggott D, et al. Uptake and Acceptability of Information and Communication Technology in a Community-Based Cohort of People Who Inject Drugs: Implications for Mobile Health Interventions. JMIR Mhealth Uhealth. 2015;3:e70. doi: 10.2196/mhealth.3437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mounteney J, Bo A, Oteo A. The internet and drug markets. Luxembourg: European Monitoring Centre for Drugs and Drug Addiction. 2016 [Google Scholar]
- 99.Hearne E, Grund JC, Van Hout MC, McVeigh J. A scoping review of home-produced heroin and amphetamine-type stimulant substitutes: implications for prevention, treatment, and policy. Harm Reduct J. 2016;13:14. doi: 10.1186/s12954-016-0105-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Collins KM, Armenta RF, Cuevas-Mota J, et al. Factors associated with patterns of mobile technology use among persons who inject drugs. Subst Abus. 2016;37:606–12. doi: 10.1080/08897077.2016.1176980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Park A, Chang H, Lee KJ. Action research on development and application of Internet of Things services in hospital. Healthc Inform Res. 2017;23:25–34. doi: 10.4258/hir.2017.23.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]


