Abstract
Objective
We examined the relation between temperament and preoperative anxiety in 40 children (aged 8–13) who were undergoing elective surgery one week prior to surgery Time 1 (T1) and on the day of surgery Time 2 (T2).
Method
Children’s temperamental shyness was examined using the Colorado Childhood Temperament Inventory at T1, and preoperative anxiety was assessed using the Children’s Perioperative Multidimensional Anxiety Scale at T1 and T2.
Results
We found that temperamental shyness predicted lower preoperative anxiety at T1 (β = −10.78; p = .03) and at T2 (β = −12.31; p = .03).
Conclusion
We speculate that temperamentally shy children although seemingly paradoxical, our findings suggest that temperamentally shy children may have developed coping strategies from dealing with persistent anxiety in their everyday environments, and they may use these coping skills in the surgical context. These findings are discussed in terms of their theoretical and practical implications for understanding person by context interactions and managing children’s preoperative anxiety.
Keywords: adolescent, anxiety, child, preoperative period, shyness, temperament
Résumé
Objectif
Nous avons examiné la relation entre le tempérament et l’anxiété préopératoire chez 40 enfants (de 8 à 13 ans) qui allaient subir une chirurgie élective une semaine avant l’opération, Temps 1 (T1), et le jour de l’opération Temps 2 (T2).
Méthode
La timidité caractérielle des enfants a été examinée à l’aide de l’inventaire du tempérament des enfants du Colorado au T1, et l’anxiété préopératoire a été évaluée à l’aide de l’échelle d’anxiété multidimensionnelle périopératoire des enfants aux T1 et T2.
Résultats
Nous avons constaté que la timidité caractérielle prédisait une anxiété préopératoire plus faible au T1 (β = −10,78; p = 0,03) et au T2 (β = −12,31; p = 0.03).
Conclusion
Nous déduisons que les enfants caractériellement timides peuvent avoir développé des stratégies d’adaptation du fait de vivre avec une anxiété persistante dans leur environnement quotidien, et qu’ils peuvent utiliser ces habiletés d’adaptation dans le contexte chirurgical. Ces résultats sont discutés sous l’angle de leurs implications théoriques et pratiques pour comprendre la personne par les interactions contextuelles et prendre en charge l’anxiété préopératoire des enfants.
Mots clés: adolescent, anxiété, enfant, période préopératoire, timidité, tempérament
The psychological sciences have come under considerable scrutiny recently for the lack of reproducibility of empirical findings (Lindsay, 2015). In a recent opinion article published in the New York Times, Barrett (2015) proposed that the main reason for failures to replicate study results in psychology experiments was the failure to consider context. Barrett described this non-reproducibility of results as a typical path of scientific discovery and also stressed the importance of explaining the phenomenon under study based on context.
In personality science, the consideration of context for reliably predicting behavior has been a central theme for decades. Allport (1937) argued that individuals exhibit different and unique behavioral patterns across contexts. Lewin (1951) articulated a more systematic account of person by context interactions. According to Lewin, human behavior (B) was a function of the person’s disposition (P) and the context or situation (S), expressed as B = f(P,S). These three variables formed the “personality triad” (Funder, 2006). Accordingly, people vary their behaviors across contexts, but maintain their individual differences at the same time (Funder, Guillaume, Kumagai, Kawamoto, & Sato, 2012).
Several personality or temperamental types have been identified in person by context interactions (see Rapee, 2002, for a review). One personality style that has been examined across different contexts is shyness. Shyness reflects an anxious pre-occupation with the self in response to real or imagined social situations (Melchoir & Cheek, 1990). Although shyness is a ubiquitous phenomenon that most people experience at some point in their lives (Zimbardo, 1977), some people are characterized by temperamental shyness, an early developing and stable form of shyness observed and stable across time and context (see Schmidt & Buss, 2010). Indeed, temperamental shyness has been shown to be associated with increased anxiety during situations involving social presentation (Schmidt, Fox, Schulkin, & Gold, 1999) and anxiety disorders later in life (Beidel & Turner, 2007; Chronis et al., 2009).
Temperamental shyness by context interactions have been studied in children as well. Kagan and his colleagues have described children who exhibit fear and wariness to unfamiliarity across social and non-social contexts as temperamentally shy (Coplan, Prakash, O’Neil, & Mandana, 2004; Kagan, Reznick, & Snidman, 1988). Kagan’s group found that temperamentally shy children displayed similar anxiety across two laboratory visits, but when comparing scores between two different contexts (i.e., laboratory and home), anxiety scores were not correlated, highlighting the impact of contextual factors on the manifestation of anxiety (Garcia-Coll, Kagan, & Reznick, 1984).
In other studies of children, Rubin and colleagues (Rubin, Hastings, Stewart, Henderson, & Chen, 1997) showed that there was a subset of temperamentally shy children who behaved similarly across social and non-social laboratory contexts, leading his group to conclude “some of the [temperamentally shy] children, all of the time” which highlights that although temperamental shyness is related to social novelty, some shy children also manifest fear in nonsocial, unfamiliar settings as well. More recently, Coplan and his colleagues (Coplan, DeBow, Schneider, & Graham, 2009) reported that temperamentally shy children exhibited similar social behaviors inside and outside of school. Temperamentally shy preschool-aged children displayed more reticent (on looking, unoccupied) behaviors and anxiety during free play at school, participated less in structured social activities outside of school, and were more likely to engage in dyadic play at home with a single friend than non-shy children. Overall, the extant studies suggest that temperamental shyness in children is consistent across time and situation but may also vary between some normative contexts (Coplan et al., 2009; Garcia-Coll et al., 1984; Rubin et al., 1997).
One long-standing question is whether the anxiety of temperamentally shy children in normative social and nonsocial contexts would generalize to non-normative contexts. Existing studies have been conducted largely in familiar (e.g., the home) and everyday normative environments (e.g., school) and/or the laboratory with familiar adults and settings. Accordingly, we do not know whether the anxiety observed in temperamentally shy children in these contexts generalizes to non-normative stressful contexts. In order to better understand whether temperamental shyness is a personality trait that is context specific and/or sensitive to context, it is of importance to examine the phenomenon in other contexts to enhance prediction of anxiety and the reproducibility of findings.
The surgical setting allows an unique opportunity to examine whether the relation between temperamental shyness and anxiety in everyday environments and the laboratory generalized to a presumably unfamiliar, non-normative environment, encompassing both non-social (e.g., sight of stretchers and surgical tools, smell of disinfectants, unfamiliar environment) and social stimuli (e.g., nurses, doctors, other pediatric patients and families). As well, the present study could potentially identify children who are at risk for preoperative anxiety. Since the majority of children undergoing surgery experience significant distress (see Chow et al., 2015, for a review; Kain, Mayes, O’Connor, & Cicchetti, 1996; Kain, Mayes, Caldwell-Andrews, Karas, & McClain, 2006), and as preoperative anxiety is associated with numerous adverse postoperative outcomes such as increased postoperative pain, analgesic consumption, general anxiety, and sleeping problems and decreased postoperative eating improvement (Chieng, Chan, Klainin-Yobas, & He, 2014; Kain et al., 2006), the findings of this study could inform future research into the influence that temperament has on preoperative anxiety and its associated negative outcomes. Accordingly, the results of the present study could therefore help guide the development of intervention strategies to optimize perioperative care.
Here we conducted a preliminary investigation using the perioperative environment and surgery as non-normative, stressful, context which involves social and nonsocial elements. More specifically, we examined whether the relation between children’s temperamental shyness and anxiety reported in the extant literature would generalize to a unfamiliar, non-normative, surgical context.
We collected measures of children’s temperamental shyness at a preoperative clinic visit to the hospital prior to surgery and preoperative anxiety ratings at this time and on the day of surgery in children who were undergoing elective surgical procedures. We predicted that increases in temperamental shyness would be associated with increases in preoperative anxiety.
This a priori prediction was based on findings from the extant literature that have examined links between temperament and anxiety in children, both inside and outside of the surgical contexts. For example, Kain and colleagues (Kain, Mayes, Weisman, & Hofstadter, 2000) found children who received lower ratings of sociability (i.e. higher shyness) exhibited increased preoperative anxiety in the preoperative holding area. Other studies that have examined the relation between shyness and anxiety in non-surgical context have also demonstrated similar results to the preoperative setting. For example, Kagan and his group (Kagan, Reznick, & Snidman, 1987) found that shy or inhibited children tend to become more anxious in unfamiliar social and non-social settings. than non-shy children. Moreover, Schmidt and colleagues (1997; 1999; 2005) found that shy children displayed relatively higher levels of morning salivary cortisol levels (a measure of stress reactivity) prior to any social interactions and greater increases in right frontal EEG activity (another measure of stress reactivity) during a self-presentation task than non-shy children.
Method
Participants
A total of 69 children and families were approached and 29 were excluded because they declined participation (n=20) or did not meet our eligibility criteria (n=9). Forty children (21 boys, 19 girls, Mage = 9.19 years, age range: 7.15–11.23 [boys] and Mage = 9.11 years, age range: 7.26–10.96 [girls]) and their parents were therefore included in this study. They were recruited during the child’s preoperative clinic visit, occurring an average of 11 days (M = 10.86, SD = 10.28) before surgery. The mean age of children’s parents was Mage = 41.00 years (SD = 7.21) for boys, and Mage = 38.44 years (SD = 8.99) for girls. Recruitment was limited to elective outpatient otolaryngologic (Ear-Nose-Throat [ENT]) surgical procedures (i.e., tonsillectomy and adenoidectomy, etc.) at the McMaster Children’s Hospital Children’s Hospital located in Southwestern Ontario, Canada. Children diagnosed with significant neurodevelopmental disorders (e.g., organic brain disorders, visual and/or hearing impairments, etc.), and families who were unable to provide assent and consent due to language barriers were not eligible for participation.
Measures
Colorado Child Temperament Inventory (CCTI; Buss & Plomin, 1984; Rowe & Plomin, 1977). The CCTI is a 30-item questionnaire that uses parent-reports to assess temperament using a Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The scale measures temperament on six dimensions: shyness, sociability, emotionality, activity, attention-span persistence, and soothability. This scale has been widely-used in studies that examined individual differences of shyness in school-aged populations (Pérez-Edgar & Fox, 2003; Tsui, Lahat, & Schmidt, 2017). The majority of the CCTI temperament measures were completed by mothers (80%). The remainders were provided by fathers (17.5%) or other guardians (2.5%). Of particular interest to this study was the subscale measuring shyness [(e.g., “Child tends to be shy”). The 5-item shyness subscale had good internal consistency in the present study (Cronbach’s α = 0.77). Given that temperament is a stable characteristic, children’s temperament was assessed only during their preoperative clinic visit (T1) in order to reduce participant burden during the day of surgery.
Children’s Perioperative Multidimensional Anxiety Scale (CPMAS; Chow, Van Lieshout, Buckley, & Schmidt, 2016). The CPMAS is a recently developed and validated self-report scale designed to measure children’s state anxiety within a surgical context. This scale has been validated on school-aged children between the ages of 7–13 years. The CPMAS contains five items, to which the child responds on a visual analog scale that ranges from 0 to 100. The CPMAS was found to have strong internal consistency (Cronbach’s α > 0.89), and good test-retest reliability (Intraclass Correlation Coefficient = 0.71) in the present study. A sample question from the CPMAS includes: “Right now, how worried are you?” 0 = (not at all worried) and 100 = (very worried). Children’s anxiety was assessed at two time-points: preoperatively, approximately one week prior to surgery (T1), and immediately before surgery (T2). CPMAS anxiety scores were stable between T1 and T2 (r = .66, p < .01).
Procedure
All children between the ages of 7–11 receiving ENT surgeries were approached in the waiting room before their preoperative clinic appointment and invited to participate in the study at T1. As part of the standard of care at the McMaster Children’s Hospital, children and families met with a child life specialist, a pediatric nurse, and an anesthetist during this visit. After providing consent and assent, the parent completed the CCTI measure at T1, and the child completed the CPMAS at T1 and T2. Demographic information such as sex, age, previous hospitalizations, parental sex, and parental age were also collected during this time.
On the day of surgery, children and families were greeted by a research assistant in the Same-Day-Surgery waiting room. Children and families were prepared by a pediatric nurse (i.e., changing of gowns and vital sign recordings) up to two hours before their operation. Approximately 30 minutes prior to surgery, families were asked to move to the holding area outside of the operating room (OR), where the child completed the CPMAS to report on their anxiety levels immediately prior to surgery. Children and families were then accompanied by a nursing staff into the OR ten minutes before their operation.
All procedures were approved by the Hamilton Integrated Research Ethics Board.
Participant Attrition
Five children were lost to follow-up between T1 and T2. Only data collected at T1 were analyzed for these five families. A chi-square analysis revealed that there was a significant difference in sex (5 boys and 0 girls) between those who did and those who did not complete the study χ2 (1, N = 40) = 5.17, p < .023. No significant differences were found for child’s age, parental age, previous hospitalizations, or preoperative preparations by a Child Life specialist between those who remained in the study and those who dropped out (p > 0.05).
Statistical Analysis
We conducted chi-square tests and independent-samples t-tests to assess differences between participant sex for all demographic data and outcome measures. No group differences were observed between male and female children on the temperamental shyness and CMPAS measures at T1 and T2 (p > 0.05). As well, these measures were not related to participant’s age. Data were normally distributed and met assumptions for t-tests and linear regression. A paired-samples t-test was conducted to compare the CPMAS scores at T1 and T2. Linear regression was used to examine the relation between temperamental shyness and preoperative anxiety at T1 and T2. In the first model, temperamental shyness scores were entered with T1 CPMAS continuous scores as the dependent measure. In the second model, temperamental shyness scores served as the predictor with T2 CPMAS scores as the dependent measure. Covariates including the child’s sex, age, and previous hospitalizations were examined in the regression models. We intentionally did not control for T1 CPMAS scores in the second model because we treated T1 and T2 as distinct contexts. All statistical analyses were performed using SPSS Version 23.0, with significance levels set at α = 0.05.
Power analysis for a linear regression was conducted in G-POWER to determine a sufficient sample size using an alpha of 0.05, a power of 0.80, and a large effect size (f2 = 0.35) (Faul, Erdfelder, Buchner, & Lang, 2009). Based on these parameters, a sample size of 25 met these assumptions.
Results and Discussion
Table 1 shows the sample characteristics of the children and families in the study.
Table 1.
Sample characteristics of children and families (N=40)
| Sample | Characteristics | n = 40 |
|---|---|---|
| Children | ||
| Sex, n (Boys/Girls) | 21/19 | |
| Age, M ± SD (in years) | 9.15 ± 1.93 | |
| Child life Specialist Use, n (Yes/No) | 40/0 | |
| Previous Hospitalization, n (Yes/No) | 9/31 | |
| Parents | ||
| Mother/Father/Other*, n (Mother/Father/Other) | 32/7/1 | |
| Age, M ± SD (in years) | 39.72 ± 8.13 | |
Grandparent or Caregiver
There were no statistically significant differences in CPMAS scores at T1 (M=200.86, SD=143.02) and T2 (M=231.57, SD=153.67); t(35)=−1.479, p = 0.148.
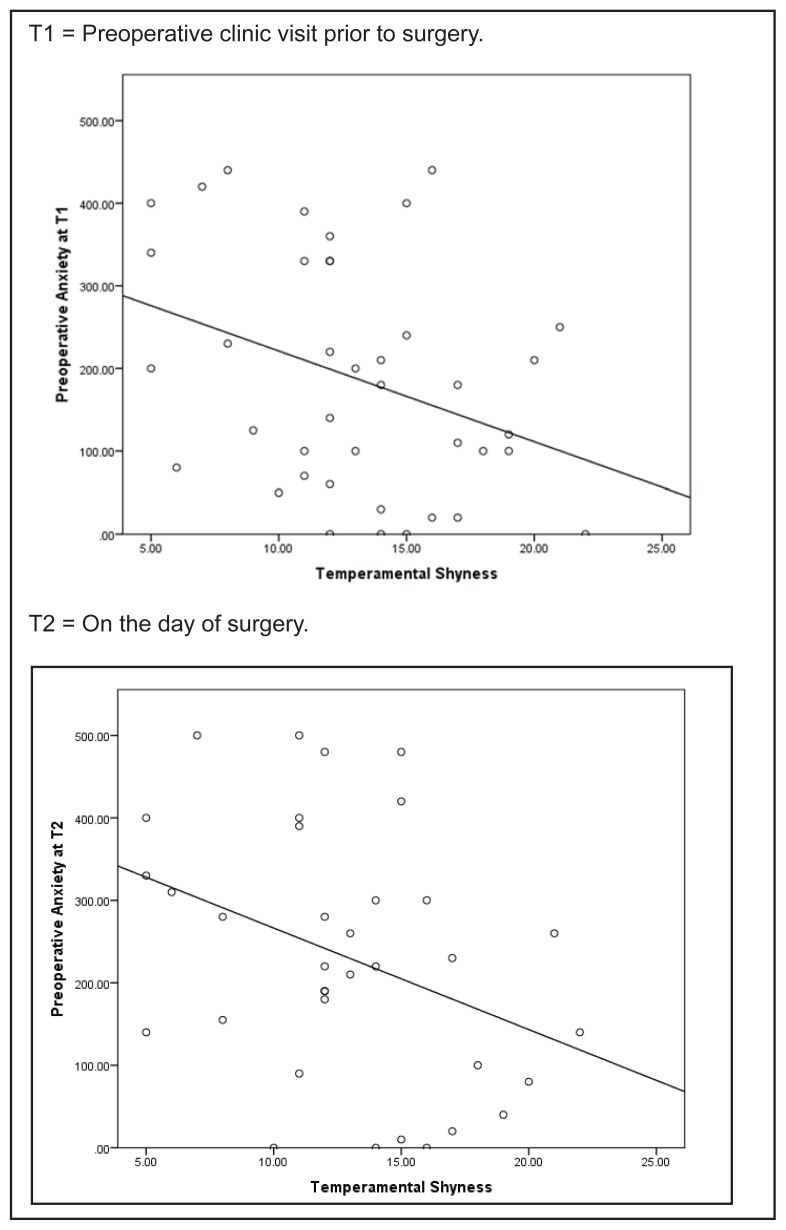
Table 2 summarizes the results of all linear regression models. Contrary to prediction, increases in children’s shyness were associated with decreases in preoperative anxiety at T1 (β = −10.78; p = .03) and at T2 (β = −12.31; p = .03) (see Figure 1).
Table 2.
Linear regressions of temperamental shyness predicting children’s preoperative anxiety (CPMAS) at Time 1 (T1) and Time 2 (T2)
| Predictor | Pre-operative Visit (T1) | Day of Surgery Visit (T2) | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Unstandardized Beta | S.E. | R2 | ΔR2 | Unstandardized Beta | S.E. | R2 | ΔR2 | |
| Temperamental shyness | −10.78* | 4.89 | .12* | .09* | −12.31* | 5.58 | .13 | .10 |
S.E. = standard error; N = 40;
p ≤ .05.
Note: Temperamental shyness remained a significant predictor after controlling for sex, age and previous hospitalization at T1 and T2
Figure 1.
Scatterplots of the relation between children’s temperamental shyness and preoperative anxiety (CPMAS score) at (A) Time1 (T1) and (B) Time 2 (T2).
We found, unexpectedly, that temperamental shyness was inversely related to preoperative anxiety. This result was not consistent with the findings of Kain and his colleagues (2000) who found a relation between reduced sociability (i.e., increased shyness) and increased preoperative anxiety in children undergoing surgery. As well, contrary to existing literature on shyness by context interactions in children, our preliminary data suggest that temperamental shyness was associated with experiencing less preoperative anxiety in a surgical context. This finding was not consistent with previous findings involving temperamentally shy children who have been shown to behave consistently across contexts (Coplan et al., 2009; Rubin, et al., 1997). However, it is important to point out that Rubin and colleagues also used different measures to classify shy children, and conducted their study in the laboratory. Thus, the discrepancy between our findings and those of Rubin and colleagues (1997) could be due to the fact that the group of children in Rubin and colleagues’ study was selected for extreme shyness based on cutpoints on the researchers’ shyness composite, resulting in a more restricted subset of younger and more temperamentally shy children than in the present study. The difference could be due to the nature of the context: in the present study, we used a non-normative context which was outside of the home, school, and laboratory and arguably a different type of stressor than used in past studies of shyness.
What does the inverse relation between children’s temperamental shyness and preoperative anxiety reflect? There are at least two possible explanations. First, it could be that parenting influences played a role. It is possible that parenting styles differed between shy versus non-shy children (Rubin, Nelson, Hastings, & Asendorpf, 1999). The parents of shy children may view their shy child as vulnerable and thus have prepared them to handle their emotions, both in stressful situations in general and particularly for the perioperative environment. Conversely, the parents of non-shy children may have viewed their child as less vulnerable to stressful situations and thus did not prepare their child for how to handle their emotions in the perioperative environment. Higher levels of shyness in children may also lead to less anxiety because parents may be aware of these difficulties and attempt to compensate by more actively preparing them for surgery. In this unique context, perhaps differential parenting styles served to protect some children and placed others at risk. In a study by Kain’s group (2006) that examined the interaction of child-parent dyads in the OR, they found that an anxious child benefits from the presence of a calm parent during anesthetic induction, but not from an overly anxious parent (Kain et al., 2006). Therefore, even though the majority of parents want to participate in their child’s perioperative experience, not all may provide optimal support. Because parental anxiety also has been linked to children’s preoperative anxiety in the surgical context in other studies (Kain et al., 1996; Shirley, Thompson, Kenward, & Johnston, 1998), future work should seek to further examine the role of parental influences on children’s perioperative anxiety by assessing the role they may play in these associations.
Second, it might be that temperamentally shy children may exhibit relatively lower preoperative anxiety in a surgical context because they may have developed coping strategies in dealing with their persistent anxiety in their everyday environments. In other studies, we have found that there are age-related changes in cortisol stress levels with cortisol levels decreasing from middle childhood to adulthood in people who are temperamentally shy (Beaton et al., 2006; Beaton, Schmidt, Schulkin, & Hall, 2013; Schmidt, Santesso, Schulkin & Segalowitz, 2007). We have argued that these changes might reflect “recalibration” of stress systems due to a life history of dealing with persistent stress and a psychological central state of fear in the temperamentally shy person’s everyday environments. Furthermore, this neuroendocrine change might also reflect a protective mechanism against system breakdown.
The present study, however, had several limitations that warrant further discussion. First, the present results are based on a relatively small sample. This is a unique medical sample with children undergoing elective ENT surgeries, thus, the recruitment and follow-up with children and families on the day of surgery were challenging which limits our sample size. Second, the findings are based on subjective reports. Although we used reliable and validated subjective measures, these measures can be inherently biased. It is possible that shy children might be less likely to disclose their anxiety through self-report due to fear of negative evaluations. Third, there may have been issues related to informant biases. We had different informants complete measures, so issues of measurement variance may have occurred. Fourth, we did not use an extreme group design to classify temperamentally shy children overtime, so our findings might not generalize to extremely temperamentally shy children. Fifth, although the surgical environment has a novel social component (e.g., doctors, nurses, pediatric patients and families), it may not have reflected the type of stressful social context needed to elicit anxiety in shy children. It is possible that the unfamiliar, non-social stimuli (i.e., surgical tools, unfamiliar hospital routine and novel environment) would elicit stronger anxiety among children with non-social behavioral inhibition. Future studies should use a larger sample, objective behavioral measures coded from direct observations of child’s anxiety and within the surgical settings, clarify the social context within the surgical setting, and use extreme groups to classify temperamentally shy and social children in order to ensure the reliability and generalizability of the present results.
The present preliminary findings have implications to theory, reproducibility, and practice. The study of person by context interactions on behavior has had a long history in psychology (Allport, 1937; Lewin, 1951; Mischel, 1979). However, a majority of studies with children over the years have used relatively normative environments such as the home, school, and laboratory, so it is not clear the extent to which person by context interactions would generalize to non-normative stressful contexts. Our findings highlight the importance of considering other contexts, normative and non-normative, ecologically-salient, which is necessary to enhance reliable prediction of behavior, fully understand individual differences and person by context interactions, and to reproduce findings.
In terms of practice, our preliminary findings highlight the need to consider individual differences in temperament when preparing children for surgery. Studies have shown that there are individual differences in children’s reactions to the surgical context and that children who are anxious require more anesthetic induction, are more likely to refuse procedures, and take longer to recover post-operatively (Chow et al., 2015; Kain et al., 2000; Kain, Wang, Mayes, Caramico, & Hofstadter, 1999; Long & Rajagopalan, 2002; Maranets & Kain, 1999; McCann, & Kain, 2001). The present preliminary results imply that temperament may be predictive of who may or may not be at risk for heightened preoperative anxiety. Our data also suggest that low shyness scores should not be interpreted for a lack of apprehension in the surgical setting. The findings of this study could be helpful to parents and health practitioners for developing precision medical approaches for managing children’s preoperative anxiety.
Acknowledgements / Conflicts of Interest
This study was supported by an Ontario Graduate Scholarship and the Ontario Mental Health Foundation Studentship awarded to Cheryl H.T. Chow and operating grants from the Social Sciences and Humanities Research Council of Canada (SSHRC), the Natural Sciences and Engineering Research Council of Canada (NSERC) awarded to Louis A. Schmidt, and the operating grant from the Canadian Institutes of Health Research (CIHR) awarded to Louis A. Schmidt, Ryan J. Van Lieshout, Norman Buckley and Desigen Reddy. We wish to thank the many children and family who participated in the study, Mark Hwang, Pauline Leung, Eliza Pope, and Stephanie Wan who assisted with data collection and data entry, and the support from Ms. Toni Tidy and Ms. Debbie O’Rouke, the Department of Anesthesia, the Child Life Specialists and Program and the OR staff at the McMaster Children’s Hospital. The authors declare no conflict of interest.
References
- Allport GW. Personality: A psychological interpretation. New York, NY: H Holt and Company; 1937. [Google Scholar]
- Barrett L. Psychology Is Not in Crisis. The New York Times. 2015 Sep 1;:A23. [Google Scholar]
- Beaton EA, Schmidt LA, Ashbaugh AR, Santesso DL, Antony MM, McCabe RE, … Schulkin J. Low salivary cortisol levels among socially anxious young adults: Preliminary evidence from a selected and a non-selected sample. Personality and Individual Differences. 2006;41(7):1217–1228. [Google Scholar]
- Beaton EA, Schmidt LA, Schulkin J, Hall GB. Repeated measurement of salivary cortisol within and across days among shy young adults. Personality and Individual Differences. 2013;55(6):705–710. [Google Scholar]
- Buss AH, Plomin R. Temperament: Early developing personality traits. New York: Psychology Press; 1984. Theory and measurement of EAS. [Google Scholar]
- Beidel DC, Turner SM. Shy children, phobic adults: Nature and treatment of social anxiety disorder. Washington, DC: American Psychological Association; 2007. pp. 11–46. [Google Scholar]
- Chieng YJS, Chan WCS, Klainin-Yobas P, He HG. Perioperative anxiety and postoperative pain in children and adolescents undergoing elective surgical procedures: A quantitative systematic review. Journal of Advanced Nursing. 2014;70(2):243–255. doi: 10.1111/jan.12205. [DOI] [PubMed] [Google Scholar]
- Chow C, Van Lieshout RJ, Buckley N, Schmidt LA. Children’s Perioperative Multidimensional Anxiety Scale (CPMAS): Development and validation. Psychological Assessment. 2016;28(9):1101–1109. doi: 10.1037/pas0000318. [DOI] [PubMed] [Google Scholar]
- Chow C, Van Lieshout RJ, Schmidt LA, Dobson KG, Buckley N. Systematic Review: Audiovisual interventions for reducing preoperative anxiety in children undergoing elective surgery. Journal of Pediatric Psychology. 2015;41(2):182–203. doi: 10.1093/jpepsy/jsv094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Degnan KA, Pine DS, Perez-Edgar K, Henderson HA, Diaz Y, … Fox NA. Stable early maternal report of behavioral inhibition predicts lifetime social anxiety disorder in adolescence. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48(9):928–935. doi: 10.1097/CHI.0b013e3181ae09df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coplan RJ, DeBow A, Schneider BH, Graham AA. The social behaviors of inhibited children in and out of preschool. British Journal of Developmental Psychology. 2009;27(4):891–905. doi: 10.1348/026151008x396153. [DOI] [PubMed] [Google Scholar]
- Coplan RJ, Prakash K, O’Neil K, Mandana A. Do you “want” to play? Distinguishing between conflicted shyness and social disinterest in early childhood. Developmental Psychology. 2004;40:244–258. doi: 10.1037/0012-1649.40.2.244. [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods. 2009;41(4):1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- Funder DC. Towards a resolution of the personality triad: Persons, situations, and behaviors. Journal of Research in Personality. 2006;40(1):21–34. [Google Scholar]
- Funder DC, Guillaume E, Kumagai S, Kawamoto S, Sato T. The person-situation debate and the assessment of situations. Personality Research. 2012;21(1):1–11. [Google Scholar]
- Garcia-Coll C, Kagan J, Reznick JS. Behavioral inhibition in young children. Child Development. 1984;55(3):1005–1019. [Google Scholar]
- Kagan J, Reznick JS, Snidman N. The physiology and psychology of behavioral inhibition in children. Child Development. 1987;58(6):1459–1473. [PubMed] [Google Scholar]
- Kagan J, Reznick JS, Snidman N. Biological bases of childhood shyness. Science. 1988;240(4849):167–171. doi: 10.1126/science.3353713. [DOI] [PubMed] [Google Scholar]
- Kain ZN, Mayes LC, Caldwell-Andrews AA, Karas DE, McClain BC. Preoperative anxiety, postoperative pain, and behavioral recovery in young children undergoing surgery. Pediatrics. 2006;118(2):651–658. doi: 10.1542/peds.2005-2920. [DOI] [PubMed] [Google Scholar]
- Kain ZN, Mayes LC, O’Connor TZ, Cicchetti DV. Preoperative anxiety in children: Predictors and outcomes. Archives of Pediatrics & Adolescent Medicine. 1996;150(12):1238–1245. doi: 10.1001/archpedi.1996.02170370016002. [DOI] [PubMed] [Google Scholar]
- Kain ZN, Mayes LC, Weisman SJ, Hofstadter MB. Social adaptability, cognitive abilities, and other predictors for children’s reactions to surgery. Journal of Clinical Anesthesia. 2000;12(7):549–554. doi: 10.1016/s0952-8180(00)00214-2. [DOI] [PubMed] [Google Scholar]
- Kain ZN, Wang SM, Mayes LC, Caramico L, Hofstadter MB. Distress during the induction of anesthesia and postoperative behavioral outcomes. Anesthesia & Analgesia. 1999;88(5):1042–1047. doi: 10.1097/00000539-199905000-00013. [DOI] [PubMed] [Google Scholar]
- Lewin K. Field theory in social science. New York, NY: Harper & Row; 1951. [Google Scholar]
- Lindsay DS. Replication in psychological science. Psychological Science. 2015;26(12):1827–1832. doi: 10.1177/0956797615616374. [DOI] [PubMed] [Google Scholar]
- Long EO, Rajagopalan S. Stress signals activate natural killer cells. Journal of Experimental Medicine. 2002;196(11):1399–1402. doi: 10.1084/jem.20021747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maranets I, Kain ZN. Preoperative anxiety and intraoperative anesthetic requirements. Anesthesia & Analgesia. 1999;89(6):1346–1351. doi: 10.1097/00000539-199912000-00003. [DOI] [PubMed] [Google Scholar]
- McCann EM, Kain ZN. The management of preoperative anxiety in children: An update. Anesthesia and Analgesia. 2001;93(1):98–105. doi: 10.1097/00000539-200107000-00022. [DOI] [PubMed] [Google Scholar]
- Melchoir LA, Cheek JM. Shyness and anxious self-preoccupation during a social interaction. Journal of Social Behavior and Personality. 1990;5(2):117–130. [Google Scholar]
- Mischel W. On the interface of cognition and personality: Beyond the person-situation debate. American Psychologist. 1979;34(9):740–754. [Google Scholar]
- Pérez-Edgar K, Fox NA. Individual differences in children’s performance during an emotional Stroop task: A behavioral and electrophysiological study. Brain and Cognition. 2003;52(1):33–51. doi: 10.1016/s0278-2626(03)00007-1. [DOI] [PubMed] [Google Scholar]
- Rapee RM. The development and modification of temperamental risk for anxiety disorders: Prevention of a lifetime of anxiety? Biological Psychiatry. 2002;52(10):947–957. doi: 10.1016/s0006-3223(02)01572-x. [DOI] [PubMed] [Google Scholar]
- Rowe DC, Plomin R. Temperament in early childhood. Journal of Personality Assessment. 1977;41(2):150–156. doi: 10.1207/s15327752jpa4102_5. [DOI] [PubMed] [Google Scholar]
- Rubin KH, Hastings PD, Stewart SL, Henderson HA, Chen X. The consistency and concomitants of inhibition: Some of the children, all of the time. Child Development. 1997;68(3):467–483. [PubMed] [Google Scholar]
- Rubin KH, Nelson LJ, Hastings P, Asendorpf J. The transaction between parents’ perceptions of their children’s shyness and their parenting styles. International Journal of Behavioral Development. 1999;23(4):937–957. [Google Scholar]
- Schmidt LA, Buss AH. Understanding shyness: Four questions and four decades of research. In: Rubin KR, Coplan RJ, editors. The Development of Shyness and Social Withdrawal. New York, NY: Guildford Publications; 2010. pp. 23–41. [Google Scholar]
- Schmidt LA, Fox NA, Rubin KH, Sternberg EM, Gold PW, Smith CC, Schulkin J. Behavioral and neuroendocrine responses in shy children. Developmental Psychobiology. 1997;30(2):127–140. doi: 10.1002/(sici)1098-2302(199703)30:2<127::aid-dev4>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- Schmidt LA, Fox NA, Schulkin J, Gold PW. Behavioral and psychophysiological correlates of self-presentation in temperamentally shy children. Developmental Psychobiology. 1999;35(2):119–135. [PubMed] [Google Scholar]
- Schmidt LA, Polak CP, Spooner AL. Biological and environmental contributions to childhood shyness: A diathesis-stress model. In: Crozier WR, Alden LE, editors. The Essential Handbook of Social Anxiety for Clinicians. United Kingdom: John Wiley & Sons; 2005. pp. 33–55. [Google Scholar]
- Schmidt LA, Santesso DL, Schulkin J, Segalowitz SJ. Shyness is a necessary but not sufficient condition for high salivary cortisol in typically developing 10 year-old children. Personality and Individual Differences. 2007;43(6):1541–1551. [Google Scholar]
- Shirley PJ, Thompson N, Kenward M, Johnston G. Parental anxiety before elective surgery in children: A British perspective. Anaesthesia. 1998;53(10):956–959. doi: 10.1046/j.1365-2044.1998.00533.x. [DOI] [PubMed] [Google Scholar]
- Tsui TY, Lahat A, Schmidt LA. Linking temperamental shyness and social anxiety in childhood and adolescence: Moderating influences of sex and age. Child Psychiatry & Human Development. 2017:1–8. doi: 10.1007/s10578-016-0702-z. in press. [DOI] [PubMed] [Google Scholar]
- Zimbardo PG. Shyness: What it is, what to do about it. Massachusetts: Addison-Wesley; 1977. [Google Scholar]