Abstract
Objective
To examine the association between household food insecurity (HFI) and risk of childhood stunting and to determine whether this association is modified by maternal–child overweight/obesity.
Design
Observational cross-sectional study.
Setting
Data come from the Mexican National Health and Nutrition Survey (ENSANUT 2012 by its initials in Spanish), representative of rural and urban areas.
Participants
Our study sample included 5087 mother–preschool child pairs and 7181 mother–schoolchild pairs.
Main outcome measures
Differences in the prevalence (95% CI) of each HFI category by socioeconomic characteristics and maternal–child nutritional status were estimated. A logistic regression model was conducted for stunting and overweight among preschool children and for stunting and overweight/obesity among schoolchildren, adjusting for pertinent covariates. HFI was measured according to the Latin American and Caribbean Food Security Scale (ELCSA by its initials in Spanish). Weight and recumbent lenght or height measures were obtained from children. Overweight and obesity in women were determined according to the WHO Growth Reference Charts. The following covariates were included: sex of the child. urbanicity (urban/rural), region of residence and maternal education. Benefiting from food assistance programmes and socioeconomic status index were also included. Results were expressed as adjusted ORs.
Results
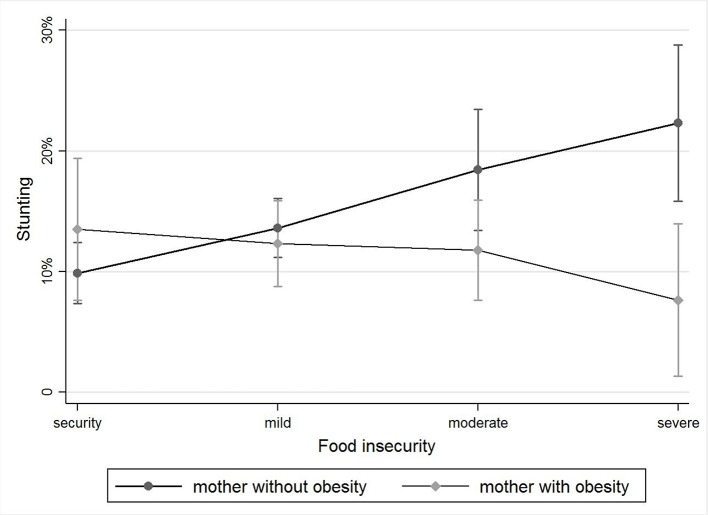
Stunting proved more prevalent in preschool children with moderate or severe HFI (16.2% and 16.8%, respectively) (p=0.036 and p=0.007, respectively) than in their counterparts with mild or no HFI (13.2% and 10.7%, respectively). Furthermore, the interaction between HFI and maternal obesity had a significant impact on stunting in preschool children (p<0.05). Severe HFI increased risk of stunting in children with non-obese mothers but not in those with obese mothers.
Conclusion
We have discovered a new relationship between HFI and maternal obesity on the one hand and risk of childhood stunting on the other hand. This may reflect a shared mechanism involving dual forms of malnutrition.
Keywords: Nutrition & dietetics, Public health, epidemiology
Strengths and limitations of this study.
The cross-sectional study design restricts the drawing of causal inferences, and our results cannot be generalised, as they refer specifically to children, adolescents and similar population groups in Mexico.
The findings of the study provide a significant contribution to the limited research available on the relationship between household food insecurity and the nutritional status of mother–child pairs.
This study is a pioneering study in the field, dealing specifically with the Mexican population.
The large sample size of the study allowed us to introduce possible confounding variables in our statistical models and draw conclusions at the national level.
Introduction
Background
Food security ‘exists when all people, at all times, have physical, social and economic access to sufficient, safe and nutritious food which meets their dietary needs and food preferences for an active and healthy life, and is supported by an environment of adequate sanitation, health services and care’.1 2
The term hunger refers both to a feeling of discomfort from not eating and to the state of undernutrition, particularly within the context of food insecurity (FI).3 Experience-based indices can serve to assess hunger directly at the household level.4
Household food insecurity (HFI) has been defined as ‘limited or uncertain availability of nutritionally adequate and safe food and also as limited and uncertain ability to acquire adequate food in socially acceptable ways’.5
FI is a growing concern worldwide. It is estimated that over one billion people suffer from insufficient availability of dietary energy and at least twice that number suffer from micronutrient deficiency.6
FI in Mexico has evolved within a complex and contrasting environment where undernutrition and overweight/obesity, together, form part of an advanced nutritional transition characterised by widespread HFI. One out of three Mexican households suffers from moderate or severe FI. This condition heightens the risk of malnutrition in children and the incidence of diabetes, overweight and obesity in adults, principally among women.7
Recent studies have suggested a link between HFI and obesity,8 especially in adult women.9–11 For instance, it has been documented that women with FI are more likely to suffer from obesity than women without FI.12 It has also been reported that racial/ethnic minority communities and low-income households are the population groups most severely affected by HFI.13
Generally viewed as separate public health problems, there is growing concern that FI and obesity may be related. FI can lead to weight gain because high-fat, high-calorie and energy-dense foods offer the least expensive option for obtaining calories,14 and these products, available at lower prices than healthful foods,15 have been identified as risk factors for child and adult obesity.16 Furthermore, HFI can trigger disorderly eating patterns characterised by bingeing and restricted eating, depending on the availability of supplies, thus negatively affecting the body's metabolism.17
Recent decades have witnessed alarming increases in prevalence of overweight/obesity among Mexican children: from 7.8% in 1988 to 9.7% in 2012 for children under 5 years old; from 26.9% in 1999 to 34.4% in 2012 for 5–11 years old; and from 11.1% in 1988 to 35.8% in 2012 for female adolescents aged 12–19 years. In the adult population aged 20 years and older, prevalence jumped from 61.8% to 71.3% in 12 years.18
In 2012, children under 5 years old living in severe-FI households had add 42% higher risk of stunting or chronic malnutrition than did their counterparts living in food-secure households.19 That same year, women aged 20–59 years old had an average body mass index (BMI) of 28.9. More specifically, those living in mild, moderate and severe HFI had BMIs of 28.3, 29.3 and 29.4 (p<0.001, p=0.011 and p=0.007), respectively.11
The double burden of malnutrition can occur within the same country, city or household (mother–child pairs) and also within the same individual at different stages of his or her life.20 The fact that HFI may be associated with both undernutrition and obesity has been documented.17
The twofold purpose of this article is to examine the association between HFI and risk of childhood stunting and to determine whether this association is modified by maternal–child overweight/obesity.
Methods
Study population
Data were drawn from ENSANUT 2012, a cross-sectional, probabilistic and cluster survey with national, regional, urban–rural and state-level representativity. Oversampling was directed to Mexican households of lower socioeconomic status (SES). A sample of 50 528 households of an estimated 29 429 252 households nationwide was obtained between October 2011 and May 2012. Details of sample size and sampling design have been described elsewhere.21
Our study consisted of a secondary analysis based on ENSANUT 2012. A total of 5087 preschool children (1–4 years old), 8401 schoolchildren (5–11 years old) and 9581 mothers were included in the survey. We used a matching process to identify mother–preschool child and mother–schoolchild pairs, and we included a total of 5087 mother–preschool child pairs in our analysis. None of the mothers in this group had more than one child. A total of 7181 mother–schoolchild pairs were included, with 2432 mothers having more than one schoolchild, in which cases where only one schoolchild was used in the matching process. Finally, the 2677 mothers in the sample who had preschool children and schoolchildren were included in both pair groups.
Our analytical sample included 5087 mother–preschool child pairs and 7181 mother–schoolchild pairs with complete data. Whenmothers had more than one schoolchild meeting the study criteria, the analysesconsidered all their children.
Informed consent was obtained from all respondents—or their parents/guardians in cases of children under 7 years old—prior to their participation in the study. The survey protocol was approved by the Ethics Committee of the National Institute of Public Health in Mexico.
HFI measurement
HFI was measured using a version of the Latin American and Caribbean Food Security Scale (ELCSA by its initials in Spanish). The scale included 15 questions targeting the head of the family or the woman in charge of preparing meals. Eight questions referred directly to HFI either in the household or specifically in the adults within the household; the remaining seven referred to HFI in minors (<18 years old). The reference time frame was 3 months prior to survey administration. Based on the number of positive responses, and depending on whether or not households included people under 18 years old, they were grouped into the following categories: households without minors: no HFI (0 positive responses), mild HFI (1–3), moderate HFI (4–6) and severe HFI (7–8) and households with adults and minors under 18 years old: no HFI (0 positive responses), mild HFI (1–5), moderate HFI (6–10) and severe HFI (11–15).22 ELCSA has been validated in populations in the United States as well as in Mexico and other Latin American countries.23–25
Anthropometric measurements
Weight and recumbent length measures were obtained from children <2 years old and standing height measures were obtained from children aged 2 to <5 years following standard recommended procedures.26 27
The anthropometric measures together with the age and sex of the children were used to calculate the weight-for-age, height-for-age and weight-for-height a z-scores according to the WHO growth standards.28 Prevalence of undernutrition in its different forms (underweight, wasting and stunting) was calculated using z-score cut-off point less than −2 using the WHO growth standards.
Overweight and obesity were determined according to the WHO Growth Reference charts,29 with BMI (kg/m2) z-scores adjusted for age: values between −5.0 and +5.0 were considered outside this range and regarded as implausible. There were no implausible values for BMI z-scores in children. For adults, the WHO standard BMI cut-off points were used to classify mothers into the following categories: underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2) and obese (≥30 kg/m2).30 Only BMI values between 10 and 58 were considered; no BMI values were regarded as implausible.
Covariates
The following covariates were included in our statistical analyses: sex of the child, urbanicity (urban/rural), region of residence (northern, central, southern and Mexico City) and maternal education: none, primary, secondary, high school (preparatoria according to its Spanish equivalent) and university (bachelor's degree and beyond). Benefiting from a food assistance programme was also included.
Socioeconomic index
We used a standard SES index developed in Mexico on the basis of various household characteristics: type of floor, wall and ceiling materials; the ratio of number of rooms used for sleeping to number of persons residing in the household; basic service infrastructure including water source and water disposal; and possession of domestic appliances such as a refrigerator, washing machine, microwave oven, stove, boiler, radio, television, cable television signal, telephone and computer. This SES index was selected to facilitate comparison with previous surveys in Mexico.31
Ethical considerations
All study procedures involving human participants were approved by the Ethics Committee of the National Institute of Public Health in Mexico. Written informed consent was obtained from all survey participants. Parents/guardians served as proxies for minors <7 years old.
Statistical analyses
We calculated the prevalence (95% CI) of each HFI category by socioeconomic characteristics and maternal–child nutritional status. We then conducted logistic regression models for stunting and overweight among preschool children and for stunting and overweight/obesity among schoolchildren, adjusting for pertinent covariates. The cluster effect for mothers with more than one schoolchild was tested and proved non-significant. No mothers had more than one preschool child. Results were expressed as adjusted ORs (AORs) with their corresponding 95% CIs. Prevalence estimates and logistic regression models considered clustered sample effects and sampling weights using STATA 13 SVY procedures for complex surveys.
Results
Our analytical sample included 5087 pairs of mother–preschool children and 7181 mother–schoolchild pairs with complete data.
In the mother–preschool child pairs, moderate HFI was significantly more prevalent among those residing in the southern, as opposed to the northern or central, regions of Mexico. As expected, severe HFI was five and six times more prevalent in the low and very low quintiles, respectively, than in the top quintile. Moderate and severe HFI were more prevalent in households with mothers who had not studied beyond junior high school and with beneficiaries of government food assistance programmes (table 1).
Table 1.
FI level according to the sociodemographic characteristics of the mother–preschool child and mother–schoolchild pairs
| Total | N* (thousands) | Secure | Mild | Moderate | Severe | |||||
| n | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | ||
| FI level in preschool children | ||||||||||
| Sex of child | ||||||||||
| Female | 2539 | 1452.9 | 24.2 | 21.7 to 26.79 | 43.8 | 40.9 to 46.6 | 21.6 | 19.5 to 23.8 | 10.5 | 9.0 to 12.2 |
| Male | 2548 | 1522.1 | 24.7 | 22.3 to 27.13 | 45.0 | 42.4 to 47.7 | 18.4 | 16.5 to 20.6 | 11.9 | 10.3 to 13.8 |
| Urbanicity | ||||||||||
| Urban | 3142 | 2123.0 | 26.8 | 24.6 to 29.1 | 43.3 | 40.9 to 45.8 | 18.9 | 17.1 to 20.9 | 10.9 | 9.4 to 12.6 |
| Rural | 1945 | 851.9 | 18.5 | 16.3 to 20.9 | 47.0 | 43.8 to 50.2 | 22.4 | 20.1 to 25.0 | 12.0 | 10.3 to 14.1 |
| Region | ||||||||||
| Northern | 1083 | 524.5 | 30.5 | 27.2 to 34.0 | 42.5 | 38.9 to 46.2 | 15.8 | 13.3 to 18.6 | 11.2 | 9.2 to 13.5 |
| Central | 1804 | 941.8 | 26.7 | 24.0 to 29.6 | 45.3 | 42.2 to 48.4 | 17.4 | 15.1 to 20.0 | 10.6 | 8.8 to 12.6 |
| Mexico City | 200 | 426.5 | 22.1 | 15.6 to 30.4 | 45.5 | 37.9 to 53.4 | 21.9 | 16.3 to 28.8 | 10.5 | 6.3 to 16.9 |
| Southern | 2000 | 1082.2 | 20.4 | 18.1 to 22.8 | 44.1 | 41.1 to 47.1 | 23.4 | 21.2 to 25.9 | 12.1 | 10.3 to 14.2 |
| SES | ||||||||||
| Very low (Q1) | 1319 | 666.0 | 12.4 | 9.9 to 15.4 | 45.8 | 41.9 to 49.6 | 23.8 | 20.8 to 27.1 | 18.0 | 15.1 to 21.4 |
| Low (Q2) | 1187 | 629.8 | 17.6 | 15.0 to 20.6 | 43.4 | 39.3 to 47.7 | 25.1 | 21.5 to 29.2 | 13.8 | 11.2 to 16.9 |
| Medium (Q3) | 1028 | 584.5 | 20.0 | 17.1 to 23.4 | 48.4 | 44.8 to 52.1 | 20.3 | 17.3 to 23.8 | 11.1 | 8.7 to 14.2 |
| High (Q4) | 879 | 575.7 | 29.1 | 25.1 to 33.5 | 44.2 | 39.7 to 48.7 | 18.5 | 15.1 to 22.4 | 8.2 | 6.2 to 10.8 |
| Very high (Q5) | 674 | 519.0 | 47.7 | 42.3 to 53.2 | 39.5 | 34.4 to 44.7 | 10.0 | 7.2 to 13.6 | 2.8 | 1.8 to 4.6 |
| Maternal education | ||||||||||
| None | 349 | 196.4 | 10.0 | 6.8 to 14.4 | 40.6 | 34.2 to 47.4 | 24.7 | 19.4 to 30.9 | 24.7 | 18.9 to 31.5 |
| Primary and/or secondary school | 3568 | 1951.6 | 19.1 | 17.4 to 20.9 | 46.1 | 43.7 to 48.5 | 21.5 | 19.6 to 23.6 | 13.3 | 11.8 to 15.1 |
| Beyond secondary school | 1165 | 823.0 | 40.4 | 36.4 to 44.6 | 41.4 | 37.6 to 45.3 | 15.1 | 12.5 to 18.1 | 3.0 | 2.0 to 4.6 |
| Beneficiaries of food assistance programmes | ||||||||||
| Beneficiaries | 2246 | 1187.1 | 15.7 | 13.6 to 18.1 | 45.8 | 42.7 to 48.8 | 24.5 | 22.1 to 27.1 | 14.0 | 12.0 to 16.3 |
| Non-beneficiaries | 2400 | 1520.1 | 30.2 | 27.6 to 33.0 | 43.8 | 41.1 to 46.6 | 16.9 | 14.9 to 19.1 | 9.0 | 7.6 to 10.8 |
| Indigenous | ||||||||||
| Yes | 101 | 1150.9 | 20.3 | 11.7 to 32.8 | 38.3 | 27.8 to 50.1 | 29.5 | 20.1 to 40.9 | 12.0 | 6.4 to 21.2 |
| No | 1906 | 41.9 | 23.5 | 21.2 to 25.9 | 44.1 | 41.2 to 47.1 | 20.3 | 18.0 to 22.9 | 12.0 | 9.9 to 14.3 |
| FI level in schoolchildren | ||||||||||
| Sex of child | ||||||||||
| Female | 4269 | 2413.0 | 23.1 | 21.3 to 25.1 | 42.3 | 40 to 44.3 | 20.1 | 18.4 to 22.0 | 14.4 | 12.9 to 15.9 |
| Male | 4132 | 2337.1 | 24.0 | 21.9 to 26.2 | 43.6 | 41.3 to 45.9 | 19.8 | 18.1 to 21.6 | 12.6 | 11.1 to 14.2 |
| Urbanicity | ||||||||||
| Urban | 5267 | 3444.7 | 26.2 | 24.3 to 28.1 | 42.0 | 39.9 to 43.9 | 18.4 | 16.8 to 20.1 | 13.5 | 12.1 to 15.1 |
| Rural | 3134 | 1306.3 | 16.7 | 14.8 to 18.8 | 45.8 | 43.2 to 48.3 | 24.2 | 22.1 to 26.4 | 13.4 | 11.8 to 15.3 |
| Region | ||||||||||
| Northern | 1796 | 884.6 | 29.5 | 26.4 to 32.8 | 42.3 | 39.2 to 45.4 | 16.2 | 13.9 to 18.8 | 12.0 | 10.2 to 14.2 |
| Central | 2928 | 1446.1 | 25.8 | 23.2 to 8.5 | 45.1 | 42.3 to 47.9 | 16.8 | 14.8 to 19.0 | 12.3 | 10.6 to 14.2 |
| Mexico City | 353 | 717.3 | 25.6 | 20.4 to 31.7 | 36.2 | 30.4 to 42.4 | 21.6 | 16.7 to 27.5 | 16.6 | 12.0 to 22.3 |
| Southern | 3324 | 1738.9 | 18.0 | 16.2 to 19.9 | 44.2 | 42.1 to 46.5 | 23.8 | 21.8 to 25.9 | 14.0 | 12.4 to 15.7 |
| SES | ||||||||||
| Very low (Q1) | 1977 | 980.7 | 9.6 | 7.9 to 11.6 | 42.5 | 39.1 to 46.1 | 26.2 | 23.3 to 29.4 | 21.7 | 18.7 to 25.1 |
| Low (Q2) | 1874 | 947.06 | 15.0 | 12.9 to 17.5 | 39.6 | 36.3 to 42.9 | 25.5 | 22.4 to 28.9 | 19.9 | 17.1 to 22.9 |
| Medium (Q3) | 1717 | 914.6 | 16.0 | 13.6 to 18.7 | 50.5 | 46.8 to 54.2 | 19.7 | 17.1 to 22.6 | 13.9 | 11.5 to 16.6 |
| High (Q4) | 1583 | 995.9 | 29.8 | 26.4 to 33.4 | 43.8 | 40.4 to 47.2 | 17.4 | 14.7 to 20.5 | 9.05 | 7.3 to 11.1 |
| Very high (Q5) | 1250 | 912.7 | 48.2 | 43.8 to 52.7 | 38.5 | 34.7 to 42.4 | 10.7 | 8.0 to 14.1 | 2.6 | 1.6 to 4.4 |
| Maternal education | ||||||||||
| None | 651 | 339.1 | 13.4 | 10.0 to 17.7 | 40.9 | 35.8 to 46.2 | 21.6 | 17.6 to 26.1 | 24.1 | 19.5 to 29.5 |
| Primary and/or secondary school | 5970 | 3212.5 | 18.7 | 17.2 to 20.3 | 44.0 | 41.9 to 45.9 | 22.0 | 20.4 to 23.7 | 15.4 | 13.9 to 16.9 |
| Beyond secondary school | 1780 | 1199.4 | 39.5 | 35.9 to 43.1 | 41.0 | 37.8 to 44.4 | 14.1 | 11.8 to 16.8 | 5.4 | 4.2 to 6.9 |
| Beneficiaries of food assistance programmes | ||||||||||
| Beneficiaries | 4527 | 2362.1 | 16.5 | 14.9 to 18.2 | 44.9 | 42.5 to 47.3 | 22.2 | 20.5 to 24.1 | 16.4 | 14.6 to 18.4 |
| Non-beneficiaries | 3299 | 2032.0 | 30.8 | 28.2 to 33.4 | 41.6 | 39.1 to 44.1 | 17.4 | 15.4 to 19.6 | 10.2 | 8.8 to 11.9 |
| Indigenous | ||||||||||
| Yes | 595 | 228.1 | 10.8 | 8.0 to 14.3 | 44.4 | 39.2 to 49.8 | 26.1 | 21.8 to 30.9 | 18.7 | 14.7 to 23.5 |
| No | 7806 | 4522.9 | 24.2 | 22.7 to 25.8 | 42.9 | 41.2 to 44.5 | 19.7 | 18.3 to 21.1 | 13.2 | 12.1 to 14.5 |
*N refers to the sample population size.
FI, food insecurity; SES, socioeconomic status.
Similarly, in the mother–schoolchild pairs, general HFI was more prevalent among those living in southern Mexico than among those living in the north. In addition, HFI was higher in the low and very low socioeconomic quintiles. Prevalence of moderate and severe HFI was significantly higher among those pairs where the mothers had not studied beyond junior high school, benefited from government food assistance programmes and belonged to an indigenous population group (table 1).
Table 2 describes the nutritional status of the population by household food security/insecurity level. Stunting in preschool children was more prevalent in households with severe/moderate HFI (over 16%, respectively) than in those with mild (13.2%) or no HFI (10.7%). Likewise, wasting was more prevalent in households with severe (3.7%) than in those with mild (1.7%), moderate (1.9%) or no HFI (2.2%).
Table 2.
Prevalence of nutritional status by level of food insecurity
| Nutritional status | Food security | Mild | Moderate | Severe | ||||||||
| n (thousands) | % | 95% CI | n (thousands) | % | 95% CI | n (thousands) | % | 95% CI | n (thousands) | % | 95% CI | |
| FI in preschool-age children | ||||||||||||
| Underweight | 8.3 | 1.1 | 0.6 to 2.1 | 40.6 | 3.0 | 2.3 to 4.1 | 18.8 | 3.1 | 2.2 to 4.6 | 15.8 | 4.7 | 2.7 to 8.1 |
| Stunting | 77.6 | 10.7 | 8.6† to 13.2 | 175.4 | 13.2 | 11.4 to 15.4 | 96.2 | 16.2 | 13.1 to 19.8 | 56.0 | 16.8 | 12.8 to 21.6 |
| Wasting | 15.8 | 2.2 | 1.1 to 4.1 | 23.1 | 1.7 | 1.0‡ to 2.8 | 11.1 | 1.9 | 0.1‡ to 3.1 | 12.5 | 3.7 | 0.0* to 6.9 |
| Overweight | 75.9 | 11.0 | 8.8 to 13.5 | 120.7 | 9.7 | 8.2 to 11.5 | 47.6 | 8.3 | 6.1 to 11.2 | 31.5 | 9.6 | 6.8 to 13.3 |
| FI in schoolers | ||||||||||||
| Stunting | 48.4 | 4.4 | 3.3 to 5.8 | 128.7 | 6.4 | 5.4 to 7.4 | 75.8 | 8.0 | 6.3 to 10.3 | 64.2 | 10 to 10.1 | 7.9 to 12.7 |
| Overweight | 250.4 | 23.0 | 20.4 to 25.7 | 377.2 | 18.9 | 7.21 to 20.8 | 161.3 | 17.4 | 15.1 to 19.9 | 112.5 | 17.8 | 14.9 to 21.0 |
| Obesity | 190.6 | 17.5 | 15.1 to 20.2 | 310.8 | 15.6 | 14.0 to 17.3 | 136.4 | 14.7 | 12.5 to 17.3 | 68.6 | 10.8 | 8.3 to 14.0 |
| Overweight and obesity | 441.0 | 40.4 | 37.3 to 43.7 | 688.0 | 34.5 | 32.3 to 36.8 | 297.7 | 32.1 | 28.9 to 35.5 | 181.1 | 28.6 | 24.8 to 32.6 |
| FI in women | ||||||||||||
| Underweight | 20.9 | 1.2 | 0.6 to 2.1 | 22.7 | 0.69 | 0.5 to 0.9 | 19.1 | 1.2 | 0.6 to 2.5 | 12.9 | 1.3 | 0.8 to 2.3 |
| Overweight | 683.5 | 37.9 | 35.1 to 40.7 | 1301.7 | 39.8 | 37.7 to 41.9 | 563.9 | 37.2 | 33.9 to 40.8 | 344.7 | 35.6 | 31.9 to 39.5 |
| Obesity | 589.9 | 32.7 | 29.9 to 35.5 | 1206.9 | 36.9 | 34.9 to 38.9 | 584.1 | 38.6 | 35.3 to 41.9 | 365.7 | 37.8 | 33.6 to 42.3 |
| Overweight and obesity | 1273.4 | 70.5 | 67.7 to 73.3 | 2508.7 | 76.7 | 74.8 to 78.6 | 1148.0 | 75.9 | 73.1 to 78.4 | 710.4 | 73.5 | 69.8 to 76.8 |
z-score cut-off point of <−2 SD to classify low weight for age, WHO; z-score cut-off point of <−2 SD to classify low height for age, WHO; z-score cut-off point of <−2 SD to classify low weight for height, WHO; z-score cut-off point of >+2 SD to classify BMI for age, WHO; z-score cut-off point of >+1 and ≤+2 SD to classify BMI for age, WHO; BMI <18.5 kg/m2; BMI 25–29.9 kg/m2; BMI ≥30 kg/m2.
*N refers to the sample population size.
BMI, body mass index.
Preschool children presented no significant differences in prevalence of overweight by HFI level.
While prevalence of stunting among schoolchildren was 10% in households with severe HFI, prevalence of overweight/obesity was markedly higher in households with food security (40%) as compared with households with mild (34.5%), moderate (32.1%) or severe (28.6%) HFI. Prevalence of maternal obesity was high regardless of HFI status: >70% overall and 77% in mild HFI households.
In the logistic regression model for preschool children, prevalence of stunting was significantly higher (AOR>1, p<0.05) in households with moderate or severe HFI as opposed to mild HFI (table 3).
Table 3.
Logistic regression model for mother–preschool child pairs: stunting in children <5 years old
| AOR* | p Value | 95% CI | |
| Mild HFI | 1.26 | 0.232 | 0.9 to 1.8 |
| Moderate HFI | 1.66 | 0.036 | 1.0 to 2.7 |
| Severe HFI | 1.99 | 0.007 | 1.2 to 3.3 |
| Maternal obesity | 1.40 | 0.266 | 0.8 to 2.5 |
| Mild HFI and maternal obesity | 0.62 | 0.207 | 0.3 to 1.3 |
| Moderate HFI and maternal obesity | 0.46 | 0.069 | 0.2 to 1.1 |
| Severe HFI and maternal obesity | 0.23 | 0.011 | 0.1 to 0.7 |
| Age of children | 0.89 | 0.007 | 0.8 to 0.9 |
| Beneficiaries of food assistance programmes | 1.24 | 0.119 | 0.9 to 1.6 |
| Urbanicity | |||
| Rural | 1.42 | 0.006 | 1.1 to 1.8 |
| Maternal education | |||
| Primary school | 0.53 | <0.001 | 0.4 to 0.8 |
| Secondary school | 0.46 | 0.001 | 0.3 to 0.7 |
| Senior high school (preparatoria) | 0.34 | <0.001 | 0.2 to 0.6 |
| Bachelor or higher | 0.48 | 0.042 | 0.2 to 0.9 |
| Constant | 0.26 | <0.001 | 0.2 to 0.4 |
*Model included all independent variables listed in the table.
AOR, adjusted OR; HFI, household food insecurity.
We identified an interaction between HFI and maternal obesity. Estimated marginal prevalence rates and confidence intervals obtained from the logistic regression model are plotted in figure 1. Severe HFI raises the risk of stunting in children with non-obese mothers but not in children with obese mothers. Preschool children showed no significant interaction among HFI, overweight and maternal characteristics.
Figure 1.
Effect of HFI-maternal obesity interaction on stunting among children <5 years.
For schoolchildren, the logistic regression model revealed a significantly lower prevalence of overweight and obesity among those with mild, moderate or severe HFI (p<0.05) (table 4); mothers having higher levels of education (bachelor's and beyond) (p<0.001); and residence in rural areas (p=0.007).
Table 4.
Logistic regression model for mother–schoolchild pairs: Both mother and child with overweight/obesity (overweight and obesity in schoolchildren)
| AOR* | p Value | 95% CI | |
| Mild HFI | 0.79 | 0.017 | 0.6 to 0.9 |
| Moderate HFI | 0.72 | 0.005 | 0.57 to 0.90 |
| Severe HFI | 0.67 | 0.004 | 0.51 to 0.9 |
| Maternal overweight | 2.25 | <0.001 | 1.8 to 2.8 |
| Maternal obesity | 3.96 | <0.001 | 3.3 to 4.8 |
| Age of child | 1.12 | <0.001 | 1.1 to 1.2 |
| Beneficiaries of food assistance programmes | 0.85 | 0.039 | 0.7 to 0.9 |
| Urbanicity | |||
| Rural | 0.79 | 0.007 | 0.7 to 0.9 |
| Maternal education | |||
| Primary school | 0.87 | 0.342 | 0.6 to 1.2 |
| Secondary school | 1.11 | 0.484 | 0.8 to 1.5 |
| Senior high school (preparatoria) | 1.12 | 0.485 | 0.8 to 1.6 |
| Bachelor or higher | 1.93 | <0.001 | 1.3 to 2.9 |
| Constant | 0.12 | <0.001 | 0.1 to 0.2 |
*Model included all independent variables listed in table.
AOR, adjusted OR; HFI, household food insecurity.
The logistic regression model for stunting in schoolchildren documented significant associations of this condition with maternal characteristics but not with HFI (data not shown).
Discussion
We sought to describe the nutritional status of children <11 years old and their mothers and to explore the relationship between their nutritional status and HFI. One of the strengths of this study concerns the fact that our research sample was representative of the Mexican population.
Many countries are witnessing an increase in the prevalence of adult overweight while still struggling with childhood stunting. Our study found that moderate and severe HFI were associated with low height in children who were under 5 years old and lived with mothers with overweight or obesity. Similar results have been obtained by other studies on the double burden of malnutrition, where stunted children live with overweight mothers in the same, and particularly in poor, households.32 33 The problem has been analysed at the household and individual levels both globally and within a number of countries, Mexico among them.34
Studies conducted in the Latin American and Arctic regions have demonstrated that FI households exhibit a reduced variety of available food and also inadequate consumption of fruits and vegetables35 and foods of animal origin.36 37 These findings have been explained by insufficient local food availability as well as the presence of inferior-quality, high-cost foods, both of which favour the choice of widely available cheaper foods of low nutritional value.38 It has been reported that FI in Mexico has similar effects to those observed in the rest of Latin America as regards dietary diversity and food availability. Mexican children under 5 years old are not receiving the recommended daily energy intake39 and female heads of household show diminished dietary diversity.40
Evidence from a study of <5 children of Mexican origin living in immigrant communities in California and in Mexico itself underscores the fact that FI contributes not only to increased energy and fat intake as a result of consuming cheap and energy-rich foods such as snacks, sweets and fried foods but also to increased consumption of meat, especially fried chicken. For children living in Mexico, FI was associated with low consumption of carbohydrates, dairy products and vitamin B6.41
The pathway through which FI can lead to an increase in body fat is based on the following factors: (1) Diets characterised by high quantities of fat and carbohydrates together with a limited variety of vegetables are associated with high energy intake and a subsequent increase in body fat.42 43 (2) According to one hypothesis, involuntary restriction of food including episodic lack of access can lead to compulsive eating and to ignoring internal signs of satiety,44 as well as to physiological adaptations in response to the periodic scarcity of food.17
Conversely, our study demonstrated an association between FI and stunting among Mexican preschool children. The way in which FI negatively affects the nutritional state of these children relates largely to insufficient consumption of highly nutritious foods (such as products of animal origin, fruits and vegetables) coupled with recurrent infections and unhealthy living conditions linked to poverty. These factors contribute to loss of appetite, an increase in metabolic requirements and a deficit of nutrients.45
Our results agree with those of a previous study where children from HFI households weighed less than their peers from food-secure households. Their average body weight was within the normal range, whereas their peers were at risk of becoming overweight.
Adequate growth is not the only indicator of nutritional well-being among children living with HFI.36 Nutritional status is also influenced by the quality of foods consumed. It has been demonstrated that obesity is an expected consequence of HFI for some subpopulations and at certain ages. Moreover, it has been shown that children and adolescents are often affected by HFI through both nutritional and non-nutritional pathways despite parental intentions or beliefs to the contrary.46
A recent analysis of 16 Latin American countries revealed that all of them were running programmes aimed at preventing undernutrition, and most were in the process of implementing obesity prevention strategies as part of their policy agendas.47 According to the literature, cash transfers and food distribution programmes may be triggering increased energy intake at the household level48 49 and exacerbating the HFI-obesity link in populations that do not need assistance programmes focused on caloric intake. This has raised concerns about the possible contribution of these programmes to obesity in populations who are not energy deficient, and this highlights the need for countries with a double burden of malnutrition to include obesity prevention strategies as an essential component of their cash and food transfer programmes.
The principal findings of our study are particularly relevant for countries undergoing nutritional transition. Mexico has been facing rapid epidemiological and demographic changes with nutritional and environmental components. The health profile of the Mexican population indicates a shift from high rates of mortality and infectious diseases—typical of poor countries—to low rates of mortality and high rates of non-communicable diseases (the main cause of mortality in wealthy countries).50
Our study was subject to several limitations. First, its cross-sectional design restricts the drawing of causal inferences. Additionally, its findings refer specifically to Mexican children, adolescents and similar population groups and therefore cannot be generalised to others.
Nevertheless, our study also has a number of strengths. For instance, our findings contribute to the limited research available on the relationship between HFI and the nutritional status of mother–child pairs. In addition, this is one of the first studies in this field dealing specifically with the Mexican population. The large sample size of our study constitutes another strength. It allowed us to introduce possible confounders in the statistical models and to provide evidence useful at the national level.
In order to develop effective and integral nutritional strategies, policy-makers need to recognise the apparently contradictory presence of adult overweight/obesity and childhood stunting in the same household and understand its association with HFI. For households at different HFI levels to experience an actual improvement in their nutritional status, efforts to abate overnutrition, undernutrition and inadequate dietary quality must be rooted in this knowledge.
Interestingly, our study found that, in preschool children, HFI severity increased the risk of stunting only if their mothers were not obese. This may be explained by the growth of urbanisation resulting in higher household incomes and greater food availability and as regards quantity, not quality.51 The foods available to poor urban households are likely to be energy rich but nutrient poor. The presence of non-obese mothers in FI households may indicate a dearth of adequate quality food for children redounding in micronutrient deficiencies and protein quality issues that hinder their growth—particularly in relation to height. By contrast, the presence of maternal obesity in FI households may indicate greater access to the calories and nutrients needed for adequate child development and may also account for the lower prevalence of stunting in these homes. This may explain the relative lack of any relationship of stunting to HFI severity in households with obese mothers.
Conclusions
The double burden of malnutrition in Mexico occurs most notably among mother–child pairs living with HFI. Crafting a sound approach to combat malnutrition is complex because of its multidimensional nature.52 These conditions hamper the implementation of effective measures capable of protecting vulnerable population groups and ensuring adequate livelihoods. Policies and programmes must tackle chronic undernutrition and overnutrition according to the food and nutritional needs of each age group, rather than assuming that their needs will be met by targeting the household as a homogeneous unit. Consistent with other studies, our work highlights the importance of monitoring household food security based on experience-related scales such as ELCSA. These have proved highly useful for food security governance.53
Supplementary Material
Acknowledgments
The authors wish to thank Erick Mauricio Rolando López for his support in developing the tables. They also gratefully acknowledge the staff of the National Health and Nutrition Survey 2012 who made this work possible.
Footnotes
Contributors: The responsibilities of the authors were distributed as follows: TS-L and IM-G-H contributed to data analysis and interpretation. They drafted the manuscript based on the input and feedback of all the coauthors. VM-R, LC-N and CM-R contributed to the study design and critical review of the manuscript. TS-L and RP-E contributed to the study design, interpretation of results and critical review of the manuscript. All the authors read and approved the final version of the manuscript.
Funding: The National Health and Nutrition Survey (ENSANUT 2012) was funded by the Mexican Ministry of Health.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: All study procedures involving human participants were approved by the Ethics Committee of the National Institute of Public Health in Mexico.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1. Food and Agriculture Organization FAO. Food security statistics home. 2016. http://www.fao.org/economic/ess/ess-fs/en/ (accessed 14 Apr 2016).
- 2. Food and Agriculture Organization, International Fund for Agricultural Development, World Food Programme. The state of food insecurity in the world 2014. Rome, Italy: Strengthening the enabling environment for food security and nutrition, 2014. [Google Scholar]
- 3. UN Millennium Project 2005. Halving hunger: it can be done: Task Force on Hunger, 2005. http://www.unmillenniumproject.org/documents/Hunger-lowres-complete.pdf (accessed 14 Apr 2016). [Google Scholar]
- 4. Jones AD, Ngure FM, Pelto G, et al. What are we assessing when we measure food security? A compendium and review of current metrics. Adv Nutr 2013;4:481–505. 10.3945/an.113.004119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pérez-Escamilla R, Melgar-Quiñonez H, Nord M, et al. Escala Latinoamericana y Caribeña de Seguridad Alimentaria (ELCSA) Memorias de la 1ª Conferencia en América Latina y el caribe sobre la medición de la seguridad alimentaria en el hogar: Perspectivas en Nutrición Humana, 2007:117–34. [Google Scholar]
- 6. Barrett CB. Measuring food insecurity. Science 2010;327:825–8. 10.1126/science.1182768 [DOI] [PubMed] [Google Scholar]
- 7. Shamah-Levy T, Mundo-Rosas V, Rivera-Dommarco JA. [Magnitude of food insecurity in Mexico: its relationship with nutritional status and socioeconomic factors]. Salud Publica Mex 2014;56(suppl 1):S79–S85. [PubMed] [Google Scholar]
- 8. Martin KS, Ferris AM. Food insecurity and gender are risk factors for obesity. J Nutr Educ Behav 2007;39:31–6. 10.1016/j.jneb.2006.08.021 [DOI] [PubMed] [Google Scholar]
- 9. Townsend MS, Peerson J, Love B, et al. Food insecurity is positively related to overweight in women. J Nutr 2001;131:1738–45. [DOI] [PubMed] [Google Scholar]
- 10. Adams EJ, Grummer-Strawn L, Chavez G. Food insecurity is associated with increased risk of obesity in California women. J Nutr 2003;133:1070–4. [DOI] [PubMed] [Google Scholar]
- 11. Morales-Ruán MC, Humarán M-G I, Shamah-Levy T, et al. Food insecurity is associated with obesity in adult women of Mexico. Salud Publica Mex 2014;56(Suppl 1):54–61. [PubMed] [Google Scholar]
- 12. Hanson KL, Sobal J, Frongillo EA. Gender and marital status clarify associations between food insecurity and body weight. J Nutr 2007;137:1460–5. [DOI] [PubMed] [Google Scholar]
- 13. Nord M, Andrews M, Carlson S. Household food security in the US, 2008. US Department of Agriculture. Economic Research Service. Washington DC 2009. [Google Scholar]
- 14. Healthy Eating Research A National Program of the Robert Wood Johnson Foundation. Food Insecurity and risk for obesity among children and families: is there a relationship?. Healthy Eating Research building evidence to prevent childhood obesity. A Research Synthesis 2010. [Google Scholar]
- 15. Pérez-Escamilla R, Obbagy JE, Altman JM, et al. Dietary energy density and body weight in adults and children: a systematic review. J Acad Nutr Diet 2012;112:671–84. 10.1016/j.jand.2012.01.020 [DOI] [PubMed] [Google Scholar]
- 16. Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr 2004;79:6–16. [DOI] [PubMed] [Google Scholar]
- 17. Dietz WH. Does hunger cause obesity? Pediatrics 1995;95:766–7. [PubMed] [Google Scholar]
- 18. Barquera S, Campos-Nonato I, Hernández-Barrera L, et al. [Prevalence of obesity in mexican adults 2000-2012]. Salud Publica Mex 2013;55(Suppl 2):151–60. [PubMed] [Google Scholar]
- 19. Cuevas-Nasu L, Rivera-Dommarco JA, Shamah-Levy T, et al. Food insecurity and nutritional status of pre-school children in Mexico. Salud Publica Mex 2014;56(Suppl 1):47–53. [PubMed] [Google Scholar]
- 20. Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013;382:427–51. 10.1016/S0140-6736(13)60937-X [DOI] [PubMed] [Google Scholar]
- 21. Romero-Martínez M, Shamah-Levy T, Franco-Núñez A, et al. [National Health and Nutrition Survey 2012: design and coverage]. Salud Publica Mex 2013;55 Suppl 2(Suppl 2):332–40. [PubMed] [Google Scholar]
- 22. Perez-Escamilla R, Melgar-Quiñonez H, Nord M, et al. Escala Latinoamericana y Caribeña de Seguridad Alimentaria (ELCSA). Memorias de la 1a. Conferencia en América Latina y el Caribe sobre la medición de la seguridad alimentaria en el hogar. Perspectivas en Nutrición Humana 2007;Supp:117–34. [Google Scholar]
- 23. Pérez-Escamilla R, Segall-Corrêa AM, Kurdian Maranha L, et al. An adapted version of the U.S. Department of Agriculture Food Insecurity module is a valid tool for assessing household food insecurity in Campinas, Brazil. J Nutr 2004;134:1923–8. [DOI] [PubMed] [Google Scholar]
- 24. Pérez-Escamilla R, Parás P, Acosta MJ, et al. Are the Latin American and Caribbean Food Security Scale (ELCSA) items comparable across countries? FASEB J 2011;25:226.8. [Google Scholar]
- 25. Álvarez MC, Melgar-Quiñonez H, Estrada A, et al. Validación interna y externa de la escala Latinoamericana y Caribeña para la medición de la Seguridad Alimentaria en El Hogar. Medellín: Editorial Divergráficas, 2008. [Google Scholar]
- 26. Lohman T, Roche AF, Martorell R. Anthropometric standardization reference manual: abridged edition. Champaign, IL: Human Kinetics Books, 1988. [Google Scholar]
- 27. Habicht JP. [Standardization of quantitative epidemiological methods in the field]. Bol Oficina Sanit Panam 1974;76:375–84. [PubMed] [Google Scholar]
- 28. World Health Organization. WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. 2006. http://www.who.int/childgrowth/standards/Technical_report.pdf (accessed 19 Apr 2016).
- 29. de Onis M, Onyango AW, Borghi E, et al. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 2007;85:660–7. 10.2471/BLT.07.043497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. World Health Organization. Obesity: preventing and managing the global epidemic: Report of a WHO consultation, 2000. http://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/ (accessed 19 Apr 2016). [PubMed] [Google Scholar]
- 31. Gutiérrez JP, Rivera-Dommarco J, Shamah-Levy T, et al. ; Encuesta Nacional de Salud Y Nutrición 2012. Resultados Nacionales. Cuernavaca, México: Instituto Nacional de Salud Pública (MX), 2012:137–8. [Google Scholar]
- 32. Popkin BM. Global nutrition dynamics: the world is shifting rapidly toward a diet linked with noncommunicable diseases. Am J Clin Nutr 2006;84:289–98. [DOI] [PubMed] [Google Scholar]
- 33. Gubert MB, Spaniol AM, Segall-Corrêa AM, et al. Understanding the double burden of malnutrition in food insecure households in Brazil. Maternal Child Nutr 2016. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kroker-Lobos MF, Pedroza-Tobías A, Pedraza LS, et al. The double burden of undernutrition and excess body weight in Mexico. Am J Clin Nutr 2014;100:1652S–8. 10.3945/ajcn.114.083832 [DOI] [PubMed] [Google Scholar]
- 35. Kaiser LL, Melgar-Quiñonez H, Townsend MS, et al. Food insecurity and food supplies in latino households with young children. J Nutr Educ Behav 2003;35:148–53. 10.1016/S1499-4046(06)60199-1 [DOI] [PubMed] [Google Scholar]
- 36. Segall Correa AM, Panigass G, Archanjo Sampaio MF, et al. Validación de instrumento de medida de la inseguridad alimentaria y hambre en el contexto de las políticas brasileñas de combate al hambre. Memorias de la 1ª Conferencia en América Latina y el Caribe sobre la medición de la seguridad alimentaria en el hogar. Perspectivas en Nutrición Humana 2007(Suppl):89–102. [Google Scholar]
- 37. Hackett M, Zubieta AC, Hernandez K, et al. Food insecurity and household food supplies in Rural Ecuador. Arch Latinoam Nutr 2007;57:10–17. [PubMed] [Google Scholar]
- 38. Huet C, Rosol R, Egeland GM. The prevalence of food insecurity is high and the diet quality poor in Inuit communities. J Nutr 2012;142:541–7. 10.3945/jn.111.149278 [DOI] [PubMed] [Google Scholar]
- 39. Mundo-Rosas Verónica, La Cruz-Géngora V, Jiménez-Aguilar A, et al. Diversidad de la dieta y consumo de nutrimentos en ni?os de 24 a 59 meses de edad y su asociaci?n con inseguridad alimentaria. Salud Pública de Mex 2014;56:39–s46. [PubMed] [Google Scholar]
- 40. Melgar-Quiñonez H, Zubieta AC, Valdez E, et al. [Validation of an instrument to monitor food insecurity in Sierra de Manantlán, Jalisco]. Salud Publica Mex 2005;47:413–22. [DOI] [PubMed] [Google Scholar]
- 41. Rivera JA, Pedraza LS, Martorell R, et al. Introduction to the double burden of undernutrition and excess weight in Latin America. Am J Clin Nutr 2014;100(Suppl):1613S–6. 10.3945/ajcn.114.084806 [DOI] [PubMed] [Google Scholar]
- 42. McCrory MA, Fuss PJ, McCallum JE, et al. Dietary variety within food groups: association with energy intake and body fatness in men and women. Am J Clin Nutr 1999;69:440–7. [DOI] [PubMed] [Google Scholar]
- 43. Matheson DM, Varady J, Varady A, et al. Household food security and nutritional status of hispanic children in the fifth grade. Am J Clin Nutr 2002;76:210–7. [DOI] [PubMed] [Google Scholar]
- 44. Townsend MS, Peerson J, Love B, et al. Food insecurity is positively related to overweight in women. J Nutr 2001;131:1738–45. [DOI] [PubMed] [Google Scholar]
- 45. Caulfield E, Richard S, Rivera JA, et al. Stunting, wasting, and micronutrient deficiency disorders : Jamison DT, Breman JG, Measham AR, Disease Control Priorities in Developing Countries. Washington, (DC: The International Bank for Reconstruction and Development / The World Bank, 2006. [PubMed] [Google Scholar]
- 46. Frongillo EA. Confronting myths about household food insecurity and excess weight. Cad Saude Publica 2013;29:229–30. 10.1590/S0102-311X2013000200005 [DOI] [PubMed] [Google Scholar]
- 47. Fanzo J, Pronyk P, Dasgupta A, et al. An evaluation of progress toward the Millennium Development Goal one Hunger target: a country-level, food and nutrition security perspective: Center for Global Health and Economic Development. The Earth Institute of Columbia University, 2010. http://millenniumvillages.org/wp-content/uploads/2010/01/Evaluation-of-Progress_Fanzo.pdf (accessed 21 Jun 2016). [Google Scholar]
- 48. Dinour LM, Bergen D, Yeh MC. The food insecurity-obesity paradox: a review of the literature and the role food stamps may play. J Am Diet Assoc 2007;107:1952–61. 10.1016/j.jada.2007.08.006 [DOI] [PubMed] [Google Scholar]
- 49. Leroy JL, Gadsden P, Rodríguez-Ramírez S, et al. Cash and in-kind transfers in poor rural communities in Mexico increase household fruit, vegetable, and micronutrient consumption but also lead to excess energy consumption. J Nutr 2010;140:612–7. 10.3945/jn.109.116285 [DOI] [PubMed] [Google Scholar]
- 50. Stevens G, Dias RH, Thomas KJ, et al. Characterizing the epidemiological transition in Mexico: national and subnational burden of diseases, injuries, and risk factors. PLoS Med 2008;5:e125 10.1371/journal.pmed.0050125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kolopaking R, Bardosono S, Fahmida U. Maternal self-efficacy in the home food environment: a qualitative study among low-income mothers of nutritionally at-risk children in an urban area of Jakarta, Indonesia. J Nutr Educ Behav 2011;43:180–8. 10.1016/j.jneb.2009.10.010 [DOI] [PubMed] [Google Scholar]
- 52. Mahmudiono T, Nindya TS, Andrias DR, et al. The effectiveness of nutrition education for overweight/obese mothers with stunted children (NEO-MOM) in reducing the double burden of malnutrition in Indonesia: study protocol for a randomized controlled trial. BMC Public Health 2016;16:1 10.1186/s12889-016-3155-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Pérez-Escamilla R. Can experience-based household food security scales help improve food security governance? Glob Food Sec 2012;1:120–5. 10.1016/j.gfs.2012.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.