Abstract
The rate of opioid overdose continues to rise, necessitating improved treatment options. Current therapeutic approaches rely on administration of either a blocking agent, such as naloxone, or chronic treatment with replacement drugs, including methadone and/or buprenorphine. Recent findings suggest that males and females respond to these treatments uniquely. In an effort to better understand this sex-specific variation in treatment efficacy, we investigated the effects of acute opioid withdrawal in male and female rats using 18FDG and microPET. These data demonstrate that acute opioid withdrawal produces metabolic alterations in brain regions associated with reward and drug dependence, namely corpus striatum, thalamic nuclei, septum, and frontal cortex. Furthermore, certain changes are unique to males. Specifically, males demonstrated increased metabolism in the anterior cingulate cortex and the ventral hippocampus (CA3) following acute opioid withdrawal. If males and females exhibit sex-specific changes in regional brain metabolism following acute opioid withdrawal, then perhaps it is not surprising that they respond to treatment differently.
Keywords: Drug dependence, Opioid withdrawal, Brain metabolism
Introduction
The escalating use of prescription pain relievers has contributed to the current opioid abuse epidemic in the United States. This has resulted in a surge of acute intoxication related deaths [1–3]. Although naloxone (Narcan®) expansion and administration has proven effective as a short-term measure, saving countless lives, it fails to address the underlying issue [4,5]. Unfortunately, the development of effective treatment strategies targeting patients suffering from opioid abuse and withdrawal has lagged behind its clinical necessity. In fact, current options are limited to opioid replacement with methadone and buprenorphine. While these medications represent first-line treatments for opioid detoxification, their efficacy remains controversial. Furthermore, these replacement therapies retain the addictive liability and side effect profile associated with illicit opioids.
Interestingly, there is an understudied observation that males and females respond to these treatments uniquely, consistent with knowledge that both substance abuse and dependence rates vary between males and females [6–11]. Two studies, a 25-year follow-up of heroin-dependent patients treated with methadone and a seven-year follow-up of patients prescribed buprenorphine both found that women were significantly more likely than men to have stopped heroin use [12,13]. This could be attributed to differences in analgesic tolerance, which is known to vary between males and females [14–17].
In the current study, we investigated whether sex would influence the metabolic representation of opioid withdrawal. Specifically, we examined the effects of acute opioid withdrawal on drug-naïve adolescent animals via micro positron emission tomography (microPET). Using 18F-fluorodeoxyglucose (18FDG), we compared the regional metabolic effects of acute opioid withdrawal between sexes. We hypothesized that males and females would respond to opioid withdrawal uniquely as evidenced by regional differences in brain glucose metabolism.
Methods
Adolescent male (n=8) and female (n=8) Sprague-Dawley rats were acquired from Taconic Farms. Animals arrived on postnatal day (PND) 22. Animals were maintained on a 12-hour light-dark cycle and received food and water ad libitum. Following an acclimation period, all animals received baseline 18FDG microPET scans (PND 31, Scan 1). Injectable morphine sulfate (15 mg/mL, 20 mL/vial) was acquired from Sigma Aldrich. Animals received morphine treatment for 5 days at a dose of 10 mg/kg/day subcutaneously (PND 35-39). Following a two-day withdrawal period (PND 40-41), animals received a second 18FDG scan (PND 42, Scan 2).
Prior to scanning, animals were fasted for 12 hours to ensure blood glucose stability [18,19]. All images were acquired using a Siemens Inveon microPET. Each animal received a single intraperitoneal injection of 18FDG (1.8–2.0 mCi). After 18FDG administration, animals were left undisturbed in their home cage for 40 minutes to ensure radiotracer uptake. Animals were then transferred to a clear acrylic chamber, where isoflurane/oxygen was used to induce anesthesia. Five minutes post-induction, animals were transferred to the imaging platform and were secured. Continuous isoflurane/oxygen at 2.0–2.5% was administered via nasal cannula for the entire 10-minute static scan. These imaging protocols have been shown to effectively reflect brain glucose metabolism [20–22].
All microPET images were corrected for attenuation and then reconstructed using a Maximum a Posteriori (MAP) probability estimate with 20 iterations as described previously [23,24]. Raw data files were uploaded into Pixel-wise Modeling Tool software (PXMOD version 3.3, PMOD Technologies LLC), and were aligned to a reference template created using the Paxinos and Watson Sprague-Dawley rat brain atlas. After placement in anatomical space, images were skull-stripped to subtract extraneous metabolic activity, and then were corrected for injected dose to ensure comparability of regional uptake values [20,25]. Post-processing including realignment to an atlas, normalization to a mean template, and smoothing was accomplished using Statistical Parametric Mapping (SPM5, Welcome Trust Centre for Neuroimaging). Between and within group comparisons were carried out using paired and 2-sample T-tests, respectively. Post-processed images were aligned to the Paxinos and Watson rat brain atlas [26] and regions were identified using x, y, and z coordinates. Increases and decreases in relative brain glucose metabolism were visually represented using color mapping. Images were overlaid onto an anatomical cryostat template with increases set as hot (red-yellow), and metabolic decreases set as winter (blue-green). The color scale used represents all T distributions achieving statistical significance [27–29]. All corresponding brain areas are significant at a value of p ≤ 0.001 (corrected) with a cluster-extent threshold of k=0 voxels.
Results
There were no regional differences in brain metabolism between males and females at baseline (Figure 1A). However, acute opioid withdrawal produced significant changes in both cortical and subcortical brain metabolism (Figure 1B). When all animals were grouped together and compared to baseline, subjects experiencing acute morphine withdrawal demonstrated bilateral metabolic increases in the corpus striatum and thalamic nuclei, as well as in prelimbic and frontal cortices. Additionally, marked decreases were observed in the septum, ventral striatum, and ventral hippocampus compared to baseline (Figure 1B). When separated by sex, male and female groups exhibited significant differences. Specifically, males demonstrated increased metabolism in the anterior cingulate cortex and the dorsal hippocampus (CA3) compared to females (Figure 1C). No significant decreases in glucose metabolism were noted between males and females.
Figure 1.
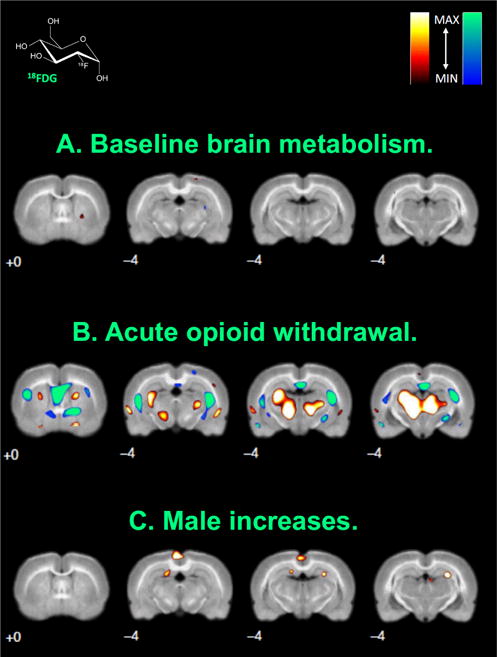
18FDG microPET images highlighting significant brain regions. Coronal slices showing the (A) baseline brain metabolism comparison of males and females, (B) changes in brain metabolism of all animals following acute opioid withdrawal, and (C) increases in male brain metabolism relative to female metabolism during acute opioid withdrawal. Slice distance in millimetres from bregma is noted in the lower left hand corner of each image. Significant increases and decreases in regional brain glucose metabolism are visually represented using hot (red-yellow) and winter (blue-green) color maps, respectively. MAX and MIN refer to the degree of regional radioisotope decay (percent injected dose per gram). The color scale used represents all T distributions achieving statistical significance. All corresponding brain areas are significant at a value of p ≤ 0.001 (corrected) with a cluster-extent threshold of k=0 voxels.
All reported increases and decreases were significant at a strict p-value threshold of p ≤ 0.001 (corrected) with a cluster-extent threshold of k=0 voxels. These constraints were chosen based on previous studies where liberal primary cluster extent thresholds were kept at a minimum. These parameters ensure the statistical validity of reported regions of interest by eliminating large activations in overlapping anatomical areas [30].
Discussion
In the present study, no regional differences in brain metabolism were observed between adolescent males and females at baseline. However, following acute opioid withdrawal, brain metabolism was altered both cortically and subcortically. Specifically, metabolic increases were measured in the corpus striatum and the deep thalamic nuclei, in addition to increases in both the prelimbic and frontal cortices. Furthermore, metabolic decreases were noted in the septum, ventral striatum and ventral hippocampus. These findings reflect metabolic averages of male and female animals grouped together. When images were disaggregated according to sex, males demonstrated increased metabolism in the anterior cingulate and the dorsal hippocampus (CA3) compared to females. There were no metabolic decreases observed between sexes.
Before treatment with morphine, both males and females exhibited similar patterns of brain glucose metabolism. However, following a five-day challenge with morphine and subsequent acute spontaneous withdrawal, males and females exhibited significantly different metabolic profiles, notably increased metabolism in anterior cingulate cortex among males. This is interesting given that disruption of the cingulate cortex can lead to an imbalance in dopaminergic signaling. This has been associated with impairment of executive function, reward-directed behavior, and conditioning, all of which have been implicated in impulsivity, compulsive drug use, and addiction [31–33]. More recently, Zakiniaeiz et al. demonstrated that the cingulate cortex may be a key region in the disruption of functional connectivity during cue-induced processing, while changes in its function may serve as a marker of subsequent alcohol relapse [34].
As noted earlier, previous studies suggest that sex differences likely affect the successful treatment of opioid abuse [12,13]. Here we demonstrate that it also impacts the primary metabolic representation of opioid withdrawal. The effects of opioids on the brain have been studied extensively [35]. Our findings support previous data indicating that opioids disrupt known reward pathways, notably in the corpus striatum [36]. Additionally, opioid withdrawal produces increases in thalamic cyclic AMP, which likely plays a role in the behavioral physiology of withdrawal [37]. The septum is also an integral part of the neurocircuitry underlying reward, pleasure, and drug seeking [38]. However, despite this knowledge, recent studies have shown that sex likely influences these pathways, and may affect treatment outcomes [17].
The morphine dose used in the present study was selected based on data indicating that a dose of 10 mg/kg was adequate to achieve conditioned place preference within this time period [39,40]. A single dose of morphine (10 mg/kg) was able to elicit conditioned place avoidance after a naloxone challenge [41]. Further, morphine, at this dose for this same period of time, also produced analgesic tolerance [42], and after only 4 days, produced withdrawal behaviors including increased defecation, urination, salivation, jumping, and wet dog shakes [43]. Finally, this dosing schedule activated glial cells and enhanced proinflammatory cytokine expression in the spinal cord, which has been implicated in morphine tolerance and withdrawal-induced hyperalgesia [39].
The 18FDG doses used are consistent with those reported previously using rats/mice and microPET [44–46]. This 18FDG dosing was designed to produce count rates that do not exceed the dead time correction capabilities of our scanner and images that could be reconstructed using an iterative method (i.e., maximum a posteriori). Relative to body weight, 18FDG is injected at significantly higher doses in rodents than in humans. These higher doses are necessary to achieve sufficient counting statistics and maximal spatial resolution in the substantially smaller brains of rodents [47]. Additionally, published reports have established that roughly the same amount of radiotracer used in humans should be used in rodents, since higher doses are necessary for equivalent image quality [48].
To our knowledge, this is the first study to assess and demonstrate sex-specific changes in regional brain metabolism following acute opioid withdrawal in drug-naïve adolescent animals. These findings are consistent with earlier reports suggesting that sex differences play an important role in the clinical presentation of opioid use disorders, specifically regarding drug craving and impairment of function [49]. Sex also appears to alter the expression of spontaneous withdrawal. Males often experience more severe and prolonged withdrawal compared to females [50]. However, while men often experience higher rates of substance abuse, women generally experience more adverse outcomes, significant impairment, and comorbid psychiatric disturbances [51], thus requiring more individualized approaches to treatment [52]. Future studies should examine both gender and sex differences, and importantly similarities, to build a better profile of the neurobiological, psychiatric, and sociocultural factors characterizing male and female opioid dependent states [53,54]. Only then can we begin to devise more effective, and perhaps sex-specific, treatment strategies designed to address this urgent healthcare concern.
References
- 1.Votaw VR, Wittenauer J, Connery HS, Weiss RD, McHugh RK. Perceived risk of heroin use among nonmedical prescription opioid users. Addict Behav. 2017;65:218–223. doi: 10.1016/j.addbeh.2016.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Tayyib AA, Koester S, Riggs P. Prescription opioids prior to injection drug use: Comparisons and public health implications. Addict Behav. 2017;65:224–228. doi: 10.1016/j.addbeh.2016.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Banerjee G. Non-medical use of prescription opioids is associated with heroin initiation among US veterans: a prospective cohort study. Addiction. 2016;111:2021–2031. doi: 10.1111/add.13491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kerr D, Dietze P, Kelly AM. Intranasal naloxone for the treatment of suspected heroin overdose. Addiction. 2008;103:379–386. doi: 10.1111/j.1360-0443.2007.02097.x. [DOI] [PubMed] [Google Scholar]
- 5.Barker K, Hunjadi D, Narcan M. The amazing drug that helps save overdose patients. JEMS. 2008;33:72–76. doi: 10.1016/S0197-2510(08)70292-4. [DOI] [PubMed] [Google Scholar]
- 6.Robbins SJ, Ehrman RN, Childress AR, O’Brien CP. Comparing levels of cocaine cue reactivity in male and female outpatients. Drug Alcohol Depend. 1999;53:223–230. doi: 10.1016/s0376-8716(98)00135-5. [DOI] [PubMed] [Google Scholar]
- 7.Hitschfeld MJ. Female smokers have the highest alcohol craving in a residential alcoholism treatment cohort. Drug Alcohol Depend. 2015;150:179–182. doi: 10.1016/j.drugalcdep.2015.02.016. [DOI] [PubMed] [Google Scholar]
- 8.Fox HC, Morgan PT, Sinha R. Sex Differences in Guanfacine Effects on Drug Craving and Stress Arousal in Cocaine-Dependent Individuals. Neuropsychopharmacology. 2014;39:1527–1537. doi: 10.1038/npp.2014.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kennedy AP, Epstein DH, Phillips KA, Preston KL. Sex differences in cocaine/heroin users: Drug-use triggers and craving in daily life. Drug Alcohol Depend. 2013;132:29–37. doi: 10.1016/j.drugalcdep.2012.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kippin TE. Potentiation of cocaine-primed reinstatement of drug seeking in female rats during estrus. Psychopharmacology. 2005;182:245–252. doi: 10.1007/s00213-005-0071-y. [DOI] [PubMed] [Google Scholar]
- 11.Rubonis AV. Alcohol cue reactivity and mood induction in male and female alcoholics. J Stud Alcohol. 1994;55:487–494. doi: 10.15288/jsa.1994.55.487. [DOI] [PubMed] [Google Scholar]
- 12.Jimenez-Trevino L. A 25-year follow-up of patients admitted to methadone treatment for the first time: Mortality and gender differences. Addict Behav. 2011;36:1184–1190. doi: 10.1016/j.addbeh.2011.07.019. [DOI] [PubMed] [Google Scholar]
- 13.Ohlin L, Fridell M, Nyhlen A. Buprenorphine maintenance program with contracted work/education and low tolerance for non-prescribed drug use: a cohort study of outcome for women and men after seven years. BMC Psychiatry. 2015;15:13. doi: 10.1186/s12888-015-0415-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fillingim RB, Gear RW. Sex differences in opioid analgesia: clinical and experimental findings. Eur J Pain. 2004;8:413–425. doi: 10.1016/j.ejpain.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 15.Craft RM. Sex differences in opioid analgesia: “From mouse to man”. Clin J Pain. 2003;19:175–186. doi: 10.1097/00002508-200305000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Terner JM, Lomas LM, Smith ES, Barrett AC, Picker MJ, et al. Pharmacogenetic analysis of sex differences in opioid antinociception in rats. Pain. 2003;106:381–391. doi: 10.1016/j.pain.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 17.Becker JB, Hu M. Sex differences in drug abuse. Front Neuroendocrinol. 2008;29:36–47. doi: 10.1016/j.yfrne.2007.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wong KP, Sha W, Zhang XL, Huang SC. Effects of Administration Route, Dietary Condition, and Blood Glucose Level on Kinetics and Uptake of F-18-FDG in Mice. J Nucl Med. 2011;52:800–807. doi: 10.2967/jnumed.110.085092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fueger BJ. Impact of animal handling on the results of F-18-FDG PET studies in mice. J Nucl Med. 2006;47:999–1006. [PubMed] [Google Scholar]
- 20.Schiffer WK, Mirrione MM, Dewey SL. Optimizing experimental protocols for quantitative behavioral imaging with (IF)-I-18-FDG in rodents. J Nucl Med. 2007;48:277–287. [PubMed] [Google Scholar]
- 21.Marsteller DA. Reproducibility of intraperitoneal 2-deoxy-2-[F-18]-fluoro-D-glucose cerebral uptake in rodents through time. Nucl Med Biol. 2006;33:71–79. doi: 10.1016/j.nucmedbio.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 22.Patel VD, Lee DE, Alexoff DL, Dewey SL, Schiffer WK. Imaging dopamine release with Positron Emission Tomography (PET) and 11C-raclopride in freely moving animals. NeuroImage. 2008;41:1051–1066. doi: 10.1016/j.neuroimage.2008.02.065. [DOI] [PubMed] [Google Scholar]
- 23.Schiffer WK. Cue-Induced Dopamine Release Predicts Cocaine Preference: Positron Emission Tomography Studies in Freely Moving Rodents. J Neurosci. 2009;29:6176–6185. doi: 10.1523/JNEUROSCI.5221-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vo A. Regional brain metabolism in a murine systemic lupus erythematosus model. J Cereb Blood Flow Metab. 2014;34:1315–1320. doi: 10.1038/jcbfm.2014.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schiffer WK. Serial microPET measures of the metabolic reaction to a microdialysis probe implant. J Neurosci Methods. 2006;155:272–284. doi: 10.1016/j.jneumeth.2006.01.027. [DOI] [PubMed] [Google Scholar]
- 26.Paxinos G, Watson CRR, Emson PC. AChE-stained horizontal sections of the rat brain in stereotaxic coordinates. J Neurosci Methods. 1980;3:129–149. doi: 10.1016/0165-0270(80)90021-7. [DOI] [PubMed] [Google Scholar]
- 27.Carrion J. Imaging the Conditioned Behavioral Effects of Methamphetamine in Rodents. Brain Imaging Behav. 2009;3:176–190. [Google Scholar]
- 28.Soto-Montenegro M. Detection of Visual Activation in the Rat Brain Using 2-deoxy-2-F-18 fluoro-D-glucose and Statistical Parametric Mapping (SPM) Mol Imaging Biol. 2009;11:94–99. doi: 10.1007/s11307-008-0179-7. [DOI] [PubMed] [Google Scholar]
- 29.Nie BB, Liu H, Chen KW, Jiang XF, Shan BC. A Statistical Parametric Mapping Toolbox Used for Voxel-Wise Analysis of FDG-PET Images of Rat Brain. Plos One. 2014;9:2014. doi: 10.1371/journal.pone.0108295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Woo CW, Krishnan A, Wager TD. Cluster-extent based thresholding in fMRI analyses: Pitfalls and recommendations. Neuroimage. 2014;91:412–419. doi: 10.1016/j.neuroimage.2013.12.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Volkow ND, Wang GJ, Fowler JS, Tomasi D, Telang F. Addiction: Beyond dopamine reward circuitry. Proc the Nat Acad Sci USA. 2011;108:15037–15042. doi: 10.1073/pnas.1010654108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Volkow ND, Fowler JS, Wang GJ, Baler R, Telang F. Imaging dopamine’s role in drug abuse and addiction. Neuropharmacology. 2009;56:3–8. doi: 10.1016/j.neuropharm.2008.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goldstein RZ. The Neurocircuitry of Impaired Insight in Drug Addiction. Trends Cogn Sci. 2009;13:372–380. doi: 10.1016/j.tics.2009.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zakiniaeiz Y, Scheinost D, Seo D, Sinha R, Constable RT. Cingulate cortex functional connectivity predicts future relapse in alcohol dependent individuals. NeuroImage Clinical. 2017;13:181–187. doi: 10.1016/j.nicl.2016.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Koob GF, Le Moal M. Annual Reviews. Palo Alto: 2008. In Annual Review of Psychology; pp. 29–53. [DOI] [PubMed] [Google Scholar]
- 36.Volkow ND, Fowler JS, Wang GJ, Swanson JM, Telang F. Dopamine in drug abuse and addiction - Results of imaging studies and treatment implications. Arch Neurol. 2007;64:1575–1579. doi: 10.1001/archneur.64.11.1575. [DOI] [PubMed] [Google Scholar]
- 37.Sadava D, Mack B. The effect of methadone addiction on cyclic-nucleotide levels in regions of the rat-brain. Life Sciences. 1986;39:477–481. doi: 10.1016/0024-3205(86)90528-x. [DOI] [PubMed] [Google Scholar]
- 38.Mahler SV, Smith RJ, Moorman DE, Sartor GC, Aston-Jones G. In: Orexin/Hypocretin System. Shekhar A, editor. Elsevier Science Bv; Amsterdam: 2012. pp. 79–121. [Google Scholar]
- 39.Raghavendra V, Tanga FY, DeLeo JA. Attenuation of morphine tolerance, withdrawal-induced hyperalgesia, and associated spinal inflammatory immune responses by propentofylline in rats. Neuropsychopharmacology. 2004;29:327–334. doi: 10.1038/sj.npp.1300315. [DOI] [PubMed] [Google Scholar]
- 40.Lu L. Role of withdrawal in reinstatement of morphine-conditioned place preference. Psychopharmacol (Berl) 2005;181:90–100. doi: 10.1007/s00213-005-2207-5. [DOI] [PubMed] [Google Scholar]
- 41.Araki H. Nicotine attenuates place aversion induced by naloxone in single-dose, morphine-treated rats. Psychopharmacol (Berl) 2004;171:398–404. doi: 10.1007/s00213-003-1595-7. [DOI] [PubMed] [Google Scholar]
- 42.Beaudry H. Differential noxious and motor tolerance of chronic delta opioid receptor agonists in rodents. Neuroscience. 2009;161:381–391. doi: 10.1016/j.neuroscience.2009.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pinelli A, Trivulzio S, Ciapponi PM. Quantitative opioid withdrawal signs in rats: effects exerted by clothiapine administration. Fundam Clin Pharmacol. 1997;11:346–355. doi: 10.1111/j.1472-8206.1997.tb00848.x. [DOI] [PubMed] [Google Scholar]
- 44.Yang FY, Chang WY, Chen JC, Lee LC, Hung YS. Quantitative assessment of cerebral glucose metabolic rates after blood-brain barrier disruption induced by focused ultrasound using FDG-MicroPET. Neuroimage. 2014;90:93–98. doi: 10.1016/j.neuroimage.2013.12.033. [DOI] [PubMed] [Google Scholar]
- 45.Parthoens J, Verhaeghe J, Stroobants S, Staelens S. Deep Brain Stimulation of the Prelimbic Medial Prefrontal Cortex: Quantification of the Effect on Glucose Metabolism in the Rat Brain Using (18) F FDG MicroPET. Mol Imag Biol. 2014;16:838–845. doi: 10.1007/s11307-014-0757-9. [DOI] [PubMed] [Google Scholar]
- 46.Chen YY. MicroPET imaging of noxious thermal stimuli in the conscious rat brain. Somatosensory and Motor Research. 2010;27:69–81. doi: 10.3109/08990220.2010.508222. [DOI] [PubMed] [Google Scholar]
- 47.Hildebrandt IJ, Su H, Weber WA. Anesthesia and other considerations for in vivo imaging of small animals. Ilar J. 2008;49:17–26. doi: 10.1093/ilar.49.1.17. [DOI] [PubMed] [Google Scholar]
- 48.Jagoda EM, Vaquero JJ, Seidel J, Green MV, Eckelman WC. Experiment assessment of mass effects in the rat: implications for small animal PET imaging. Nucl Med Biol. 2004;31:771–779. doi: 10.1016/j.nucmedbio.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 49.Back SE. Comparative Profiles of Men and Women with Opioid Dependence: Results from a National Multisite Effectiveness Trial. Am J Drug Alcohol Abuse. 2011;37:313–323. doi: 10.3109/00952990.2011.596982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cicero TJ, Nock B, Meyer ER. Gender-linked differences in the expression of physical dependence in the rat. Pharmacol Biochem Behav. 2002;72:691–697. doi: 10.1016/s0091-3057(02)00740-2. [DOI] [PubMed] [Google Scholar]
- 51.Hernandez-Avila CA, Rounsaville BJ, Kranzler HR. Opioid-, cannabis- and alcohol-dependent women show more rapid progression to substance abuse treatment. Drug Alcohol Depend. 2004;74:265–272. doi: 10.1016/j.drugalcdep.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 52.Luthar SS, Gushing G, Rounsaville BJ. Gender differences among opioid abusers: Pathways to disorder and profiles of psychopathology. Drug Alcohol Depend. 1996;43:179–189. doi: 10.1016/s0376-8716(96)01310-5. [DOI] [PubMed] [Google Scholar]
- 53.Sanchis-Segura C, Becker JB. Why we should consider sex (and study sex differences) in addiction research. Addict Biol. 2016;21:995–1006. doi: 10.1111/adb.12382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Buccelli C, Casa ED, Paternoster M, Niola M, Pieri M. Gender differences in drug abuse in the forensic toxicological approach. Forensic Sci Int. 2016;265:89–95. doi: 10.1016/j.forsciint.2016.01.014. [DOI] [PubMed] [Google Scholar]


