Abstract
Objective
We sought to describe an emerging drug use pattern characterized by injection of both methamphetamine and heroin. We examined differences in drug injection patterns by demographics, injection behaviors, HIV and HCV status, and overdose.
Methods
Persons who inject drugs (PWID) were recruited as part of the National HIV Behavioral Surveillance (NHBS) system in Denver, Colorado. We used chi-square statistics to assess differences between those who reported only heroin injection, only methamphetamine injection, and combined heroin and methamphetamine injection. We used generalized linear models to estimate unadjusted and adjusted prevalence ratios to describe the association between drug injection pattern and reported nonfatal overdose in 2015. We also examined changes in the drug reported as most frequently injected across previous NHBS cycles from 2005, 2009, and 2012.
Results
Of 592 participants who completed the survey in 2015, 173 (29.2%) reported only injecting heroin, 123 (20.8%) reported only injecting methamphetamine, and 296 (50.0%) reported injecting both drugs during the past 12 months. Injecting both heroin and methamphetamine was associated with a 2.8 (95% confidence interval: 1.7, 4.5) fold increase in reported overdose in the past 12 months compared with only injecting heroin. The proportion of those reporting methamphetamine as the most frequently injected drug increased from 2.1% in 2005 to 29.6% in 2015 (p < 0.001).
Conclusions
The rapid increase in methamphetamine injection, and the emergence of combining methamphetamine with heroin, may have serious public health implications.
Keywords: Heroin, methamphetamine, overdose
In the United States, heroin use has increased significantly during the past decade (Jones, Logan, Gladden, & Bohm, 2015). Potential contributors to the rising rates of heroin use are increased availability and lower price. In addition to its lower price, an increase in heroin purity is also likely contributing to its increased use (U.S. Drug Enforcement Administration, 2016). In the Denver metropolitan area, we have also observed a steady increase in methamphetamine use over the past several years (Denver Office of Drug Strategy, 2015). Since 2011, all methamphetamine indicators including treatment admissions, hospital discharges, emergency department visits, calls to the poison center, forensic exhibits, and mortality rates have been on the rise in the Denver metropolitan area (National Drug Early Warning System, 2016).
In Colorado, heroin is predominately Mexican-sourced “black-tar” and brown powder heroin. The wholesale distribution of heroin in Denver is controlled almost exclusively by Mexican drug organizations. In recent years, the same Mexican cartels have also been producing higher purity methamphetamine and marketing methamphetamine and heroin together (Denver Office of Drug Strategy, 2015; U.S. Drug Enforcement Administration, 2015). Two of the current article’s co-authors began learning about the increase in methamphetamine use and, in particular, its use among long time heroin users during the summer of 2013 while conducting ethnographic fieldwork (Koester & Langegger, 2015). Several patterns of use have been identified and include: mixing heroin and methamphetamine in the same solution and injecting together (referred to by PWID as “goofballs”); injecting methamphetamine and heroin separately at different times, often for the purposes of countering or intensifying the effects of the other drug; and alternating injecting of methamphetamine and heroin depending on what is more readily available.
To our knowledge, there has been little discussion of the combined use of heroin and methamphetamine in the scientific literature, and what does exist focuses on reports of “goofball” injection with one group in Seattle reporting prevalence ranging from 11% in 2009 (Jenkins et al., 2011; Peavy et al., 2012) to 32.7% in 2013 (Cedarbaum & Banta-Green, 2016). In a sample of PWID recruited in Los Angeles and San Francisco between 2011 and 2013, the reported prevalence of “goofball” injection during the past 30 days was 11% (Arreola et al., 2014; Bluthenthal et al., 2015). The earliest report of injection of heroin mixed with methamphetamine appears to be from a sample of young PWID recruited in San Francisco between 2000 and 2001. In this sample, 23% reported “goofball” injection (Ochoa et al., 2005). While there is little scientific literature describing this methamphetamine and heroin injection pattern, discussions about combining the two drugs can be found on websites that provide a forum for PWID to exchange information about drug use experiences. The combination of depressant and stimulant drugs puts the cardiovascular, respiratory, and central nervous systems under immense pressure to process different messages which can result in unpredictable outcomes. Given the dearth of information and the potential associated morbidity and mortality, we sought to quantify and describe this emerging heroin and methamphetamine injection pattern in a sample of PWID in Denver, Colorado.
Methods
National HIV Behavioral Surveillance System
The National HIV Behavioral Surveillance (NHBS) system was established in 2003 by the Centers for Disease Control and Prevention (CDC) to monitor risk behaviors among three populations at highest risk for HIV infection in the United States: gay, bisexual, and other men who have sex with men, persons who inject drugs, and heterosexuals at increased risk for HIV. NHBS involves rotating 12-month cycles of surveillance activities in these three populations. Surveillance activities include ethnographic formative research, an in-depth behavioral survey, and HIV testing during each cycle. The analyses presented in the current article are from the 2015 NHBS cycle among PWID in Denver, Colorado. In addition, we examined one data point (i.e. most frequency injected drug) from previous NHBS cycles among PWID in 2005, 2009, and 2012.
Study design and protocol
Between June and December 2015, participants were recruited using respondent-driven sampling (RDS), a peer-referral sampling methodology (Heckathorn, 1997). In RDS, initial “seed” participants are identified through key stakeholders and are recruited for participation. Seeds are then asked to recruit persons from their networks using referral coupons, who in turn use coupons to recruit persons from their networks, and so on. Each eligible participant was allowed to refer up to five persons from their network. Participants were instructed to recruit someone they knew who injects drugs and who they had seen in the past 30 days. RDS employs a dual incentive structure, thus, participants were compensated for their participation in addition to being compensated a smaller amount for each eligible person they successfully recruited.
Persons were eligible to participate if they were at least 18 years or older, had injected drugs during the preceding 12 months, resided in the Denver metropolitan statistical area, had not previously participated in the 2015 NHBS cycle, and were able to provide informed consent. Additional eligibility criteria included having physical evidence of recent injection (fresh track marks) or having current knowledge of drug preparation and injection technique and syringe description.
Verbal informed consent was obtained from eligible participants. Participants completed a standardized interviewer-administered behavioral risk survey using handheld computers.
The behavioral risk survey includes questions about sexual behaviors, injection behaviors, substance use, and HIV testing. In addition to the behavioral risk survey, which is the core NHBS survey and administered nationally across all sites, participants completed a shorter local questionnaire. Local questionnaires are developed during the formative research phase of NHBS which includes interviews with key informants and focus groups to identify salient issue of concern or interest for the target population.
During the 2015 formative research phase, key informants confirmed the ethnographic report of a rising trend in the use of methamphetamine along with heroin. To address this issue we included a question in the local Denver questionnaire in which participants were asked if they injected heroin only, methamphetamine only, or both during the past 12 months. Participants who reported injecting both were asked how they usually inject the drugs. Response options to this question were: inject them separately at different times of the day, inject them both at the same time by mixing and injecting them together (i.e. goofball), or inject them separately and together as goofballs. In the local questionnaire, participants were also asked about their overdose experience in the past 12 months. Overdose was not explicitly defined for participants.
Participants were also offered a rapid HIV test in addition to a rapid test for Hepatitis C Virus (HCV). Participants were given $35 for completing the survey, $35 for HIV and HCV testing, and $20 for each eligible person they recruited. All NHBS activities were voluntary and no names were collected. The study protocol was reviewed and approved by the Colorado Multiple Institutional Review Board.
The protocol for data collection was similar for the previous NHBS cycles among PWID in 2005, 2009, and 2012.
Statistical analysis
Analysis of the 2015 NHBS data was restricted to 592 participants who had complete data on methamphetamine and heroin injection in the past 12 months. Chi-square (X2) statistics and Fisher’s exact tests were calculated to assess differences for categorical variables based on drug injection patterns (methamphetamine only, heroin only, both). We used generalized linear models with log link and binomial error distribution to estimate unadjusted and adjusted prevalence ratios (PR) and 95% confidence intervals (CI) to describe the association between drug injection patterns and overdose. Multivariate analysis was conducted to control for factors that could potentially confound the main association. All analyses were conducted using StataSE Version 12 (StataCorp, College Station, TX).
To examine trends in the drug reported as most frequently injected, we used the Cochran-Armitage test for trend over multiple years. We examined evidence for or against a constant level of the proportion of those reporting a certain drug as the most frequently injected across time. Trend analysis was conducted using XLSTAT (Addinsoft, New York, NY).
Results
Trend in most frequently injected drug
Since 2005, the proportion of participants reporting methamphetamine as their most frequently injected drug has steadily increased from 2.1% in 2005 to 13.3% in 2009 to 20.5% in 2012 to 29.6% in 2015 (p-value for Cochran-Armitage < 0.001; Figure 1). During that same time frame, the proportion of participants reporting heroin as their most frequently injected drug has fluctuated with 48.4% in 2005 to 72.4% in 2009 to 62.4% in 2012 and 58.4% in 2015. The proportion of participants reporting cocaine as their most frequently injected drug steadily decreased from 21.8% in 2005 to 2.7% in 2015 (p-value for Cochran-Armitage = 0.005).
Figure 1.
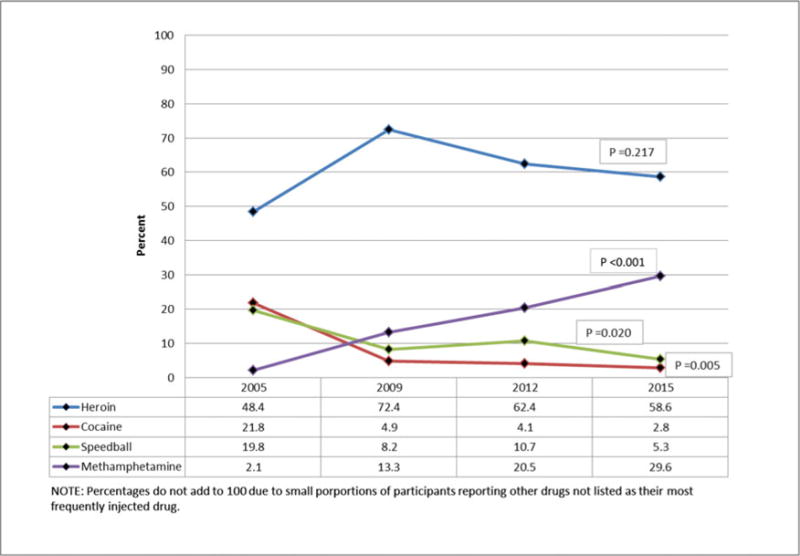
Most frequently injected drug among persons who inject drugs. Source: National HIV Behavioral Surveillance, Denver, Colorado, 2005–2015.
Characteristics of the 2015 NHBS study population
A total of 710 persons were screened for the 2015 cycle of NHBS in Denver, of whom 609 (85.8%) were eligible to participate and 592 (83.4%) completed the local questionnaire. The final sample included 19 (3.2%) seed participants, all of whom were 29 years or younger. Younger seeds were purposefully recruited in an attempt to generate a sample which more accurately represents the PWID population. Approximately three quarters (71.4%) of participants were male and more than half (58.8%) identified as non-Hispanic white (Table 1). Nearly one-quarter (22.1%) were 29 years or younger. A large proportion of participants reported experiencing homelessness with 67.1% reporting being currently homeless and 14.7% reporting being homeless, but not in the past 12 months. Among male participants, 53 (12.6%) reported having oral or anal sex with a man in the past 12 months.
Table 1.
Demographic characteristics by drug injection pattern in the past 12 months in a sample of persons who inject drugs.
| Total n (%) |
Heroin only n (%) | Methamphetamine only n (%) | Both heroin and methamphetamine n (%) | p-value | |
|---|---|---|---|---|---|
| Overall* | 592 | 173 (29.2) | 123 (20.8) | 296 (50.0) | |
| Gender | |||||
| Male | 421 (71.4) | 114 (67.6) | 89 (73.0) | 215 (72.9) | 0.435 |
| Female | 169 (28.6) | 56 (32.4) | 33 (27.0) | 80 (27.1) | |
| Race/Ethnicity | |||||
| White, non-Hispanic | 348 (58.8) | 78 (45.1) | 70 (56.9) | 200 (67.6) | <0.001 |
| Black, non-Hispanic | 35 (5.9) | 18 (10.4) | 9 (7.3) | 8 (2.7) | |
| Hispanic | 148 (25.0) | 64 (37.0) | 26 (21.1) | 58 (19.6) | |
| Other | 61 (10.3) | 13 (7.5) | 18 (14.6) | 30 (10.1) | |
| Age | |||||
| 18–29 | 131 (22.1) | 28 (16.2) | 16 (13.0) | 87 (29.4) | <0.001 |
| 30–39 | 164 (27.7) | 30 (17.30 | 26 (21.1) | 108 (36.5) | |
| 40–49 | 142 (24.0) | 41 (23.7) | 43 (35.0) | 58 (19.6) | |
| ≥50 | 155 (26.2) | 74 (42.8) | 38 (30.9) | 43 (14.5) | |
| Homeless in past 12 months | |||||
| No | 108 (18.2) | 65 (37.6) | 19 (15.5) | 24 (8.1) | < 0.001 |
| No, longer than 12 months | 87 (14.7) | 27 (15.6) | 16 (13.0) | 44 (14.9) | |
| Yes, currently homeless | 397 (67.1) | 81 (46.8) | 88 (71.5) | 228 (77.0) | |
| Reported network size | |||||
| 0–5 other PWID | 72 (12.2) | 30 (14.3) | 21 (17.1) | 21 (7.1) | < 0.001 |
| 6–20 other PWID | 213 (36.0) | 75 (43.4) | 43 (35.0) | 95 (32.1) | |
| 21–50 other PWID | 169 (28.6) | 38 (22.0) | 35 (28.5) | 96 (32.4) | |
| 51–100 other PWID | 86 (14.5) | 17 (9.8) | 17 (13.8) | 52 (17.6) | |
| Over 100 other PWID | 52 (8.8) | 13 (7.5) | 7 (5.7) | 32 (10.8) | |
| Male-male sexual activity past 12 months | |||||
| Yes | 53 (12.6) | 6 (5.1) | 19 (21.4) | 28 (13.0) | 0.002 |
| No | 368 (87.4) | 111 (94.9) | 70 (78.7) | 187 (87.0) |
Source: National HIV Behavioral Surveillance (NHBS), Denver, Colorado, 2015.
Subcategory total may not add to overall total due to missing data.
Heroin and methamphetamine injection
Approximately half of the participants reported injecting both heroin and methamphetamine during the past 12 months (Table 1). When asked about the usual method of injection, 130 (43.9%) reported injecting the drugs separately at different times, 83 (28.0%) reported mixing the drugs together and injecting (this is called a “goof-ball”), and 71 (24.0%) reported doing both (data not shown). Participants who reported injecting both heroin and methamphetamine were significantly more likely to be white, non-Hispanic, younger, currently homeless, and report knowing larger numbers of other PWID that they have seen in the past 30 days.
Injection characteristics
Overall, 7.3% of participants were recent injectors reporting that their first injection was within the past year (Table 2). A total of 244 (41.2%) participants reported heroin as the first drug they ever injected while 176 (29.7%) reported methamphetamine as their first injected drug. Nearly 80% of participants reported injecting once or more than once a day. Participants who reported injecting both heroin and methamphetamine (79.7%) were significantly more likely to report injecting more than once a day compared to those only injecting heroin and those only injecting methamphetamine, 61.9% and 45.5%, respectively. Participants who reported injecting heroin and methamphetamine were also more likely to report reusing syringes. In addition, those who reported injecting both heroin and methamphetamine were more likely to report sharing a syringe at least once in the past 12 months but less likely to report sharing water, cookers, or cottons (Table 2).
Table 2.
Injection characteristics by drug injection pattern in the past 12 months in a sample of persons who inject drugs.
| Total n (%) |
Heroin only n (%) | Methamphetamine only n (%) | Both heroin and methamphetamine n (%) | p-value | |
|---|---|---|---|---|---|
| Overall* | 592 | 173 (29.2) | 123 (20.8) | 296 (50.0) | |
| Years since first injection | |||||
| ≤ 1 year | 43 (7.3) | 8 (4.6) | 12 (9.8) | 23 (7.8) | <0.001 |
| 2–3 years | 62 (10.5) | 10 (5.8) | 10 (8.1) | 42 (14.2) | |
| 4–6 years | 65 (11.0) | 15 (8.7) | 10 (8.1) | 40 (13.5) | |
| 7–10 years | 79 (13.3) | 16 (9.3) | 14 (11.4) | 49 (16.6) | |
| > 10 years | 343 (57.9) | 124 (71.7) | 77 (62.6) | 142 (48.0) | |
| First drug injected | |||||
| Heroin | 244 (41.2) | 111 (64.2) | 7 (5.7) | 126 (42.6) | <0.001 |
| Methamphetamine | 176 (29.7) | 11 (6.4) | 77 (62.6) | 88 (29.7) | |
| Cocaine | 132 (22.3) | 41 (23.7) | 31 (25.2) | 60 (20.3) | |
| Other | 40 (6.8) | 10 (5.8) | 8 (6.5) | 22 (7.4) | |
| Frequency of injection in past 12 months | |||||
| More than once a day | 399 (67.4) | 107 (61.9) | 56 (45.5) | 236 (79.7) | < 0.001 |
| Once a day | 69 (11.7) | 27 (15.6) | 15 (12.2) | 27 (9.1) | |
| More than once a week | 61 (10.3) | 21 (12.1) | 25 (20.3) | 15 (5.1) | |
| Once a week or less | 63 (10.6) | 18 (10.4) | 27 (22.0) | 18 (6.1) | |
| Frequency of syringe reuse in past | |||||
| 12 months | |||||
| Never | 145 (24.5) | 44 (25.4) | 44 (35.8) | 57 (19.3) | 0.004 |
| Once | 108 (18.2) | 31 (17.9) | 27 (22.0) | 50 (16.9) | |
| 2–3 times | 252 (42.6) | 75 (43.4) | 40 (32.5) | 137 (46.3) | |
| 4 or more times | 87 (14.7) | 23 (13.3) | 12 (9.8) | 52 (17.6) | |
| Shared syringe in past 12 months | |||||
| No | 387 (66.2) | 121 (70.8) | 99 (81.2) | 167 (57.2) | < 0.001 |
| At least once | 198 (33.8) | 50 (29.2) | 23 (18.9) | 125 (42.8) | |
| Shared water, cooker, cottons in past 12 months | |||||
| No | 246 (42.1) | 75 (43.9) | 83 (68.0) | 88 (30.1) | < 0.001 |
| At least once | 339 (57.9) | 96 (56.1) | 39 (32.0) | 204 (49.9) |
Source: National HIV Behavioral Surveillance (NHBS), Denver, Colorado, 2015.
Subcategory total may not add to overall total due to missing data.
HIV/HCV infection
A total of 341 (60.5%) participants were infected with HCV and 21 (3.6%) were infected with HIV (Table 3). Among participants who were HIV infected, the proportion was higher among those who reported injecting methamphetamine only (11.1%) compared to those who reported injecting both methamphetamine and heroin (2.0%). Among participants who were HCV infected, the proportion was higher among those who reported injecting heroin only (67.9%) compared to those who reported injecting both (63.7%).
Table 3.
HIV and HCV test results, harm reduction characteristics, incarceration, and overdose by drug injection pattern in the past 12 months in a sample of persons who inject drugs.
| Total n (%) |
Heroin only n (%) | Methamphetamine only n (%) | Both heroin and methamphetamine n (%) | p-value | |
|---|---|---|---|---|---|
| Overall* | 592 | 173 (29.2) | 123 (20.8) | 296 (50.0) | |
| HIV rapid test result | |||||
| Reactive | 21 (3.6) | 2 (1.2) | 13 (11.1) | 6 (2.0) | < 0.001 |
| Non-reactive | 561 (96.4) | 169 (98.8) | 104 (88.9) | 288 (98.0) | |
| HCV rapid test result | |||||
| Reactive | 341 (60.5) | 112 (67.9) | 50 (42.4) | 179 (63.7) | < 0.001 |
| Non-reactive | 223 (39.5) | 53 (32.1) | 68 (57.6) | 102 (36.3) | |
| Visited local syringe exchange past 12 months | |||||
| Yes | 378 (63.9) | 98 (56.7) | 57 (46.3) | 223 (75.3) | < 0.001 |
| No | 214 (36.2) | 75 (43.4) | 66 (53.7) | 73 (24.7) | |
| Received naloxone kit in past 12 months | |||||
| Yes | 194 (32.8) | 52 (30.1) | 17 (13.8) | 125 (42.2) | < 0.001 |
| No | 353 (59.6) | 115 (66.5) | 77 (62.6) | 161 (54.4) | |
| Don’t know what naloxone is | 45 (7.6) | 6 (3.5) | 29 (23.6) | 10 (3.4) | |
| Held in detention center, jail, or prison for more than 24 hours in past 12 months | |||||
| Yes | 320 (58.4) | 73 (47.1) | 61 (53.0) | 186 (66.9) | < 0.001 |
| No | 228 (41.6) | 82 (52.9) | 54 (47.0) | 92 (33.1) | |
| Overdose in past 12 months | |||||
| No | 463 (78.2) | 153 (88.4) | 114 (92.7) | 196 (66.2) | < 0.001 |
| Once | 72 (12.2) | 12 (6.9) | 5 (4.1) | 55 (18.6) | |
| Two or more times | 57 (9.6) | 8 (4.6) | 4 (3.3) | 45 (15.2) |
Source: National HIV Behavioral Surveillance (NHBS), Denver, Colorado, 2015.
Subcategory total may not add to overall total due to missing data.
Harm reduction characteristics
Nearly two-thirds (63.9%) of participants reported visiting a syringe access program during the past 12 months (Table 3). Participants who reported injecting both heroin and methamphetamine were significantly more likely to report visiting a syringe access program compared to those reporting methamphetamine injection only and those who reported heroin injection only. In addition, those reporting heroin and methamphetamine injection were more likely to report receiving a naloxone kit in the past 12 months.
Overdose
Participants who reported injecting both heroin and methamphetamine were significantly more likely to report overdosing in the past 12 months with 18.6% reporting overdosing once and 15.2% reporting overdosing two or more times during the past 12 months (Table 3). Among those who reported injecting both drugs, we examined reported overdose by the usual method of injection. Participants who reported that they injected the drugs separately at different times were slightly more likely to report at least one overdose in the past 12 months compared to those who reported mixing the drugs and then injecting and those reporting both methods, 38.9% vs. 20.7% and 38.0%, respectively (p = 0.015). After adjusting for race/ethnicity, age, frequency of injection, being held in a detention center, jail, or prison for more than 24 hours in the past 12 months, and homelessness, injecting both heroin and methamphetamine was associated with a 2.8 (95% confidence interval: 1.7, 4.5) fold increase in the risk of overdose in the past 12 months compared with only injecting heroin (Table 4).
Table 4.
Association between overdose and drug injection pattern in the past 12 months in a sample of persons who inject drugs.
| Overdosed at least once n (%) |
Unadjusted prevalence ratio (95% CI) | Adjusted prevalence ratio* (95% CI) | |
|---|---|---|---|
| Drug injection pattern | |||
| Heroin only | 20 (11.6) | 1.0 (ref) | 1.0 (ref) |
| Methamphetamine only | 9 (7.4) | 0.63 (0.30,1.35) | 0.64 (0.29, 1.43) |
| Both heroin and methamphetamine | 99 (33.6) | 2.89 (1.85,4.49) | 2.80 (1.72,4.53) |
Source: National HIV Behavioral Surveillance (NHBS), Denver, Colorado, 2015.
Adjusted for race/ethnicity, age, frequency of injection, incarceration, and homelessness.
Discussion
In Denver, a growing number of PWID are injecting both heroin and methamphetamine. To date, only a handful of studies have reported a similar phenomenon (Bluthenthal et al., 2015; Cedarbaum & Banta-Green, 2016; Ochoa et al., 2005; Peavy et al., 2012). However, these studies only reported the use of goofballs, the injection of both drugs simultaneously in a single shot, or injected separately during the same injection episode. PWID may also consider injecting heroin and smoking methamphetamine, another form of goofball. Our results indicate that, while common, goofballs are but one way these two drugs are used in concert. While 28% of participants reported injecting goofballs, more than 40% reported injecting both drugs, but at separate times, and a quarter of participants reported injecting goofballs and injecting the drugs separately.
Increasingly, methamphetamine use and the primary methamphetamine indicators used by the Community Epidemiology Work Groups across the 20 representative regions appear to be on the rise in the Western United States (National Institute on Drug Abuse, 2014). Reporting an exhaustive analysis of data sources, including drug trafficking data from the US Drug Enforcement Agency, drug treatment admissions data, drug-treated emergency department visits, and arrestee drug monitoring data, Pollini and Strathdee documented a substantial increase in the use of methamphetamine in San Diego County, California between 2001 and 2005 (Pollini & Strathdee, 2007). However, less is known about poly-drug use in markets dominated by black tar heroin and methamphetamine, such as the Southwestern United States. A more recent latent class analysis explored polydrug use among PWID in San Diego to examine habitual drug use to identify distinct patterns of heroin and methamphetamine mixing in a drug market that is characterized predominantly by black tar heroin and methamphetamine (Roth et al., 2015). While this study identified characteristics of two distinct classes of drug use, primarily methamphetamine users with multiple routes of administration and primarily heroin injectors, simultaneous injection of methamphetamine and heroin were excluded from the analysis. A second latent class analysis to identify classes of polydrug use among heroin users in Tijuana, Mexico, concluded that a majority of individuals who use both heroin and methamphetamine report a simultaneous injection of these substances (Meacham et al., 2015). The study authors also found the injection of heroin and methamphetamine together was significantly associated with receptive and distributive syringe sharing, marginally associated with both overdose and drug use before. Identifying another heroin and methamphetamine drug use pattern in San Francisco, California, Harris and colleagues found that both injected and noninjected methamphetamine use was more prevalent among people who inject heroin infrequently, suggesting that this group comprises primary methamphetamine users who use heroin to come “down” from methamphetamine (Harris et al., 2013).
Our results showing that PWID who used both heroin and methamphetamine in Denver were more likely to be homeless supports the finding of recent ethnographic research describing an increase in methamphetamine use among homeless heroin injectors and linking it, in part, to the city’s new ordinances that control the use of public space (Langegger & Koester, 2016a, 2016b). In 2012, the city passed a camping ban rendering it illegal to dwell “temporarily in a place, with shelter.” The ordinance goes on to define dwelling as conducting activities such as eating, sleeping and the storage of personal possessions. The wording of the ban describes shelter as: “any tent, tarpaulin, lean-to, sleeping bag, bedroll, blankets, or any other form of protection from the elements other than clothing.” In the City of Denver, sleeping in public space is no longer an option. Resting with ‘shelter’ now violates municipal code. Shelters are an option. However, for undomiciled persons, many of whom see shelters as patronizing, crowded, and often dangerous places, the option of using homeless shelters is less preferable than being on the street. Consequently, incessant motion and staying awake become viable options for avoiding interactions with the police and/or being cited for violating the camping ban (Hopper & Barrow, 2003). Methamphetamine provides homeless PWID with a pharmacological aid for responding to this structurally imposed risk environment (Koester, Langegger, & Al-Tayyib, 2016).
The combined use of methamphetamine and heroin may have important implications for blood-borne disease transmission and overdose. Injecting both drugs was associated with more injection risk and knowing large numbers of other PWID. Participants who use both drugs were significantly more likely to inject multiple times per day compared to PWID who reported injecting either heroin or methamphetamine only. They were also more likely to report syringe reuse as well as sharing a syringe at least once in the past 12 months. PWID who injected both drugs reported knowing larger numbers of other PWID that they had seen in the past 30 days suggesting that they may have larger and more open drug using networks. Fortunately, PWID who reported the use of both drugs were more likely to use the services of the city’s two syringe access programs.
Although studies have found associations between overdose and polydrug use trends combining heroin with sedatives, and heroin with cocaine, the literature on the potential link between overdose and the combined use of heroin and methamphetamine is sparse at best. One study on nonfatal overdose in Seattle found an association with goofball injecting in bivariate analysis, however, in multivariate analysis, only recent incarceration and sharing injection paraphernalia remained significantly associated with overdose (Jenkins et al., 2011). Another study of overdose in San Francisco found injection of heroin mixed with methamphetamine in the past 3 months to be an independent predictor of overdose (Ochoa et al., 2005). Our results indicate the association between nonfatal overdose and the combined use of methamphetamine and heroin is not limited to the injection of goofballs but includes other patterns of combined use including injecting the drugs separately at different times of the day. Just over a third of participants who inject both heroin and methamphetamine reported overdosing at least once in the past 12 months, with 15% reporting that they overdosed more than once. Data from the Office of the Denver Medical Examiner provides additional evidence for a link between the combined use of heroin and methamphetamine and overdose. There was a fourfold increase in deaths involving both heroin and methamphetamine from 4 in 2005 to 16 in 2015 (J. Caruso, personal communication, May 12, 2016).
Our findings are subject to several limitations. First, some participants might not have reported their behaviors accurately due to the survey being administered by an interviewer. Second, while we did perform confirmatory testing for those with a reactive rapid HIV test, we did not run RNA tests on samples from participants who were HCV antibody positive so our HCV numbers may include individuals who have cleared the infection. Third, though participants were recruited using RDS, we do not present RDS-weighted estimates. Fourth, the study was a cross-sectional survey therefore causality cannot be inferred. Finally, our results are limited to respondents in one urban city and may not be generalizable to PWID in other parts of the United States.
Conclusion
It seems surprising that the combined use of heroin and methamphetamine has not received more attention. At least in the case of Denver, it has become a predominant drug pattern, particularly among homeless PWID. As our results indicate, the combination of heroin and methamphetamine involves more than goofball injecting and appears to have important public health implications, including increased risk of overdose. We would suggest that this drug use pattern merits further research including research on the factors that drive it, the forms of use it includes, and the potential health concerns it raises.
Acknowledgments
Funding
This work was supported by the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention [Grant number 5U1BPS003251] and the National Institute on Drug Abuse [Grant number K01DA036452].
Footnotes
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
References
- Arreola S, Bluthenthal RN, Wenger L, Chu D, Thing J, Kral AH. Characteristics of people who initiate injection drug use later in life. Drug and Alcohol Dependence. 2014;138:244–250. doi: 10.1016/j.drugalcdep.2014.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluthenthal RN, Wenger L, Chu D, Lorvick J, Quinn B, Thing JP, Kral AH. Factors associated with being asked to initiate someone into injection drug use. Drug and Alcohol Dependence. 2015;149:252–258. doi: 10.1016/j.drugalcdep.2015.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cedarbaum ER, Banta-Green CJ. Health behaviors of young adult heroin injectors in the Seattle area. Drug and Alcohol Dependence. 2016;158:102–109. doi: 10.1016/j.drugalcdep.2015.11.011. [DOI] [PubMed] [Google Scholar]
- Denver Office of Drug Strategy. Proceedings of the Denver Epidemiology Work Group, Spring 2015 report. 2015 Retrieved from http://denverdrugstrategy-public.sharepoint.com/SiteAssets/Pages/Program-Data/DEWG%20Report%20Spring%202015.pdf.
- Harris JL, Lorvick J, Wenger L, Wilkins T, Iguchi MY, Bourgois P, Kral AH. Low-frequency heroin injection among out-of-treatment, street-recruited injection drug users. Journal of Urban Health. 2013;90(2):299–306. doi: 10.1007/s11524-012-9720-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckathorn DD. Respondent-driven sampling: A new approach to the study of hidden populations. Social Problems. 1997;44(2):174–199. [Google Scholar]
- Hopper K, Barrow SM. Two genealogies of supported housing and their implications for outcome assessment. Psychiatric Services. 2003;54(1):50–54. doi: 10.1176/appi.ps.54.1.50. [DOI] [PubMed] [Google Scholar]
- Jenkins LM, Banta-Green CJ, Maynard C, Kingston S, Hanrahan M, Merrill JO, Coffin PO. Risk factors for nonfatal overdose at Seattle-area syringe exchanges. Journal of Urban Health. 2011;88(1):118–128. doi: 10.1007/s11524-010-9525-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM, Logan J, Gladden RM, Bohm MK. Vital signs: Demographic and substance use trends among heroin users - United States, 2002–2013. MMWR Morbidity and Mortality Weekly Report. 2015;64(26):719–725. [PMC free article] [PubMed] [Google Scholar]
- Koester S, Langegger S. “Never be stationary”: Survival drug use in the neoliberal city. Presented at the American Anthropological Association Annual Meeting; Denver, CO: 2015. Nov, [Google Scholar]
- Koester S, Langegger S, Al-Tayyib A. Never be stationary: Survival drug use in the neoliberal city. 2016 Manuscript submitted for publication. [Google Scholar]
- Langegger S, Koester S. Dwelling without a home: Denver’s splintered public spaces. In: DeBacker M, Megaco L, Varna G, Menichellil F, editors. Criminology meets geography: Order and conflict in public space. New York, NY: Routledge; 2016a. pp. 140–159. [Google Scholar]
- Langegger S, Koester S. Invisible homelessness: Anonymity, exposure and the right to the city. Urban Geography. 2016b;37:1030–1048. [Google Scholar]
- Meacham MC, Rudolph AE, Strathdee SA, Rusch ML, Brouwer KC, Patterson TL, Roesch SC. Polydrug use and HIV risk among people who inject heroin in Tijuana, Mexico: A latent class analysis. Substance Use & Misuse. 2015;50(10):1351–1359. doi: 10.3109/10826084.2015.1013132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Drug Early Warning System. NDEWS Sentinel Community Site advance report 2016: Selected findings for heroin, fentanyl, and methamphetamine. 2016 Retrieved from https://ndews.umd.edu/sites/ndews.umd.edu/files/u1424/2016_ndews_scs_advance_report_final.pdf.
- National Institute on Drug Abuse. Epidemiologic trends in drug abuse: Proceedings of the Community Epidemiology Work Group. 2014 Retrieved from https://www.drugabuse.gov/sites/default/files/cewg_jan2014_execsumm.pdf.
- Ochoa KC, Davidson PJ, Evans JL, Hahn JA, Page-Shafer K, Moss AR. Heroin overdose among young injection drug users in San Francisco. Drug and Alcohol Dependence. 2005;80(3):297–302. doi: 10.1016/j.drugalcdep.2005.04.012. [DOI] [PubMed] [Google Scholar]
- Peavy KM, Banta-Green CJ, Kingston S, Hanrahan M, Merrill JO, Coffin PO. Hooked on” prescription-type opiates prior to using heroin: Results from a survey of syringe exchange clients. Journal of Psychoactive Drugs. 2012;44(3):259–265. doi: 10.1080/02791072.2012.704591. [DOI] [PubMed] [Google Scholar]
- Pollini RA, Strathdee SA. Indicators of methamphetamine use and abuse in San Diego County, California: 2001–2005. Journal of Psychoactive Drugs. 2007;(Suppl 4):319–325. doi: 10.1080/02791072.2007.10399893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth AM, Armenta RA, Wagner KD, Roesch SC, Bluthenthal RN, Cuevas-Mota J, Garfein RS. Patterns of drug use, risky behavior, and health status among persons who inject drugs living in San Diego, California: A latent class analysis. Substance Use & Misuse. 2015;50(2):205–214. doi: 10.3109/10826084.2014.962661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health (HHS Publication No SMA 15-4927) 2015 Retrieved from https://www.samhsa.gov/data/sites/default/files/NSDUH-FRR1-2014/NSDUH-FRR1-2014.htm.
- U.S. Department of Drug Enforcement Administration. National heroin threat assessment summary (DEA-DCT-DIR-031-16) 2016 Retrieved from https://www.dea.gov/divisions/hq/2015/hq052215_National_Heroin_Threat_Assessment_Summary.pdf.
- U.S. Department of Drug Enforcement Administration. 2015 national drug threat assessment summary (DEA-DCT-DIR-008-16) 2015 Retrieved from https://www.dea.gov/docs/2015%20NDTA%20Report.pdf.


