Abstract
Objective
To examine whether or not an edrophonium challenge test is useful for diagnosing cervical dystonia.
Patients
We evaluated 10 patients with cervical dystonia and 10 with hemifacial spasms (disease controls). We administered edrophonium and saline in this double-blinded study. Before and after the injection, we recorded the participants' clinical signs using a video camera to assess the objective symptoms every two minutes. Ten minutes after the saline and edrophonium injections, participants evaluated their subjective clinical signs using a visual analog scale. The objective signs on the video recordings were scored by specialists who were blinded to the treatment. The mean visual analog scale scores were compared using the Wilcoxon rank-sum test for paired continuous variables.
Results
The clinical signs of participants with cervical dystonia were amplified by edrophonium. In contrast, the clinical signs in participants with hemifacial spasms were not affected by the edrophonium challenge test.
Conclusion
The edrophonium challenge test may be useful for diagnosing cervical dystonia.
Keywords: cervical dystonia, edrophonium
Introduction
Dystonia is a clinical syndrome characterized by sustained muscle contractions that cause twisting and repetitive movements or abnormal postures (1). The classification of dystonia has developed with increasing knowledge, and different schemes have been suggested, including the age at onset, body distribution, and etiology as the main differentiating factors (2). The most frequent phenotype in primary dystonia is adult-onset focal dystonia. Furthermore, the most frequent phenotypes in primary adult onset focal dystonia is blepharospasm, cervical dystonia, and hand dystonia (3). As few autopsies are performed, the pathology and pathophysiology of primary dystonia are unknown, except for hereditary dystonia, such as DYT3 dystonia (4). According to an electrophysiological study, sensory-motor mismatch in the central nervous system (CNS) is suggested as the cause (5). Dystonia is typically diagnosed by excluding any secondary diseases and neuropsychiatric disorders, as specific tests for dystonia are currently unavailable.
Balash and Giladi concluded that high doses of trihexyphenidyl (an anticholinergic agent) are effective, especially for treating segmental and generalized dystonia in young patients (6). It has been reported that anticholinergic agents improve the symptoms of dystonia; however, if involuntary movement of the neck is caused by cervical dystonia, then the symptoms may be made more apparent by a cholinergic agent.
Edrophonium chloride is an acetylcholinesterase inhibitor with a rapid onset (approximately 30 seconds) and short duration (approximately 5 minutes). The suppression of dysfunctional eyelid closure by administering edrophonium is used to diagnose myasthenia gravis (MG) (7). Edrophonium is hydrophilic, with a limited capacity to cross the blood-brain barrier. In addition, edrophonium is rapidly excreted by the kidneys, suggesting limited direct efficacy in the CNS (8-10). However, in our study, blepharospasm was amplified after administering edrophonium, which suggests that edrophonium may be useful for diagnosing dystonia (11).
In the present study, we examined whether or not an edrophonium challenge test was useful for diagnosing cervical dystonia. We hypothesized that edrophonium chloride, an acetylcholinesterase inhibitor, might make the symptoms of cervical dystonia more apparent. To investigate our hypothesis, we examined the clinical symptoms of 10 patients with cervical dystonia after administering edrophonium injections. We also administered physiological saline as a control and examined patients with hemifacial spasms as a disease control.
Materials and Methods
Participants
This study included 10 patients with cervical dystonia (7 men and 3 women; age range, 34-73 years) and 10 with hemifacial spasms (control group: 4 men and 6 women; age range, 46-78 years) (Table 1). Cervical dystonia was clinically diagnosed according to the definition by Fahn (12). All participants were examined by a single movement disorder specialist (S.M.) who performed general physical and neurological examinations, laboratory tests, and brain magnetic resonance imaging to exclude other causes of dystonia, including birth injury and head trauma. Patients with a history of heart disease and arrhythmia were excluded from participating in the study for their safety. All subjects underwent a 12-lead electrocardiography examination and a chest radiography examination before the study was performed to exclude those with a cardiac disease. In this study, there was no special provision for treatment before the trial commenced.
Table 1.
| A) Clinical characteristics of participants with cervical dystonia and hemifacial spasms | |||
|---|---|---|---|
| No. of participants (women) | Mean age (SD) | Age of onset (SD) | |
| Cervical dystonia | 10 (3) | 49.8 (13.3) | 45.3 (16.4) |
| Hemifacial spasms | 10 (6) | 65.3 (9.1) | 59.0 (11.5) |
SD: standard deviation
| B) Profile of patients with cervical dystonia | |||||
|---|---|---|---|---|---|
| Patient no. | Sex | Symptoms | Age (years) | Age of onset (years) | Tsui score |
| 1 | Male | Lt rotation, posterior flexion | 37 | 29 | 8 |
| 2 | Female | Rt rotation, anterior flexion | 40 | 30 | 9 |
| 3 | Male | Lt rotation, anterior flexion | 34 | 30 | 8 |
| 4 | Female | Rt rotaion, anterior flexion | 45 | 36 | 8 |
| 5 | Male | Lt flexion, shoulder elevation | 42 | 37 | 7 |
| 6 | Male | Rt flexion, shoulder elevation | 44 | 42 | 7 |
| 7 | Male | Lt rotation | 56 | 53 | 6 |
| 8 | Male | Rt rotation, anterior flexion | 65 | 55 | 8 |
| 9 | Male | Rt rotaion, anterior flexion | 62 | 64 | 8 |
| 10 | Female | Lt rotation | 73 | 77 | 6 |
SD: standard deviation, Lt: left, Rt: right
All participants with cervical dystonia had a Tsui scale score of more than 6, and we only included subjects with moderate and severe symptoms, as mild symptoms could not be determined by videos (described later) that documented their clinical symptoms. The degree of severity in patients with hemifacial spasm was determined based on their symptoms, which were confirmed by the videos.
This investigation was approved by the institutional ethics committee of Shinko Hospital. Written informed consent was obtained from all participants. The study was registered with an International Committee of Medical Journal Editors-recognized registry, the UMIN Clinical Trials Registry (number: UMIN000022557).
Administration of edrophonium and the evaluation of subjective symptoms
This was a double-blind study, as the participants and evaluators were blinded to the identity of the drug (saline or edrophonium). The protocol used for the edrophonium challenge test is shown in Table 2. We explained to the participants that we would administer two kinds of drugs among three types that might improve their symptoms, not change their symptoms, or worsen their symptoms. First, we intravenously injected saline (10 mL). Before and after the injection, we recorded the participants' clinical symptoms with a video camera (EX-S600; Casio, Tokyo, Japan) to assess the objective signs every 2 minutes (each video was 1 minute long). Ten minutes after the saline injection, participants evaluated their subjective clinical signs using a visual analog scale (VAS) (13). We explained to the participants that the left end of the scale indicated the worst possible state, whereas the right end indicated a healthy state without cervical dystonia or hemifacial spasm. To evaluate the participants' symptoms after administration, we also explained that 50 mm on the VAS indicated their symptoms before administration. Second, we administered edrophonium (10 mg in 9 mL of saline) and recorded the clinical signs as described above. Participants were directed to self-evaluate their clinical signs separately from any side effects.
Table 2.
| Protocol for administering the edrophonium challenge test in participants with movement disorders |
| Evaluation of participants’ symptoms |
| 1. Videotape (1 min) recording of the objective symptoms before the injection |
| 2. Normal saline injection |
| 3. Two min after the injection: videotape recording |
| 4. Four min after the injection: videotape recording |
| 5. Six min after the injection: videotape recording |
| 6. Eight min after the injection: videotape recording |
| 7. Ten min after the injection: videotape recording |
| 8. Visual analog scale (VAS) test (evaluation after the normal saline injection) |
| 9. Edrophonium injection |
| 10. Two min after the injection: videotape recording |
| 11. Four min after the injection: videotape recording |
| 12. Six min after the injection: videotape recording |
| 13. Eight min after the injection: videotape recording |
| 14. Ten min after the injection: videotape recording |
| 15. VAS test (evaluation after the edrophonium injection) |
| Evaluation of the video by three movement disorder specialists |
| 1. We chose videos of the isotonic sodium chloride solution and edrophonium injections, which were randomly referred to as A and B, respectively |
| 2. We chose the video acquired 8 min after the administration of A or B, because the symptoms changed the most about 8 min after the edrophonium administration |
| 3. The video before the injection was reviewed |
| 4. The video after the injection of A was reviewed |
| 5. The modified VAS assessment was performed (the value after the A injection compared to that before the injection was used as the midline) |
| 6. The video before the injection of B was reviewed |
| 7. The video after the injection of B was reviewed |
| 8. The modified VAS assessment was performed (the value after the B injection compared to that before the injection was used as the midline) |
| We evaluated videos before and after the injection of A or B as a set. |
| We randomly presented the videos before and after the injection of A or B of cervical dystonia, hand dystonia, and hemifacial spasm to the specialists. |
Evaluation of objective symptoms
Three movement disorder specialists (N.M., H.K., and M.T.) who were blinded to the treatment and purpose of the examination independently evaluated the objective symptoms from the videos after administering saline and edrophonium, which were randomly named A and B. In the pilot study, we found that the symptoms changed the most about 8 minutes after edrophonium was administered. Therefore, we chose to evaluate the 1-minute videos acquired at 8 minutes after the administration. We presented the videos before and after the injection of A or B as a set. We randomly presented these sets of videos for cervical dystonia and hemifacial spasm to the specialists.
We used a modified VAS (mVAS) to evaluate the objective clinical signs. We used the mVAS to evaluate the objective signs of blepharospasm in a previous study and found that the objective signs of blepharospasm were amplified by the administration of edrophonium (11). The mVAS, the pre-administration baseline, was set at 50 mm (midline); the amelioration and exacerbation of symptoms were indicated by lower and higher numbers on the mVAS, respectively.
The final mVAS scores for the control and drug for each participant were the sum of each specialist's score. The VAS and mVAS scores were measured from the right side, with a higher score indicating more severe symptoms. Using the subjective score estimated with the VAS and the objective score estimated using the mVAS, we evaluated the change in symptoms in the patients with cervical dystonia and hemifacial spasm equally.
Statistical analyses
The mean VAS and mVAS scores were compared using the Wilcoxon rank-sum test for paired continuous variables. We calculated the relative value as follows: the VAS score after the edrophonium injection - the VAS score after the saline injection. The relative values were also compared using the Wilcoxon rank-sum test for paired continuous variables. All statistical tests were two-sided, and p values less than 0.05 were considered statistically significant. Statistical analyses were performed using the SPSS statistical software (version 11.0 for Windows; IBM, Armonk, USA).
Results
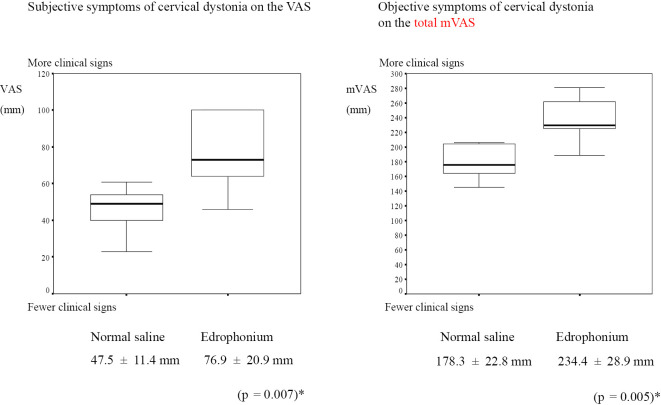
The VAS scores of the subjective clinical signs and the mVAS scores of the objective clinical signs are presented in Figs. 1, 2. Involuntary movements became obvious 4-8 minutes after edrophonium was injected. In participants with cervical dystonia, the VAS scores for the subjective signs and the mVAS scores for the objective signs were significantly higher after edrophonium was injected than after saline was injected (Fig. 1).
Figure 1.
Mean and SD values of the VAS and mVAS for placebo and edrophonium injections for cervical dystonia. SD: standard deviation, VAS: visual analog scale, mVAS: modified visual analog scale, *p indicates the difference in the VAS score between injections.
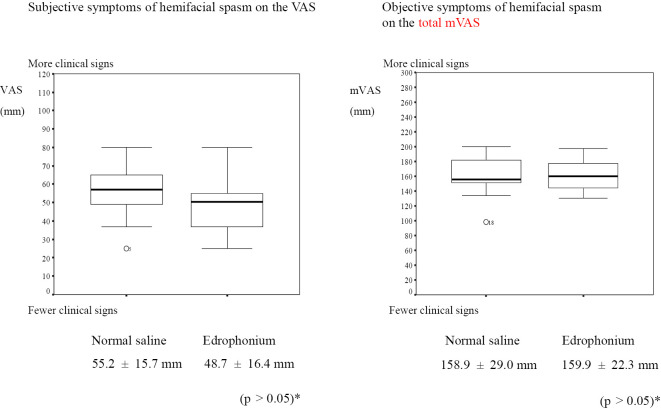
Figure 2.
Mean and SD values of the VAS and mVAS for placebo and edrophonium injections for hemifacial spasm. SD: standard deviation, VAS: visual analog scale, mVAS: modified visual analog scale, *p indicates the difference in the VAS score between injections.
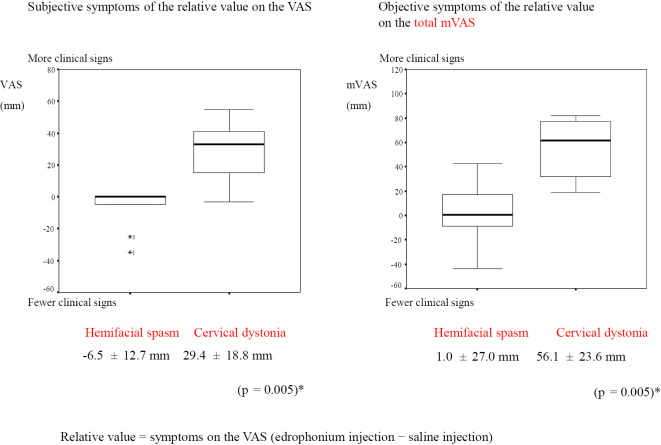
In participants with hemifacial spasms, no statistically significant difference was observed between the VAS and mVAS scores in the edrophonium injection and placebo groups (Fig. 2). The relative values were significantly higher in participants with cervical dystonia than in those with hemifacial spasms (Fig. 3).
Figure 3.
Mean and SD of the relative values for hemifacial spasm and cervical dystonia. SD: standard deviation, mVAS: modified visual analog scale, VAS: visual analog scale, *p indicates the difference in the VAS score between injections.
No severe muscarinic side effects such as bronchospasm or bradycardia were observed in this study. Typical muscarinic side effects (e.g. increased sweating, lacrimation, salivation, nausea, and diarrhea) were observed in all participants with cervical dystonia within the first minute. These side effects did not always appear when edrophonium was administered to participants with hemifacial spasms.
Discussion
The subjective and objective clinical signs of cervical dystonia were amplified by the administration of edrophonium; in contrast, the clinical signs of hemifacial spasm were not affected by the administration of edrophonium. Unlike the participants with hemifacial spasm, typical muscarinic side effects (e.g. increased sweating, lacrimation, and salivation) were observed in all participants with cervical dystonia within the first minute. It has been reported that dystonia is caused by a mismatch between motor and sensory signals. The strong reaction to edrophonium and the typical side effects observed following edrophonium administration may therefore be characteristics of dystonia. Cervical dystonia became obvious 4-8 minutes after the edrophonium injection. The primary feature of the edrophonium challenge test for cervical dystonia was a slow reaction time, unlike the edrophonium challenge test for MG. We also found that the subjective and objective relative values were significantly higher for cervical dystonia than for hemifacial spasm. Therefore, comparing the symptoms at the time of saline injection may result in a more accurate diagnosis.
In the clinical setting, cervical dystonia is typically diagnosed by excluding any secondary diseases and neuropsychiatric disorders, as specific tests for dystonia are unavailable. It has been reported that dystonia can occur with a peripheral nerve injury, after radiation therapy, and with congenital diseases (14-16). A differential diagnosis is supposed to be quite easy, made by observing the symptoms; however, clinically, it is difficult to completely exclude secondary diseases. If there is a history of secondary diseases or mental illness, making an objective diagnosis of primary dystonia is particularly difficult. In patients with complicated symptoms of dystonia (e.g. a muscle disease or congenital inflammatory peripheral disease as the underlying disease as well as abnormal neck posture), we cannot distinguish the cause of primary dystonia. For example, the occurrence of head drop is difficult to diagnose, because it is due to abnormal muscle contraction, weakness of the posterior neck muscles, a skeletal problem, or psychosomatic factor. In such cases, we need a test to aid in the diagnosis dystonia (17,18).
We performed the edrophonium challenge test in several patients with a combination of MG and dystonia. We noticed that, unlike for MG, the edrophonium challenge test response to dystonia was delayed by 7-8 minutes. Our double-blind study was designed with an observation time of 20 minutes. However, in routine practice, a long-term edrophonium challenge test is difficult to perform. Therefore, the protocol was designed so that, in all cases, physiological saline was administered first and edrophonium second, and the observation time was 10 minutes.
Multiple forms of dystonia are associated with genetic mutations, but the pathogenesis of sporadic dystonia is usually unclear. Abnormal plasticity in the basal ganglia (BG) is believed to be important to the disease etiology, and acetylcholine is a critical neuromodulator in the BG (19). As for why the reaction time to the edrophonium challenge test for cervical dystonia was slow, there are two possible sites of action for edrophonium: the CNS, including the BG, and the peripheral nerves (20).
It has been reported that edrophonium mitigates allodynia in an animal model of neuropathic pain, suggesting changes in afferent fiber transmission to the spinal cord that could in turn alter central sensorimotor integration (21). The effects of edrophonium on the neuromuscular junction and autonomic ganglia have been studied, but those on the CNS have not been studied. In the current study, dystonia became obvious 4-8 minutes after the edrophonium injection was administered, whereas the symptoms of MG improved within 1 minute. This delay suggests that the effects of edrophonium on cervical dystonia are centrally mediated by changes in afferent input.
We did not observe changes in the symptoms of participants with hemifacial spasm. There is now considerable evidence that primary hemifacial spasms are associated with vascular compression of the facial nerve at its root exit zone from the brainstem in almost all cases (22). Cholinesterase inhibitors have been shown to improve the symptoms in patients with neuromuscular junction disorders, but they do not affect peripheral nerve diseases. Therefore, for patients with hemifacial spasms, it was predicted that the symptoms would not change, which is not contradictory to our findings.
In cases of cervical dystonia, anticholinergic agent therapy can be effective or ineffective (23). The obvious symptoms induced by edrophonium are indirect proof that anticholinergic drugs are effective in patients who are responders to edrophonium. Further research is needed to establish whether or not the patients in whom the symptoms are exacerbated by edrophonium respond to anticholinergic agents.
In MG, the administration of edrophonium induces acetylcholine release, which subsequently improves the symptoms. Thus, the edrophonium challenge test has been established as a diagnostic tool for MG (7), and the safety of the edrophonium challenge test has been discussed (24). In our study, we performed a 12-lead electrocardiography examination and chest radiography before the study in all subjects to exclude the presence of cardiac disease, and no serious muscarinic side effects, such as bronchospasm and bradycardia, were observed. In Japan, physicians use edrophonium under electrocardiographic monitoring, and sulfuric acid atropine is used if a side effect of edrophonium (e.g. bradykinesia, abdominal pain, and salivation) is severe; thus, no severe side effects have been reported.
The Choi score is used as a scale for cervical dystonia (25). However, it is unsuitable for evaluating the delicate changes in cervical dystonia and hemifacial spasms after edrophonium is injected; we therefore used the mVAS for the evaluations. In addition, the Choi score is unsuitable for assessing cervical dystonia and hemifacial spasm. We used the mVAS to evaluate blepharospasm and hemifacial spasm before and after edrophonium was injected, and we found that the clinical signs of blepharospasm became obvious. Therefore, we determined that using the mVAS to perform the evaluations is appropriate.
In conclusion, our findings showed that the edrophonium challenge test is helpful for diagnosing cervical dystonia. Using the edrophonium challenge test can help reduce the rate of misdiagnoses and improve treatment efficacy. However, because of the small sample size and the fact that we did not randomize the order of the saline and edrophonium treatments, independent replication of this study with a larger sample size and treatment randomization is warranted.
The authors state that they have no Conflict of Interest (COI).
Supplementary Materials
References
- 1.Fahn S, Bressman SB, Marsden CD. Classification of dystonia. Adv Neurol 78: 1-10, 1998. [PubMed] [Google Scholar]
- 2.Skogseid IM. Dystonia-new advances in classification, genetics, pathophysiology and treatment. Acta Neurol Scand Suppl 198: 13-19, 2014. [DOI] [PubMed] [Google Scholar]
- 3.Matsuomto S, Nishimura , Shibasaki H, Kaji R. Epidemiology of primary dystonias in Japan comparison with Western countries. Mov Disord 18: 1196-1198, 2003. [DOI] [PubMed] [Google Scholar]
- 4.Goto S. A pathomechanism for the genesis of dystonia: striatal compartments and hypothesized model of basal ganglia circuits. Rinsho Shinkeigaku 46: 963-966, 2006. (in Japanese, Abstract in English). [PubMed] [Google Scholar]
- 5.Kaji R, Ikeda A, Ikeda T, et al. Physiological study of cervical dyatonia. Task specific abnormality in contingent negative variation. Brain 118: 11-22, 1995. [DOI] [PubMed] [Google Scholar]
- 6.Balash Y, Giladi N. Efficacy of pharmacological treatment of dystonia: evidence-based review including meta-analysis of the effect of botulinum toxin and other cure options. Eur J Neurol 11: 361-370, 2004. [DOI] [PubMed] [Google Scholar]
- 7.Pascuzzi RM. The edrophonium test. Semin Neurol 23: 83-88, 2003. [DOI] [PubMed] [Google Scholar]
- 8.Calvey TN, Williams NE, Muir KT, Barber HE. Plasma concentration of edrophonium in man. Clin Pharmacol Ther 19: 813-820, 1976. [DOI] [PubMed] [Google Scholar]
- 9.Gemmill JD, Venables GS, Ewing DJ. Noradrenaline response to edrophonium in primary autonomic failure: distinction between central and peripheral damage. Lancet 1: 1018-1021, 1988. [DOI] [PubMed] [Google Scholar]
- 10.Back DJ, Calvey TN. The removal of 14 C-edrophonium from the circulation. Br J Pharmacol 46: 355-357, 1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matsumoto S, Murakami N, Takahashi M, Izumi Y, Kaji R. Edrophonium challenge test for blepharospasm. Front Neurosci 10: 226, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fahn S. Concept and classification of dystonia. Adv Neurol 50: 1-8, 1988. [PubMed] [Google Scholar]
- 13.Mantha S, Thisted R, Foss J, Ellis JE, Roizen MF. A proposal to use confidence intervals for visual analog scale data for pain measurement to determine clinical significance. Anesth Analg 77: 1041-1047, 1993. [DOI] [PubMed] [Google Scholar]
- 14.Landan I, Cullis PA. Torticollis following radiation therapy. Mov Disord 2: 317-319, 1987. [DOI] [PubMed] [Google Scholar]
- 15.Chang S, Ishikawa T, Nonaka I, et al. [Merosin-positive congenital muscular dystrophy with early orthopaedic problems in relation to Ullrich's disease.]. No To Hattatsu 35: 159-164, 2003. (in Japanese, Abstract in English). [PubMed] [Google Scholar]
- 16.Cossu G, Melis M, Melis G, Ferrigno P, Molari A. Persistent abnormal shoulder elevation after accessory nerve injury and differential diagnosis with post-traumatic focal shoulder-elevation dystonia: report of a case and literature review. Mov Disord 19: 1109-1111, 2004. [DOI] [PubMed] [Google Scholar]
- 17.Hakan A, Karin EE, Anders J, Pelle N, Yngve O, Sten-Magnus A. Parkinsonism and neck extensor myopathy. Arch Neurol 58: 232-237, 2001. [DOI] [PubMed] [Google Scholar]
- 18.Ahmed MM, Lake WB, Resnick DK. Progressive severe kyphosis as a complication of multilevel cervical percutaneous facet neurotomy: a case report. Spine J 12: e5-e8, 2012. [DOI] [PubMed] [Google Scholar]
- 19.Peterson DA, Sejnowski TJ, Poizner H. Convergent evidence for abnormal striatal synaptic plasticity in dystonia. Neurobiol Dis 37: 558-573, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jankovic J. Peripherally induced movement disorders. Neurol Clin 27: 821-832, 2009. [DOI] [PubMed] [Google Scholar]
- 21.Hwang JH, Hwang KS, Leem JK, Park PH, Han SM, Lee DM. The antiallodynic effects of intrathecal cholinesterase inhibitors in a rat model of neuropathic pain. Anesthesiology 90: 492-499, 1999. [DOI] [PubMed] [Google Scholar]
- 22.Abbruzzese G, Berardelli A, Defazio G. Hemifacial spasm. Handb Clin Neurol 100: 675-680, 2011. [DOI] [PubMed] [Google Scholar]
- 23.Patel S, Martino D. Cervical dystonia from pathophysiology to pharmacotherapy. Behav Neurol 26: 275-282, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Okun MS, Charriez CM, Bhatti MT, Watson RT, Swift T. Tensilon and the diagnosis of myasthenia gravis: are we using the Tensilon test too much? Neurologist 7: 295-299, 2001. [DOI] [PubMed] [Google Scholar]
- 25.Jost WH, Hefter H, Stenner A, Reichel G. Rating scales for cervical dystonia: a critical evaluation of tools for outcome assessment of botulinum toxin therapy. J Neural Transm (Vienna) 120: 487-496, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.