Abstract
Objective
Dietary salt reduction is important for the prevention and treatment of lifestyle-related diseases, including hypertension. Thus, in order to follow a strict low-salt diet, it is necessary to assess one's salt intake and to become aware of the importance of salt reduction.
Methods
More than 2,000 employees of a company, who received a periodic health checkup, participated in the present study. They assessed their day-to-day diet-related lifestyle, using the Salt Check Sheet, and we analyzed the correlations among the Salt Check Sheet scores, the daily salt intake (as estimated by a spot urine sample), and the results of the periodic health checkup.
Results
In the overall survey population, we only found a weak correlation between the salt check scores and the salt intake. In a subgroup analysis, significant correlations between these two variables were observed among untreated hypertensive participants, but not among treated hypertensive participants. We examined the association between 13 individual questionnaire items and the estimated daily salt intake using a multivariate linear regression model and found that only 5 of the 13 questionnaire items were correlated with the daily salt intake.
Conclusion
We found that a Salt Check Sheet composed of the 5 items that showed a strong correlation with the salt intake might be more useful for periodic health checks of the working-age population.
Keywords: Salt Check Sheet, general foods, hypertension, salt intake, physical examination
Introduction
Many reports have demonstrated the involvement of dietary salt in the development and progression of hypertension. Conversely, salt reduction has been reported to be effective in the prevention and treatment of hypertension (1-3). Salt reduction is especially important in Japan, where the incidence of stroke, a major outcome of hypertension, is several times higher in comparison to the United States and European countries (4,5).
Although the World Health Organization (WHO) recommends a salt intake of <5 g/day (6), the recommended salt intake in Japanese adults was set at <8 g for men and <7 g for women in the “Dietary Reference Intakes for Japanese (2015)” established by the Japanese Government and the Ministry of Health, Labour and Welfare (MHLW) (7). According to the National Health and Nutrition Survey Japan (2015) by the MHLW, the mean daily salt intake is 11.1 g and 9.4 g in Japanese men and women, respectively, which is higher in comparison to men and women in the United States and European countries.
Thus, the reduction of one's salt intake is a major issue that cannot be avoided in the prevention and treatment of hypertension in Japan.
In the present study, we surveyed more than 2,000 participants about their salt intake-related lifestyle and their day-to-day diet using the Salt Check Sheet, and examined the correlations among the salt check scores, the daily salt intake and their periodic health checkup results.
Materials and Methods
A total of 2,317 participants received a health checkup in 2014 and provided their consent to participate in this study. They answered a questionnaire based on the Salt Check Sheet (8) created by Tsuchihashi et al., and we analyzed the correlation between their scores and their daily salt intake (estimated by a urinalysis). Of the 2,317 participants who provided consent to participate in this study, 116 participants were excluded from the analysis due to insufficient data regarding the Salt Check Sheet [56], health check [57], and urinalysis [8] (5 had multiple types of insufficient data). Thus, a total of 2,201 participants (95.0%) were included in the analysis.
We also analyzed the correlation between the results of a lifestyle survey and those of laboratory testing performed at the time of the health checkup. The present study was approved by the Ethics Committee on Human Tissue and Genome Research of Shionogi.
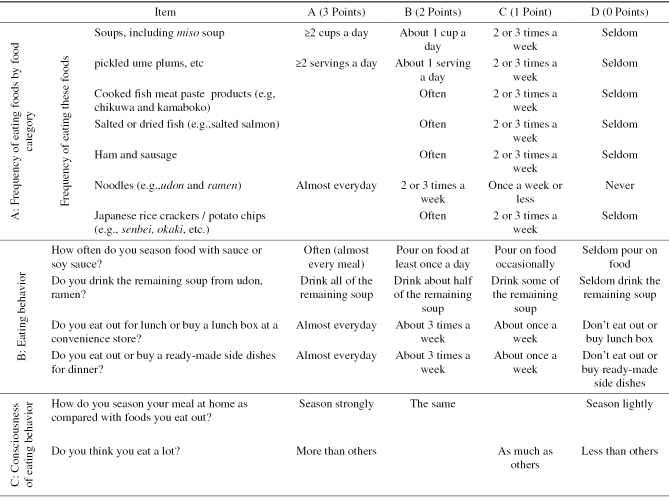
To examine salt intake-related lifestyle, we prepared a questionnaire (Table 1) consisting of 13 items related to eating habits, based on the Salt Check Sheet (1). This 13-item questionnaire is composed of 3 categories of questions that inquire about the respondent's salt intake-related lifestyle (the frequency of eating salty food [7 items], eating behavior [4 items], and consciousness of eating behavior [2 items]). Each item is scored on a 3- or 4-point scale from A to D (A: 3 points, B: 2 points, C: 1 point, and D: 0 points). The maximum possible total score was 35 points. We also asked the participants whether they had received a diagnosis of hypertension or diabetes mellitus. No information was provided to the respondents about scoring (score allocation) or the 3 question categories.
Table 1.
Questionnaire Items (Salt Check Sheet).
To estimate the participants' daily salt intake, we examined the urinary sodium and creatinine concentrations using spot urine samples collected at the time of their health checkup (SRL, Osaka, Japan). We defined the estimated daily salt intake using a formula created for estimating the 24-hour urinary salt excretion (9):
 |
Among all of the examination and interview items that were collected at the periodic health check in 2014, the following items were analyzed: age, height, body weight, body mass index (BMI), blood pressure, serum creatinine, HbA1c, blood glucose, uric acid, brain natriuretic peptide (BNP), weight gain or loss, exercise habits, walking speed, sleeping hours, smoking habits, whether the participant eats breakfast or not, the time that the participant eats dinner, habits regarding the eating of post-dinner snacks, eating speed, and drinking habits.
Participants who had already received a diagnosis of hypertension and who were currently treated with antihypertensive medications and participants who had a systolic blood pressure (SBP) of ≥140 mmHg or a diastolic blood pressure (DBP) of ≥90 mmHg at the health checkup were defined as “hypertensive”. The other participants were defined as “non-hypertensive”. Among the 2,201 participants in the study population, 346 participants were hypertensive, and 1,855 were non-hypertensive. One hundred ninety-three of the 346 hypertensive participants received antihypertensive drugs (treated participants), and 153 received no medications (untreated participants). The participants who had already received a diagnosis of diabetes mellitus were defined as “diabetic”.
Results
The baseline characteristics and the questionnaire results (Salt Check Sheet)
The baseline characteristics, including gender, age, BMI, height, body weight, systolic blood pressure, diastolic blood pressure, serum creatinine, HbA1c, blood glucose, serum uric acid, BNP, estimated salt intake and salt check scores, of the hypertensive and non-hypertensive participants are summarized in Table 2.
Table 2.
Baseline Characteristics.
| Parameter | Hypertension | Non-hypertension | p value* | Overall |
|---|---|---|---|---|
| n=346 | n=1,855 | n=2,201 | ||
| Gender: rate of male (%) | 66.7 | |||
| Age | 51.95±7.65 | 42.25±9.64 | <.0001 | 43.78±10.00 |
| BMI (kg/m2) | 25.18±3.86 | 22.06±2.98 | <.0001 | 22.55±3.33 |
| Height (cm) | 168.51±7.33 | 167.17±8.11 | 0.0023 | 167.38±8.00 |
| Body weight (kg) | 71.59±12.07 | 61.91±10.80 | <.0001 | 63.43±11.56 |
| Systolic blood pressure (mmHg) | 134.65±15.88 | 112.68±11.02 | <.0001 | 116.13±14.35 |
| Diastolic blood pressure (mmHg) | 87.69±10.74 | 70.08±8.87 | <.0001 | 72.84±11.20 |
| Blood creatinine ( mg/dL) | 0.85±0.20 | 0.77±0.15 | <.0001 | 0.78±0.16 |
| HbA1c (%) | 5.50±0.70 | 5.19±0.42 | <.0001 | 5.24±0.49 |
| Blood glucose (mg/dL) | 99.16±19.18 | 88.62±12.66 | <.0001 | 90.27±14.40 |
| Serum uric acid (mg/dL) | 6.13±1.34 | 5.29±1.32 | <.0001 | 5.42±1.36 |
| BNP (pg/mL) | 11.67±16.50 | 11.14±9.91 | 0.5711 | 11.24±11.49 |
| Urine Na (mEq/L) | 139.42±47.01 | 144.65±51.33 | 0.0622 | 143.83±50.70 |
| Urine creatinine (mg/dL) | 154.23±70.74 | 171.01±83.78 | <.0001 | 168.37±82.08 |
| Estimated salt intake (g/day) | 8.96±2.00 | 8.44±2.01 | <.0001 | 8.52±2.02 |
| Sum of salt check scores | 13.96±4.34 | 13.45±4.00 | 0.0421 | 13.53±4.05 |
*Welch t-test
BMI: body mass index, HbA1c: Hemoglobin A1c, BNP: brain natriuretic peptide
The study population of 2,201 participants included 1,469 men and 732 women; 66.7% of the participants were men. The mean (±SD) age was 43.78±10.00 years. The age, BMI, height, body weight, systolic blood pressure, diastolic blood pressure, serum creatinine, HbA1c, blood glucose, serum uric acid, estimated salt intake and salt check scores of the hypertensive group were significantly higher in comparison to the non-hypertensive group. The mean salt check scores were 13.53±4.05, and the mean estimated daily salt intake was 8.52±2.02 g (Table 2). The histograms of both parameters showed a nearly normal distribution with the mean value at the center.
Regarding the impact of the 13 questionnaire items on the estimated daily salt intake, a multivariate linear regression model revealed strong correlations (in both the t value and p value) between the salt intake and scores on 5 items (“Pickled plums”, “Noodles”, “How often do you season food with sauce or soy sauce?”, “Do you drink the remaining soup from udon, ramen?”, and “Do you think you eat a lot?”). On the contrary, 3 items (“Japanese rice crackers/potato chips,” “Do you eat out for lunch or buy a lunch box at a convenience store?” and “Do you eat out or buy ready-made side dishes for dinner?”) were negatively correlated with the estimated daily salt intake (Table 3).
Table 3.
Questionnaire Results (Salt Check Sheet).
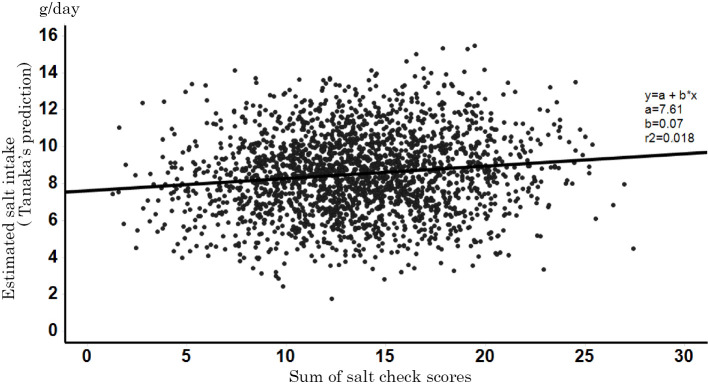
The correlation between the salt check scores and the estimated salt intake
A univariate linear regression model was fitted to the data with the estimated daily salt intake as the response variable and the sum of the salt check scores as the explanatory variable. The salt check scores were weakly correlated with the estimated daily salt intake. Figure 1 shows a scatter plot with the estimated daily salt intake on the vertical axis and the salt check scores on the horizontal axis. It also presents the regression equation and the contribution rate determined when fitting the univariate linear regression model with the estimated daily salt intake as the response variable and the salt check scores as the explanatory variable. The values of a=7.61, b=0.07, and r2=0.018 in the figure indicate y-intercept, regression coefficient, and contribution rate, respectively. The correlation coefficient (the square root of the contribution rate) was 0.13.
Figure 1.
A scatter plot showing the association between the estimated salt intake and the salt check scores. The estimated daily salt intake is shown on the vertical axis and the salt check scores are shown on the horizontal axis (n=2,201).
A one-way analysis of variance was performed to examine whether there were significant differences in the mean salt check scores and the mean daily salt intake among the subgroups defined by each baseline characteristic (Fig. 2). In the 4 subgroups defined by age (<30 years, 30-39 years, 40-49 years, and ≥50 years), the salt check scores did not change to a significant extent with an increase in age (p=0.3551), while the estimated salt intake significantly increased with increasing age (p≤0.0001). Men had significantly higher values than women for both the salt check score and the estimated salt intake (p≤0.0001). Hypertensive participants had significantly higher values than non-hypertensive participants for both the salt check score (p=0.0310) and the estimated salt intake (p≤0.0001). The subgroup of participants with high BMI values (≥25 kg/m2) had significantly higher values than the subgroup of participants with low BMI values (<25 kg/m2) for both the salt check score and the estimated salt intake (p≤0.0001). Participants with a high fasting blood glucose level (≥126 mg/dL) had significantly higher salt check scores (p=0.0095) than those with a glucose level (<126 mg/dL), while no significant difference was observed in their salt intake (p=0.4951). Participants with high HbA1c values (≥6.5 %) had significantly higher salt check scores (p=0.0495) than those with low HbA1c values (<6.5 %); however, no significant difference was found in the estimated salt intake (p=0.4870).
Figure 2.
A comparison of the salt intake and the salt check scores stratified by age (a), gender (b), hypertension (c), BMI (d), blood glucose (e), and HbA1c (f).
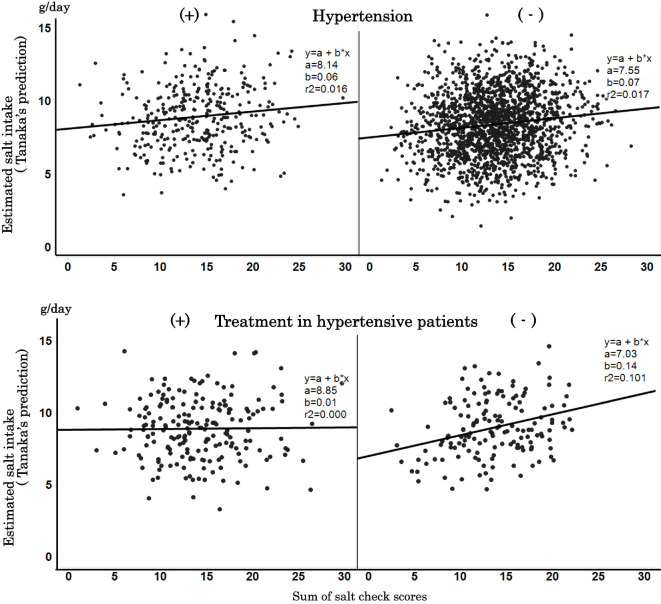
The salt check scores and the estimated salt hypertensive and non-hypertensive group
We analyzed the effect of the estimated salt intake on hypertension. Hypertensive participants had significantly higher values for both the salt check score and the estimated salt intake in comparison to non-hypertensive participants. As shown in Table 2, there were significant differences between the two groups in all of the baseline characteristics other than the BNP level. Although there was no significant difference between the hypertensive group and the non-hypertensive group in the degree of correlation between the two variables, the degree of correlation between the two variables in the untreated hypertensive participants was higher than that in the treated hypertensive participants, when the correlation among hypertensive participants was analyzed according to the use or non-use of antihypertensive medications (Fig. 3). Analyses stratified by age, gender, and blood pressure revealed similar tendencies in the correlation between the salt check scores and the estimated daily salt intake in all of those subgroups. On the other hand, the salt check score was not correlated with the estimated salt intake in the subgroups defined by BMI, blood glucose level, HbA1c level, or diabetes mellitus (Fig. 4).
Figure 3.
The relationship between the estimated salt intake and the salt check scores in (a) participants with or without hypertension and (b) hypertensive participants with or without treatment.
Figure 4.
The relationship between the estimated salt intake and the salt check scores stratified by age (a), gender (b), BMI (c), blood glucose (d), HbA1c (e), and the presence of diabetes (f).
Discussion
In the present study, we surveyed more than 2,000 participants about their salt intake-related lifestyle using the Salt Check Sheet, and demonstrated a loose correlation between the salt check score and the salt intake in both the overall population and in hypertensive participants. In addition, among the hypertensive participants, there was a clear difference in the degree of correlation between the treated participants and the untreated participants. Regarding the correlation between the salt check score and the daily salt intake in subgroups defined by baseline characteristics, the salt intake increased with increasing age; however, the salt check scores remained almost unchanged, suggesting that older people tend to eat more traditional Japanese foods that have a higher salt content. The two variables showed a higher degree of correlation in men than in women and among the sub-group of participants with higher BMI values. Similar trends were reported by previous study (4). The higher blood glucose level and higher HbA1c level subgroups showed higher salt check scores, but a similar daily salt intake in comparison to the normal blood glucose level and normal HbA1c level subgroups, suggesting that they might be careful about their intake of salty food.
Despite eating a sufficient amount of food, some of the participants with low BMI values might have suffered from poor nutrient absorption or excessive energy consumption. On the other hand, since diabetic participants might receive dietary instructions and might be more conscious about their salt intake, they might have overestimated their salt intake when answering the questionnaire.
Many reports have stated that excessive drinking is a risk factor for the development of hypertension (10). This may partly be explained by our observation that a higher frequency of alcohol consumption and a greater volume of alcohol consumption were correlated with a higher daily salt intake. On the other hand, although excessive smoking was a risk factor for hypertension, smoking habits were not correlated with the participants' daily salt intake (11).
In the present study, the mean daily salt intake, which was estimated from spot urine samples, was 8.52 g (men: 8.76 g, women: 8.04 g). Although these values were lower than those reported in the National Health and Nutrition Survey Japan (2015) by the MHLW (men: 11.1 g, women: 9.4 g), the MHLW “Dietary Reference Intakes for Japanese (2015),” proposed a target of 7-8 g/day or less, and the “Guidelines for the Management of Hypertension 2014” recommended an intake of 6 g/day or less. Furthermore, the WHO sets the target salt intake at 5 g/day or less (7). Thus, a more active, national salt reduction campaign may be necessary.
We demonstrated that hypertensive participants had a higher daily salt intake than non-hypertensive participants, and that the salt check scores showed that hypertensive participants had a higher daily salt intake-related lifestyle scores than their non-hypertensive participants. Among participants with hypertension, a higher degree of correlation between the two variables was found in the untreated hypertensive participants in comparison to participants who were treated with antihypertensive drugs. This suggested that treated participants took care of salt intake-related lifestyle. In addition, the urinary salt excretion was enhanced by the effects of various types of antihypertensive drugs, due to the effect of salt sensitivity on the participants' response to anti-hypertensive drugs (12,13).
In the present study, the estimated daily salt intake was weakly correlated with the total score on the Salt Check Sheet (correlation coefficient: 0.13, r2=0.018). We therefore analyzed the adequacy of each item in the questionnaire questions, and found that 5 of the 13 questions were positively correlated with the estimated daily salt intake, while three items were negatively correlated. The total score of the 5 positively correlated items showed a stronger correlation coefficient (0.21, r2=0.046) than the score of all 13 items (Fig. 5). These 5 positively correlated items seem to be objective parameters, while the other questions might not coincide with the contemporary dietary habits of the general working-age population. However, it should be noted that all 13 questions are reported to be correlated with hypertension, and that if only 5 items were investigated, it might be difficult to utilize hypertension patients in providing general dietary guidance.
Figure 5.
The estimated salt intake and the sum of the salt check scores (5 items). The 5 items are “Pickled plums”, “Noodles”, “How often do you season food with sauce or soy sauce?”, “Do you drink the remaining soup from udon, ramen?”, and “Do you think you eat a lot?”
The present study is associated with several limitations. First, statistically significant regression coefficients were likely yielded by fitting univariate and multivariate linear regression models, since this study had a relatively large population (n=2,201). Thus, we consider it necessary to take clinical implications into account when interpreting the results. Second, the finding that the mean salt intake of 8.52 g among participants in this research was lower than the mean salt intake of 10.0 g in the MHLW National Health and Nutrition Survey Japan (2015), might be attributable to the fact that the participants were employees of a pharmaceutical company that was engaged in health promotion. Third, we analyzed the significance of the correlation between the daily salt intake and each item score by fitting a multivariate linear regression model with the estimated daily salt intake as the response variable and the scores of each of the 13 items of the questionnaire as the explanatory variable. Unexpectedly, negative correlations were observed for 3 items, probably because the frequency of eating traditional Japanese foods is decreasing as a result of a westernized diet and lifestyle changes (14,15).
In conclusion, a weak correlation was found between the total score on the Salt Check Sheet and the salt intake. Five of the questions were more strongly correlated with the salt intake.
Author's disclosure of potential Conflicts of Interest (COI).
Yoshitaka Isaka: Employment, Shionogi & Co., Ltd., Toshiki Moriyama: Employment, Shionogi & Co., Ltd., Kiyomi Kanda: Employment, Shionogi & Co., Ltd.
Acknowledgement
We would like to express our sincere thanks to: Dr. Takuya Tsuchihashi, who kindly allowed us to utilize the Salt Check Sheet and gave us valuable comments that helped with this research; the employees of Shionogi & Co., Ltd. who gave their consent to participate and kindly cooperated with us in this study; and the Biostatistics Department of Shionogi & Co., Ltd. which cooperated in the data analysis. The Biostatistics Department, Shionogi & Co., Ltd. cooperated in the data analysis, while the employees of Shionogi & Co., Ltd., who received a periodic health checkup, took part in this study. The costs associated with the urinalysis and other analyses were borne by Shionogi & Co., Ltd.
References
- 1.Ando K, Kawarazaki H, Miura K. [Scientific statement] Report of the salt Reduction Committee of the Japanese Society of Hypertension (1) Role of salt in hypertension and cardiovascular diseases. Hypertens Res 36: 1009-1019, 2013. [DOI] [PubMed] [Google Scholar]
- 2.Kawano Y, Ando K, Matsuura H, Tsuchihashi T, Fujita T, Ueshima H. Report of the Working Group for Dietary Salt Reduction of the Japanese Society of Hypertension: (1) Rationale for salt restriction and salt-restriction target level for the management of hypertension. Hypertens Res 30: 879-886, 2007. [DOI] [PubMed] [Google Scholar]
- 3.Toda A, Ishizaka Y, Tani M, Yamakado M. Current dietary salt intake of Japanese individuals assessed during health check-up. Hypertens Res 38: 163-168, 2015. [DOI] [PubMed] [Google Scholar]
- 4.Miura K, Ando K, Tsuchihashi T, et al. . Scientific statement; Report of the salt reduction committee of Japanese Society of Hypertension (2) Goal and strategies of dietary salt reduction in management of hypertension. Hypertens Res 36: 1020-1025, 2013. [DOI] [PubMed] [Google Scholar]
- 5.Nagata C, Takatsuka N, Shimizu N, et al. . Sodum intake and risk of death from stroke in Japanese men and women. Stroke 35: 1543-1547, 2004. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization (WHO) Guideline: Sodium intake for adults and children. WHO, 2012. [PubMed] [Google Scholar]
- 7.Department of Health Care. Ministry of Health and Welfare of Japan. Overview of Dietary Reference Intakes for Japanese [Internet]. 2015 [cited 2016 Jul 19] Available from: http://www.mhlw.go.jp/file/06-Seisakujouhou-10900000-Kenkoukyoku/Overview.pdf page 30 DRIs for Sodium.
- 8.Yasutake K, Miyoshi E, Kajiyama T. Comparison of a salt check sheet with 24-h urinary salt excretion measurement in local residents. Hypertens Res 39: 879-885, 2016. [DOI] [PubMed] [Google Scholar]
- 9.Tanaka T, Okamura T, Miura K, et al. . A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens 16: 97-103, 2002. [DOI] [PubMed] [Google Scholar]
- 10.Nakamura K, Okamura T, Hayakawa T, et al. . The proportion of individuals with alcohol-induced hypertension among total hypertensives in a general japanese population: NIPPON DATA90. Hypertens Res 30: 663-668, 2007. [DOI] [PubMed] [Google Scholar]
- 11.Halperin RO, Gaziano JM, Sesso HD. Smoking and the risk of incident hypertension in middle-aged and older men. Am J Hypertens 21: 148-152, 2008. [DOI] [PubMed] [Google Scholar]
- 12.Saito F, Kimura G. Antihypertensive mechanism of diuretics based on pressure-natriuresis relationship. Hypertension 27: 914-918, 1996. [DOI] [PubMed] [Google Scholar]
- 13.Weir MR, Reisin E, Falkner B, Hutchinson HG, Sha L, Tuck ML. Nocturnal reduction of blood pressure and the antihypertensive response to a diuretic or angiotensin converting enzyme inhibitor in obese hypertensive patients. TROPHY Study Group. Am J Hypertens 11: 914-920, 1998. [DOI] [PubMed] [Google Scholar]
- 14.Ogawa K, Tsubono Y, Nishino Y, et al. . Dietary souruces of nutrient comsumption in a rural Japanese population. J Epidemiol 12: 1-8, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wakasugi M, Kazama JJ, Narita I. Associations between the intake of Miso soup and Japanese pickles and the estimated 24-hour urinary sodium excretion: A population-based cross-sectional study. Intern Med 54: 903-910, 2015. [DOI] [PubMed] [Google Scholar]