Abstract
Ataxic hemiparesis (AH) is a classic lacunar syndrome associated with localized damage to the pons, internal capsule, thalamus, or corona radiata. A depression of metabolic activity known as crossed cerebellar diaschisis (CCD) is frequently observed in the cerebellar hemisphere contralateral to the site of the lesion in patients with AH. Though small cortical or subcortical lesions may result in AH, such occurrences are rare. The current report details the case of a patient with AH resulting from acute infarction associated with localized lesions of the postcentral gyrus who presented without CCD.
Keywords: ataxic hemiparesis, crossed cerebellar diaschisis, ischemic stroke
Introduction
Ataxic hemiparesis (AH), which is characterized by both ipsilateral ataxia and paresis, was first described by Fisher in 1965. A 1978 revision expanded the definition of AH to include any combination of weakness and disproportionate incoordination presenting on the same side of the body (1,2). Lesions resulting in AH have been most commonly reported in the pons, internal capsule, thalamus, and corona radiata. Patients with AH often experience a metabolic depression of contralateral cerebellar activity known as crossed cerebellar diaschisis (CCD), the effects of which may be visualized using single photon emission computed tomography (SPECT) (3,4). CCD is thought to result from damage to the corticopontocerebellar and/or dentatorubral-thalamocortical pathways in patients with AH. While lesions in the cerebral cortex may also be implicated in the pathogenesis of AH, such occurrences are rare, and the details regarding the role of cortical damage in producing symptoms of AH as well as its association with CCD remain to be elucidated (5). The current report details a case of AH resulting from acute infarction associated with localized lesions of the postcentral gyrus in a patient without CCD.
Case Report
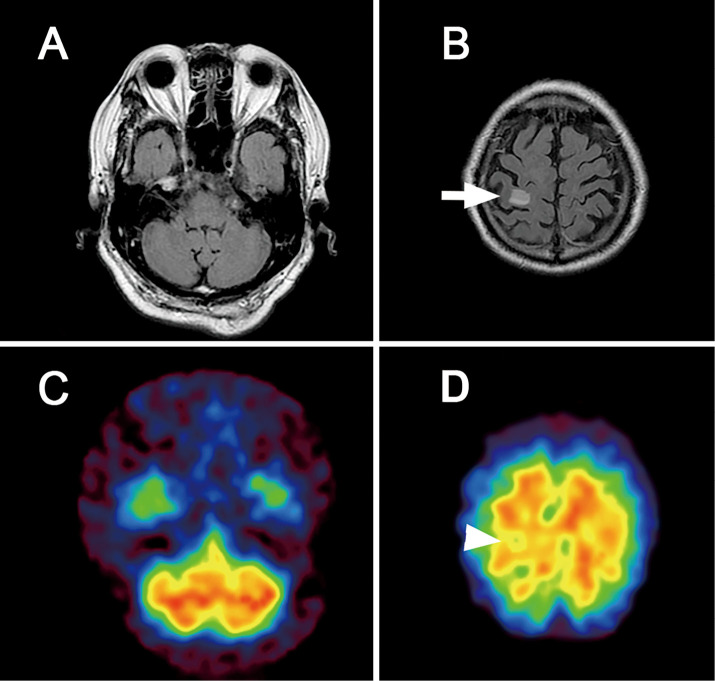
An 82-year-old right-handed man with a history of atrial fibrillation was admitted to our stroke center due to the sudden onset of left arm weakness and clumsiness. Upon admission, his blood pressure was 144/79 mmHg and his heart rate was 77 beats/min, with an irregular rhythm. He was alert and had very mild left hemiparesis accompanied by left-sided dysmetria and intention tremor. His deep sensation was substantially well preserved. Brain MRI revealed an acute infarct in the right postcentral gyrus and the absence of abnormalities in the brainstem and cerebellum (Figure A and B). Brain N-isopropyl-p-[123I]iodoamphetamine (123I-IMP) SPECT images obtained 5 days after the onset of symptoms revealed a slight decrease in the cerebral blood flow around the postcentral gyrus, though the perfusion of the cerebellar hemisphere was normal (Figure C and D). The patient was diagnosed with cardioembolic stroke and received anticoagulant therapy for secondary prevention. Although there was no remarkable change in the brain MRI findings during hospitalization, the patient's left-sided weakness and ataxia began to improve 8 days after the onset of symptoms, and marked improvement was observed at the time of discharge (16 days after the onset of symptoms).
Figure.
(A, B) Brain fluid attenuated inversion recovery (FLAIR) and single photon emission computed tomography (SPECT) images from a patient with ataxic hemiparesis. FLAIR imaging revealed no abnormalities in the cerebellum or brainstem that were associated with the lesions of the postcentral gyrus (white arrow). (C, D) Brain SPECT revealed a slight decrease in the cerebral blood flow around the postcentral gyrus (white arrowheads); however, no signs of crossed cerebellar diaschisis were observed.
Discussion
The present report details the case of an 82-year-old man with AH associated with a cortical infarct localized to the postcentral gyrus. Although some reports suggest that lesions of the precentral gyrus and frontal white matter can produce AH (5,6), AH associated with cortical infarction (rather than deep infarction) is rare. To our knowledge, the present report is the first to discuss AH associated with localized lesions of the postcentral gyrus. Research has suggested that ataxia occurs due to the dysfunctional involvement of the pons, internal capsule, thalamus, and corona radiata in the corticopontocerebellar and dentatorubral-thalamocortical pathways. The results of previous experimental studies have indicated that the cerebellar hemispheres receive strong connections from the somatosensory areas via the pontine nuclei (7). Moreover, one clinical electrophysiological report further revealed that lesions of the parietal lobe with minimal precentral involvement may result in the development of AH, and that such postcentral infarcts are capable of influencing the cerebellar afferent system (8). When taken with the results of previous investigations, the present case provides evidence that postcentral lesions may result in ataxia due to the disruption of the cerebellar afferent system. As researchers have observed that edema within the region of the postcentral infarct results in mild hemiparesis, the resolution of edema in the present case may have led to the marked improvement of the patient's hemiparesis. In a SPECT analysis of 55 patients who experienced unilateral ischemic stroke, Pantano et al. hypothesized that CCD results from the deafferentation of the affected cerebellar hemisphere, due to the contralateral interruption of the corticopontocerebellar or dentatorubral-thalamocortical fibers (9). One study further reported that three patients with AH due to small frontal subcortical infarcts also exhibited CCD and that the degree of CCD may provide useful information regarding an individual's potential for recovery. However, another recent study demonstrated that two patients with precentral infarcts exhibited no signs of CCD (5). Taken together, these findings and the presentation of the current case suggest that CCD is not always required for the development of AH following cortical infarct. Further studies should more closely examine patient symptoms in addition to the MRI/SPECT findings in order to clarify the pathogenesis of AH associated with cortical infarction.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Fisher CM. Ataxic hemiparesis. A pathologic study. Arch Neurol 35: 126-128, 1978. [DOI] [PubMed] [Google Scholar]
- 2.Fisher CM, Cole M. Homolateral ataxia and crural paresis: a vascular syndrome. J Neurol Neurosurg Psychiatry 28: 48-55, 1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moulin T, Bogousslavsky J, Chopard JL, et al. Vascular ataxic hemiparesis; a reevaluation. J Neurol Neurosurg Psychiatry 58: 422-427, 1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schonewille WJ, Tuhrim S, Singer MB, et al. Diffusion-weighted MRI in acute lacunar syndromes. A clinical-radiological correlation study. Stroke 30: 2066-2069, 1999. [DOI] [PubMed] [Google Scholar]
- 5.Hiraga A, Uzawa A, Kamitsukasa I. Diffusion weighted imaging in ataxic hemiparesis. J Neurol Neurosurg Psychiatry 78: 1260-1262, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Flint AC, Naley MC, Wright CB. Ataxic hemiparesis from strategic frontal white matter infarction with crossed cerebellar diaschisis. Stroke 37: e1-e2, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brodal P, Bjaalie JG. Salient anatomic features of the cortico-pontocerebellar pathway. Prog Brain Res 114: 227-249, 1997. [DOI] [PubMed] [Google Scholar]
- 8.Nighoghossian N, Trouillas P, Mauguière F. Ataxic monoparesis of the upper limb and suspension of the tonus caused by parietal lesion. Rev Neurol 149: 262-266, 1993. [PubMed] [Google Scholar]
- 9.Pantano P, Baron JC, Samson Y, et al. Crossed cerebellar diaschisis: further studies. Brain 109: 677-694, 1986. [DOI] [PubMed] [Google Scholar]