Abstract
Background
A large body of research has focused on identifying the optimal number of dimensions—or spectra—to model individual differences in psychopathology. Recently, it has become increasingly clear that ostensibly competing models with varying numbers of spectra can be synthesized in empirically derived hierarchical structures.
Methods and Materials
We examined the convergence between top-down (bass-ackwards or sequential principal components analysis) and bottom-up (hierarchical agglomerative cluster analysis) statistical methods for elucidating hierarchies to explicate the joint hierarchical structure of clinical and personality disorders. Analyses examined 24 clinical and personality disorders based on semi-structured clinical interviews in an outpatient psychiatric sample (n = 2900).
Results
The two methods of hierarchical analysis converged on a three-tier joint hierarchy of psychopathology. At the lowest tier, there were seven spectra—disinhibition, antagonism, core thought disorder, detachment, core internalizing, somatoform, and compulsivity—that emerged in both methods. These spectra were nested under the same three higher-order superspectra in both methods: externalizing, broad thought dysfunction, and broad internalizing. In turn, these three superspectra were nested under a single general psychopathology spectrum, which represented the top tier of the hierarchical structure.
Conclusions
The hierarchical structure mirrors and extends upon past research, with the inclusion of a novel compulsivity spectrum, and the finding that psychopathology is organized in three superordinate domains. This hierarchy can thus be used as a flexible and integrative framework to facilitate psychopathology research with varying levels of specificity (i.e., focusing on the optimal level of detailed information, rather than the optimal number of factors).
Keywords: Hierarchical taxonomy of psychopathology, clinical disorders, personality disorders, bass-ackwards analysis, hierarchical agglomerative cluster analysis
Categorical models of psychopathology have been challenged by dimensional models in recent years, given the lack of discrete boundaries among clinical and personality disorders [1]. The overlap among diagnoses in the Diagnostic and Statistical Manual of Mental Disorders [DSM; 2]—particularly their systematic patterns of co-occurrence—highlights the presence of shared underlying spectra of psychopathology that cut across traditional diagnostic boundaries and offer an empirical framework for research and clinical practice that addresses the shortcomings of the DSM [3, 4]. Large bodies of research have consequently focused on identifying the optimal number of spectra to summarize the dimensional structure of pathological personality traits and common clinical disorders.
1.1 The Dimensional Structure of Personality
Studies on dimensional models of pathological personality traits (e.g., personality disorders from the DSM) tend to converge at the five-factor level. The consistent dimensional factors include internalizing or negative affectivity—characterized by feeling anxious, depressed, or despondent; detachment or introversion—characterized by inhibition or social withdrawal; psychoticism—characterized by cognitive-perceptual aberrations; and externalizing, which is split into a combination of antagonistic (e.g., aggressive and antisocial traits) and disinhibited (e.g., impulsive and irresponsible traits) components [5–8]. These five factors also reflect the dimensional classification system of personality disorders in Section III of the DSM-5 [2, 9, 10].
1.2 The Dimensional Structure of Clinical Disorders
Similarly, structural models of common clinical disorders have consistently converged on three core dimensional spectra: (1) internalizing, characterized by depressive and anxiety disorders; (2) externalizing, characterized by substance use and antisocial behavior; and (3) thought disorder, characterized by cognitive aberrations [e.g., psychosis and mania; 11, 12, 13]. The internalizing spectrum often bifurcates into fear and distress spectra, distinguishing between phobic anxiety versus depression and generalized anxiety [14]; with the inclusion of more varied disorder indicators, nested spectra of eating pathology and low sexual function also emerge as part of the internalizing spectrum [4]. Symptom-level analyses of the externalizing spectrum also have shown distinct nested spectra of disinhibition, aggression, and substance use [15].
1.3 The Joint Structure of Clinical and Personality Disorders
Although most research to date has focused on the dimensional structure of either clinical or personality disorders, there are clear parallels in their underlying dimensions. This is consistent with the finding that personality traits act as stable orienting dispositions that confer risk for psychopathology [16]. During the development of the DSM-5, these similarities led to the proposal that personality could be used to elucidate the underlying phenotypic structure of psychopathology [e.g., 5, 8]. Six studies to date have examined the joint structure of clinical and personality disorders, generally converging on replicable domains: An internalizing spectrum consistently emerges [17–22], often alongside a detachment or pathological introversion domain [17, 19–21]; an externalizing spectrum consistently emerges [17, 19, 22], sometimes split into disinhibition and antagonism components [18, 20, 21]; and a thought disorder spectrum also emerges when there are sufficient indicators and variability in the sample [18, 19, 21]. Kotov and colleagues [18] also found evidence for a somatoform spectrum; in contrast, however, Markon [19] found somatoform indicators to be nested under the internalizing spectrum. Other studies on the joint structure of clinical and personality disorders have not included sufficient indicators to identify a somatoform factor [17, 20–22], but analyses of omnibus measures of self-reported psychopathology have found evidence for a distinct somatoform factor [23, 24].
1.4 Hierarchical Models as Integrative Frameworks
Studies of dimensional structure have largely focused on identifying the optimal number of shared underlying factors to model variation in psychopathological experiences [25, 26]. However, it has become increasingly clear that ostensibly competing models of individual differences can be synthesized into a multilevel hierarchical structure. For example, recent personality research has converged on a hierarchy that integrates longstanding 2-, 3-, 4-, and 5-factor accounts of the structure of personality and temperament domains [5–8, 27–29]. Similarly, analyses of clinical disorders have found an interpretable hierarchy that includes the three core dimensional spectra, their narrower nested components, and a higher-order general factor. This higher-order factor represents a general propensity towards psychopathology, and is hypothesized to account for shared, nonspecific etiologic mechanisms that span multiple dimensions of psychopathology [30–32]. Hierarchical models of these dimensional factors of clinical disorders have been found to maintain reliability and validity, with each level differentially predicting important outcomes such as psychosocial functioning, and disorder onset and maintenance [33, 34].
Given the similarities between the dimensional factors that underlie clinical and personality disorders, it is likely these currently disparate fields of research could be unified in a joint hierarchical model. One study to date has examined factors that emerge using maladaptive personality as a scaffold for the hierarchical structure of psychopathology: Wright and Simms [21] analyzed 35 indicators of maladaptive personality alongside 10 indicators of psychopathology, and their results strongly mirrored the hierarchical structure of personality, as expected. At the third tier of the hierarchy, internalizing, externalizing, and detachment emerged, which Wright and Simms noted mirror the “big three” of personality and temperament [e.g., 35]; at the fourth tier, a thought disorder domain emerged, accounting for the “big three” of psychopathology research [e.g., 11]; and at the fifth level, the disinhibition and antagonism domains split, converging on the DSM-5 dimensional model of personality pathology [2, 9, 10]. Lower levels of the hierarchy were characterized by the addition of unitary personality factors, including histrionism and suspiciousness.
Wright and Simms [21] explicated the five factor model, but did not depict the hierarchy (i.e., how each level was connected to the next). As such, it is not clear to what extent these sequential factors would represent hierarchical components in a structural model, or even whether these factors would form a hierarchy at all. For example, it is likely that the disinhibition and antagonism components represent narrower components of externalizing [cf. 18, 20, 21], but the other five domains that emerged in the sequential factor analysis may represent substantively distinct domains, rather than nested hierarchical factors [36]. We need to determine whether and where the spectra of psychopathology form a hierarchical structure in order to integrate the disparate literatures on clinical and personality disorders. The resultant model would offer a flexible and empirically derived framework to facilitate psychopathology research with varying levels of specificity—allowing researchers to select spectra with the optimal level of detail for their research question. Further, a joint hierarchy—based on robust representation of both clinical and personality disorders—could clarify the nature and boundaries of the shared underlying dimensions of psychopathology. Such a model may also pave the way toward more replicable and accurate etiologic research [21, 32].
1.5 The Present Study
The aim of the present study, therefore, was to explicate the joint hierarchical structure of psychopathology. We analyzed the systematic patterns of covariance among 24 indicators of clinical and personality disorders from the DSM to elucidate the spectra of psychopathology identified in the present sample [37]. The hierarchical structure of the spectra was delineated using two statistical methods: (1) Goldberg’s [38] bass-ackwards method, which sequentially extracts principal components from the top-down1. In this method, a single component is extracted at the first and highest level of the hierarchy; two uncorrelated (i.e., orthogonal) factors are extracted at the second level, and so on. This method extracts maximally distinct components at each level of the hierarchy [39] and maps the disorder indicators in a multidimensional space (i.e., all indicators load on all components at each level of the hierarchy). (2) Hierarchical agglomerative cluster analysis was used as a bottom-up analysis of the hierarchy. This method sorts disorder indicators into distinct sets based on their dissimilarity from one another, mapping their agglomeration into progressively larger mutually exclusive clusters in a tree-like structure [40]. The latter method has been used in three studies on the structure of psychopathology as a complement to exploratory factor analysis to examine convergence in the nature and number of clusters and factors that emerge [19, 41, 42]. However, it is also an ideal complement to the bass-ackwards method for delineating hierarchical models because both methods allow each level of the hierarchy to retain all the variance in the systematic patterns of covariation among the disorder indicators 2. The methods also have complementary strengths and weaknesses. For example, hierarchical cluster analysis is a robust method for delineating the hierarchical structure among highly correlated variables [40], but it may be more prone to illusory hierarchies than principal components analysis [43]. If these methods converge on a joint hierarchy that is systematic and reliable, this hierarchy could be used as an integrative framework to guide future research.
Methods and Materials
2.1 Participants, Procedure, and Measures
The methods for data collection in the present study were described in Kotov et al. [18], which previously reported a confirmatory factor analysis of these data focused on a 5-factor solution. Briefly, the participants for this study were the first 2,900 consecutive patients from the outpatient practice of Rhode Island Hospital’s Department of Psychiatry, who had enrolled in the Methods to Improve Diagnostic and Assessment Services project [44, 45]. Axis II diagnoses were measured with the Structured Interview for DSM-IV Personality [46], and subthreshold cases with one criterion less than DSM-IV thresholds were included to ensure a sufficient number of cases for analysis of each disorder. Prevalence using these criteria ranged from 1.3% for schizotypal personality to 18.3% for avoidant personality. Lifetime Axis I diagnoses—for consistency with the timeframe of personality disorder assessment—were made using the Structured Clinical Interview for DSM-IV [47]. Diagnoses affected by hierarchical rules could not be analyzed because hierarchical rules prohibit certain combinations of diagnoses, which would confound our analyses based on the patterns of covariation among the disorders. Therefore, we used a non-hierarchical generalized anxiety disorder diagnosis and examined mood episodes (major depressive and manic) rather than mood disorders, as these diagnoses include exclusion rules. Psychosis—defined as the presence of definite psychotic symptoms—was analyzed as a single category (overall prevalence of 8.1%) that included diagnoses of schizophrenia (0.5%), schizophreniform disorder (0.1%), schizoaffective disorder (0.6%), delusional disorder (0.2%), brief psychotic disorder (0.2%), psychosis not otherwise specified (1.0%), major depressive disorder with psychosis (1–1.9%), and bipolar I with psychosis (0.5%), as well as psychotic symptoms from Module B. Exclusion rules precluded the analysis of the disorders separately. For the same reason, a broad eating disorder group (combined prevalence of 7.7%) was used that consisted of anorexia nervosa (1.5%), bulimia nervosa (2.6%), and binge eating disorder (3.9%). Also, the undifferentiated somatoform disorder group (combined prevalence of 3.3%) included cases with somatization disorder (0.7%), which represents an extreme form of this condition. Not otherwise specified (NOS) diagnoses were not counted in any of the categories other than psychosis. Overall, Axis I diagnoses ranged in prevalence from 1.2% for hypochondriasis to 72.4% for major depressive episode [see 18 for more detailed information on the sample].
In contrast with Kotov et al. [18], we included only adult psychopathology (i.e., we excluded conduct disorder). We also combined social phobia with avoidant personality disorder to account for their collinearity (r = .81, p < .0005; combined prevalence of 32.9%), which is consistent with the literature arguing that avoidant PD is an extreme form of social phobia [e.g., 48]. These were the only very strongly correlated variables; the next most closely related pairs were alcohol and substance use disorders (r = .64, p < .0005). In total, 24 dichotomous diagnostic indicators were included in the analyses.
2.2 Data Analysis
All analyses were conducted in the R environment [49] using the stats [49] and psych packages [50]. Both sets of analyses were computed based on the tetrachoric correlation matrix (i.e., the bivariate relationships among binary variables), which was smoothed in the psych package by scaling selected off-diagonal rows and columns to achieve a positive definite matrix [51]. We used this correlation matrix as the basis of the top-down and bottom-up analyses so that the results were directly comparable (i.e., derived from the same information).
2.2.1 Top-Down Analysis
Bass-ackwards analyses [38] were conducted based on varimax-rotated (orthogonal) principal components analysis, starting with the first unrotated principal component, and iteratively adding a component at each level of the model. In the bass-ackwards model, the paths between levels depict correlations ≥ .3 between the component scores. Loehlin and Goldberg [36] suggested that a higher-order component correlating ≤ .9 but ≥ .3 with emergent lower-order components is an indication of hierarchical structure—i.e., the emergence of nested components, rather than the perpetuation of factors that are substantively distinct from one another throughout levels of the model, which is indicated by higher-order components correlating > .9 with lower-order components. We extended this method across all levels of the bass-ackwards hierarchy to summarize the emergence of the hierarchical structure into a more parsimonious tier-based model 3.
Standard criteria for determining the number of components and clusters to extract had little convergence, providing preliminary evidence that a hierarchical model (i.e., with a varying number of factors at each level) is appropriate. Parallel analysis suggested a model with up to eight components; Velicer’s minimum average partial test suggested a model with two components; and the very simple structure criterion suggested one component for a complexity of one (i.e., indicators can only have one non-zero loading at each level of the hierarchy, as is the case in cluster analysis), seven components for a complexity of two (i.e., indicators can have two non-zero loadings), and eight components for complexity of three or four. We therefore examined a bass-ackwards model with one to eight components. At each level, diagnoses were assigned to components based on the highest component loading, and substantial cross-loadings are noted in the results. The model had a consistent and stable structure from one to seven components, but the eighth component did not have a clear substantive interpretation (i.e., indicated only by eating disorders and dependent personality disorder). We therefore interpret only the first seven levels of the model below.
2.2.2 Bottom-Up Analysis
Hierarchical agglomerative cluster analysis using Ward’s [52] method was conducted based on a distance matrix, which summarized the dissimilarity among the indicators as 1-|r|, where r is the tetrachoric correlation coefficient. The cluster analysis dendrogram was interpreted using cutree from the stats package in R, which cuts the dendrogram horizontally into a specified number of clusters. The cluster analysis results were compared to each level of the bass-ackwards model in terms of the emergence of components and clusters in the hierarchical structures, and the disorder-to-component and disorder-to-cluster assignment. Since clusters are mutually exclusive, disorders are automatically assigned to a single cluster.
Results
3.1 Top-Down Analysis
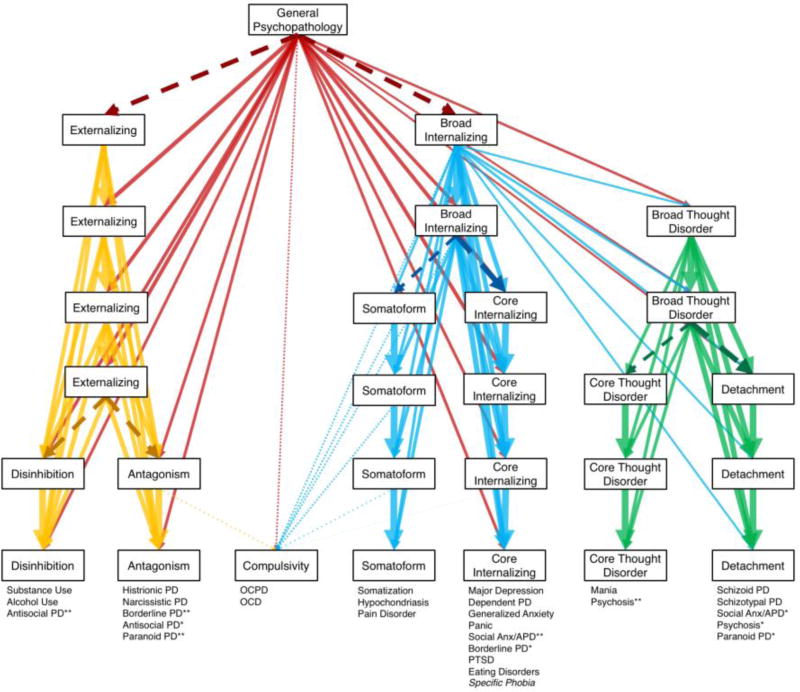
The hierarchical results from the bass-ackwards analysis are summarized in Figure 1; the disorder-to-component assignment at each level of the hierarchy is shown in the animation in Figure 2. All indicators except somatization, pain, and hypochondriasis had substantial loadings (> .3) on the first unrotated principal component, representing a general psychopathology spectrum at the top tier of the hierarchy. At the second level, the general psychopathology component split: An externalizing component emerged—characterized by Cluster B personality disorders—alongside a broad internalizing component—characterized by core internalizing (e.g., depressive and anxiety) and somatoform disorders. A broad thought disorder component characterized by Cluster A personality disorders and psychosis also emerged at the third level, correlating most strongly with the general psychopathology component. These three components appear to form the second tier of the hierarchy.
Figure 1.
Bass-ackwards model elucidating the emerging hierarchical factors. All correlations ≥ .3 are shown except where components persist through multiple levels (e.g., correlations between externalizing on level two and level four are not shown). This format explicates the hierarchical structure of the analyses by depicting whether and to what extent lower-order and higher-order components are related across all levels of the structure. Line weights represent the strength of the correlations. Darker dashed lines represent the bifurcation of a component, based on correlations with emerging components ≥ .3 and ≤ .9. Dotted lines represent the loadings for compulsivity; none of the loadings for compulsivity were ≥ .3, so loadings ≥ .2 for levels one through five are shown, and ≥ .1 for level six, as these were the thresholds to display even the strongest loadings at those levels. Disorders are listed under the components on which they loaded ≥ .4, sorted by the strength of their loading at the seven-component level (strongest to weakest). Specific phobia is italicized because its primary loading was < .4.
*denotes disorders that loaded ≥ .4 on more than one component.
**denotes the component on which cross-loading disorders loaded most strongly.
Note. OCPD = obsessive-compulsive personality disorder, OCD = obsessive-compulsive disorder, PD = personality disorder, Social Anx/APD = social anxiety and/or avoidant personality disorder, PTSD = posttraumatic stress disorder. PD variables include subthreshold cases with one criterion less than DSM-IV thresholds.
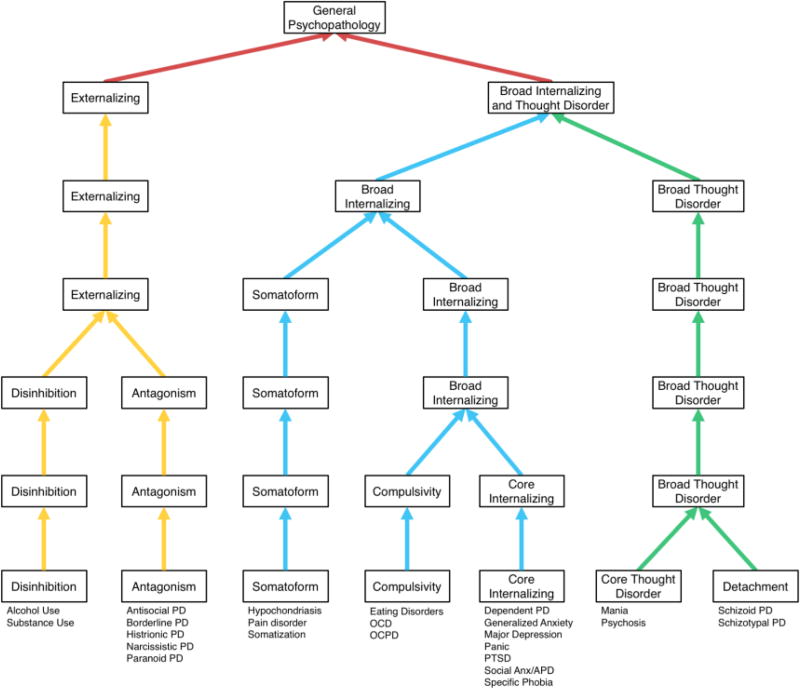
Figure 2.
Cluster-analytic hierarchy based on the agglomeration of clusters from the bottom-up. Disorders are listed alphabetically under the cluster they identified.
Note. OCPD = obsessive-compulsive personality disorder, OCD = obsessive-compulsive disorder, PD = personality disorder, Social Anx/APD = social anxiety and/or avoidant personality disorder, PTSD = posttraumatic stress disorder. PD variables include subthreshold cases with one criterion less than DSM-IV thresholds.
At the fourth level, broad internalizing bifurcated into somatoform and core internalizing components. At the fifth level, broad thought disorder bifurcated into core thought disorder (i.e., mania and psychosis) and detachment components. At the sixth level, externalizing bifurcated into disinhibition and antagonism. These six components thus belong to a third tier of the hierarchy, representing factors nested under the second tier.
Finally, a compulsivity component emerged at the seventh level (see Table 1 for all components loadings at this level). The compulsivity component correlated only weakly (r < .3) with other components in the model, and had similar relationships across levels one to five with the general psychopathology (r = .24, p < .0005), broad internalizing (r = .24–.25, p < .0005), and somatoform (r = .23–.24, p < .0005) components. It had only weak relationships with the level six antagonism (r = .19, p < .0005), somatoform (r = .18, p < .0005), and core internalizing (r = .13, p < .0005) components. To better understand the position of the compulsivity component in a hierarchical model, we turn to the hierarchical clustering results.
Table 1.
Component Loadings for the Disorder Indicators at the Seventh Level of the Bass-Ackwards Analyses
| Components
|
|||||||
|---|---|---|---|---|---|---|---|
| Disorder | Disinhibition | Antagonism | Compulsivity | Somatoform | Core Internalizing |
Core Thought Disorder |
Detachment |
| Substance Use | .86 | .11 | .10 | −.05 | .08 | .09 | .00 |
| Alcohol Use | .82 | .13 | .05 | −.03 | .04 | .04 | .03 |
| Antisocial PD | .59 | .54 | −.06 | −.03 | .07 | .05 | .16 |
| Histrionic PD | .14 | .86 | −.04 | −.11 | .15 | .15 | −.09 |
| Narcissistic PD | .17 | .80 | .34 | .09 | −.11 | −.07 | .09 |
| Borderline PD | .25 | .59 | .07 | .11 | .50 | .12 | .28 |
| Paranoid PD | .22 | .42 | .29 | .34 | .21 | .15 | .41 |
| OCPD | .14 | .13 | .83 | .14 | .09 | .08 | .14 |
| OCD | −.10 | .16 | .42 | .03 | .31 | .30 | .14 |
| Somatization | −.03 | −.04 | .20 | .77 | .04 | −.02 | .00 |
| Hypochondriasis | .05 | −.15 | .07 | .69 | .18 | .00 | .03 |
| Pain Disorder | −.14 | .29 | −.11 | .67 | −.02 | .00 | .03 |
| Major Depressive Episode | .01 | .11 | .16 | .00 | .67 | .15 | −.09 |
| Dependent PD | .09 | .14 | −.05 | −.19 | .66 | −.18 | .33 |
| Generalized Anxiety | .10 | −.01 | .37 | .10 | .61 | −.18 | .00 |
| Panic | .05 | −.04 | −.07 | .28 | .55 | .21 | −.02 |
| Social Anx/APD | .10 | −.10 | .15 | .10 | .51 | −.11 | .50 |
| PTSD | .28 | −.06 | −.08 | .21 | .48 | .39 | .08 |
| Eating Disorders | −.16 | .33 | .17 | −.01 | .42 | .21 | .00 |
| Specific Phobia | −.04 | .19 | −.11 | .20 | .36 | .04 | .31 |
| Mania | .10 | .12 | .16 | −.15 | .13 | .86 | −.06 |
| Psychosis | .08 | .06 | .00 | .16 | −.04 | .73 | .47 |
| Schizoid PD | −.09 | −.07 | .21 | −.04 | −.03 | .00 | .85 |
| Schizotypal PD | .19 | .24 | −.04 | .01 | .10 | .32 | .77 |
Note. Loadings are sorted by size within components, and loadings ≥ |.4| are bolded.
PD = personality disorder, OCPD = obsessive-compulsive personality disorder, OCD = obsessive-compulsive disorder, Social Anx/APD = social anxiety and/or avoidant personality disorder, PTSD = posttraumatic stress disorder. PD variables include subthreshold cases with one criterion less than DSM-IV thresholds.
3.2 Bottom-Up Analysis
The emergence of clusters is shown in the animation in Figure 2, and summarized in the static Figure 3. Notably, the same seven components emerged and were identified by the same indicators in 22 of 24 (91.7%) cases. The hierarchies themselves are also highly similar: Externalizing bifurcated into antagonism and disinhibition, the broad thought disorder cluster bifurcated into core thought disorder and detachment clusters, and the somatoform and core internalizing clusters emerged from the larger broad internalizing cluster, mirroring the bass-ackwards results.
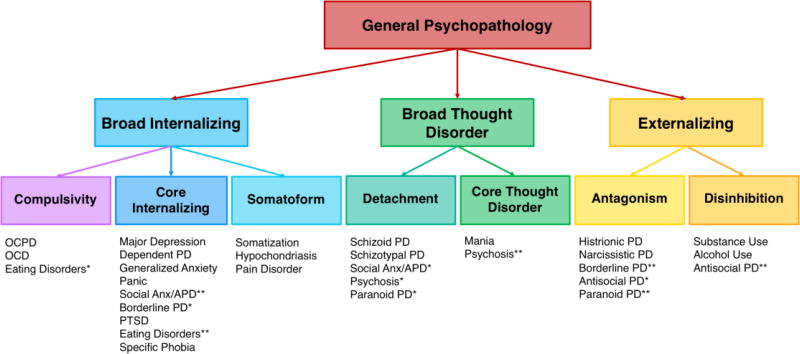
Figure 3.
A summary of the hierarchical structural relationships based on convergence between the bass-ackwards model and the cluster analysis. Disorders are listed under the spectra that they indicate, sorted by the strength of their component loadings in the seven-component bass-ackwards model (strongest to weakest).
*denotes disorders that indicated more than one spectrum, based on the top-down and bottom-up analyses, as well as cross-loadings ≥ .4 in the seven-component bass-ackwards model.
**denotes the stronger component loading for disorders that indicated more than one spectrum.
Note. OCPD = obsessive-compulsive personality, OCD = obsessive-compulsive disorder, PD = personality disorder, Social Anx/APD = social anxiety and/or avoidant personality disorder, PTSD = posttraumatic stress disorder. PD variables include subthreshold cases with one criterion less than DSM-IV thresholds.
In contrast to the bass-ackwards results, the compulsivity cluster was most closely related to the core internalizing cluster, and emerged from the larger broad internalizing cluster. Combined with its equal relationships across the broad internalizing and somatoform components in the bass-ackwards analysis, it seems most likely that compulsivity represents a factor nested under the broad internalizing spectrum.
The convergence between the top-down and bottom-up analyses is shown in Figure 2, and a summary of the resultant integrative hierarchical model is shown in Figure 4. Indicators were assigned to spectra based on their cluster assignment, and based on substantial component loadings (≥ .4) in the seven-component bass-ackwards model (i.e., after all seven spectra had emerged).
Discussion
This study empirically elucidated the joint hierarchical structure of clinical and personality disorders. The top-down and bottom-up analyses converged on remarkably similar results, forming a three-tier hierarchical model of psychopathology. The bottom tier of both hierarchies included the same seven spectra: disinhibition, antagonism, core thought disorder, detachment, core internalizing, somatoform, and compulsivity. These spectra were nested under three superspectra in both methods: externalizing, broad thought disorder, and broad internalizing. In turn, these superspectra were nested under a single general psychopathology dimension. Although the focus on only maladaptive behaviors and traits in the present study means that the general factor may be a positive manifold in this instance [i.e., a consequence of the systematic positive correlations among all the indicators, cf. 26], there is a growing body of evidence supporting the validity and utility of a factor representing the general propensity towards psychopathology [e.g., 32]. We discuss the lower tiers of the hierarchy—one branch of the hierarchy at a time—in the context of the extant literature below.
4.1 Externalizing Spectra
Disinhibition was characterized by alcohol use and substance use disorders in both methods; in addition, antisocial personality disorder spanned both disinhibition and antagonism in the bass-ackwards model, in line with past research [7]. A disinhibition spectrum has consistently emerged in a five-factor psychopathology structure [18, 20, 21] and also mirrors the impulsivity factor in the hierarchical structure of personality [7]. Antagonism was characterized by histrionic, narcissistic, borderline, antisocial, and paranoid personality disorders in both methods, also mirroring previous studies integrating clinical and personality disorders, as well as normal and maladaptive personality [7, 17, 18, 20, 21]. Disinhibition and antagonism were nested components of the broader externalizing spectrum, which has emerged in all studies of the structure of psychopathology in the absence of distinct lower-order factors [17, 19].
4.2 Thought Disorder Spectra
The core thought disorder spectrum was characterized by mania and psychosis in the top-down and bottom-up methods. Although this representation of the thought disorder spectrum was narrower than past research [53], the classification of psychosis and mania together mirrors prior structural studies of clinical and personality disorders [18, 19, 21], likely reflecting disorganized symptoms and delusions common in both conditions. The other disorders that have typically been assigned to a thought disorder spectrum [e.g., schizotypal and paranoid personality disorders; 53] were indicators for the detachment spectrum in our results. Of note, schizotypal personality disorder is highly heterogeneous—including symptoms of both detachment and psychoticism—which likely accounted for its loading on detachment in the present analyses and on a core thought disorder spectrum in past analyses [e.g., 11]. Otherwise, detachment mirrored the pathological/anhedonic introversion factors in prior work [17, 19–21], with the absence of dependent personality disorder, which fell on this spectrum in some other studies [17, 19, 20]—although not in all [18, 21]. As mentioned below, dependent personality instead loaded onto the core internalizing spectrum in our study, highlighting its prominent neuroticism component [7]. Delineating the boundaries of these spectra using symptom-level data to account for heterogeneity within disorders is an important topic for future research.
Together, the detachment and core thought disorder spectra were nested under a broad thought disorder spectrum, consistent with the previous analysis of these data [18], but representing a more generalized thought disorder spectrum compared to some other studies [e.g., 4, 11]. These results are in line with classifying negative symptoms—which are extreme manifestations of detachment—with positive symptoms—which are extreme manifestations of psychoticism—under the common rubric of schizophrenia [53].
4.3 Internalizing Spectra
A core internalizing spectrum emerged, representing the fifth factor that is consistently found in joint structures of psychopathology, and of normal and maladaptive personality [17, 18, 20, 21, 54]. In top-down and bottom-up analyses, core internalizing was characterized by major depressive episode, dependent personality, generalized anxiety, panic, social phobia/avoidant personality, posttraumatic stress, and specific phobia, consistent with the existing literature [12, 18, 21]. Borderline personality and eating disorders also had substantial loadings onto the internalizing factor in the bass-ackwards model, mirroring other studies [e.g., 18, 21, 55]. In contrast with past research on the structure of clinical disorders, distinct fear and distress spectra did not emerge [e.g., 14, 17], but they may only emerge at lower levels of the structure.
The somatoform spectrum was characterized in both methods by somatization, hypochondriasis, and pain disorder. This mirrored the previous analysis of these data, which provided the first evidence for a somatoform spectrum of psychopathology [18]. Although a somatoform factor did not emerge in Markon’s [19] analyses due to limited indicators, Krueger et al. [56] found that structural models with a distinct somatoform factor had similar model fit to those that subsumed somatization indicators under an internalizing factor. The latter finding is consistent with a hierarchical internalizing spectrum and a nested somatoform subspectrum, as both models provide adequate fit. However, given the limited number of studies that have included multiple indicators of somatoform disorders, this issue requires further research.
Finally, a novel compulsivity spectrum emerged that was characterized by obsessive-compulsive personality and obsessive-compulsive disorder in both methods. Eating disorders also were classified as indicators for the compulsivity spectrum in the cluster analysis, although it is noteworthy that eating disorders were only a weak indicator for compulsivity in the seven-component bass-ackwards model (b = .17). The assignment of eating disorders to the compulsivity cluster is consistent with the concurrent and prospective associations among obsessive-compulsive personality disorder and obsessive-compulsive disorder symptoms with restricting, binging, and purging eating pathology [57–59], as well as their shared familial risk and shared traits [e.g., perfectionism, 60]. In addition to the primary assignment of antisocial personality disorder to both disinhibition (bass-ackwards) and antagonism (cluster analyses), the assignment of eating disorders to both internalizing (bass-ackwards) and compulsivity (cluster analyses) represented the only other instance wherein disorder indicators did not have the same primary assignment for both methods. Future research should include symptom-level measurement of these disorders—indeed of all psychopathology—to allow the homogeneous syndromes nested within disorder indicators to be classified and characterized with more specificity.
Although obsessive-compulsive disorder has tended to load under broader internalizing factors in past research [e.g., 19, 21, 61], the emergence of a compulsivity factor of psychopathology mirrors models of personality, which consistently include a domain regarding the control and regulation of behavior [7]. It is noteworthy that the grouping of obsessive-compulsive disorder and obsessive-compulsive personality disorder is consistent with research that has found a unique relationship between these disorders, diverging from depressive and anxiety disorders [62], but is in contrast to research highlighting the distinctions between them [63]. Further, the compulsivity component was aberrant in the bass-ackwards analyses, as it did not emerge from the higher-order components as did the other six lower-order components. This spectrum therefore requires replication and validation before it can be reliably implemented to guide future research.
The agglomeration of the core internalizing, somatoform, and compulsivity spectra into a broad internalizing superspectrum is consistent with the interrelationships among the indicators for these spectra, which have been found to cluster together in past research [e.g., 17, 18, 19, 21]. In contrast, other nested dimensions of the broad internalizing superspectrum that have been found in prior work—such as distinct eating pathology and low sexual function subspectra [55, 64]—did not emerge, due to the lack of sufficient indicators. The internalizing spectra found in the present study thus highlight the influence of the nature and number of indicators used to delineate structural models, as well as the variability of these symptoms, as the nested somatoform and compulsivity spectra also would not emerge in studies without sufficient indicators or variability to characterize these factors [e.g., 17, 19, 21; cf. example of thought disorder in section 1.3].
4.4 Comparing the Top-Down and Bottom-Up Methods
Overall, the consistency between the two sets of analyses was remarkable, given the differences in the underlying methods; they converged at all tiers of the hierarchy. The maximum divergence in grouping of diagnoses between component and cluster analyses did not exceed 12.5%, and there was 91.7% overlap between them at the seven-spectrum level. Both methods also converged on three superspectra representing disordered emotion (broad internalizing), cognition (broad thought disorder), and behavior (externalizing), reflecting the three core components of psychopathology. The convergence between the methods reinforces the evidence for a hierarchical model. For example, cluster analysis is more prone to illusory hierarchies than principal components analysis because the mutually exclusive clusters do not allow for indicators to have cross-loadings to multiple domains, which have been found to account for apparent hierarchical relationships in personality research [43, 65]. In contrast, the bass-ackwards analyses allowed all indicators to load on all components. The cross-loadings in the bass-ackwards method therefore not only relaxed the highly restrictive structure of cluster analysis, but also accounted for some of the heterogeneity within diagnostic categories, such as the distinct internalizing and externalizing components of borderline personality disorder [66, 67]. Taken together, the constancy of the hierarchy in both methods suggests that these are not illusory hierarchical relationships due to residual correlations between factors [cf. 43], or to substantively distinct factors perpetuating through multiple levels of analysis [36].
4.5 Limitations and Future Directions
These results should be interpreted in the context of the limitations of the present study. The primary limitation of the present study was the use of dichotomous indicator variables to represent each DSM diagnosis. There was evident heterogeneity within these disorder indicators. For example, a quarter of the indicators were assigned to multiple spectra based primarily on substantial cross-loadings in the bass-ackwards analyses (i.e., multiple component loadings ≥ .4) reflecting the conflation of multiple syndromes within the diagnostic categories. This heterogeneity within DSM diagnoses highlights the importance of future research including symptom-level measurement of disorders, as mentioned above, rather than relying on the arbitrary diagnostic thresholds that suppress variability in the clinical presentation of disorders. A symptom-level approach in future research not only would allow for the modelling of this diagnostic heterogeneity, but also would allow for more comprehensive examination of variation in functioning. Further, the measurement of anorexia nervosa, bulimia nervosa, and binge eating disorder symptoms was limited to a single dichotomous variable, which excluded delineation of the factors that distinguish between these disorders [e.g., 68, 69]. Finer grained measurement of eating pathology in particular should therefore be a focus in future research.
This study was also limited to maladaptive traits and behaviors, and did not include normative variants of clinical and personality disorders. Some research has suggested that normal personality and clinical disorders may have weak integration [70, 71]. However, other studies have found that normal and maladaptive personality are integrable [e.g., 54], that normal personality has strong relationships with clinical disorders [e.g., 29, 72], and that maladaptive personality and clinical disorders are integrable [7, 73]. Taken together, these past findings suggest that there is scope to extend the present framework, which would be an interesting avenue for future research.
Finally, we did not account for the method variance associated with using different structured interviews for clinical and personality disorders. The hierarchical structure in the present study generally integrated these traditionally separate groups of disorders, suggesting this is indeed a joint hierarchical structure—akin to Wright and Simms [21], which did account for method variance. Whereas factors derived in bass-ackwards analyses of personality have been found to distinguish among clinical disorders [29, 74], here the spectra in the hierarchy represented the shared characteristics among clinical and personality disorders. It is noteworthy, however, that the antagonism, core thought disorder, and somatoform spectra were exclusively identified by either clinical or personality disorders. Given Røysamb and colleagues [20] suggested axis clustering may be substantial in the joint structure of psychopathology, future research should also investigate this further.
4.6 Conclusions
Despite these limitations, our study found interesting and novel results. Two methods of hierarchical analysis converged on a joint hierarchy of psychopathology that appears to be systematic and reliable, and is directly applicable to clinical populations. This hierarchy can thus be used as a flexible and integrative framework to facilitate psychopathology research with varying levels of specificity. For example, rather than focusing on the optimal number of factors to characterize personality or clinical phenomena, researchers can focus on the optimal resolution for their research; selecting a level of the hierarchy (e.g., broader higher-order factors, or narrower lower-order factors) based on whether they are interested in generalist or specialist processes. This hierarchy should also be extended upon in future research—including refinement downwards based on symptom-level analyses—and should be iteratively refined using different disorder indicators and samples.
Supplementary Material
An animation of the convergence between cluster analysis and bass-ackwards analyses. Indicators are grouped by their cluster and component assignments, respectively. Since clusters are mutually exclusive, indicators were automatically assigned to a cluster; indicators were assigned to components based on their highest component loading.
Note. PD variables include subthreshold cases with one criterion less than DSM-IV thresholds.
Acknowledgments
Role of Funding Source: Dr. Forbes was supported by the National Institute of Drug Abuse (T320A037183). NIDA had no further role in the study design; in the collection, analysis, and interpretation of data; in writing; nor in the decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: None.
The bass-ackwards method can also be conducted in an exploratory structural equation modelling framework [e.g., 34]. We chose to use a principal components framework based on Goldberg’s [38] recommendation.
In traditional hierarchical models (e.g., a hierarchical confirmatory factor analysis, or a bifactor model), the variance in the higher-order factors is removed from the lower-order factors. For example, in a hierarchical model of the internalizing spectrum, the subordinate fear and distress factors capture only the small distinctions between fear and distress indicators (e.g., what makes Generalized Anxiety Disorder different from Panic Disorder), but not the shared aspects within the subfactors (e.g., what makes Generalized Anxiety Disorder similar to Major Depression); the latter actually represent most of the variance in the model. This means that the subordinate factors in these hierarchical models have little independent substantive meaning.
We refer to tiers of the hierarchy to distinguish between nested components of the hierarchical structure and levels of the hierarchical analyses. For example, the internalizing and externalizing spectra are forced onto different levels in the analyses because only one new component or cluster can emerge at each level. However, we can collapse them into a single tier to represent their equivalent rank (i.e., “superspectra”) in the hierarchical model [4].
References
- 1.Haslam N, Holland E, Kuppens P. Categories versus dimensions in personality and psychopathology: A quantitative review of taxometric research. Psychological medicine. 2012;42:903–20. doi: 10.1017/S0033291711001966. [DOI] [PubMed] [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and statistical manual of mental disorders, (5th ed.), International Version. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 3.Eaton NR, Rodriguez-Seijas C, Carragher N, Krueger RF. Transdiagnostic factors of psychopathology and substance use disorders: A review. Social Psychiatry and Psychiatric Epidemiology. 2015;50:171–82. doi: 10.1007/s00127-014-1001-2. [DOI] [PubMed] [Google Scholar]
- 4.Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby M, et al. The Hierarchical Taxonomy Of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of abnormal psychology. doi: 10.1037/abn0000258. in press. [DOI] [PubMed] [Google Scholar]
- 5.Bagby RM, Sellbom M, Ayearst LE, Chmielewski MS, Anderson JL, Quilty LC. Exploring the hierarchical structure of the MMPI-2-RF Personality Psychopathology Five in psychiatric patient and university student samples. Journal of personality assessment. 2014;96:166–72. doi: 10.1080/00223891.2013.825623. [DOI] [PubMed] [Google Scholar]
- 6.Morey LC, Krueger RF, Skodol AE. The hierarchical structure of clinician ratings of proposed DSM-5 pathological personality traits. Journal of abnormal psychology. 2013;122:836–41. doi: 10.1037/a0034003. [DOI] [PubMed] [Google Scholar]
- 7.Widiger TA, Simonsen E. Alternative dimensional models of personality disorder: Finding a common ground. Journal of Personality Disorders. 2005;19:110–30. doi: 10.1521/pedi.19.2.110.62628. [DOI] [PubMed] [Google Scholar]
- 8.Wright AG, Thomas KM, Hopwood CJ, Markon KE, Pincus AL, Krueger RF. The hierarchical structure of DSM-5 pathological personality traits. Journal of abnormal psychology. 2012;121:951–7. doi: 10.1037/a0027669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krueger RF, Derringer J, Markon KE, Watson D, Skodol AE. Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychological medicine. 2012;42:1879–90. doi: 10.1017/S0033291711002674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krueger RF, Eaton NR, Clark LA, Watson D, Markon KE, Derringer J, et al. Deriving an empirical structure of personality pathology for DSM-5. Journal of Personality Disorders. 2011;25:170–91. doi: 10.1521/pedi.2011.25.2.170. [DOI] [PubMed] [Google Scholar]
- 11.Kotov R, Chang S, Fochtmann L, Mojtabai R, Carlson G, Sedler M, et al. Schizophrenia in the internalizing-externalizing framework: A third dimension. Schizophrenia Bulletin. 2010;24:1–11. doi: 10.1093/schbul/sbq024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krueger RF, Caspi A, Moffit T, Silva P. The structure and stability of common mental disorders (DSM-III-R): A longitudinal-epidemiological study. Journal of abnormal psychology. 1998;107:216–27. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- 13.Keyes KM, Eaton NR, Krueger RF, Skodol AE, Wall MM, Grant B, et al. Thought disorder in the meta-structure of psychopathology. Psychological medicine. 2013;43:1673–83. doi: 10.1017/S0033291712002292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Watson D. Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. Journal of abnormal psychology. 2005;114:522–36. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- 15.Krueger RF, South SC. Externalizing disorders: Cluster 5 of the proposed meta-structure for DSM-V and ICD-11. Psychological medicine. 2009;39:2061–70. doi: 10.1017/S0033291709990328. [DOI] [PubMed] [Google Scholar]
- 16.Lahey BB. Public health significance of neuroticism. The American Psychologist. 2009;64:241–56. doi: 10.1037/a0015309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blanco C, Krueger RF, Hasin DS, Liu SM, Wang S, Kerridge BT, et al. Mapping common psychiatric disorders: Structure and predictive validity in the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2013;70:199–208. doi: 10.1001/jamapsychiatry.2013.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kotov R, Ruggero CJ, Krueger RF, Watson D, Yuan Q, Zimmerman M. New dimensions in the quantitative classification of mental illness. Archives of General Psychiatry. 2011;68:1003–11. doi: 10.1001/archgenpsychiatry.2011.107. [DOI] [PubMed] [Google Scholar]
- 19.Markon KE. Modeling psychopathology structure: A symptom-level analysis of Axis I and II disorders. Psychological medicine. 2010;40:273–88. doi: 10.1017/S0033291709990183. [DOI] [PubMed] [Google Scholar]
- 20.Roysamb E, Kendler KS, Tambs K, Orstavik RE, Neale MC, Aggen SH, et al. The joint structure of DSM-IV Axis I and Axis II disorders. Journal of abnormal psychology. 2011;120:198–209. doi: 10.1037/a0021660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wright AGC, Simms LJ. A metastructural model of mental disorders and pathological personality traits. Psychological medicine. 2015;45:2309–19. doi: 10.1017/S0033291715000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Forbush KT, Watson D. The structure of common and uncommon mental disorders. Psychological medicine. 2013;41:97–108. doi: 10.1017/S0033291712001092. [DOI] [PubMed] [Google Scholar]
- 23.McNulty JL, Overstreet SR. Viewing the MMPI-2-RF structure through the Personality Psychopathology Five (PSY-5) lens. Journal of personality assessment. 2014;96:151–7. doi: 10.1080/00223891.2013.840305. [DOI] [PubMed] [Google Scholar]
- 24.Sellbom M. Mapping the MMPI-2-RF Specific Problems Scales Onto Extant Psychopathology Structures. Journal of personality assessment. 2016:1–10. doi: 10.1080/00223891.2016.1206909. [DOI] [PubMed] [Google Scholar]
- 25.American Psychiatric Association. Diagnostic and statistical manual of mental disorders, (4th ed.), Text Revision, International Version. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 26.Revelle W, Wilt J. The general factor of personality: A general critique. Journal of Research in Personality. 2013;47:493–504. doi: 10.1016/j.jrp.2013.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kushner SC, Quilty LC, Tackett JL, Bagby RM. The hierarchical structure of the Dimensional Assessment of Personality Pathology (DAPP-BQ) Journal of Personality Disorders. 2011;25:504–16. doi: 10.1521/pedi.2011.25.4.504. [DOI] [PubMed] [Google Scholar]
- 28.Tackett JL, Krueger RF, Iacono WG, McGue M. Personality in middle childhood: A hierarchical structure and longitudinal connections with personality in late adolescence. Journal of Research in Personality. 2008;42:1456–62. doi: 10.1016/j.jrp.2008.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tackett JL, Quilty LC, Sellbom M, Rector NA, Bagby RM. Additional evidence for a quantitative hierarchical model of mood and anxiety disorders for DSM-V: The context of personality structure. Journal of abnormal psychology. 2008;117:812–25. doi: 10.1037/a0013795. [DOI] [PubMed] [Google Scholar]
- 30.Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, et al. The p Factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science. 2014;2:119–37. doi: 10.1177/2167702613497473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lahey BB, Van Hulle CA, Singh AL, Waldman ID, Rathouz PJ. Higher-order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Archives of General Psychiatry. 2011;68:181–9. doi: 10.1001/archgenpsychiatry.2010.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lahey BB, Krueger RF, Rathouz PJ, Waldman ID, Zald DH. A hierarchical causal taxonomy of psychopathology across the life span. Psychological bulletin. 2016 doi: 10.1037/bul0000069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Farmer RF, Seeley JR, Kosty DB, Olino TM, Lewinsohn PM. Hierarchical organization of Axis I psychiatric disorder comorbidity through age 30. Comprehensive Psychiatry. 2013;54:523–32. doi: 10.1016/j.comppsych.2012.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim H, Eaton NR. The hierarchical structure of common mental disorders: Connecting multiple levels of comorbidity, bifactor models, and predictive validity. Journal of abnormal psychology. 2015;124:1064–78. doi: 10.1037/abn0000113. [DOI] [PubMed] [Google Scholar]
- 35.Clark LA, Watson D. Temperament: An organizing paradigm for trait psychology. In: John OP, Robins RW, Pervin LA, editors. Handbook of Personality: Theory and Research. New York: Guilford Press; 2008. pp. 265–86. [Google Scholar]
- 36.Loehlin JC, Goldberg LR. Do personality traits conform to lists or hierarchies? Personality and Individual Differences. 2014;70:51–6. doi: 10.1016/j.paid.2014.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Forbes MK, Tackett JL, Markon KE, Krueger RF. Beyond comorbidity: Toward a dimensional and hierarchical approach to understanding psychopathology across the life span. Development and Psychopathology. 2016;28:971–86. doi: 10.1017/S0954579416000651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Goldberg LR. Doing it all Bass-Ackwards: The development of hierarchical factor structures from the top down. Journal of Research in Personality. 2006;40:347–58. [Google Scholar]
- 39.Saucier G. Orthogonal Markers for Orthogonal Factors: The Case of the Big Five. Journal of Research in Personality. 2002;36:1–31. [Google Scholar]
- 40.Bacon DR. An evaluation of cluster analytic approaches to initial model specification. Structural Equation Modeling. 2001;8:397–429. [Google Scholar]
- 41.Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, personality: an integrative quantitative model of the adult externalizing spectrum. Journal of abnormal psychology. 2007;116:645–66. doi: 10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wilson S, Schalet BD, Hicks BM, Zucker RA. Identifying Early Childhood Personality Dimensions Using the California Child Q-Set and Prospective Associations With Behavioral and Psychosocial Development. J Res Pers. 2013;47 doi: 10.1016/j.jrp.2013.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ashton MC, Lee K, Goldberg LR, de Vries RE. Higher-order factors of personality: Do they exist? Personality and Social Psychology Review. 2009;13:79–91. doi: 10.1177/1088868309338467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zimmerman M. Integrating the assessment methods of researchers in routine clinical practice: the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) project. In: First MB, editor. Standardized Evaluation in Clinical Practice. Arlington, VA: American Psychiatric Publishing; 2003. pp. 29–74. [Google Scholar]
- 45.Zimmerman M. A review of 20 years of research on overdiagnosis and underdiagnosis in the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) Project. Canadian Journal of Psychiatry. 2016;61:71–9. doi: 10.1177/0706743715625935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pfohl B, Blum N, Zimmerman M. Structured Interview for DSM-IV Personality. Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- 47.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders—Patient Edition (SCID-I/P, Version 2.0) New York: Biometrics Research Department, New York State Psychiatric Institute; 1995. [Google Scholar]
- 48.Widiger TA. Generalized social phobia versus avoidant personality disorder: a commentary on three studies. Journal of abnormal psychology. 1992;101:340–3. doi: 10.1037//0021-843x.101.2.340. [DOI] [PubMed] [Google Scholar]
- 49.R Development Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2016. [Google Scholar]
- 50.Revelle W. psych: Procedures for personality and psychological research. 1.6.9. Evanston, Illinois, USA: Northwestern University; 2016. [Google Scholar]
- 51.Bentler PM, Yuan K-H. Positive definiteness via off-diagonal scaling of a symmetric indefinite matrix. Psychometrika. 2011;76:119–23. doi: 10.1007/s11336-010-9191-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ward JH. Hierarchical grouping to optimize an objective function. Journal of the American Statistical Association. 1963;58:236–44. [Google Scholar]
- 53.Kotov R, Krueger RF, Watson D, Chmielewski M, Waszczuk MA, Docherty AR, et al. Thought disorder spectrum of the Hierarchical Taxonomy of Psychopathology (HiTOP): Bridging psychosis and personality pathology. Schizophrenia Bulletin. under review. [Google Scholar]
- 54.Wright AG, Simms LJ. On the structure of personality disorder traits: Conjoint analyses of the CAT-PD, PID-5, and NEO-PI-3 trait models. Personality Disorders. 2014;5:43–54. doi: 10.1037/per0000037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Forbush KT, South SC, Krueger RF, Iacono WG, Clark LA, Keel PK, et al. Locating eating pathology within an empirical diagnostic taxonomy: Evidence from a community-based sample. Journal of abnormal psychology. 2010;119:282–92. doi: 10.1037/a0019189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Krueger RF, Chentsova-Dutton YE, Markon KE, Goldberg D, Ormel J. A cross-cultural study of the structure of comorbidity among common psychopathological syndromes in the general health care setting. Journal of abnormal psychology. 2003;112:437–47. doi: 10.1037/0021-843x.112.3.437. [DOI] [PubMed] [Google Scholar]
- 57.Halmi KA, Sunday SR, Klump KL, Strober M, Leckman JF, Fichter M, et al. Obsessions and compulsions in anorexia nervosa subtypes. International Journal of Eating Disorders. 2003;33:308–19. doi: 10.1002/eat.10138. [DOI] [PubMed] [Google Scholar]
- 58.Hasler G, LaSalle-Ricci VH, Ronquillo JG, Crawley SA, Cochran LW, Kazuba D, et al. Obsessive–compulsive disorder symptom dimensions show specific relationships to psychiatric comorbidity. Psychiatry Research. 2005;135:121–32. doi: 10.1016/j.psychres.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 59.Anderluh MB, Tchanturia K, Rabe-Hesketh S, Treasure J. Childhood obsessive-compulsive personality traits in adult women with eating disorders: Defining a broader eating disorder phenotype. American Journal of Psychiatry. 2003;160:242–7. doi: 10.1176/appi.ajp.160.2.242. [DOI] [PubMed] [Google Scholar]
- 60.Halmi KA, Tozzi F, Thornton LM, Crow S, Fichter MM, Kaplan AS, et al. The relation among perfectionism, obsessive-compulsive personality disorder and obsessive-compulsive disorder in individuals with eating disorders. International Journal of Eating Disorders. 2005;38:371–4. doi: 10.1002/eat.20190. [DOI] [PubMed] [Google Scholar]
- 61.Slade T, Watson D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychological medicine. 2006;36:1593–600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- 62.Eisen JL, Coles ME, Shea MT, Pagano ME, Stout RL, Yen S, et al. Clarifying The Convergence Between Obsessive Compulsive Personality Disorder Criteria And Obsessive Compulsive Disorder. Journal of Personality Disorders. 2006;20:294–305. doi: 10.1521/pedi.2006.20.3.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wu KD, Clark LA, Watson D. Relations between Obsessive-Compulsive Disorder and personality: beyond Axis I-Axis II comorbidity. Journal of anxiety disorders. 2006;20:695–717. doi: 10.1016/j.janxdis.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 64.Forbes MK, Baillie AJ, Eaton NR, Krueger RF. A place for sexual dysfunctions in an empirical taxonomy of psychopathology. Annual Review of Sex Research. doi: 10.1080/00224499.2016.1269306. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Marsh HW, Morin AJ, Parker PD, Kaur G. Exploratory structural equation modeling: An integration of the best features of exploratory and confirmatory factor analysis. Annual Review of Clinical Psychology. 2014;10:85–110. doi: 10.1146/annurev-clinpsy-032813-153700. [DOI] [PubMed] [Google Scholar]
- 66.Eaton NR, Krueger RF, Keyes KM, Skodol AE, Markon KE, Grant BF, et al. Borderline personality disorder co-morbidity: Relationship to the internalizing-externalizing structure of common mental disorders. Psychological medicine. 2011;41:1041–50. doi: 10.1017/S0033291710001662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.James LM, Taylor J. Revisiting the structure of mental disorders: Borderline personality disorder and the internalizing/externalizing spectra. The British Journal of Clinical Psychology. 2008;47:361–80. doi: 10.1348/014466508X299691. [DOI] [PubMed] [Google Scholar]
- 68.Allen KL, Byrne SM, Crosby RD. Distinguishing between risk factors for bulimia nervosa, binge eating disorder, and purging disorder. Journal of Youth and Adolescence. 2015;44:1580–91. doi: 10.1007/s10964-014-0186-8. [DOI] [PubMed] [Google Scholar]
- 69.Stice E. Risk and maintenance factors for eating pathology: A meta-analytic review. Psychological bulletin. 2002;128:825–48. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- 70.Slobodskaya HR. The contribution of reinforcement sensitivity to the personality-psychopathology hierarchical structure in childhood and adolescence. Journal of abnormal psychology. 2016;125:1067–78. doi: 10.1037/abn0000179. [DOI] [PubMed] [Google Scholar]
- 71.van der Heijden PT, Rossi GMP, van der Veld WM, Derksen JJL, Egger JIM. Personality and psychopathology: Higher order relations between the five factor model of personality and the MMPI-2 Restructured Form. Journal of Research in Personality. 2013;47:572–9. [Google Scholar]
- 72.Kotov R, Gamez W, Schmidt F, Watson D. Linking "big" personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychological bulletin. 2010;136:768–821. doi: 10.1037/a0020327. [DOI] [PubMed] [Google Scholar]
- 73.Markon KE, Krueger RF, Watson D. Delineating the structure of normal and abnormal personality: An integrative hierarchical approach. Journal of Personality and Social Psychology. 2005;88:139–57. doi: 10.1037/0022-3514.88.1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Uliaszek AA, Al-Dajani N, Bagby RM. The relationship between psychopathology and a hierarchical model of normal personality traits: Evidence from a psychiatric patient sample. Journal of Personality Disorders. 2015;29:719–34. doi: 10.1521/pedi_2014_28_170. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
An animation of the convergence between cluster analysis and bass-ackwards analyses. Indicators are grouped by their cluster and component assignments, respectively. Since clusters are mutually exclusive, indicators were automatically assigned to a cluster; indicators were assigned to components based on their highest component loading.
Note. PD variables include subthreshold cases with one criterion less than DSM-IV thresholds.