Abstract
Objective
This study aims to determine the distribution of observed atherosclerotic cardiovascular disease (ASCVD) incidence in contemporary cohorts in China, and to identify cut-off points for ASCVD risk classification based on traditional criteria and new equations developed by Prediction for ASCVD Risk in China (China-PAR).
Methods
The study populations included cohorts in the China-PAR project, with 34,757 participants eligible for the current analysis. Traditional risk stratification was assessed by using Chinese guidelines on prevention of CVD and hypertension, and 5 risk groups were classified based on these guidelines after slight modification for available risk factors. Kaplan–Meier analysis was conducted to obtain the cumulative incidence of observed ASCVD events for all subjects and sub-groups. The predicted 10-year ASCVD risk was obtained using the China-PAR equations.
Results
A total of 1922 ASCVD events were identified during an average follow-up of 14.1 years. According to the group classification based on traditional risk stratification, the observed 10-year risks for ASCVD were 4.61% (95% confidence interval [CI]: 4.11–5.10%) in the moderate-risk group and 8.74% (95% CI: 7.82–9.66%) in the high-risk group. Based on the China-PAR equations for risk assessment of ASCVD, those with predicted risks of <5%, 5–10%, and ≥10% could be classified into categories of low-, moderate-, and high-risk for ASCVD, respectively.
Conclusion
The findings enable development of a simple method for classification of individuals into low-, moderate-, and high-risk groups, based on the China-PAR equations. The method will be useful for self-management and prevention of ASCVD in Chinese adults.
Keywords: Risk stratification, Atherosclerotic cardiovascular disease, Cohort, China-PAR project
Introduction
Atherosclerotic cardiovascular disease (ASCVD) is the leading cause of mortality and disease burden in China.1 From 1990 to 2010, stroke became the leading cause of death in China, followed by ischemic heart disease.2 The rapid increase in ASCVD is attributable to the aging population, lifestyle changes, and high prevalence of ASCVD risk factors such as hypertension, dyslipidemia, diabetes, and obesity.3, 4, 5
Risk factors for ASCVD were first identified by the Framingham Heart Study,6, 7, 8 followed by extensive research in China and other countries.9, 10 Several tools and equations for risk stratification, such as the Framingham general cardiovascular disease (CVD) equations8 and the Pooled Cohort Equations (PCE),11 have been developed to help healthcare practitioners identify individuals at high-risk of CVD. In China, Liu et al and Wu et al also developed risk prediction tools for coronary heart disease (CHD) and ischemic CVD, respectively, over 10 years ago.12, 13 However, risk factor profiles in China have changed dramatically, and new equations have recently been developed by Prediction for ASCVD Risk in China (China-PAR) to predict 10-year ASCVD risk; these have been derived and validated using 4 contemporary Chinese cohorts, based on traditional lifestyles, metabolic risk factors, and several new indicators such as waist circumference (WC), geographic region (Northern vs. Southern), urbanization (Urban vs. Rural), and family history of ASCVD.14 To facilitate the use of China-PAR equations for ASCVD risk assessment in prevention and clinical practice in China, we examined ASCVD incidence and differences in ASCVD risk among diverse age groups, genders, and geographic regions.
In addition, the Chinese Guideline on Prevention of CVD was published in 2011 and recommended a scale of risk stratification for CVD prevention by classifying 5 groups as very-low-, low-, moderate-, high-, and very-high-risk.15 This scale of risk stratification was also one of the main references for Chinese guidelines on prevention and control of hypertension and dyslipidemia in the evaluation of risk for CVD. However, traditional risk stratification was somewhat complicated, and was not commonly used by primary healthcare practitioners, especially in defined communities and rural areas. As an alternative, the newly developed China-PAR equations can serve as a valuable tool for prediction of 10-year ASCVD risk in the general Chinese population; for the equations to be useful, we must identify cut-off points for ASCVD risk classification, and make these more accessible for physicians and the general populations. Availability through Web App tools is also necessary.
Therefore, we aimed to identify the distribution of observed ASCVD incidence in large-scale contemporary cohorts in China, and to determine cut-off points for 10-year ASCVD risk stratification based on the new China-PAR equations and traditional risk stratification criteria derived from the Chinese Guidelines on Prevention of CVD and hypertension.
Methods
Study population
The study population was derived from cohorts in the China-PAR project, including those in the International Collaborative Study of Cardiovascular Disease in Asia (InterASIA) and China Multi-Center Collaborative Study of Cardiovascular Epidemiology (China MUCA-1998 and China MUCA-1992-1994). Details of baseline and follow-up information for the cohorts have been published elsewhere.14 Briefly, a total of 41,412 participants were enrolled in the 3 cohorts. After excluding participants lost to follow-up, those with ASCVD at baseline, and those with inadequate blood test measurements, 34,757 participants were eligible for the current analysis.
In addition to the 3 cohorts, the Community Intervention of Metabolic Syndrome in China & Chinese Family Health Study (CIMIC) was used for the comparison of trends for proportions of participants in different risk categories. The CIMIC was a large community-based cohort that was established for study from 2007 to 2008 and completed follow-up surveys from 2012 to 2015. Data from 69,102 participants aged 35–74 years and free of ASCVD were included in the study.
These preceding studies were all approved by the Institutional Review Board at Fuwai Hospital in Beijing. Written informed consent was obtained from each participant before data collection.
Definition of traditional risk stratification
Traditional risk stratification was assessed by using the Chinese Guideline on Prevention of CVD.15 Five risk groups were classified based on the guideline after slight modification for the risk factors that we measured (shown in Table S1). These risk factors included: (1) aging (age > 55 years in men and >65 years in women); (2) current smoking; (3) lipid disorder (total cholesterol [TC] ≥ 200 mg/dl, or low-density lipoprotein cholesterol [LDL-C] ≥ 130 mg/dl, or high-density lipoprotein cholesterol [HDL-C] < 40 mg/dl, or triglyceride [TG] ≥ 150 mg/dl); (4) 100 ≤ fast plasma glucose < 126 mg/dl; (5) obesity according to WC (≥90 cm in men and ≥85 cm in women) or body mass index (BMI ≥ 28 kg/m2); and (6) family history of ASCVD.
Additionally, risk stratification for hypertensive patients was modified based on the Chinese Guideline on Hypertension Management in Primary Health-care Clinics 2014 (shown in Table S2).16 The risk factors required for the risk stratification scale were the same as those shown above.
Definition of ASCVD
ASCVD was defined as nonfatal acute myocardial infarction (MI), or CHD death, or fatal or nonfatal stroke. Acute MI was defined as an increase in biochemical markers of myocardial necrosis, accompanied by either ischemic symptoms, pathological Q waves, ST segment elevation or depression, or coronary intervention.17 CHD death included all fatal events due to MI or other coronary deaths. Fatal or nonfatal stroke included cases with signs of hemorrhage or cerebral infarction, with rapidly developing focal (or global) disturbances in cerebral function and lasting more than 24 h without apparent nonvascular cause.
Statistical analysis
Means or corresponding percentages of baseline characteristics were calculated. Person-years of follow-up were calculated as the difference between the date of baseline and the date of ASCVD occurrence, the date of death, or the last follow-up interview, whichever occurred first.
Kaplan–Meier analysis was used to obtain the observed ASCVD event rate in the cohorts from the China-PAR project. The predicted 10-year ASCVD risk was obtained using the China-PAR equations for the same cohort participants. The China-PAR equations for 10-year ASCVD risk prediction were developed from gender-specific Cox proportional hazards models, and the variables in the equations included age, treated or untreated systolic blood pressure (SBP), total cholesterol (TC), HDL-C, current smoking (Yes/No), diabetes (Yes/No), WC, geographic region (Northern/Southern), urbanization (Urban/Rural), and family history of ASCVD (Yes/No), as well as available interaction terms for age with risk factors that met predefined statistical criteria.14
All analyses were conducted using the SAS statistical package (version 9.2; SAS Institute, Inc., Cary, North Carolina, USA) and R software (version 3.2.3. https://www.r-project.org/).
Results
The baseline characteristics of the participants are presented in Table 1 according to the stratification based on the Chinese Guideline on Prevention of CVD. There were 6018, 16,922, 7303, 3813, and 701 participants in the very-low-, low-, moderate-, high-, and very-high-risk cohorts, respectively. The ages, BMI, WC, blood pressure, TC, LDL-C, TG, and glucose increased from the very-low-risk to the high-risk group. Other than SBP and diastolic blood pressure (DBP), the metabolic characteristics of participants in the very-high-risk group were similar to those in the high-risk group. Most current smokers and diabetic patients were in the high-risk group, with 53.50% and 19.91%, respectively.
Table 1.
Baseline characteristics of 34,757 subjects in cohorts from the China-PAR project.
| Risk groupsa | Very low | Low | Moderate | High | Very high |
|---|---|---|---|---|---|
| Sample size, n | 6018 | 16,922 | 7303 | 3813 | 701 |
| Age, years | 43.72 (6.57) | 46.58 (7.96) | 50.54 (8.86) | 53.28 (9.45) | 53.23 (8.63) |
| Male, n (%) | 1066 (17.71) | 8332 (49.24) | 4121 (56.43) | 2506 (65.72) | 379 (54.07) |
| BMI, kg/m2 | 21.59 (2.41) | 22.55 (3.14) | 24.14 (3.68) | 25.76 (3.90) | 25.65 (4.26) |
| WC, cm | 71.21 (6.45) | 75.74 (8.32) | 80.98 (9.96) | 86.85 (10.31) | 85.08 (11.17) |
| SBP, mmHg | 112.33 (11.42) | 116.27 (12.24) | 132.68 (19.59) | 142.71 (14.44) | 184.24 (19.11) |
| DBP, mmHg | 72.57 (8.09) | 75.02 (8.39) | 83.89 (11.40) | 88.46 (9.42) | 107.95 (12.36) |
| Current smoker, n (%) | 0 (0.00) | 6078 (35.92) | 3120 (42.72) | 2040 (53.50) | 268 (38.23) |
| TC, mg/dl | 162.78 (22.37) | 182.16 (37.56) | 192.05 (39.91) | 202.79 (41.03) | 198.47 (43.59) |
| LDL-C, mg/dl | 91.28 (19.89) | 109.51 (33.06) | 116.41 (35.36) | 123.80 (36.15) | 122.44 (40.73) |
| HDL-C, mg/dl | 56.00 (10.88) | 52.03 (13.54) | 49.60 (13.89) | 46.83 (13.55) | 49.51 (13.61) |
| TG, mg/dlb | 80.90 (65.00, 102.95) | 104.60 (77.70, 145.00) | 125.20 (90.00, 177.60) | 151.80 (106.60, 212.50) | 135.80 (97.30, 188.00) |
| Fasting plasma glucose, mg/dl | 83.08 (10.60) | 87.34 (12.58) | 99.29 (32.63) | 112.80 (41.81) | 102.94 (34.66) |
| Diabetes, n (%) | 0 (0.00) | 0 (0.00) | 637 (8.72) | 759 (19.91) | 88 (12.55) |
| Family history of ASCVD, n (%) | 0 (0.00) | 2336 (13.80) | 1587 (21.73) | 1095 (28.72) | 158 (22.54) |
Data were presented as means with standard derivation or the number of participants with percentages.
ASCVD: atherosclerotic cardiovascular disease; China-PAR project: Prediction for ASCVD Risk in China project; BMI: body mass index; TC: total cholesterol; LDL-C: low-density lipoprotein cholesterol; HDL-C: high-density lipoprotein cholesterol; TG: triglyceride.
Risk groups based on Chinese Guideline on Prevention of CVD in 2011.
TG, median with interquartile range.
During an average follow-up of 14.1 years, a total of 1922 ASCVD events were identified. As shown in Table 2, the observed 10-year risk for ASCVD using Kaplan–Meier adjustment ranged from 1.63% to 13.22% in men and from 0.89% to 10.65% in women. We found that the risk of ASCVD was higher among elderly and urban subgroups, and in northern regions of China. Men were consistently more susceptible to ASCVD than women, regardless of subgroup. In addition, the proportions of individuals with moderate-, high- and very-high-risk for ASCVD have been increasing, when we compared the trends in different risk categories (Table S3).
Table 2.
Kaplan–Meier-adjusted 10-year ASCVD risk in 34,757 subjects in cohorts from the China-PAR project.
| Risk groups | Kaplan–Meier adjusted 10-year risk of ASCVD, % |
|||
|---|---|---|---|---|
| Men (95% CI) | P-valuea | Women (95% CI) | P-valuea | |
| Age, years | <0.001 | <0.001 | ||
| 35–44 | 1.63 (1.33, 1.93) | 0.89 (0.68, 1.10) | ||
| 45–54 | 3.98 (3.47, 4.49) | 2.38 (2.00, 2.76) | ||
| 55–64 | 8.39 (7.38, 9.40) | 5.23 (4.46, 6.00) | ||
| 65–74 | 13.22 (10.49.15.94) | 10.65 (8.15, 13.16) | ||
| Area | 0.05 | 0.42 | ||
| Urban | 4.18 (3.68, 4.67) | 2.54 (2.16, 2.92) | ||
| Rural | 4.03 (3.64, 4.41) | 2.46 (2.18, 2.75) | ||
| Geographic region | <0.001 | <0.001 | ||
| Northern | 5.40 (4.89, 5.90) | 3.64 (3.25, 4.04) | ||
| Southern | 2.90 (2.54, 3.26) | 1.43 (1.19, 1.67) | ||
ASCVD: atherosclerotic cardiovascular disease; China-PAR project: Prediction for ASCVD Risk in China project.
P-value, log-rank tests for 10-year risk of ASCVD across subgroups.
Furthermore, the distribution of 10-year ASCVD risk after Kaplan–Meier adjustment was described for 5 groups using traditional risk stratification, based on the Chinese Guideline on Prevention of CVD, as shown in Table 3. We found that the observed 10-year risks for ASCVD among all subjects were 4.61% (95% CI: 4.11–5.10%) in the moderate-risk group and 8.74% (95% CI: 7.82–9.66%) in the high-risk group. Gender-specific analysis showed similar results and good consistency for the 10-year risks for ASCVD in a comparison of men and women. When analyses were conducted among hypertensive patients based on risk stratification from Chinese guideline on hypertension management, the observed 10-year risks of ASCVD after Kaplan–Meier adjustment were 5.42% in the moderate-risk group and 12.54% in the high-risk group (Table S4).
Table 3.
Ten-year ASCVD risk after Kaplan–Meier-adjustment across different groups for risk stratification.
| Risk groups | Sample size, n | Kaplan–Meier adjusted 10-year ASCVD risk, % |
||
|---|---|---|---|---|
| All (95% CI) | Men (95% CI) | Women (95% CI) | ||
| Very low | 6018 | 0.61 (0.41, 0.81) | 0.68 (0.18, 1.18) | 0.60 (0.38, 0.82) |
| Low | 16,922 | 1.63 (1.44, 1.82) | 1.80 (1.51, 2.09) | 1.46 (1.20, 1.72) |
| Moderate | 7303 | 4.61 (4.11, 5.10) | 4.65 (3.98, 5.31) | 4.55 (3.81, 5.29) |
| High | 3813 | 8.74 (7.82, 9.66) | 9.14 (7.98, 10.30) | 7.98 (6.47, 9.49) |
| Very high | 701 | 23.29 (20.06, 26.51) | 27.92 (23.25, 32.59) | 17.88 (13.59, 22.18) |
| Total | 34,757 | 3.25 (3.06, 3.44) | 4.13 (3.82, 4.44) | 2.49 (2.26, 2.72) |
ASCVD: atherosclerotic cardiovascular disease.
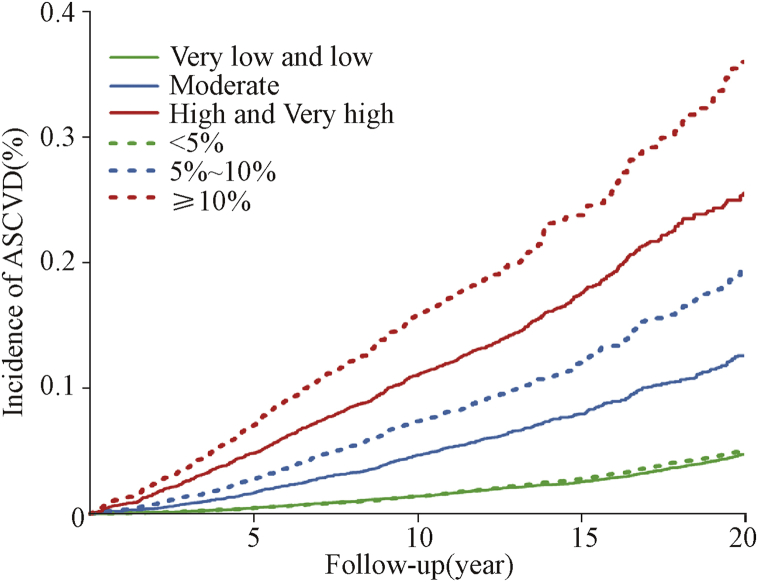
We published gender-specific China-PAR equations for use as a tool to estimate 10-year risks of ASCVD in general populations. The gender-specific equations included variables of age, treated or untreated SBP, TC, HDL-C, current smoking, diabetes, WC, geographic region (Northern/Southern), urbanization (Urban/Rural), and family history of ASCVD, as well as available interaction terms for age with risk factors that met predefined statistical criteria. To facilitate risk assessment by using the China-PAR equations, 5% and 10% were used as cut-off points for simplified risk categories based on the Kaplan–Meier-adjusted risk for ASCVD. Thus, a total of 34,757 participants in the cohorts were divided into 3 new risk categories of <5%, 5–10%, and ≥10%, as predicted by the China-PAR equations; the participants in these cohorts were also reclassified into 3 risk groups (very low and low, moderate, and high and very high) based on traditional stratification criteria derived from the Chinese Guideline on Prevention of CVD. Fig. 1 shows that compared with the high- and very-high-risk groups, the ASCVD incidence increased more quickly among individuals with predicted 10-year ASCVD risk of ≥10%, based on our China-PAR equations. However, the trend in the incidence of ASCVD among individuals with predicted risk of 5–10% increased faster than for those in the traditional moderate group. Our new classification cut-off points of 5% and 10% enabled easier identification of moderate- to high-risk individuals for primary prevention of ASCVD, compared with the results using traditional risk stratification criteria based on the Chinese Guideline on Prevention of CVD.
Fig. 1.
Incidence of ASCVD across different risk stratification groups. The 3 solid lines show the incidence of ASCVD based on the Chinese Guideline on Prevention of CVD, with the very low and low group as the green line, the moderate group as the blue line, and the high and very high group as the red line. The 3 dashed lines show the incidence of ASCVD based on the cut-off points from the China-PAR equations, with green, blue, and red dashed lines for <5%, 5–10%, and ≥10%, respectively. ASCVD: atherosclerotic cardiovascular disease. China-PAR project: Prediction for ASCVD Risk in China project.
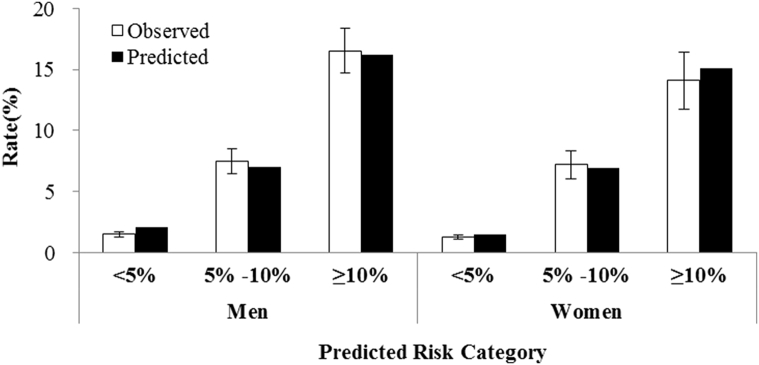
In addition, we compared the observed ASCVD event rates to the predicted rates using our China-PAR equations for the 3 groups with <5%, 5–10%, and ≥10% risk in the cohorts from the China-PAR project (Fig. 2). After gender-specific analysis, there were no substantial differences between the observed and predicted rates. For example, the observed ASCVD event rates in men were 1.49%, 7.46%, and 16.52% across the 3 categories, for which the corresponding predicted risks were 2.07%, 7.03%, and 16.23%, respectively. Similar results were shown for women. This illustrated the good agreement between observation and prediction when participants were classified using predicted risk categories of <5%, 5–10%, and ≥10%.
Fig. 2.
Ten-year Kaplan–Meier observed and predicted ASCVD event rates among 34,757 participants in the cohorts from the China-PAR Project. The observed ASCVD rates after Kaplan–Meier-adjustment are shown as white bars, and the predicted ASCVD rates using the China-PAR equations are shown as black bars. ASCVD: atherosclerotic cardiovascular disease; China-PAR: Prediction for ASCVD Risk in China.
Discussion
The current study showed the distribution of observed 10-year risk for ASCVD among 34,757 Chinese adults aged 35–74 years. The 10-year risk after Kaplan–Meier adjustment was higher in men, and in those living in urban areas and northern regions in China. Furthermore, we compared the 10-year risk for ASCVD across different risk categories based on the Chinese Guideline on Prevention of CVD and the predicted risk based on the China-PAR equations. We propose that predicted 10-year risk of less than 5%, between at least 5% and less than 10%, and 10% or more can be used as cut-off points for low-, moderate-, and high-risk categories. The 3 simplified categories based on predicted ASCVD risk derived from the China-PAR equations provides an additional option for evaluation of 10-year ASCVD risk, and enables identification of high-risk individuals beyond the traditional stratification derived from the Chinese Guideline on Prevention of CVD.
It is a major challenge to control the epidemic of CAD, stroke, and other forms of ASCVD, as well as the associated risk factors in China. According to the data in Table S3, the proportions of individuals with moderate-, high- and very-high-risk for ASCVD have been increasing in recent decades, although the study design and inclusion of participants from 4 cohorts were not perfectly comparative. For example, high- and very-high-risk groups accounted for 14.79% of total participants in 1998–2000, while subjects in the CIMIC cohort at baseline in 2007–2008 accounted for 18.15% in the high- and very-high-risk groups. In addition, Table 2 shows that men and women aged 55 years or older had a 10-year ASCVD risk of over 5%. Men living in northern regions had a higher risk of ASCVD. The distribution of 10-year ASCVD risk varied among different subgroups. Therefore, risk prediction is critical for identification of high-risk individuals and for primary prevention of ASCVD in general populations.
We developed and validated the China-PAR equations for 10-year ASCVD risk prediction in 4 contemporary Chinese cohorts. Based on the incidence risk of ASCVD across 5 groups of risk stratification (Table 3), we proposed 3 simpler risk categories of low-, moderate-, and high-risk, with cutoff points of 5% and 10%. Furthermore, we also examined the observed 10-year risk for ASCVD among hypertensive patients, for whom risk stratification was performed according to the Chinese Guideline on Hypertension Management in Primary Health-care Clinics 2014 (shown in Table S2). Although the ASCVD risks were slightly higher in men than in women across the 3 risk groups as shown in Table S4, the cut-off points of 5% and 10% were also applicable for classification of hypertensive individuals into low-, moderate-, and high-risk groups.
Risk prediction and assessment are also important for guidance in lifestyle modification and management of ASCVD risk factors. For example, the estimated absolute 10-year risk of ASCVD, using the PCE released by the American College of Cardiology and American Heart Association (ACC/AHA), recommended initiation of statin therapy for primary prevention of ASCVD in individuals aged 40–75 with LDL-C 70–189 mg/dl without clinical ASCVD or diabetes.18 They should be treated with moderate- to high-intensity statin therapy if they have an estimated 10-year ASCVD risk ≥7.5%, based on strong evidence from randomized clinical trials; however, treatment with a moderate-intensity statin was reasonable with an estimated 10-year ASCVD risk of 5–7.5%. As another example, the Systematic Coronary Risk Estimation (SCORE) charts developed by the European Society of Cardiology used age, sex, smoking status, TC, and SBP to estimate 10-year risk of a first CVD event, and were recommended for estimation of risk and prevention of CVD in European populations.19 Categories in Europe were defined as low-risk with a SCORE <1%, moderate-risk with a 1% ≤ SCORE <5%, high-risk with a 5% ≤ SCORE <10%, and very-high-risk with a SCORE ≥10%. Based on our current population data and analyses, we simplified 3 risk categories by cut-off points of <5%, 5–10%, and ≥10%. We suggested that low-risk individuals with risk of <5% should be offered lifestyle advice to maintain their low-risk status, while moderate-risk individuals with predicted risk of 5–10% qualify for intensive lifestyle changes and drug treatment if necessary. For high-risk individuals with risk ≥10%, drug therapy should be recommended in addition to lifestyle changes. Nevertheless, uncritical initiation of drug treatment for all individuals with risk over the 10% threshold should be discouraged. The risk classification derived from cut-off points of the China-PAR equations provides easily-applied evaluation criteria to assist in risk assessment, while the predicted risk must be interpreted in light of the clinician's knowledge and experience of overall risk factors that might modify the calculated risk.
Several limitations should be addressed in the current study. In the traditional risk stratification using the Chinese guidelines for both CVD prevention and hypertension management, organ damage was one of the risk classification criteria, reflected by electrocardiographic or echocardiographic left ventricular hypertrophy, carotid wall thickening or plaque, and chronic kidney disease with estimated glomerular filtration rate (eGFR) < 60 ml·min−1·1.73 m−2. Using our population-based design of large-scale cohort studies, it was not possible to access detailed clinical test data. Thus, we used age, smoking, blood pressure and other metabolic risk factors such as lipids and fasting glucose from routine blood tests to define the 5 groups of ASCVD risk, which was feasible and reasonable in large-scale population screening or studies of risk assessment. Furthermore, we had eGFR measurements for 11,746 participants in the InterASIA cohort. The results for ASCVD incidence and cut-off point analysis did not change substantially after the traditional risk stratification included eGFR <60 ml·min−1·1.73 m−2 (data not shown). Finally, the principles of risk estimation and cut-off points derived from the China-PAR equations reflect an attempt to make complex issues simple and accessible, but their simplicity also makes them vulnerable to criticism. The risk classification determined by cut-off points is arbitrary and an easily-applied alternative to ASCVD risk assessment beyond traditional stratification based on the Chinese guidelines on CVD prevention and hypertension management. The health gains from preventive efforts for individuals with different risk levels will warrant further investigation in clinical trials and longer observational studies.
In conclusion, risk assessment is a fundamental component of prevention and management for ASCVD. After determining the distribution of observed 10-year ASCVD risk across traditional risk stratification categories based on the Chinese guidelines on prevention of CVD and hypertension in our cohorts, we proposed a simplified and easily-applied method for classification of individuals into low-, moderate-, and high-risk groups, with cut-off points of <5%, 5–10%, and ≥10% predicted by the China-PAR equations. More aggressive risk factor modification should be required among individuals with predicted high risk. The China-PAR equations are valuable for identification of high-risk individuals, and can be widely applied for self-assessment and primary prevention of ASCVD risk among general populations, as well as potentially used for secondary prevention of CVD in clinical practice in China.
Acknowledgements
This study was supported by grants from the Ministry of Science and Technology of China (2006BAI01A01, 2011BAI09B03, and 2011BAI11B03).
Footnotes
Peer review under responsibility of Chinese Medical Association.
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.cdtm.2016.10.001.
Conflicts of interest
The authors declare that they have no competing interests.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Zhou M., Wang H., Zhu J. Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387:251–272. doi: 10.1016/S0140-6736(15)00551-6. [DOI] [PubMed] [Google Scholar]
- 2.Yang G., Wang Y., Zeng Y. Rapid health transition in China, 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet. 2013;381:1987–2015. doi: 10.1016/S0140-6736(13)61097-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mills K.T., Bundy J.D., Kelly T.N. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–450. doi: 10.1161/CIRCULATIONAHA.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xu Y., Wang L., He J. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310:948–959. doi: 10.1001/jama.2013.168118. [DOI] [PubMed] [Google Scholar]
- 5.Mi Y.J., Zhang B., Wang H.J. Prevalence and secular trends in obesity among Chinese adults, 1991–2011. Am J Prev Med. 2015;49:661–669. doi: 10.1016/j.amepre.2015.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dawber T.R. Summary of recent literature regarding cigarette smoking and coronary heart disease. Circulation. 1960;22:164–166. [PubMed] [Google Scholar]
- 7.Kannel W.B., Dawber T.R., Kagan A., Revotskie N., Stokes J., 3rd Factors of risk in the development of coronary heart disease – six year follow-up experience. The Framingham Study. Ann Intern Med. 1961;55:33–50. doi: 10.7326/0003-4819-55-1-33. [DOI] [PubMed] [Google Scholar]
- 8.Kannel W.B., McGee D., Gordon T. A general cardiovascular risk profile: the Framingham Study. Am J Cardiol. 1976;38:46–51. doi: 10.1016/0002-9149(76)90061-8. [DOI] [PubMed] [Google Scholar]
- 9.Gu D., Gupta A., Muntner P. Prevalence of cardiovascular disease risk factor clustering among the adult population of China: results from the International Collaborative Study of Cardiovascular Disease in Asia (InterAsia) Circulation. 2005;112:658–665. doi: 10.1161/CIRCULATIONAHA.104.515072. [DOI] [PubMed] [Google Scholar]
- 10.Ezzati M., Lopez A.D., Rodgers A. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–1360. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 11.Goff D.C., Jr., Lloyd-Jones D.M., Bennett G. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 suppl 2):S49–S73. doi: 10.1161/01.cir.0000437741.48606.98. [DOI] [PubMed] [Google Scholar]
- 12.Liu J., Hong Y., D'Agostino R.B., Sr. Predictive value for the Chinese population of the Framingham chd risk assessment tool compared with the Chinese multi-provincial cohort study. JAMA. 2004;291:2591–2599. doi: 10.1001/jama.291.21.2591. [DOI] [PubMed] [Google Scholar]
- 13.Wu Y., Liu X., Li X. Estimation of 10-year risk of fatal and nonfatal ischemic cardiovascular diseases in Chinese adults. Circulation. 2006;114:2217–2225. doi: 10.1161/CIRCULATIONAHA.105.607499. [DOI] [PubMed] [Google Scholar]
- 14.Yang X., Li J., Hu D. Predicting the ten-year risk of atherosclerotic cardiovascular disease in Chinese population: the China-PAR project. Circulation. 2016 [Epub ahead of print] [Google Scholar]
- 15.Chinese Society of Cardiology Chinese guideline on prevention of cardiovascular disease. Zhonghua Xin Xue Guan Bing Za Zhi. 2011;39:3–22. [in Chinese] [PubMed] [Google Scholar]
- 16.Revision Committee for Chinese Guideline on Hypertension Management in Primary Health-care Clinics Chinese guideline on hypertension management in primary health-care Clinics (2014 Revised Edition) Zhonghua Jian Kang Guan Li Xue Za Zhi. 2015;9:10–30. [in Chinese] [Google Scholar]
- 17.Alpert J.S., Thygesen K., Antman E., Bassand J.P. Myocardial infarction redefined – a consensus document of the Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;36:959–969. doi: 10.1016/s0735-1097(00)00804-4. [DOI] [PubMed] [Google Scholar]
- 18.Stone N.J., Robinson J.G., Lichtenstein A.H. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 suppl 2):S1–S45. doi: 10.1161/01.cir.0000437738.63853.7a. [DOI] [PubMed] [Google Scholar]
- 19.Piepoli M.F., Hoes A.W., Agewall S. 2016 European guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR) Eur Heart J. 2016;1(37):2315–2381. doi: 10.1093/eurheartj/ehw106. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.