To the editor:
The Non-steroidal antiinflammatory drugs (NSAIDs) are one of the most widely prescribed drugs, commonly used for rheumatoid diseases and illnesses accompanied by pain. However, the use of NSAIDs is often limited by the gastrointestinal toxicity. The NSAIDs inhibit cyclooxygenase (COX), which is an enzyme in the prostaglandin synthetic pathway, thereby decreasing pain, fever, and inflammation. The likely reason for toxicity is that gastric cytoprotection resulting from prostaglandin is decreased.1 The most common adverse effects of ibuprofen are gastrointestinal symptoms, such as nausea, vomiting, abdominal pain, gastric ulcers, and gastrointestinal bleeding. This is the report of an unusual case of an esophageal ulcer induced by ibuprofen tablets.
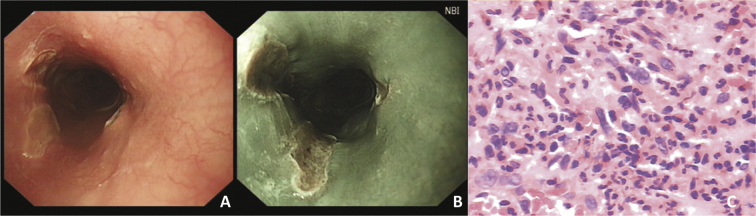
A 32-year-old woman visited our institute due to retrosternal pain. She suffered from dysmenorrheal and took three tablets (0.2 g/tablet) of ibuprofen at one time without drinking water. About two minutes later she felt a severe retrosternal burning sensation that lasted for two minutes, then she felt relief. But she still had retrosternal burning pain and dysphagia after eating. Prior to this problem, the patient was in good health and had no history of gastrointestinal disease or coronary heart disease. Physical examination results included; blood pressure 110/70 mmHg, pulse rate 70/min, there was no conjunctival congestion, rash nor oral ulcer. No particular findings were observed regarding respiration and circulation. Laboratory test results; autoantibody (−), ECG (−), chest CT (−), colonoscopy (−). Gastroscopy found three parallel longitudinal ulcers covered by a small amount of white coating and clear boundaries observed in the mid esophagus (Fig. 1A). Narrow Band Imaging (NBI) showed normal intraepithelial papillary capillary loops (IPCL) and a pit pattern in the esophageal ulcers (Fig. 1B). Biopsy specimens obtained from the margins of the ulcer revealed inflammatory changes (Fig. 1C). The treatment proposed stopping the oral administration of ibuprofen and take 20 mg omeprazole per day. The symptoms disappeared within one week. After two weeks, symptoms greatly decrease. No abnormalities were observed under gastroscopy after three months, and no similar symptoms were seen again in the following year. The final diagnosis was concluded as simple esophageal ulcer.
Fig. 1.
(A) Three parallel longitudinal ulcers covered by a small amount of white coating and clear boundaries observed in the mid esophagus; (B) Normal intraepithelial papillary capillary loops and a pit pattern in the esophageal ulcers; (C) Inflammatory changes (HE).
It has been recognized that both the efficacy and toxicity of NSAIDs result from their inhibition of COX, which primarily has two structurally and functionally distinct isoforms, COX-1 and COX-2. The COX-1 is the constitutive isoform expressed throughout the body and plays an important role in gastrointestinal protection and platelet aggregation. While COX-2 is an inducible COX that is involved in the inflammatory response. Strong evidence indicates that COX-2 inhibitors are associated with significantly lower incidence of gastrointestinal adverse effects than nonselective NSAIDs.2, 3
Ibuprofen belongs to nonselective NSAIDs, so it easily induces gastrointestinal harm. Some reports had illustrated that gastric ulcers could be induced by ibuprofen.4, 5 Our patient was prescribed omeprazole once daily for a short-term, and the esophageal ulcer disappeared. Moreover, there was no recurrence observed during one year. Given the ulcer characteristics and healing process, the lesion was mainly due to entrapment of the tablet and/or its mucosal lesion. The patient had no upper gastrointestinal (GI) symptoms before taking ibuprofen, and the retrosternal pain appeared after taking the ibuprofen. The patient was cured by discontinuing ibuprofen intake, and taking proton pump inhibitor (PPI). It was considered that the esophageal ulcer was induced by ibuprofen.
In conclusion, this is a report of an unusual case of esophageal ulcer induced by ibuprofen tablets. In the current report, the ulcer was in the esophageal second physiological narrow, indicating that it may involve the spasm of the esophagus. In addition, the patient did not drink water while taking ibuprofen tablets. The best approach to management is to remove or reduce exposure to NSAIDs whenever possible. The newer NSAIDs (cyclo-oxygenase [COX]-2-selective inhibitors) have a much lower risk of inducing endoscopic ulcers and minimal platelet effects, which are likely to translate into lower risk of GI complications.
Footnotes
Peer review under responsibility of Chinese Medical Association.
Contributor Information
Xiao-Ling Xu, Email: sbyy_xxl@163.com.
Jian Yin, Email: woshiyisheng_1980@163.com.
References
- 1.A Argentieri J., Morrone K., Pollack Y. Acetaminophen and Ibuprofen overdosage. Pediatr Rev. 2012;33:188–189. doi: 10.1542/pir.33-4-188. [DOI] [PubMed] [Google Scholar]
- 2.Brown T.J., Hooper L., Elliott R.A. A comparison of the cost effectiveness of five strategies for the prevention of non-steroidal anti-inflammatory drug-induced gastrointestinal toxicity: a systematic review with economic modelling. Health Technol Assess. 2006;10 doi: 10.3310/hta10380. 1–183. [DOI] [PubMed] [Google Scholar]
- 3.Yang M., Wang H.T., Zhao M. Network meta-analysis comparing relatively selective COX-2 inhibitors versus coxibs for the prevention of NSAID-induced gastrointestinal injury. Med Baltim. 2015;94:e1592. doi: 10.1097/MD.0000000000001592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lanza F.L., Royer G.L., Nelson R.S. Effect of acetaminophen on human gastric mucosal injury caused by ibuprofen. Gut. 1986;27:440–443. doi: 10.1136/gut.27.4.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Laine L., Kivitz A.J., Bello A.E. Double-blind randomized trials of single-tablet ibuprofen/high-dose famotidine vs. ibuprofen alone for reduction of gastric and duodenal ulcers. Am J Gastroenterol. 2012;107:379–386. doi: 10.1038/ajg.2011.443. [DOI] [PMC free article] [PubMed] [Google Scholar]