Abstract
Background
Adjustment disorder with anxiety (ADA) is the most frequent and best characterized stress-related psychiatric disorder. The rationale for prescription of benzodiazepine monotherapy is a public health issue. Cognitive behavioral stress management programs have been studied in many countries. Several reports have shown beyond reasonable doubt their efficiency at reducing perceived stress and anxiety symptoms and improving patient quality of life. Considering the number of people who could benefit from such programs but are unable to access them, self-help programs have been offered. First presented as books, these programs became enriched with computer-based and digital supports. Regrettably, programs for stress management based on cognitive behavioral therapy (CBT), both face-to-face and digital support, have been only minimally evaluated in France. To our knowledge, the Seren@ctif program is the first French language self-help program for stress management using digital supports.
Objective
The aim of this study is to assess the effectiveness of a 5-week standardized stress management program for reducing anxiety conducted via eLearning (iCBT) or through face-to-face interviews (CBT) with patients suffering from ADA compared with a wait list control group (WLC). These patients seek treatment in a psychiatric unit for anxiety disorders at a university hospital. The primary outcome is change in the State Trait Anxiety Inventory scale trait subscale (STAI-T) between baseline and 2-month visit.
Methods
This is a multicenter, prospective, open label, randomized controlled study in 3 parallel groups with balanced randomization (1:1:1): computer-based stress management with minimal contact (not fully automated) (group 1), stress management with face-to-face interviews (group 2), and a WLC group that receives usual health care from a general practitioner (group 3). Programs are based on standard CBT principles and include 5 modules in 5 weekly sessions that include the following topics: stress and stress reaction and assessment; deep respiration and relaxation techniques; cognitive restructuring, mindfulness, and acceptance; behavioral skills as problem solving; and time management, healthy behaviors, and emotion regulation. In the Internet-based group, patients have minimal contact with a medical professional before and after every session. In the first session, a flash memory drive is supplied containing videos, audio files, a self-help book portfolio in the form of an eGuide, and log books providing the exercises to be completed between 2 sessions. The patient is encouraged to practice a 20-minute daily exercise 5 or 6 times per week. In the face-to-face group, patients receive the same program from a therapist with 5 weekly sessions without digital support. Interviews and self-assessments were collected face-to-face with the investigator.
Results
The feasibility of this program is being tested, and results show good accessibility in terms of acceptance, understanding, and treatment credibility. Results are expected in 2018.
Conclusions
To our knowledge, this is the first French study to examine the effectiveness of a computer-based stress management program for patients with ADA. The Seren@ctif program may be useful within the framework of a psychoeducative approach. It could also be advised for people suffering from other diseases related to stress and for people with a clinical level of perceived stress.
Trial Registration
Clinicaltrials.gov NCT02621775; https://clinicaltrials.gov/ct2/show/NCT02621775 (Archived by WebCite at http://www.webcitation.org/6tQrkPs1u)
Keywords: computer-assisted therapy, eHealth, cognitive therapy, behavior therapy, psychological stress, adjustment disorders, randomized controlled trial
Introduction
Background
Numerous studies have shown that exposure to a stressor increases the risk of psychiatric symptoms and disorders, especially anxiety. When anxiety symptoms are at a higher level than a normal reaction to a stressful event, we consider the possibility of a diagnosis of adjustment disorders, which are classified as stress-related disorders. They are responsible for significant direct and indirect costs from treatment, work stoppages, and loss of productivity [1].
Adjustment Disorder With Anxiety
Definition
Adjustment disorder with anxiety (ADA) is the most frequent and best characterized stress-related psychiatric disorder [2]. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), a diagnosis of ADA is appropriate with the finding of anxiety occurring within 3 months of a psychosocial stressor or life event (eg, divorce, job loss, serious physical illness) [3] with symptoms generally abating by 6 months after the event. Considered a common disorder ranging from mild to moderate intensity, ADA is a true diagnostic entity. A general medical study showed that the level of anxiety is comparable to that of other anxiety disorders such as generalized anxiety disorder [4].
Current Recommendations for Adjustment Disorder With Anxiety
Patients are generally not treated with a tailored approach but with medication, mainly benzodiazepine monotherapy. Benzodiazepine misuse is a public health problem. Although stress management is considered the most appropriate psychological treatment for ADA, the evidence base for this approach is limited [5] . However, several studies compared cognitive behavioral therapy (CBT) with other treatments for generalized anxiety disorders and found greater improvements in stress and anxiety symptoms from CBT. In a study comparing CBT with relaxation, a posttreatment progression for State-Trait Anxiety Inventory scale (STAI-T trait subscale) scores from 53.04 to 46 and for Penn State Worry Questionnaire (PSWQ) scores from 61 to 51.13 were shown for the group that received CBT [6]. A study comparing psychodynamic psychotherapy with CBT found a greater improvement in the symptoms of stress and anxiety for the CBT intervention (a posttreatment progression of STAI-T trait subscale scores from 58.83 to 43.41 and of PSWQ scores from 63.48 to 49.86 in this group) [7]. In addition, eMental health options are considered uniquely suited for offering early intervention after patients experience stressful life events that can potentially trigger adjustment disorders [8].
Development of Preventive and Curative Measures for Adjustment Disorder With Anxiety
It seems legitimate, given the prevalence and the human, economic, and social costs of this pathology linked to stress, to develop preventive and curative measures for ADA. It is not always possible to intervene upstream to reduce the exposure to stress and prevent the occurrence of ADA (primary prevention). Secondary and tertiary prevention measures are therefore useful to limit their consequences.
Stress and Anxiety Management
Stress management is a set of educational and psychotherapeutic measures that combines several cognitive behavioral techniques. The aim is to allow the patient to reach a satisfactory level of emotional and cognitive control and cope with stressors in order to reduce the negative consequences. The common practice is to offer group sessions or individual interviews in the form of a structured module limited in time [9].
Cognitive Behavioral Therapy
CBT has been shown to be an effective treatment for reducing anxiety symptoms in various somatic pathologies such as cardiovascular disease [10,11], diabetes [12], chronic fatigue syndrome [13], and breast cancer [14] and in subjects with high levels of perceived stress or anxiety or burnout, particularly in the workplace [15]. A meta-analysis by Richardson and Rothstein [16] showed a moderate effect size (d=0.53) of stress management programs in the context of work, which is considered an average effect size according to the Cohen criteria [17]. For structured programs based on CBT, the effect is clearly greater (d=1) [9].
Self-Help Therapy
Given that many patients do not have any access to stress and anxiety management programs, therapeutic education modules based on guides and self-help books have been offered and have shown positive results compared with classical CBT programs and control groups [18,19].
Digital Stress Management
In recent years, the development of new technologies has enriched self-help programs by integrating new tools (CD-ROM, flash memory drive, or directly accessible on the Internet), allowing better interactivity and use other than contact with the therapist for patients [20].
These computer-assisted programs are intended to limit the amount of contact time with a mental health professional [21-23]. They have been evaluated in many countries in general, student, and corporate populations [24-36]. Unfortunately, computer-assisted programs have not been evaluated in France.
Recently, a meta-analysis evaluating the effect sizes of 26 computer- and Internet-based interventions was conducted on psychological stress and found significant results in terms of reduction of symptoms of stress (Cohen d=0.43, 95% CI 0.31-0.54), depression (Cohen d=0.34, 95% CI 0.21-0.48), and anxiety (Cohen d=0.32, 95% CI 0.17-0.47) compared to other types of interventions. These results provide evidence that Web- and computer-based stress management interventions can be effective and have the potential to reduce stress-related mental health problems on a large scale [37].
Development of the Seren@ctif Program
It was in this context that Seren@ctif, a computer-based self-help management program, was developed at Lille University Hospital. It is the first French CBT program using digital support (iCBT). Seren@ctif is a neologism formed from 2 French words: seren for serenité, which means serenity, and actif, which means active and refers to self-help. The words are joined with an “at” sign to indicate the use of a digital format.
A pilot study was carried out between January and June 2014 to study the feasibility of this therapeutic program [38]. The results are satisfactory (average scores for satisfaction questionnaires were high, with scores ranging from 4 to 5 on a 5-point Likert scale). These results were the reason why it seemed appropriate to go further by evaluating this program in a controlled manner.
Aims of the Study
The primary objective of this study is to assess the effectiveness of our stress management program conducted via e-learning (iCBT) or through face-to-face sessions compared with a wait list control (WLC) to reduce the anxiety level after 2 months in patients with a diagnosis of ADA.
The primary outcome is the change in the STAI-T score between the baseline and the 2-month visits.
The secondary objectives of this study are as follows:
Evaluate the maintenance of effectiveness of the 2 therapeutic stress management programs (iCBT and CBT) at 6 months
Compare the change in stress, worry, anxiety, and depressive symptoms in the 2 therapeutic programs at 2 and 6 months
Measure the impact of the 2 therapeutic programs on the consumption of tobacco, alcohol, and drugs
Assess overall satisfaction with the 2 therapeutic programs at 2 and 6 months and with the WLC at 6 months
The secondary outcome measures include the following:
Change in STAI-T scores at 6 months
Hospital Anxiety Depression Scale (HADS) anxiety subscale scores at 2 and 6 months
Worry symptoms evaluated by the PSWQ
Stress level evaluated by the Perceived Stress Scale (PSS) and the Visual Analog Scale–stress (VAS-stress) at 2 and 6 months
Depressive symptoms evaluated by the Beck Depression Inventory (BDI) and the HADS depression subscale at 2 and 6 months
Overall satisfaction evaluated by the VAS-satisfaction at 2 and 6 months for the 2 therapeutic groups and at 6 months for the WLC group
Change in consumption of tobacco, alcohol, and drugs evaluated at 2 and 6 months
Hypotheses
We hypothesize that (1) both therapeutic programs will have a greater clinical impact on the reduction of anxiety symptoms, perceived stress, and depressive symptoms compared with a WLC in the short term (2 months), and this effect will be maintained in the long term (6 months); (2) the 2 therapeutic programs will have the same effectiveness in reducing these symptoms; (3) both therapies will be more cost effective than will WLC; (4) these 2 programs both reduce the consumption of tobacco, alcohol, and drugs compared with WLC; and (5) participants will be satisfied with the 2 therapeutic programs.
Choice of Comparators
The comparison with the program implemented face-to-face is intended to highlight the value of eLearning, and the comparison with the control group, whose members receive general medical care, is intended for comparison with the current recommendations for therapeutic studies.
Prospect of the Project
The future goal of this project is to enrich the program with new information and communication technologies, such as the Internet (eCBT) [39-41] and mobile (mCBT) options [42-45], and propose the program to a large population for prevention of stress-related disorders.
Methods
Setting and Procedure
Type of Study
It is a multicenter, comparative, prospective, unblinded, randomized, controlled study in 3 parallel groups. As it is not possible to mask the different treatment groups, patients were not blinded from their intervention group.
Ethics
The project was approved by the local ethics committee, Comité de Protection des Personnes Nord Ouest IV (approval number CPP 15/12), as is required for medical intervention research in France. Data processing will be carried out in accordance with the requirements of the Commission Nationale de l’Informatique et des Libertés reference methodology, MR 06001 (Multimedia Appendix 1).
Recruitment
The study is being conducted at 3 university hospitals (Lille, Amiens, Caen) in the northwest area of France as part of the university communities (InterRégional). Patients are referred by their general practitioner to a psychiatric consultation service for psychological treatment of anxiety symptoms in a context of recent stress. To improve recruitment, general practitioners in the 3 areas were informed of the study by a local investigator during continuing medical education, during scientific meetings, and through all types of collaborative contacts between primary care and psychiatry services. We also directly informed the general practitioners who were involved in previous research on ADA and CBT and invited them to refer patients.
Agreement of the Subjects
During a medical interview, participants will receive oral and written information detailing the progress of the trial and be allowed a period of reflection. Informed consent will be collected from each subject before they enter the study (Multimedia Appendix 2).
Criteria for Discontinuing Participation in the Study
Participants are told they are free to leave the study at any time. Participants will be released from the study by the investigator in cases of adverse events such as diagnosis of an illness requiring hospitalization or surgery, beginning a new medication, or changing medication doses. The current research does not involve any risk, with the exception of the possible negative psychological impact of completing the psychological questionnaires.
Eligibility
Each newly referred patient is asked to answer the optional adjustment disorder section of the Mini International Neuropsychiatric Interview (MINI) [46], French version [47], to confirm he or she meets to the ADA criteria according the DSM-5. The MINI is administered during a face-to-face interview by clinical investigators who are trained in psychiatry. See Textbox 1 for selection criteria for study subjects.
Selection criteria.
Inclusion criteria:
Ambulatory patient (as inpatients are frequently a mixed anxiety depressive type of adjustment disorder)
Male or female aged 18 to 60 years (we use a cutoff age of 60 years for inclusion to limit chronic somatic comorbidities)
Diagnosis of adjustment disorder with anxiety (ADA) according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition criteria
Currently not supported by structured psychotherapeutic treatment for ADA or any other problem
Taking no new psychotropic drug therapy or stabilized for at least 3 months (in the latter case, the patient will be informed of the need to keep the same dosages for the duration of the study)
Minimum score on the Hospital Anxiety and Depression scale (HADS) anxiety subscale greater than or equal to 10 and a maximum score on the HADS depression subscale of less than 10
Access to a computer
Exclusion criteria:
Inability to read or use a computer with support (the platform is easy-to-use and a nurse is available to guide the patient in the navigation of the computer program)
Pregnancy (as recommended by the French ethics committee; urine pregnancy test performed on female patients)
Not capable of consenting, not having legal protection, or being deprived of liberty
Diagnosis of another psychiatric disorder (according to the Mini International Neuropsychiatric Interview)
Randomization
Immediately after inclusion and assessment, patients are randomly allocated in a 1:1:1 ratio into 3 groups using a Web-based central randomization: patients using a digital stress management module (group 1), patients following the stress management module guided by a therapist in attendance (group 2), and patients on a waiting list and benefiting from usual care through their attending physician (group 3).
The randomization sequence is provided by an independent statistician (who does not take part in assessing the patients at any point in the study) using computer-generated random numbers with block sizes of 6 and center stratification consistent with the Consolidated Standards of Reporting Trials (CONSORT) [48]. The randomization sequence is implemented in the electronic case report form (eCRF) system to ensure a centralized, real-time randomization procedure.
A document describing the randomization procedure is kept confidential in the Clinical Investigation Centre of Lille University Hospital.
Assessments
Assessments are conducted for the 3 groups at baseline, 2 months, and 6 months. At baseline, participants complete the self-administered questionnaires for anxiety and depressive symptoms, and care contacts and medications are recorded. At 2 and 6 months, an evaluation of overall satisfaction as well as adverse events is additionally carried out. Self-assessments are collected in the face-to-face sessions with the investigator.
It is the same psychiatrist investigator for each site who generated the random allocation sequence, enrolled the participants, assigned the participants to the interventions, and assessed the participants, so he is not blinded to the intervention group.
The flowchart in Figure 1 summarizes the experimental design.
Figure 1.
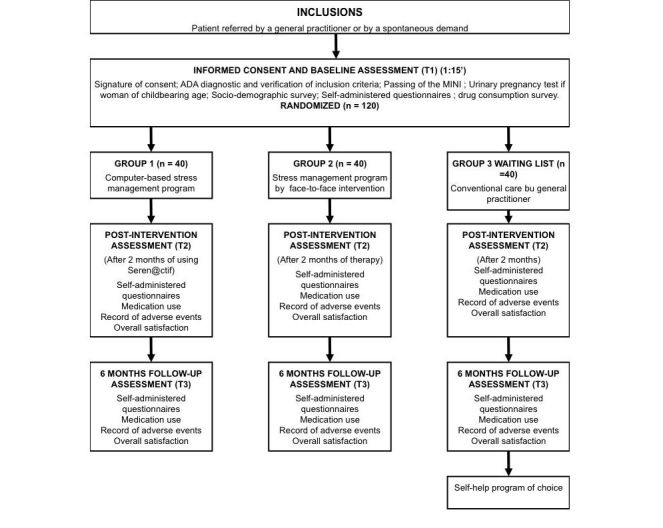
Flowchart of the study.
Interventions
The content of the 2 programs is identical; one is delivered by computer and the other face-to-face. The details of the programs are presented in Table 1.
Table 1.
Seren@ctif content.
| Module theme | Aims of the module | Content of the module |
| Introduction and education regarding stress and anxiety |
Provide psychoeducation about stress and anxiety and their treatment; identify anxiety symptoms and discuss treatment goals and expectations. | Psychoeducation about stress and anxiety (the model of the cognitive emotional stress spiral from a concrete example of stressful situations in everyday life); query about anxiety symptoms, treatment goal and expectations. Daily exercise: anxiety monitoring. |
| Body relaxation | Introduce different relaxation techniques and their respective targets and learn to practice them. | Different relaxation techniques: deep breathing, progressive muscle relaxation, and imagery and their relevance to stressful situations. Daily exercise: podcasts. |
| Cognitive therapy | Introduce the concept of changing thoughts; explain common thinking errors, alternative thoughts, and coping statements; practice. | Cognitive work on automatic thoughts based on concrete situations in everyday life; rationalization of the content of thoughts through cognitive restructuring and identification of repetitive negative ruminations. Daily exercise: identify dysfunctional automatic thoughts and search for other less stressful thoughts. |
| Mindfulness | Understand the interest in accepting rather than repressing emotions to focus attention on the present moment; focus on sensations to relieve negative thoughts and sensations. |
Direct attention to breathing and bodily sensations to overcome stressful thoughts and accept the world and its surrounding thoughts. Daily exercise: podcasts. |
| Exposure and developing positive attitudes | Introduce the concept of changing behavior and practice it. | Principles of problem-solving, exposition, time management, planning pleasant activities, developing empathy, better assertiveness, exercise of full consciousness by concentration on the present moment. |
Computer-Based Stress Management Program
The program includes 5 weekly sessions lasting 1 hour that patients follow from a program accessible on a computer in our unit.
Participants have minimal contact with a clinician to encourage adherence and engagement with the program. This minimal contact of 5 minutes is performed before and after every session by a trained nurse, who investigates the adverse events and drug dose changes since the last session, answers any questions, discusses the progress of the session, and possibly guides participants in the navigation of the computer program.
To avoid connection problems, a flash memory drive is supplied to the participant at the first session that contains videos, audio files, self-help books, a portfolio in the form of an eGuide, and a log book with the program of exercises to be completed between 2 successive sessions of the program. The patient is encouraged to practice 1 or several daily exercises for 20 minutes each, 5 or 6 days per week (Multimedia Appendix 3).
Stress Management by Face-to-Face Interviews
The program includes 5 weekly sessions lasting 45 minutes or 1 hour with trained clinical psychologists (graduate of a master’s program in cognitive and emotional therapy with a minimum of 1 year of practice in CBT and cognitive behavioral stress management). Information, exercises, and homework assignments are delivered by the therapist without self-help support. At the beginning of each session, the therapist asks the participant about adverse events and changes in drug doses since the last session.
Wait List Control
Control group patients received usual care consisting of contact with their general practitioner and nonspecific psychoeducation about stress and anxiety. Medication is prescribed as a stable dose during the period prior to assessment at 2 months.
Outcome Measures
We used the French version of self–report measures for which reliability and validity have been demonstrated.
Anxiety
Spielberger State Trait Anxiety Inventory (STAI)–Form Y Trait version [49]. The French adaptation by Bruchon-Schweitzer and Paulhan [50] is a 20-item questionnaire with 4 levels of ratings from 1=not at all to 4=much (total score of 20 to 80) that captures how the subjects feel generally (9 reversed items).
Hospital Anxiety and Depression Scale (HADS). This questionnaire queries anxiety and depressive disorders using 14 items rated on a 0 to 3 scale with 7 questions relate to anxiety (total A). A score between 8 and 10 on each of the subscales is considered a risk (possible or probable) of anxiety or depressive disorders [51]. The French version is used [52].
Penn State Worry Questionnaire (PSWQ). This is a self-assessment questionnaire consisting of 16 items measuring the general tendency to worry with answers based on a 5-point Likert scale ranging from 1=not at all characteristic to 5=extremely characteristic (scores range from 16 to 80) [53]. A French version of the PSWQ is used [54].
Stress
Perceived Stress Scale (PSS) comes from the stress transactional model and contains 14 items. The total score ranges from 0 to 56, and higher scores represent higher stress levels. Two dimensions emerge from this scale: perceived threat and perceived personal effectiveness [55]. The French version is used [56].
Visual analog scale of stress (VAS-stress) is often used to measure the intensity of various symptoms, especially pain. It was used for the first time in 1996 for a subjective assessment of stress. The simplest VAS scale is a horizontal segment whose ends are defined as the limits of the parameter to be measured, oriented from the best to the worst. A study found external validity for the French version of VAS-stress by comparing its scores with the PSS, and it has a good sensitivity/specificity ratio [57].
Depression
Abbreviated Beck Depression Inventory (BDI) is a self-assessment questionnaire measuring the severity of depression with 13 items rated from 0 to 3 [58,59].
Hospital Anxiety and Depression Scale (HADS) assesses anxiety and depressive disorders using 14 items rated 0 to 3 with 7 questions relative to depressive symptoms (total D). A score between 8 and 10 on each of the subscales is considered a risk (possible or probable) of anxiety or depressive disorders [52].
Interview for Diagnosis of Psychiatric Disorders
The Mini International Neuropsychiatric Interview Version 5.0.0 (MINI) is a fully structured diagnostic interview that assesses a major axis for the diagnosis of disorders [46]. Each newly referred patient was asked to answer the optional adjustment disorder section of the MINI from the French version [47]. The MINI was administered by research assistants who were trained to established reliability criteria. Any participant who met diagnostic criteria for a DSM-5 Axis I diagnosis was excluded from the study. There was no major change between DSM-IV and DSM-5 for anxiety and depressive disorders.
Satisfaction
The visual analog scale of satisfaction (VAS-satisfaction) measures the overall satisfaction with the program.
Main Criterion
The change in the STAI scale between baseline and the 2-month visit was the main criterion. We chose this criterion because it is a self-report measure, and self-report is commonly used in CBT and seems particularly indicated for Internet-based interventions [60]. In addition, the trait of anxiety is the core of a diagnosis of ADA, and the STAI-T measures the trait of anxiety, which is distinguished from a state of anxiety. The HADS scale and the Hamilton Anxiety Rating scale do not make this distinction.
Secondary Criteria
Change in the STAI scale between baseline and the 6-month visit
Changes in other validated self-report measures of anxiety and worry at 2 and 6 months (HADS anxiety subscale, PSWQ)
Changes in validated self-report measures of stress at 2 and 6 months (VAS-stress, PSS)
Changes in validated self-report measures of depression at 2 and 6 months (BDI, HADS depression subscale)
Consumption of tobacco (number of cigarettes smoked per day), alcohol (number of drinks of alcohol per week—in France, the standard drink contains 10 grams of alcohol) and drug use (days per week for each product) at 2 and 6 months
VAS-satisfaction at 2 and 6 months for the 2 therapeutic groups and at 6 months for the WLC group
Sample Size
In a study on the clinical and psychometric characteristics of ADA, the mean (standard deviation) of the STAI baseline score was 52.1 (SD 14.6) [4]. Two clinical studies with patients with generalized anxiety disorder, 1 comparing CBT with relaxation [61] and the other comparing CBT with brief psychodynamic psychotherapy [62], showed changes in the STAI-T scores of 7 and 16, respectively. In view of these results, we hypothesize that an average difference between each experimental arm and the control arm of 11.5 (the mean of 7 and 16). To demonstrate this difference in variation with a standard deviation of the STAI score change of 14.6 (assuming a conservative correlation coefficient of 0.5 between the baseline and 2-month STAI measures), a 2.5% type I error (using a Bonferroni correction for the 2 prespecified comparisons), and a power of 80%, it is necessary to include 32 patients per group. Although analysis of the primary outcome will be adjusted for baseline values, the sample size calculation does not take into account this adjustment to maximize the power. Finally, considering 20% missing data, 120 patients (40 per group) are planned in this clinical trial.
Data Collection and Management
Data are recorded in an eCRF developed using Clinsight (Ennov Inc). The eCRF is used for data entry at each investigator site, and every center is responsible for patient anonymization. The eCRF was created, tested, and validated before the start of data entry. The data necessary for monitoring the primary and secondary endpoints are identified and managed at regular intervals throughout the trial. Data are monitored by the data management team of the data management department of University Hospital of Lille using predefined data management rules, and queries are automatically edited. Finally, overall automated monitoring is performed by the data manager at the end of data entry. In case of discrepancies, queries are edited to resolve the problems encountered. After validation, the database is frozen and exported for analysis.
Statistical Analysis
Overview
Statistical analysis will be conducted in a blinded fashion with a blinded code for the intervention. All statistical analyses will be carried out independently in the Department of Biostatistics of the University Hospital of Lille. SAS 9.3 (SAS Institute Inc) software or later will be used. P values will be reported as the actual values, unless P<.001. No interim analyses are planned. A detailed statistical analysis plan (SAP) will be drafted and validated before the database is frozen. Patient characteristics at baseline will be described for each of the 3 arms; the quantitative variables will be described either by the mean and standard deviation in case of a Gaussian distribution or by the median and interquartile range if not. The normality of the distributions will be verified graphically by histograms and by the Shapiro-Wilk test. The qualitative variables will be described by the numbers and percentages of each category. All analyses for the primary and secondary objectives will be performed on all randomized patients in their original group of randomization according to intention-to-treat (ITT) principles. No subgroup analysis will be performed.
Main Objective
Comparison of the primary endpoint (2-month change in STAI scale) between each experimental group and the control group will be performed separately using an analysis of covariance with an adjustment for the STAI baseline value and the center. Since 2 comparisons will be made for the primary analysis, each of them will be performed at the 2.5% significance level (Bonferroni correction). The absolute mean differences and effect sizes (standardized mean difference) will be reported with the 95% confidence interval. In case of deviation from normality of model residuals, nonparametric analysis will be used; absolute changes between baseline and 2-month visits will be calculated and compared between the experimental arm and control arm using nonparametric analysis of covariance adjusted for baseline values [63,64]. The primary analysis will be conducted according to the ITT principle. Missing values will be handled by multiple imputation procedures. Missing data will be imputed under the missing at random assumption using a regression switching approach (chained equation with m=20 imputations) with predictive mean matching method for continuous variables and logistic regression (binary, ordinal, or polynomial) for qualitative variables [65]. The imputation procedure will be performed using the main baseline characteristics, outcome, and variable group of randomization, and multiple imputed data sets will be combined using Rubin’s rules [66,67]. Sensitivity analyses will first be conducted using all available STAI measurements (complete cases analysis) and second in patients without major deviation from protocol (per protocol analysis); major deviations will be specified in the SAP.
Secondary Objectives
For the secondary endpoints of the HADS anxiety subscale, PSWQ, VAS-stress, PSS, BDI, and HADS depression subscale scores, comparisons of the changes between the baseline and the 2-month visit between each experimental group and the control group will be performed separately with the same methodology used for the primary endpoint.
Comparison of the change between the baseline and the 6-month visit for the primary endpoint and secondary endpoints between each experimental group and the control group will be performed separately using a linear mixed model. In this model, we will include the 2 measurements (at 2 and 6 months) for the time effect, the group effect (experimental/control), an adjustment for baseline values and center, and a time × group interaction. A contrast with a 2.5% type I error will be used to compare the 6-month change between the experimental and the control group.
The efficacy of the 2 therapeutic programs (face-to-face versus digital support) at 2 and 6 months will be compared using an analysis of covariance at the 5% significance level to compare the variations in the STAI score between the groups, adjusting for the baseline value.
VAS satisfaction and consumption of tobacco, alcohol, and drug use will be analyzed in each group using descriptive statistics.
The full version of the protocol can be viewed in Multimedia Appendix 4.
Results
Recruitment started in January 2016. The duration of the inclusion period is 24 months, and the duration of research is 3 years (including 6 months for conducting the study with the last patients included and 6 months for data analysis). The final report will be written based on the CONSORT statement [48] and its adaptation for an eHealth trial [68] (Multimedia Appendix 5).
As of this writing, there have been no major changes during the study (eg, staff turnover, equipment breakdowns). We have lost a subject during the protocol. We are currently making an attrition or engagement diagram of the subjects over time that we will include in the final article once we have the results of the study.
To our knowledge, this is the first French study to examine the effectiveness of a computer-based stress management program (CBT) for patients with ADA.
Discussion
The aim of this study is to demonstrate the efficacy of 2 therapeutic programs with 120 patients suffering from ADA and to compare these programs. To date, we have 50 of the required 120 participants (42%).
We can already cite as a limitation that because this is an eHealth study, the participants are not blinded to the treatment group.
Some elements of this randomized controlled trial would be different if it were conducted in routine clinical practice. Indeed, currently, patients come to do their eLearning sessions in consultation, so one can easily control adherence, which we would not be able to do if it were in clinical practice. This adherence is reinforced by minimal contact time with a nurse before each session (which is very short).
In clinical practice, a way to assess and reinforce adherence should be found. This issue is why we plan to improve this program by integrating tools from new information and communication technologies (eCBT, mCBT, eCoaching, telemedicine) and rely on a recent literature review concerning adherence to self-help treatment with digital media [37].
We would propose that the program is not just for the psychiatric population (tertiary prevention) but for a wider population exposed to stress who may suffer from stress-related disorders (primary and secondary prevention).
This program would make it easier to access treatment with the aim of preventing stress, which is not available in France at the present time.
Acknowledgments
The study is sponsored by the University Hospital of Lille. This work was supported by funding from the French Ministry of Health. We thank Pascal Delamillieure from the University Hospital of Caen (France) and Cyrille Guillaumont from the Centre Philippe Pinel of Amiens (France) for approval and joining us in this research project. Our study team would like to thank the Department of Research of the University Hospital of Lille. Special thanks to Anne Laure Demarty and Stephane Duhez for their assistance with this project.
Abbreviations
- ADA
adjustment disorder with anxiety
- BDI
Beck Depression Inventory
- CBT
cognitive behavioral therapy
- eCRF
electronic case report form
- DSM-5
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- HADS
Hospital Anxiety and Depression Scale
- iCBT
CBT program using digital support
- ITT
intention-to-treat
- MINI
Mini International Neuropsychiatric Interview
- PSS
Perceived Stress Scale
- PSWQ
Penn State Worry Questionnaire
- SAP
statistical analysis plan
- STAI-T
State-Trait Anxiety Inventory scale, trait subscale
- VAS-stress
visual analog scale–stress
- WLC
wait list control
Declaration to Commission Nationale de l’Informatique et des Libertés.
Patient information and informed consent.
Screenshots of the Seren@ctif program.
Full version of the protocol.
CONSORT-HEALTH check list.
Footnotes
Authors' Contributions: DS conceived of the study. OB, LR, and GV initiated the study design. AD conducted the statistical analysis. ACL participated in the initial protocol development. ACL, AD, and DS participated in writing the manuscript. All authors read and approved the final manuscript. All authors will be involved in data analysis, interpretation, and future manuscript preparation.
Conflicts of Interest: None declared.
References
- 1.Sauter SL, Murphy LR, Hurrell JJ. Prevention of work-related psychological disorders. A national strategy proposed by the National Institute for Occupational Safety and Health (NIOSH) Am Psychol. 1990 Oct;45(10):1146–1158. doi: 10.1037//0003-066x.45.10.1146. [DOI] [PubMed] [Google Scholar]
- 2.Fernández A, Mendive JM, Salvador-Carulla L, Rubio-Valera M, Luciano JV, Pinto-Meza A, Haro JM, Palao DJ, Bellón JA, Serrano-Blanco A, DASMAP investigators Adjustment disorders in primary care: prevalence, recognition and use of services. Br J Psychiatry. 2012 Aug;201:137–142. doi: 10.1192/bjp.bp.111.096305. http://bjp.rcpsych.org/cgi/pmidlookup?view=long&pmid=22576725. [DOI] [PubMed] [Google Scholar]
- 3.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th Edition. Washington: American Psychiatric Association; 2013. [Google Scholar]
- 4.Servant D, Pelissolo A, Chancharme L, Le Guern M, Boulenger J. [Adjustment disorders with anxiety. Clinical and psychometric characteristics in patients consulting a general practitioner] Encephale. 2013 Oct;39(5):347–351. doi: 10.1016/j.encep.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 5.Casey P. Adjustment disorder: new developments. Curr Psychiatry Rep. 2014 Jun;16(6):451. doi: 10.1007/s11920-014-0451-2. [DOI] [PubMed] [Google Scholar]
- 6.Dugas MJ, Brillon P, Savard P, Turcotte J, Gaudet A, Ladouceur R, Leblanc R, Gervais NJ. A randomized clinical trial of cognitive-behavioral therapy and applied relaxation for adults with generalized anxiety disorder. Behav Ther. 2010 Mar;41(1):46–58. doi: 10.1016/j.beth.2008.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leichsenring F, Salzer S, Jaeger U, Kächele H, Kreische R, Leweke F, Rüger U, Winkelbach C, Leibing E. Short-term psychodynamic psychotherapy and cognitive-behavioral therapy in generalized anxiety disorder: a randomized, controlled trial. Am J Psychiatry. 2009 Aug;166(8):875–881. doi: 10.1176/appi.ajp.2009.09030441. [DOI] [PubMed] [Google Scholar]
- 8.Maercker A, Bachem RC, Lorenz L, Moser CT, Berger T. Adjustment disorders are uniquely suited for eHealth interventions: concept and case study. JMIR Ment Health. 2015;2(2):e15. doi: 10.2196/mental.4157. http://mental.jmir.org/2015/2/e15/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ong L, Linden W, Young S. Stress management: what is it? J Psychosom Res. 2004 Jan;56(1):133–137. doi: 10.1016/S0022-3999(03)00128-4. [DOI] [PubMed] [Google Scholar]
- 10.Turner L, Linden W, van der Wal R, Schamberger W. Stress management for patients with heart disease: a pilot study. Heart Lung. 1995;24(2):145–153. doi: 10.1016/s0147-9563(05)80009-3. [DOI] [PubMed] [Google Scholar]
- 11.Campbell TS, Stevenson A, Arena R, Hauer T, Bacon SL, Rouleau CR, Cannon C, Stone JA. An investigation of the benefits of stress management within a cardiac rehabilitation population. J Cardiopulm Rehabil Prev. 2012;32(5):296–304. doi: 10.1097/HCR.0b013e318265e0eb. [DOI] [PubMed] [Google Scholar]
- 12.Attari A, Sartippour M, Amini M, Haghighi S. Effect of stress management training on glycemic control in patients with type 1 diabetes. Diabetes Res Clin Pract. 2006 Jul;73(1):23–28. doi: 10.1016/j.diabres.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 13.Lopez C, Antoni M, Penedo F, Weiss D, Cruess S, Segotas M, Helder L, Siegel S, Klimas N, Fletcher MA. A pilot study of cognitive behavioral stress management effects on stress, quality of life, and symptoms in persons with chronic fatigue syndrome. J Psychosom Res. 2011 Apr;70(4):328–334. doi: 10.1016/j.jpsychores.2010.11.010. http://europepmc.org/abstract/MED/21414452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nzila N, Laga M, Thiam MA, Mayimona K, Edidi B, Behets F, Hassig S, Nelson A, Mokwa K. HIV and other sexually transmitted diseases among female prostitutes in Kinshasa. AIDS. 1991 Jun;5(6):715–721. doi: 10.1097/00002030-199106000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Bhui KS, Dinos S, Stansfeld SA, White PD. A synthesis of the evidence for managing stress at work: a review of the reviews reporting on anxiety, depression, and absenteeism. J Environ Public Health. 2012;2012:515874. doi: 10.1155/2012/515874. doi: 10.1155/2012/515874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Richardson KM, Rothstein HR. Effects of occupational stress management intervention programs: a meta-analysis. J Occup Health Psychol. 2008 Jan;13(1):69–93. doi: 10.1037/1076-8998.13.1.69. [DOI] [PubMed] [Google Scholar]
- 17.Cohen J. A power primer. Psychol Bull. 1992 Jul;112(1):155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 18.Sharma V, Sood A, Prasad K, Loehrer L, Schroeder D, Brent B. Bibliotherapy to decrease stress and anxiety and increase resilience and mindfulness: a pilot trial. Explore (NY) 2014;10(4):248–252. doi: 10.1016/j.explore.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 19.Abramowitz JS, Moore EL, Braddock AE, Harrington DL. Self-help cognitive-behavioral therapy with minimal therapist contact for social phobia: a controlled trial. J Behav Ther Exp Psychiatry. 2009 Mar;40(1):98–105. doi: 10.1016/j.jbtep.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 20.Andersson G. Using the Internet to provide cognitive behaviour therapy. Behav Res Ther. 2009 Mar;47(3):175–180. doi: 10.1016/j.brat.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 21.Matcham F, Rayner L, Hutton J, Monk A, Steel C, Hotopf M. Self-help interventions for symptoms of depression, anxiety and psychological distress in patients with physical illnesses: a systematic review and meta-analysis. Clin Psychol Rev. 2014 Mar;34(2):141–157. doi: 10.1016/j.cpr.2014.01.005. https://linkinghub.elsevier.com/retrieve/pii/S0272-7358(14)00033-6. [DOI] [PubMed] [Google Scholar]
- 22.Kawai K, Yamazaki Y, Nakayama K. Process evaluation of a Web-based stress management program to promote psychological well-being in a sample of white-collar workers in Japan. Ind Health. 2010;48(3):265–274. doi: 10.2486/indhealth.48.265. http://joi.jlc.jst.go.jp/JST.JSTAGE/indhealth/48.265?from=PubMed. [DOI] [PubMed] [Google Scholar]
- 23.Zetterqvist K, Maanmies J, Ström L, Andersson G. Randomized controlled trial of internet-based stress management. Cogn Behav Ther. 2003;32(3):151–160. doi: 10.1080/16506070302316. [DOI] [PubMed] [Google Scholar]
- 24.Cook RF, Billings DW, Hersch RK, Back AS, Hendrickson A. A field test of a Web-based workplace health promotion program to improve dietary practices, reduce stress, and increase physical activity: randomized controlled trial. J Med Internet Res. 2007;9(2):e17. doi: 10.2196/jmir.9.2.e17. http://www.jmir.org/2007/2/e17/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beatty L, Lambert S. A systematic review of internet-based self-help therapeutic interventions to improve distress and disease-control among adults with chronic health conditions. Clin Psychol Rev. 2013 Jun;33(4):609–622. doi: 10.1016/j.cpr.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 26.Rose RD, Buckey JC, Zbozinek TD, Motivala SJ, Glenn DE, Cartreine JA, Craske MG. A randomized controlled trial of a self-guided, multimedia, stress management and resilience training program. Behav Res Ther. 2013 Feb;51(2):106–112. doi: 10.1016/j.brat.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 27.Clarke J, Proudfoot J, Birch M, Whitton AE, Parker G, Manicavasagar V, Harrison V, Christensen H, Hadzi-Pavlovic D. Effects of mental health self-efficacy on outcomes of a mobile phone and web intervention for mild-to-moderate depression, anxiety and stress: secondary analysis of a randomised controlled trial. BMC Psychiatry. 2014;14:272. doi: 10.1186/s12888-014-0272-1. http://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-014-0272-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ruwaard J, Lange A, Schrieken B, Dolan CV, Emmelkamp P. The effectiveness of online cognitive behavioral treatment in routine clinical practice. PLoS One. 2012;7(7):e40089. doi: 10.1371/journal.pone.0040089. http://dx.plos.org/10.1371/journal.pone.0040089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van Straten A, Cuijpers P, Smits N. Effectiveness of a Web-based self-help intervention for symptoms of depression, anxiety, and stress: randomized controlled trial. J Med Internet Res. 2008;10(1):e7. doi: 10.2196/jmir.954. http://www.jmir.org/2008/1/e7/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grime PR. Computerized cognitive behavioural therapy at work: a randomized controlled trial in employees with recent stress-related absenteeism. Occup Med (Lond) 2004 Aug;54(5):353–359. doi: 10.1093/occmed/kqh077. http://occmed.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=15289593. [DOI] [PubMed] [Google Scholar]
- 31.Heber E, Lehr D, Ebert DD, Berking M, Riper H. Web-based and mobile stress management intervention for employees: a randomized controlled trial. J Med Internet Res. 2016;18(1):e21. doi: 10.2196/jmir.5112. http://www.jmir.org/2016/1/e21/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ahtinen A, Mattila E, Välkkynen P, Kaipainen K, Vanhala T, Ermes M, Sairanen E, Myllymäki T, Lappalainen R. Mobile mental wellness training for stress management: feasibility and design implications based on a one-month field study. JMIR Mhealth Uhealth. 2013;1(2):e11. doi: 10.2196/mhealth.2596. http://mhealth.jmir.org/2013/2/e11/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ebert DD, Lehr D, Heber E, Riper H, Cuijpers P, Berking M. Internet- and mobile-based stress management for employees with adherence-focused guidance: efficacy and mechanism of change. Scand J Work Environ Health. 2016 Sep 01;42(5):382–394. doi: 10.5271/sjweh.3573. [DOI] [PubMed] [Google Scholar]
- 34.Day V, McGrath PJ, Wojtowicz M. Internet-based guided self-help for university students with anxiety, depression and stress: a randomized controlled clinical trial. Behav Res Ther. 2013 Jul;51(7):344–351. doi: 10.1016/j.brat.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 35.Glück TM, Maercker A. A randomized controlled pilot study of a brief Web-based mindfulness training. BMC Psychiatry. 2011;11:175. doi: 10.1186/1471-244X-11-175. http://www.biomedcentral.com/1471-244X/11/175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Frazier P, Meredith L, Greer C, Paulsen JA, Howard K, Dietz LR, Qin K. Randomized controlled trial evaluating the effectiveness of a Web-based stress management program among community college students. Anxiety Stress Coping. 2015;28(5):576–586. doi: 10.1080/10615806.2014.987666. [DOI] [PubMed] [Google Scholar]
- 37.Heber E, Ebert DD, Lehr D, Cuijpers P, Berking M, Nobis S, Riper H. The benefit of Web- and computer-based interventions for stress: a systematic review and meta-analysis. J Med Internet Res. 2017 Feb 17;19(2):e32. doi: 10.2196/jmir.5774. http://www.jmir.org/2017/2/e32/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Servant D, Rougegrez L, Barasino O, Demarty A, Duhamel A, Vaiva G. [Interest of computer-based cognitive behavioral stress management. Feasability of the Seren@ctif program] Encephale. 2016 Oct;42(5):415–420. doi: 10.1016/j.encep.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 39.Mehring M, Haag M, Linde K, Wagenpfeil S, Schneider A. Effects of a Web-based intervention for stress reduction in primary care: a cluster randomized controlled trial. J Med Internet Res. 2016 Feb 12;18(2):e27. doi: 10.2196/jmir.4246. http://www.jmir.org/2016/2/e27/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Drozd F, Raeder S, Kraft P, Bjørkli CA. Multilevel growth curve analyses of treatment effects of a Web-based intervention for stress reduction: randomized controlled trial. J Med Internet Res. 2013;15(4):e84. doi: 10.2196/jmir.2570. http://www.jmir.org/2013/4/e84/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lucini D, Solaro N, Lesma A, Gillet VB, Pagani M. Health promotion in the workplace: assessing stress and lifestyle with an intranet tool. J Med Internet Res. 2011 Nov 08;13(4):e88. doi: 10.2196/jmir.1798. http://www.jmir.org/2011/4/e88/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zarski A, Lehr D, Berking M, Riper H, Cuijpers P, Ebert DD. Adherence to Internet-based mobile-supported stress management: a pooled analysis of individual participant data from three randomized controlled trials. J Med Internet Res. 2016;18(6):e146. doi: 10.2196/jmir.4493. http://www.jmir.org/2016/6/e146/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhu B, Hedman A, Feng S, Li H, Osika W. Designing, prototyping and evaluating digital mindfulness applications: a case study of mindful breathing for stress reduction. J Med Internet Res. 2017 Jun 14;19(6):e197. doi: 10.2196/jmir.6955. http://www.jmir.org/2017/6/e197/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Þórarinsdóttir H, Kessing LV, Faurholt-Jepsen M. Smartphone-based self-assessment of stress in healthy adult individuals: a systematic review. J Med Internet Res. 2017 Feb 13;19(2):e41. doi: 10.2196/jmir.6397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Donker T, Petrie K, Proudfoot J, Clarke J, Birch M, Christensen H. Smartphones for smarter delivery of mental health programs: a systematic review. J Med Internet Res. 2013;15(11):e247. doi: 10.2196/jmir.2791. http://www.jmir.org/2013/11/e247/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59 Suppl 20:22–34. [PubMed] [Google Scholar]
- 47.Lecrubier Y, Sheehan D, Weiller E, Amorim P, Bonora I, Harnett Sheehan K, Janavs J, Dunbar G. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: reliability and validity according to the CIDI. European Psychiatry. 1997;12(5):224–231. doi: 10.1016/S0924-9338(97)83296-8. [DOI] [Google Scholar]
- 48.Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet. 2001 Apr 14;357(9263):1191–1194. [PubMed] [Google Scholar]
- 49.Spielberger C. Manual for the State-Trait Anxiety Inventory (Form Y) Self-Evaluation Questionnaire. Palo Alto: Consulting Psychologist Press; 1983. [Google Scholar]
- 50.Bruchon-Schweitzer M, Paulhan I. In: Inventaire d'anxiété, état-trait: forme Y (STAI-Y) Adaptation française. Spielberger CD, editor. Paris: Les Editions du Centre de Psychologie Appliquée; 1993. [Google Scholar]
- 51.Olssøn I, Mykletun A, Dahl AA. The Hospital Anxiety and Depression Rating Scale: a cross-sectional study of psychometrics and case finding abilities in general practice. BMC Psychiatry. 2005 Dec 14;5:46. doi: 10.1186/1471-244X-5-46. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/1471-244X-5-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lépine JP, Godchau M, Brun P, Lempérière T. [Evaluation of anxiety and depression among patients hospitalized on an internal medicine service] Ann Med Psychol (Paris) 1985 Feb;143(2):175–189. [PubMed] [Google Scholar]
- 53.Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther. 1990;28(6):487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- 54.Gosselin P, Dugas MJ, Ladouceur R, Freeston MH. [Evaluation of worry: validation of a French translation of the Penn State Worry Questionnaire] Encephale. 2001;27(5):475–484. [PubMed] [Google Scholar]
- 55.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983 Dec;24(4):385–396. [PubMed] [Google Scholar]
- 56.Lesage F, Berjot S, Deschamps F. Psychometric properties of the French versions of the Perceived Stress Scale. Int J Occup Med Environ Health. 2012 Jun;25(2):178–184. doi: 10.2478/S13382-012-0024-8. doi: 10.2478/S13382-012-0024-8. [DOI] [PubMed] [Google Scholar]
- 57.Lesage F, Berjot S, Deschamps F. Clinical stress assessment using a visual analogue scale. Occup Med (Lond) 2012 Dec;62(8):600–605. doi: 10.1093/occmed/kqs140. http://occmed.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=22965867. [DOI] [PubMed] [Google Scholar]
- 58.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961 Jun;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 59.Pichot P, Lemperiere T. Analyse factorielle d'un questionnaire d'auto-évaluation des symptômes dépressifs. Revue Psychologie Appliquée. 1964:15. [Google Scholar]
- 60.Olthuis JV, Watt MC, Bailey K, Hayden JA, Stewart SH. Therapist-supported Internet cognitive behavioural therapy for anxiety disorders in adults. Cochrane Database Syst Rev. 2016 Mar 12;3:CD011565. doi: 10.1002/14651858.CD011565.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dugas MJ, Brillon P, Savard P, Turcotte J, Gaudet A, Ladouceur R, Leblanc R, Gervais NJ. A randomized clinical trial of cognitive-behavioral therapy and applied relaxation for adults with generalized anxiety disorder. Behav Ther. 2010 Mar;41(1):46–58. doi: 10.1016/j.beth.2008.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Leichsenring F, Salzer S, Jaeger U, Kächele H, Kreische R, Leweke F, Rüger U, Winkelbach C, Leibing E. Short-term psychodynamic psychotherapy and cognitive-behavioral therapy in generalized anxiety disorder: a randomized, controlled trial. Am J Psychiatry. 2009 Aug;166(8):875–881. doi: 10.1176/appi.ajp.2009.09030441. [DOI] [PubMed] [Google Scholar]
- 63.Vickers AJ. Parametric versus non-parametric statistics in the analysis of randomized trials with non-normally distributed data. BMC Med Res Methodol. 2005 Nov 03;5:35. doi: 10.1186/1471-2288-5-35. https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-5-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Conover WJ, Iman RL. Analysis of covariance using the rank transformation. Biometrics. 1982 Sep;38(3):715–724. [PubMed] [Google Scholar]
- 65.Van Buuren S, Groothuis-Oudshoorn K. MICE: Multivariate Imputation by Chained Equations in R. J Stat Softw. 2011 [Google Scholar]
- 66.Rubin D. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley and Sons; 1987. [Google Scholar]
- 67.Li K, Meng X, Raghunathan T, Rubin D. Significance levels from repeated p-values with multiply-imputed data. Statistica Sinica. 1991;1(1):65–92. [Google Scholar]
- 68.Eysenbach G. CONSORT-EHEALTH: improving and standardizing evaluation reports of Web-based and mobile health interventions. J Med Internet Res. 2011;13(4):e126. doi: 10.2196/jmir.1923. http://www.jmir.org/2011/4/e126/ [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Declaration to Commission Nationale de l’Informatique et des Libertés.
Patient information and informed consent.
Screenshots of the Seren@ctif program.
Full version of the protocol.
CONSORT-HEALTH check list.


