Introduction
Radiofrequency catheter ablation (RFCA) of the cavotricuspid isthmus (CTI) is performed as the first-line treatment for typical atrial flutter (AFL), as CTI ablation has proved to be very effective with a high long-term success rate and a low risk of procedural complications. However, acute coronary artery occlusion is a very rare but potentially life-threatening complication of RFCA.1 There are a few reports on acute right coronary occlusion following CTI ablation and it is speculated that the causes are spasm, edema of the arterial wall, thrombus formation, and/or plaque rupture; however, the mechanism in humans is not fully understood.2 Herein, we describe a new case and the first use of optical frequency domain imaging (OFDI) to evaluate the acute vessel response of a coronary occlusion after CTI ablation.
Case report
A 69-year-old man was referred to our institution for RFCA of a paroxysmal atrial fibrillation and CTI-dependent AFL with the CHADS2 score of 1. Despite taking antiarrhythmic drugs, he presented with palpitations on several occasions. We therefore decided to proceed with isolation of the pulmonary vein and CTI ablation. Coronary angiography revealed that bifurcation of the posterior descending artery and posterolateral artery (PLA) in the proximal right coronary artery (RCA), compared with usual anatomy (Figure 1A).
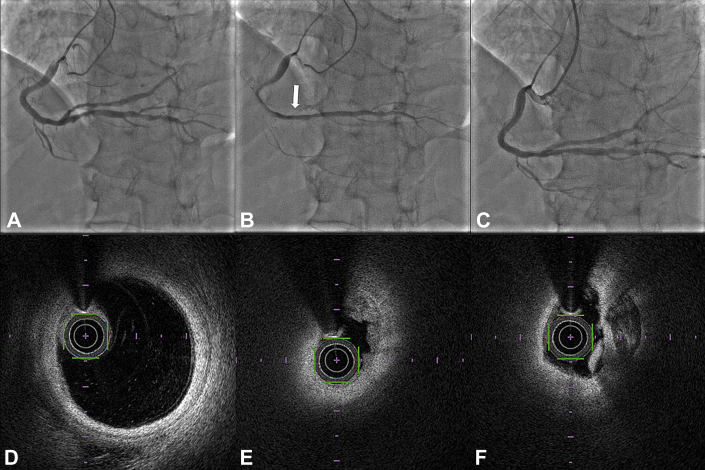
Figure 1.
Coronary angiography (A, B, C) and optical frequency domain imaging (D, E, F). A: Initial angiography. B: An immediate coronary angiography showed an occlusion (white arrow) of the posterolateral branch. C: Final angiography. D: Proximal site maintained a normal “three-layer” structure. E: Optical frequency domain imaging revealed thickening of the intima and thrombus at the target lesion. F: Distal site had fibrous and fibrocalcific plaques.
In the electrophysiology laboratory, we maintained activated clotting time above 300 seconds with intravenous heparin during the procedure. The pulmonary vein isolation was performed with a 4-mm-tip irrigated ablation catheter. CTI ablation was then performed with the same catheter with a maximum power of 35 W and a temperature limit of 42°C. The CTI was successfully ablated. When the patient returned to the ward, ventricular fibrillation was suddenly observed on the monitor. The staff immediately performed defibrillation. The patient’s electrocardiogram showed ST depression in the inferior leads. The echocardiogram revealed hypokinetic wall motion abnormalities in the RCA territory.
An immediate coronary angiography showed occlusion of the ostium of the PLA (Figure 1B). Intracoronary nitroglycerin was administered with no effect. A very small red thrombus was aspirated; however, no reperfusion was obtained. After dilation with a 2.5 mm balloon, OFDI revealed thickening of the intima and thrombus, with an irregular surface, at the target lesion (Figure 1E). OFDI revealed no evidence of plaque rupture either proximal or distal to the occluded point (Figure 1D, F). As the vessel occluded repeatedly a few minutes after balloon dilation, a 3.0 × 30-mm stent was placed and good blood flow was obtained (Figure 1C).
Discussion
To our knowledge, in the present case report, the acute vessel wall injury to the RCA following RFCA of the CTI to treat typical AFL was assessed for the first time in humans by OFDI. OFDI showed vessel wall thickening, thrombus but no evidence of plaque rupture, and spasm at the lesion. This appearance resembles “plaque erosion,” characterized by the presence of thrombi with no plaque rupture and occurring over a lesion with a thick intima.3 Pathologic evaluation of the aspirated thrombus revealed no findings suggestive of plaque rupture. These findings suggest that, as the mechanism of acute coronary occlusion during RFCA, thermal trauma produces wall thickening owing to edema and leads to thrombus formation and vessel occlusion, while the patient is negative for coronary spasm and plaque rupture.
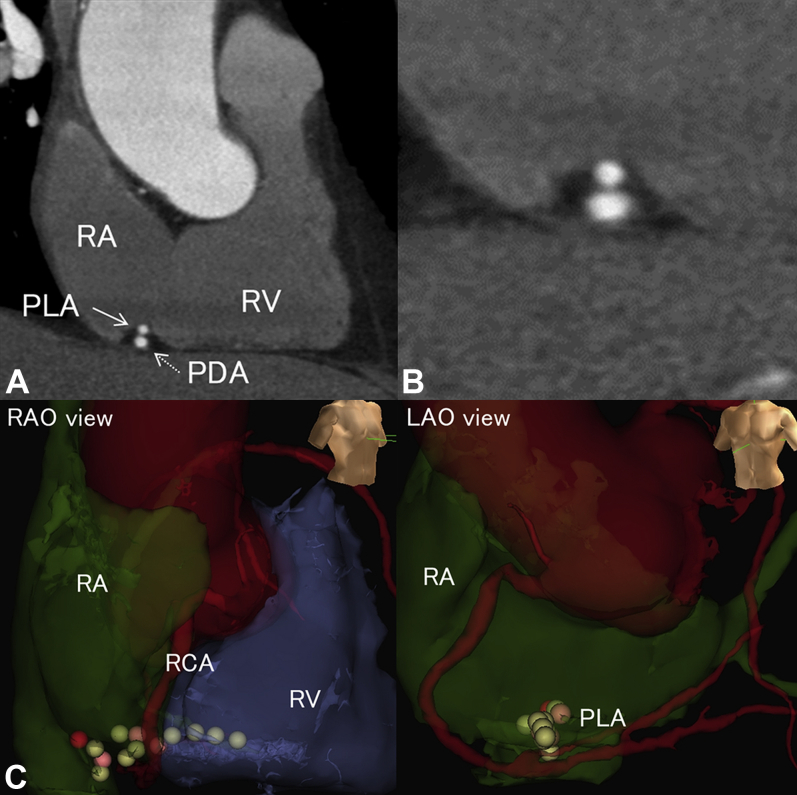
The previous computed tomography showed that the PLA lay in a deeper position in the right atrioventricular groove (Figure 2A, B). The RCA occlusion site was quite close to the ablation site (Figure 2C). This case suggests that the anatomic proximity of the RCA to the CTI should be evaluated before ablation for AFL.
Key Teaching Points.
-
•
Radiofrequency catheter ablation (RFCA) of the cavotricuspid isthmus (CTI) is performed as the common treatment for typical atrial flutter (AFL); however, acute coronary artery occlusion is a very rare but potentially life-threatening complication of RFCA.
-
•
Optical frequency domain imaging (OFDI) to evaluate the acute vessel response of a coronary occlusion after CTI ablation revealed vessel wall thickening and thrombus but no evidence of plaque rupture at the lesion. The mechanism of acute coronary occlusion after RFCA is speculated that thermal trauma produces wall thickening owing to edema and leads to thrombus formation and vessel occlusion.
-
•
The anatomic proximity of the right coronary artery to the CTI should be evaluated before ablation for AFL to avoid this complication.
Figure 2.
A: Computed tomography (CT) image. PDA = posterior descending artery; PLA = posterolateral artery; RA = right atrium; RV = right ventricle. B: Enlarged view. C: Corresponding view of 3-dimensional electroanatomic mapping system and CT. The dots present the radiofrequency applications. Right anterior oblique (RAO) view and left anterior oblique (LAO) view. RCA = right coronary artery.
References
- 1.Perez F.J., Schubert C.M., Parvez B., Pathak V., Ellenbogen K.A., Wood M.A. Long-term outcomes after catheter ablation of cavo-tricuspid isthmus dependent atrial flutter: a meta-analysis. Circ Arrhythm Electrophysiol. 2009;2:393–401. doi: 10.1161/CIRCEP.109.871665. [DOI] [PubMed] [Google Scholar]
- 2.Yune S., Lee W.J., Hwang J.W., Kim E., Ha J.M., Kim J.S. Acute myocardial infarction after radiofrequency catheter ablation of typical atrial flutter. J Korean Med Sci. 2014;29:292–295. doi: 10.3346/jkms.2014.29.2.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kubo T., Ino Y., Tanimoto T., Kitabata H., Tanaka A., Akasaka T. Optical coherence tomography imaging in acute coronary syndromes. Cardiol Res Pract. 2011;2011:312978. doi: 10.4061/2011/312978. [DOI] [PMC free article] [PubMed] [Google Scholar]