Abstract
Dilated cardiomyopathy (DCM) is extremely heterogeneous with a large proportion due to dominantly inherited disease-causing variants in sarcomeric genes. Recessive metabolic diseases may cause DCM, usually with onset in childhood, and in the context of systemic disease. Whether metabolic defects can also cause adult-onset DCM is currently unknown. Therefore, we performed an extensive metabolic screening in 36 consecutive adult-onset DCM patients. Diagnoses were confirmed by Sanger sequencing and multiplex ligation-dependent probe amplification (MLPA). Measurement of propionyl-CoA carboxylase (PCC) activity was done in fibroblasts. Whole exome sequencing (WES) data of 157 additional DCM patients were analyzed for genetic defects. We found a metabolic profile characteristic for propionic acidemia in a patient with severe DCM from 55 years of age. Genetic analysis demonstrated compound heterozygous variants in PCCA. Enzymatic activity of PCC in fibroblasts was markedly reduced. A targeted analysis of the PCCA and PCCB genes using available WES data from 157 further DCM patients subsequently identified another patient with propionic acidemia. This patient had compound heterozygous variants in PCCB, and developed severe DCM from 42 years of age. Adult-onset DCM can be caused by propionic acidemia, an autosomal recessive inheritable metabolic disorder usually presenting as neonatal or childhood disease. Current guidelines advise a low-protein diet to ameliorate or prevent detrimental aspects of the disease. Long-term follow-up of a larger group of patients may show whether this diet would also ameliorate DCM. Our results suggest that diagnostic metabolic screening to identify propionic acidemia and related disorders in DCM patients is justified.
Introduction
Dilated cardiomyopathy (DCM) is a cardiac condition characterized by dilatation of either the left ventricle or both ventricles and systolic dysfunction. DCM has an estimated prevalence of 1:250 and is one of the main causes of heart failure that requires heart transplantation. After prevalent causes such as coronary artery disease, valvular disease, congenital heart disease and hypertension have been excluded, DCM comprises a number of incompletely defined etiologies including cardiac inflammation with or without infectious agents, cytotoxic medication or drugs, arrhythmias and genetic causes. In some patients multiple etiologies combine in a multifactorial pathogenesis.1, 2, 3 More than 25% of DCM patients remain ‘idiopathic’ after extensive diagnostic investigations.4 Overall, in 20–48% of DCM patients their disease is familial5, 6, 7 and over 50 DCM disease genes are currently known.8 Genetic forms of DCM usually have autosomal dominant inheritance with reduced penetrance.3 A small fraction is due to an X-linked, autosomal recessive or mitochondrial inheritance pattern.9 Some of these recessive genes are involved in metabolic processes, including the mitochondrial proteins Tafazzin10 and SDHA11 and the glycosylation genes DOLK12 and FKTN.13 Of note, in patients with metabolic disease, the onset of DCM is usually in the neonatal or childhood period. The contribution of metabolic disease to adult-onset DCM is currently unknown. We therefore searched for metabolic defects in a cohort of adult-onset DCM patients using an extensive metabolic screen.
Methods
Patient recruitment
Patients with initially unexplained heart failure caused by DCM were enrolled in the Maastricht Cardiomyopathy Registry, as previously described.4 A complete diagnostic work-up included a.o. medical history, 12-lead electrocardiogram, echocardiography and Holter monitoring. After informed consent, an endomyocardial biopsy (EMB) and genetic evaluation was performed in all patients. Detailed inclusion and exclusion criteria are given in Supplementary Methods.
Starting in January 2015, an extensive metabolic screen using blood and urine samples was performed for 36 consecutive DCM patients to identify metabolic diseases. A targeted analysis of data from WES was then performed for a further 157 consecutive DCM patients in order to identify patients with propionic acidemia due to defects in PCCA or PCCB (Supplementary Figure 1).
The patients gave informed consent for this study and for publication of the results. The study was approved by the Institutional Review Board (RVE 124013).
Echocardiography
Echocardiographic measurements were performed in the standard parasternal, apical and subxiphoid views.14 The measured parameters included left ventricular end-diastolic diameter (LVEDD), LV end-systolic diameter and the end-diastolic thickness of the interventricular septum and of the LV posterior wall. The left ventricular ejection fraction (LVEF) was measured with Simpson’s biplane method from apical views to assess global LV systolic function.
Endomyocardial biopsy
Six EMB samples were taken from the right ventricle as described in Supplementary Methods. In short, 2–3 specimens were used for immunohistological analysis and three for the detection of viral genomes15 using polymerase chain reaction (PCR) and reverse transcriptase PCR analysis as previously described.16 Six primer pairs were used to detect cardiotropic DNA and RNA viruses (ie adenovirus, enterovirus, cytomegalovirus, Parvovirus B19, Human herpes virus-6 and Epstein–Barr virus). Significant viral load was defined as ≥500 copies per microgram DNA, as previously described.17 Increased cardiac inflammation was defined as ≥14 infiltrating cells per mm2, according to the definition of the World Health Organization/International Society and Federation of Cardiology.18
Metabolic screening
The screening protocol included assays by which known inborn errors of metabolism associated with cardiac involvement could be identified (Supplementary Tables 1 and 4). Metabolite screening in urine included organic acids, amino acids, acylcarnitines, oligosaccharides, mucopolysaccharides, sugars and polyols.19, 20, 21 The protocol in heparine plasma consisted of amino acids, acylcarnitines, homocysteine, methylmalonic acid, guanidino acetic acid and creatine and very long-chain fatty acids. Screening for disorders of glycosylation was performed by sialotransferrin isoelectric focusing in serum.22
Sequencing
Next-generation sequencing was performed on DNA from peripheral blood, for patient 1 using custom-made single molecule Molecular Inversion Probe (smMIP)23 panels containing 47 DCM associated genes (Supplementary Table 2), followed by multiplexed analysis on a NextSeq 500 System (Illumina) (patient 1). For patient 2 WES was performed with Illumina Hiseq 2000 (Illumina) sequencer after enrichment with SureSelectXT Human All Exon V4+UTRs, followed by analysis of the 47 DCM associated genes (Supplementary Table 2). Experimental details are described in Supplementary Methods.
For patient 1, direct sequencing of all exons within the coding region of the PCCA (NM_000282.3) and PCCB (NM_001178014.1) gene was applied. To test for heterozygous deletions/duplications in PCCA gene, we performed multiplex ligation-dependent probe amplification (MLPA) using the SALSA MLPA P278 PCCA probemix (MRC-Holland, the Netherlands) according to the instructions of the manufacturer. Exon numbering was according to the specifications of the manufacturer (MRC Holland, Amsterdam, the Netherlands). For patient 2, PCCA and PCCB were analyzed in the WES data.
All variants were submitted to the Leiden Open Variant Database (LOVD.nl/PCCA, patient ID 104049 and LOVD.nl/PCCB, patient ID 104050).
RNA analysis
Fibroblasts were cultured in the absence or presence of cycloheximide and cell pellets from both cultures were used to isolate RNA with the SV Total RNA Isolation kit (Promega, Madison, WI, USA) according to the manufacturer’s guideline and a RT-PCR was performed to amplify exons 19–24. Subsequently these PCR products were analyzed by Sanger sequencing.
Enzyme assay
A skin biopsy was taken from both patients. Fibroblasts were cultured and used to analyze the enzyme complex propionyl-CoA carboxylase (PCC) activity according to the procedures described in Supplementary Methods.
Results
Metabolic screening revealed propionic acidemia
Extensive metabolic screening was performed on 36 consecutive patients of our DCM cohort. This demonstrated an abnormal metabolic profile in a single DCM patient (patient 1). Elevated levels of 2-methylcitric acid in urine and glycine and propionylcarnitine were detected in plasma. A second set of measurements confirmed elevated levels of 2-methylcitric acid, glycine and propionylcarnitine, and also showed elevated levels of 3-hydroxypropionic acid and propionylglycine in urine. Methylmalonic acid excretion in urine was normal (Table 1). This metabolic profile is diagnostic for propionic acidemia (Figure 1).24
Table 1. Metabolites in plasma and urine.
| Patient 1 Measurement 1 | Patient 1 Measurement 2 | Patient 2 Measurement 1 | Patient 2 Measurement 2 | Son of patient 2 | Ref. value | |
|---|---|---|---|---|---|---|
| Organic acids in urine | ||||||
| Lactic acid | 4 | 117 | 5 | 8 | 4 | <37 |
| 3-hydroxypropionic acid | 25 | 282 | 115 | 205 | 3 | <30 |
| 2-methylcitric acid | 31 | 21 | 177 | 191 | 0 | <15 |
| Methylmalonic acid | 0 | 1 | 0 | 1 | 1 | <6 |
| 3-hydroxy-2-methylbutyric acid | 1 | 2 | 2 | 2 | 1 | <10 |
| 3-hydroxy-n-valeric acid | 1 | 4 | 3 | 7 | 3 | <20 |
| Glycine conjugates in urine | ||||||
| Propionylglycine | 0.05 | 5.38 | 4.39 | 12.42 | 0.00 | <0.07 |
| Isobutyrylglycine | 1.69 | 0.78 | 10.46 | 19.10 | 0.90 | <0.99 |
| Butyrylglycine | 0.01 | 0.12 | 0.09 | 0.23 | 0.62 | <0.16 |
| 2-methylbutyrylglycine | 0.73 | 0.42 | 5.18 | 6.99 | 0.22 | <0.57 |
| Isovalerylglycine | 0.60 | 0.30 | 5.63 | 9.22 | 0.46 | <1.15 |
| Valerylglycine | 0.02 | 0.06 | 0.12 | 0.33 | 0.00 | <0.11 |
| Tiglylglycine | 6.44 | 4.47 | 8.90 | 7.33 | 0.60 | <7 |
| 3-methylcrotonylglycine | 0.41 | 0.22 | 3.84 | 6.54 | 0.15 | <0.48 |
| Suberylglycine | 0.03 | 0.02 | 0.10 | 0.18 | 0.01 | <0.2 |
| Hexanoylglycine | 0.08 | 0.07 | 0.69 | 1.27 | 0.05 | <0.39 |
| Phenylpropionylglycine | 0.03 | 0.02 | 0.01 | 0.01 | 0.02 | <0.13 |
| Amino acids in plasma | ||||||
| Glycine | 487 | 495 | 1022 | 1105 | 263 | 147–321 |
| Amino acids in urine | ||||||
| Glycine | 56 | 416 | 1157 | 1300 | 129 | <525 |
| Acylcarnitines in plasma | ||||||
| Free carnitine | 55.20 | 32.36 | 28.98 | 21.87 | 41.02 | 22.29–54.81 |
| Propionylcarnitine | 16.43 | 10.12 | 28.17 | 39.25 | 0.36 | 0.13–0.95 |
| Acylcarnitines in urine | ||||||
| Free carnitine | 7.21 | 17.73 | 0.96 | 8.33 | 9.13 | NA |
| Propionylcarnitine | 2.09 | 7.77 | 1.70 | 21.07 | 0.18 | NA |
All values are given in μmol/mmol creatinine. Aberrant values are underlined.
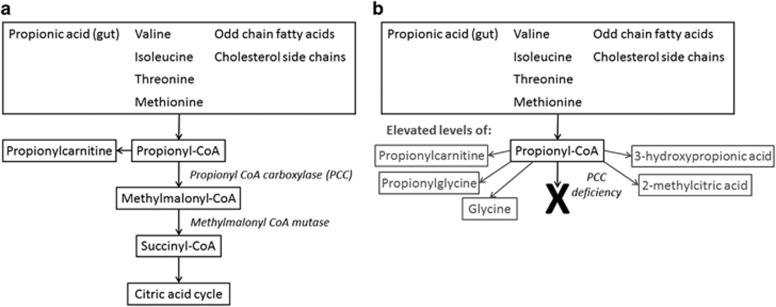
Figure 1.
Metabolic pathway of the propionyl-CoA carboxylase (PCC) complex involved in propionic acidemia. Under normal conditions (a) the amino acids valine, isoleucine, threonine and methionine, as well as propionic acid and odd chain fatty acids and cholesterol side chains are broken down to propionyl-CoA. The PCC complex converts propionyl-CoA to methylmalonyl-CoA, which is further converted to succinyl-CoA, a substrate of the citric acid cycle. A deficient PCC complex (b) prevents formation of methylmalonyl-CoA and gives rise to elevated levels of propionylcarnitine, propionylglycine, glycine, 3-hydroxypropionic acid and 2-methylcitric acid causing propionic acidemia.24, 39
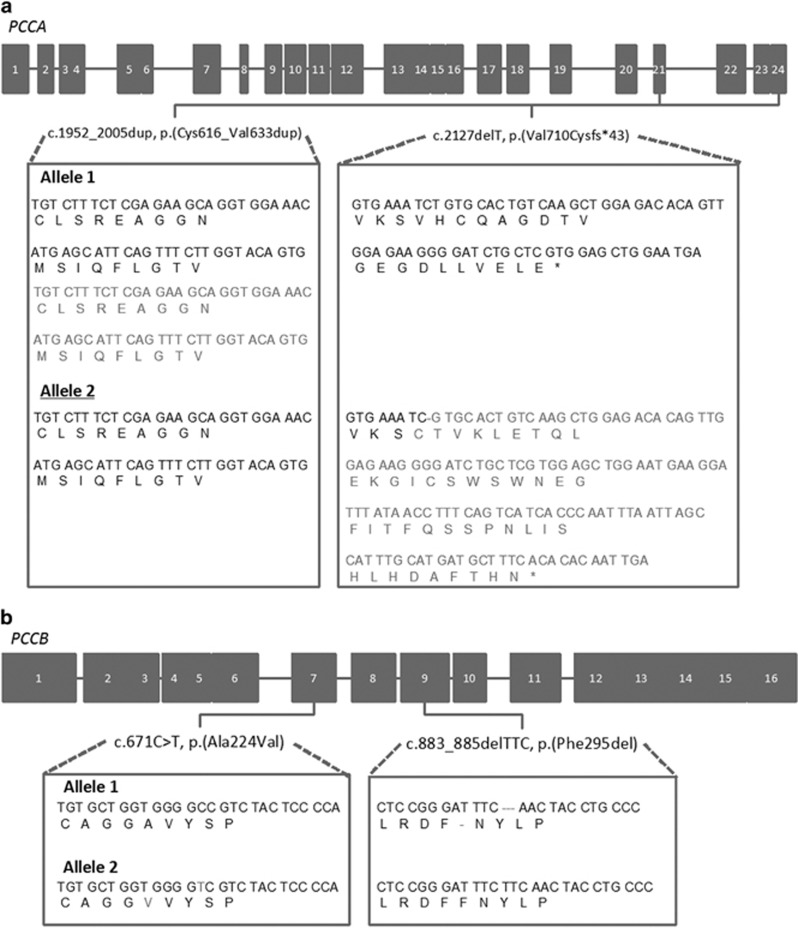
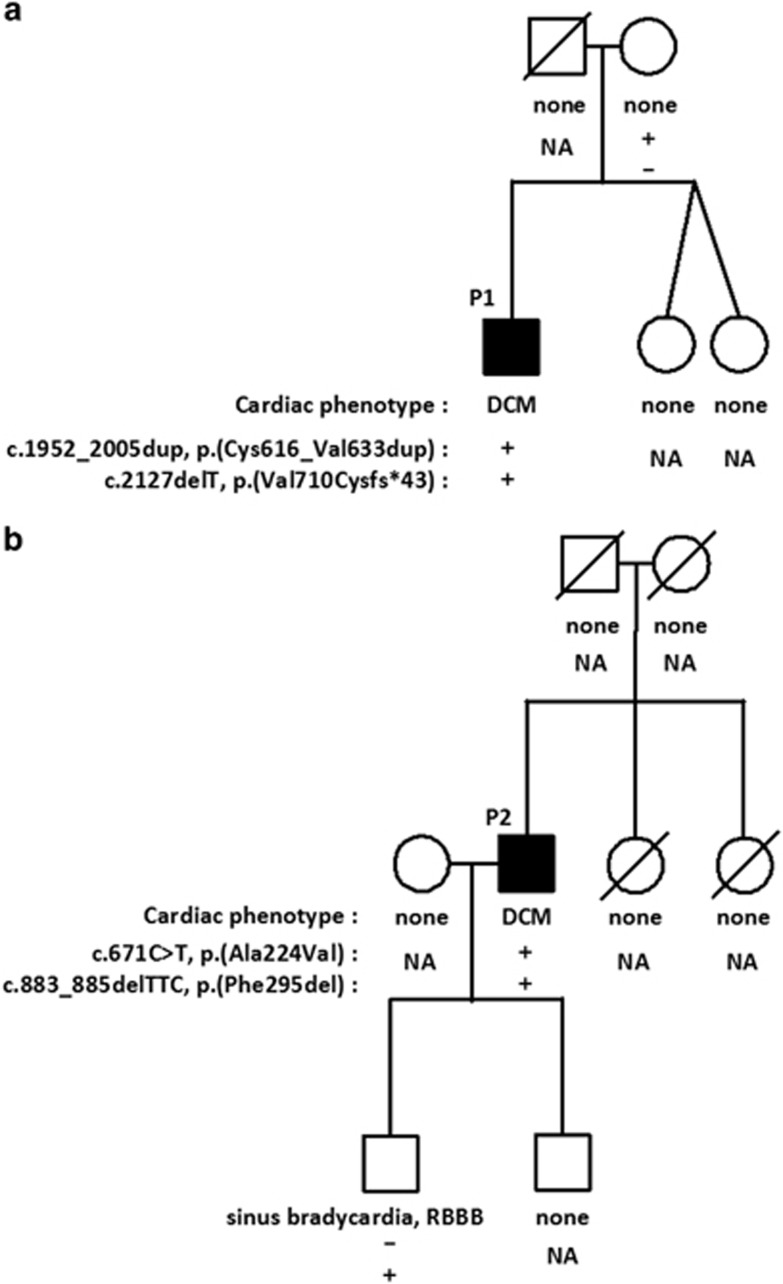
Propionic acidemia is caused by defects in the PCCA and PCCB genes that encode the subunits of the PCC complex.25 DNA sequencing detected a heterozygous PCCA frameshift variant (c.2127delT, p.(Val710Cysfs*43)) and MLPA revealed a duplication of exon 21 of PCCA (c.1952_2005dup, p.(Cys616_Val633dup)). As the mother of this patient only harbors the exon 21 duplication and the patient has two affected alleles, he is compound heterozygous for the two variants (Figures 2a and 3a). Both variants are not present in the data set of the Exome Aggregation Consortium (ExAC) (Cambridge, MA, USA (URL: http://exac.broadinstitute.org), accessed July 2016), containing 60 000 individuals.26
Figure 2.
PCCA (a) and PCCB (b) gene structure and localization of the compound heterozygous variants. Patient 1 harbors an exon 21 duplication of PCCA on one allele and has a frameshift variant on the other allele (a). Patient 2 has a missense variant in exon 7 of PCCB on one allele and an in-frame deletion of three base pairs in exon 9 on the other allele (b). In black the wild-type sequence, in red the mutated sequence.
Figure 3.
Pedigrees of the families. The father of patient 1 (P1) (a) passed away at age 85, his mother is now 86 years, both are not known with cardiological problems. His dizygotic twin sisters have no (cardiac) complaints. The parents of patient 2 (P2) (b) died at age 77 and 74 and both were not known with cardiological problems. His only two sibs died, one at 4 years of age from meningitis, the other one from cancer at age 48. Two sons have no signs of cardiomyopathy at ages 22 and 29, respectively. The youngest is known with sinus bradycardia and a complete right bundle branch block (RBBB) from age 19, but did not show a DCM phenotype with an LVEF of 57% and normal LV dimensions
mRNA analysis was performed on cultured fibroblasts from the patients. Only the c.2127delT variant was detected, even when the cells were cultured in the presence of cycloheximide to prevent nonsense mediated decay. Thus, only the allele containing the frameshift variant was detected in RNA from fibroblasts, suggesting that the duplication is probably a null allele. The activity of PCC in fibroblasts was markedly reduced (two independent measurements: 0.04 and 0.08 nmol/(min.mg protein), reference range: 0.28–1.16 nmol/(min.mg protein)). To exclude other possible genetic causes, 47 DCM associated genes (Supplementary Table 2) were analyzed by smMIP sequencing as part of our routine diagnostic procedure and revealed no variants affecting function (Supplementary table 5). Altogether, the results of the genetic and enzymatic studies confirm the diagnosis of propionic acidemia (Supplementary Figure 2A), as was suggested by the metabolic profile.
A genetic screen for propionic acidemia
Available genetic data from WES of all 22 000 human genes was analyzed for 157 further consecutive DCM patients, to specifically screen for variants affecting the function of the PCCA and PCCB genes. This uncovered another adult-onset DCM patient with propionic acidemia (patient 2). This patient carries two variants in PCCB: c.671C>T, p.(Ala224Val) and c.883_885delTTC, p.(Phe295del). Similar to patient 1, no other variants affecting function were identified in 47 genes known to be associated with DCM (Supplementary Tables 2 and 5). Analysis showed that a son who does not have DCM only harbors the c.883_885delTTC, p.(Phe295del) variant in PCCB. This confirms that the variants in patient 2 are in compound heterozygous state (Figures 2b and 3b and Supplementary Table 3). The in-frame deletion is not described in the ExAC data set, while the c.671C>T missense variant is only found in heterozygous state in 0.002% of this cohort.26 Metabolic analysis of patient 2 confirmed propionic acidemia (Table 1). In addition, analysis of PCC activity in his cultured fibroblasts revealed a markedly reduced activity of 0.016 nmol/(min.mg protein) compared to the reference range: 0.28–1.16 nmol/(min.mg protein) (Supplementary Figure 2B). As expected, metabolic analysis did not show any abnormalities for his son (Table 1).
Clinical phenotype of the patients
Both patients had adult-onset severe DCM in the absence of other characteristics of a metabolic disease. Furthermore, they did not demonstrate any dysmorphic features upon physical examination.
Patients were from non-consanguineous parents (Figure 3). Patient 1 was in good health until he was diagnosed with DCM (LVEF 20%, LVEDD 70 mm) at 55 years of age, in the absence of common causes of DCM. His cardiac function did not improve, after 6 months optimal heart failure medical therapy. An EMB was then performed to further evaluate the cause of his DCM, which did not demonstrate abnormalities (ie no increased cardiac inflammation, no viral presence or signs of an infiltrative disease). Subsequent cardiac resynchronization therapy with an implantable cardioverter-defibrillator (CRT-D) was instigated to treat the persistent systolic dysfunction and presence of complete left bundle branch block (cLBBB), but again cardiac function failed to improve. Finally, after 3 years, the diagnosis of propionic acidemia was made by metabolic studies.
Patient 2 is currently 61 years old. He was diagnosed with DCM (LVEF 40%, LVEDD 70 mm) and cLBBB at 42 years of age. Over the years, his cardiac function deteriorated towards 25–30% despite optimal medical heart failure therapy. He declined an EMB for further database. At the age of 53 years, he received a CRT-D, but his cardiac function failed to improve.
Discussion
In this study we describe two patients with adult-onset DCM that were diagnosed with propionic acidemia. The first patient with this specific metabolic disorder was identified via a relative easy and inexpensive metabolic screening using blood and urine. We detected corresponding genetic variants and showed a decreased activity of PCC. We identified the second propionic acidemia patient in our cohort by targeted analysis of existing WES data. Subsequent metabolic screening and measurement of PCC activity confirmed the metabolic diagnosis of propionic acidemia also in this patient, in the absence of systemic disease.
Propionic acidemia and treatment
Propionic acidemia is a metabolic disorder caused by variants in either PCCA or PCCB, which together encode the PCC complex that is deficient in propionic acidemia. The PCC complex, which consists of six PCCα and six PCCβ subunits,25 is involved in the metabolism of the amino acids methionine, threonine, valine and isoleucine as well as certain odd-chain fatty acids and cholesterol side chains and converts propionyl-CoA to methylmalonyl-CoA. Next, methylmalonyl-CoA is converted to succinyl-CoA, an intermediate of the citric acid cycle.24 A reduced PCC activity leads to elevated levels of propionylcarnitine, propionylglycine, glycine, 3-hydroxypropionic acid and 2-methylcitric acid (Figure 1). To prevent the accumulation of these toxic metabolites, a low protein diet is strongly recommended24 and both patients were recently put on such a diet. The daily food intake was lowered from 0.41–0.76 g/kg (natural protein/body mass) (patient 1) or 0.67–1.34 g/kg (patient 2) to 0.35–0.41 g/kg, supplemented with 0.35 g/kg protein equivalents amino acids without the PCC precursors methionine, threonine and valine, and with low amounts of isoleucine. Besides, the patients received metronidazole 500 mg t.i.d. in a cycle of 2 weeks on/2 weeks off, to reduce the production of propionyl-CoA by anaerobic gut flora. Additionally, the patients were supplemented with coenzyme Q10, an antioxidant which is hypothesized to prevent cardiac failure in propionic acidemia patients.27, 28 Long-term follow-up will be required to show whether this therapy might ameliorate DCM in these patients.
DCM in propionic acid patients
The patients described in this study were diagnosed with propionic acidemia several years after the onset of DCM. The reason for this diagnostic delay is that the usual clinical picture of propionic acidemia is an onset at birth with acute metabolic decompensation, including vomiting, refusal to feed and hypotonia due to hyperammonemia. Late onset (after the first year of life) propionic acidemia is characterized by developmental regression, protein intolerance, failure to thrive and movement disorders during childhood.29 DCM is observed in 9–23% of the newborns and children with propionic acidemia24 and usually presents within the first years of life.30, 31 To date, only two teenage propionic acidemia patients (age 14 and 16 years) with isolated DCM are described.32, 33 In contrast to neonatal patients, who usually have almost no PCC activity,31, 34 the two teenage DCM patients showed a residual PCC activity.32, 33 In fact, measurement of enzymatic activity showed limited but detectable residual activity in both patients reported here, supportive of hypomorphic alleles. A bundle branch block was observed in both DMC patients with propionic acidemia. Bundle branch block is seen frequently (25–30%) in DCM patients, and therefore does not constitute a disease-specific feature.4 The development of DCM in propionic acidemia is not associated with the age of onset and appears to be unrelated to clinical features or metabolic markers.31 The underlying pathophysiology is not yet understood. The citric acid cycle might be inhibited by accumulated toxic metabolites or by a lack of the substrate succinyl-CoA, which is the final product of the PCC complex-involved catabolic pathway.28, 31 Liver transplantation has a positive effect on cardiac functioning in propionic acidemia patients, possibly by reducing the amount of toxic metabolites. However, probably other pathophysiological mechanisms are important as well, as liver transplantation will not reduce in situ accumulation of toxic metabolites in the heart and good metabolic control in patients does not influence the development of DCM.31
Adult-onset DCM in propionic acidemia
Here we show that propionic acidemia can remain unnoticed until adulthood. A previous study reported on a series of approximately 100 propionic acidemia patients, aged between a few days and 27 years, who were mostly diagnosed via newborn screening. Of these, almost 20% remained asymptomatic, indicating that propionic acidemia can indeed remain unnoticed until later life.
Two explanations are possible as to why a disease that typically manifests with multi-organ involvement in the neonatal period can present with adult-onset DCM in our patients. First, the variants affecting the function of the protein in the neonatal cases are complete nulls with virtually no residual enzymatic function. In contrast, the variants in our cases are likely hypomorphic, such that the residual enzyme function may avert severe systemic disease before progressive DCM finally manifests in adulthood. In fact, measurement of enzymatic activity showed limited but detectable residual activity in both patients, supportive of a hypomorphic alleles (Table 1). Hypomorphic variants have been found in other diseases and can be accompanied by both a later presentation and a specific subset of phenotypic features.35, 36, 37 In fact, some experimental data exist that supports our hypothesis. When a hypomorphic PCCA variant was introduced in a mouse model, the resulting phenotype was DCM rather than early lethality as occurs in mice that carry homozygous severe PCCA variants.38
Secondly, we noted that patient 1 already had a diet relatively low in protein (0.41–0.76 g/kg, reference advised by National Board of Health: 0.9 g/kg), even before his metabolic diagnosis. If, and how much, this low protein intake contributed to his delayed presentation is unknown.
Conclusion
After in-depth DCM work-up, including EMB and genetic evaluation of 47 DCM-associated genes, we identified propionic acidemia as the most parsimonious cause in two patients with adult-onset DCM. However, a scenario in which propionic acidemia is a modifier of a yet unknown DCM-related gene cannot be formally excluded. In contrast to neonates and children with classical propionic acidemia who develop DCM in the course of severe multisystem disease, our patients developed DCM in the absence of other symptoms. Propionic acidemia is a rare cause of DCM, occurring in about 1% (1 of 36 metabolic screened patients and 1 of 157 WES screened patients) of the patients in our cohort. A prospective study on similar patients with propionic acidemia leading to adult-onset DCM may resolve whether the combination of a low-protein diet and supplements can improve cardiac function. Regardless, we recommend metabolic screening for adult-onset DCM patients.
Acknowledgments
We would like to thank Irene Körver-Keularts, PhD and Daphna Habets, PhD from the Department of Clinical Genetics, Maastricht University Medical Center+, the Netherlands for assistance with the interpretation of the metabolic screening, Dirk Lefeber, PhD from the Department of Neurology and Translation Metabolic Laboratory, Radboudumc Nijmegen, the Netherlands for performing the mucopolysaccharides analysis and Christian Gilissen, PhD from the Department of Human Genetics, Radboudumc Nijmegen, the Netherlands for providing the Gene Checker tool. Warsha Kanhai and Matilde Fernandez Ojeda are acknowledged for their enthusiastic and excellent laboratory assistance in the Metabolic Unit, Amsterdam, the Netherlands.
Footnotes
Supplementary Information accompanies this paper on European Journal of Human Genetics website (http://www.nature.com/ejhg)
The authors declare no conflict of interest.
Supplementary Material
References
- Maron BJ, Towbin JA, Thiene G et al: Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation 2006; 113: 1807–1816. [DOI] [PubMed] [Google Scholar]
- Caforio AL, Pankuweit S, Arbustini E et al: Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J 2013; 34: 2636–2648, 2648a–2648d. [DOI] [PubMed] [Google Scholar]
- Hershberger RE, Hedges DJ, Morales A: Dilated cardiomyopathy: the complexity of a diverse genetic architecture. Nat Rev Cardiol 2013; 10: 531–547. [DOI] [PubMed] [Google Scholar]
- Hazebroek MR, Moors S, Dennert R et al: Prognostic relevance of gene–environment interactions in patients with dilated cardiomyopathy: applying the MOGE(S) classification. J Am Coll Cardiol 2015; 66: 1313–1323. [DOI] [PubMed] [Google Scholar]
- Michels VV, Moll PP, Miller FA et al: The frequency of familial dilated cardiomyopathy in a series of patients with idiopathic dilated cardiomyopathy. N Engl J Med 1992; 326: 77–82. [DOI] [PubMed] [Google Scholar]
- Grünig E, Tasman JA, Kücherer H, Franz W, Kübler W, Katus HA: Frequency and phenotypes of familial dilated cardiomyopathy. J Am Coll Cardiol 1998; 31: 186–194. [DOI] [PubMed] [Google Scholar]
- Baig MK, Goldman JH, Caforio AL, Coonar AS, Keeling PJ, McKenna WJ: Familial dilated cardiomyopathy: cardiac abnormalities are common in asymptomatic relatives and may represent early disease. J Am Coll Cardiol 1998; 31: 195–201. [DOI] [PubMed] [Google Scholar]
- Posafalvi A, Herkert JC, Sinke RJ et al: Clinical utility gene card for: dilated cardiomyopathy (CMD). Eur J Hum Genet 2013; 21, doi:10.1038/ejhg.2012.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mestroni L, Rocco C, Gregori D et al: Familial dilated cardiomyopathy: evidence for genetic and phenotypic heterogeneity. Heart Muscle Disease Study Group. J Am Coll Cardiol 1999; 34: 181–190. [DOI] [PubMed] [Google Scholar]
- D'Adamo P, Fassone L, Gedeon A et al: The X-linked gene G4.5 is responsible for different infantile dilated cardiomyopathies. Am J Hum Genet 1997; 61: 862–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitas A, Muhammad E, Harel G et al: Familial neonatal isolated cardiomyopathy caused by a mutation in the flavoprotein subunit of succinate dehydrogenase. Eur J Hum Genet 2010; 18: 1160–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lefeber DJ, de Brouwer AP, Morava E et al: Autosomal recessive dilated cardiomyopathy due to DOLK mutations results from abnormal dystroglycan O-mannosylation. PLoS Genet 2011; 7: e1002427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Müller T, Krasnianski M, Witthaut R, Deschauer M, Zierz S: Dilated cardiomyopathy may be an early sign of the C826A Fukutin-related protein mutation. Neuromuscul Disord 2005; 15: 372–376. [DOI] [PubMed] [Google Scholar]
- Gottdiener JS, Bednarz J, Devereux R et al: American Society of Echocardiography recommendations for use of echocardiography in clinical trials. J Am Soc Echocardiogr 2004; 17: 1086–1119. [DOI] [PubMed] [Google Scholar]
- Heymans S, Schroen B, Vermeersch P et al: Increased cardiac expression of tissue inhibitor of metalloproteinase-1 and tissue inhibitor of metalloproteinase-2 is related to cardiac fibrosis and dysfunction in the chronic pressure-overloaded human heart. Circulation 2005; 112: 1136–1144. [DOI] [PubMed] [Google Scholar]
- Dennert R, Velthuis S, Schalla S et al: Intravenous immunoglobulin therapy for patients with idiopathic cardiomyopathy and endomyocardial biopsy-proven high PVB19 viral load. Antivir Ther 2010; 15: 193–201. [DOI] [PubMed] [Google Scholar]
- Bock CT, Klingel K, Kandolf R: Human parvovirus B19-associated myocarditis. N Engl J Med 2010; 362: 1248–1249. [DOI] [PubMed] [Google Scholar]
- Richardson P, McKenna W, Bristow M et al: Report of the 1995 World Health Organization/International Society and Federation of Cardiology Task Force on the Definition and Classification of cardiomyopathies. Circulation 1996; 93: 841–842. [DOI] [PubMed] [Google Scholar]
- Waterval WAH, Scheijen JLJM, Ortmans-Ploemen MMJC, Habets-van der Poel CD, Bierau J: Quantitative UPLC-MS/MS analysis of underivatised amino acids in body fluids is a reliable tool for the diagnosis and follow-up of patients with inborn errors of metabolism. Clin Chim Acta 2009; 407: 36–42. [DOI] [PubMed] [Google Scholar]
- Vreken P, van Lint AE, Bootsma AH, Overmars H, Wanders RJ, van Gennip AH: Quantitative plasma acylcarnitine analysis using electrospray tandem mass spectrometry for the diagnosis of organic acidaemias and fatty acid oxidation defects. J Inherit Metab Dis 1999; 22: 302–306. [DOI] [PubMed] [Google Scholar]
- Blau N, Duran M, Gibson KM: Laboratory Guide to the Methods in Biochemical Genetics. Berlin Heidelberg: Springer-Verlag, 2008. [Google Scholar]
- de Jong G, van Noort WL, van Eijk HG: Optimized separation and quantitation of serum and cerebrospinal fluid transferrin subfractions defined by differences in iron saturation or glycan composition. Adv Exp Med Biol 1994; 356: 51–59. [DOI] [PubMed] [Google Scholar]
- O'Roak BJ, Vives L, Fu W et al: Multiplex targeted sequencing identifies recurrently mutated genes in autism spectrum disorders. Science 2012; 338: 1619–1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumgartner MR, Horster F, Dionisi-Vici C et al: Proposed guidelines for the diagnosis and management of methylmalonic and propionic acidemia. Orphanet J Rare Dis 2014; 9: 130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall PR, Wang YF, Rivera-Hainaj RE et al: Transcarboxylase 12S crystal structure: hexamer assembly and substrate binding to a multienzyme core. EMBO J 2003; 22: 2334–2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lek M, Karczewski KJ, Minikel EV et al: Analysis of protein-coding genetic variation in 60 706 humans. Nature 2016; 536: 285–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fragaki K, Cano A, Benoist JF et al: Fatal heart failure associated with CoQ10 and multiple OXPHOS deficiency in a child with propionic acidemia. Mitochondrion 2011; 11: 533–536. [DOI] [PubMed] [Google Scholar]
- Baruteau J, Hargreaves I, Krywawych S et al: Successful reversal of propionic acidaemia associated cardiomyopathy: evidence for low myocardial coenzyme Q10 status and secondary mitochondrial dysfunction as an underlying pathophysiological mechanism. Mitochondrion 2014; 17: 150–156. [DOI] [PubMed] [Google Scholar]
- Shchelochkov OA, Carrillo N, Venditti C. Propionic Acidemia; 2012 May 17 [Updated 2016 Oct 6] In: Pagon RA, Adam MP, Ardinger HH et al. (eds): GeneReviews® [Internet]. University of Washington: Seattle, WA, 1993–2017.
- Massoud AF, Leonard JV: Cardiomyopathy in propionic acidaemia. Eur J Pediatr 1993; 152: 441–445. [DOI] [PubMed] [Google Scholar]
- Romano S, Valayannopoulos V, Touati G et al: Cardiomyopathies in propionic aciduria are reversible after liver transplantation. J Pediatr 2010; 156: 128–134. [DOI] [PubMed] [Google Scholar]
- Lee TM, Addonizio LJ, Barshop BA, Chung WK: Unusual presentation of propionic acidaemia as isolated cardiomyopathy. J Inherit Metab Dis 2009; 32 (Suppl 1): S97–S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laemmle A, Balmer C, Doell C, Sass JO, Haberle J, Baumgartner MR: Propionic acidemia in a previously healthy adolescent with acute onset of dilated cardiomyopathy. Eur J Pediatr 2014; 173: 971–974. [DOI] [PubMed] [Google Scholar]
- Kraus JP, Spector E, Venezia S et al: Mutation analysis in 54 propionic acidemia patients. J Inherit Metab Dis 2012; 35: 51–63. [DOI] [PubMed] [Google Scholar]
- den Hollander AI, Koenekoop RK, Yzer S et al: Mutations in the CEP290 (NPHP6) gene are a frequent cause of Leber congenital amaurosis. Am J Hum Genet 2006; 79: 556–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costes B, Girodon E, Ghanem N et al: Frequent occurrence of the CFTR intron 8 (TG)n 5T allele in men with congenital bilateral absence of the vas deferens. Eur J Hum Genet 1995; 3: 285–293. [DOI] [PubMed] [Google Scholar]
- Drenth JP, Cuisset L, Grateau G et al: Mutations in the gene encoding mevalonate kinase cause hyper-IgD and periodic fever syndrome. International Hyper-IgD Study Group. Nat Genet 1999; 22: 178–181. [DOI] [PubMed] [Google Scholar]
- Guenzel AJ, Hofherr SE, Hillestad M et al: Generation of a hypomorphic model of propionic acidemia amenable to gene therapy testing. Mol Ther 2013; 21: 1316–1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofherr SE, Senac JS, Chen CY, Palmer DJ, Ng P, Barry MA: Short-term rescue of neonatal lethality in a mouse model of propionic acidemia by gene therapy. Hum Gene Ther 2009; 20: 169–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.