Abstract
Aim:
Restoration of normal function and jaw movements in patients with temporomandibular joint (TMJ) ankylosis has been a challenge. Various techniques have been provided for its treatment; but the results have been variable. The purpose of this paper is to present an easy and versatile method for the treatment of TMJ ankylosis and to decrease postoperative complications such as reankylosis.
Materials and Methods:
This paper is a review of surgical outcome of interposition arthroplasty with temporalis fascia in 17 patients of unilateral TMJ ankylosis who underwent the above procedure. The review is based on the pre-, intra- and post-operative evaluation of these seventeen patients who were treated between 2008 and 2013. The follow-up time was 1–5 years.
Results:
Reankylosis was seen in only one of the patients; the remaining patients had satisfactory mouth openings.
Conclusion:
Surgical treatment of TMJ ankylosis with interposition of temporal fascia is an effective and easy procedure for prevention for reankylosis. The autogeneous nature and proximity to the joint are the main advantages of the temporal fascia flap when compared with other interpositional materials.
Keywords: Interpositional arthroplasty, temporal fascia flap, temporomandibular joint ankylosis
Introduction
Temporomandibular joint (TMJ) ankylosis is a condition associated with stiffening of the joint due to disease process resulting in fibrous or bony fusion of the mandibular condyle to the skull base. The resultant significant reduction in the mouth opening manifests primarily as impaired speech, difficulty in mastication, facial deformity (bird face deformity)[1] and associated features viz-poor oral hygiene and periodontal disease, occlusal and growth disturbances involving maxilla and mandible, difficulty in breathing, and compromised airway characterized by sleep apnea.
TMJ ankylosis may be classified as false or true,[2] extra- or intra-articular, fibrous or bony, unilateral or bilateral, partial or complete.
The most common etiological factor is trauma followed by infections, inflammatory conditions, and systemic diseases. Laskin[3] in1978 outlined various factors that may be implicated in the genesis of ankylosis following trauma to mandible. Miyamoto et al.[4] emphasized that hemarthrosis alone does not lead to ankylosis. It is hypothesized that intra-articular hematoma with scarring results in hypomobility of the joint and subsequent bone formation which leads to ankylosis. Treatment of TMJ ankylosis and its associated complications along with its high recurrence rate,[5,6] pose a significant challenge to the clinician.
Treatment aims at restoring joint function, improving patient's esthetics, quality of life (as many TMJ ankylosis patients are malnourished), and also to prevent recurrence. The treatment of TMJ ankylosis is always surgical. Gap arthroplasty and interpositional arthroplasty are the treatment of choice. Various autologous interpositional graft materials such as temporalis and masseter muscle, temporalis fascia, fascia lata, dermis, fat, auricular cartilage, and costochondral graft have been used for the above purpose. Nonbiological options comprise insertion of silastic,[7] silicone,[8] materials, and T-plates.
Yolovine in 1898 first described the use of temporalis fascia flaps. Temporalis fascia flaps were first used in TMJ surgery by Murphy in 1912,[9] and there have been other advocates of its use over the years.[10] The present review aims to examine the efficacy of the surgical procedure, namely, –interpositional arthroplasty with temporalis fascia flap in 17 patients with unilateral TMJ ankylosis.
Materials and Methods
In the 5-year period from 2008 to 2013, 17 patients underwent surgical treatment – interpositional arthroplasty with temporalis fascia – for ankylosis at our institute. Pre- and post-operative assessment included detailed history and a thorough clinical examination. Data concerning patients' age, gender, etiology of ankylosis, joints affected, preoperative and postoperative mouth openings, and follow up periods were recorded [Table 1]. Radiographic assessment was carried out for all patients using orthopantomogram (OPG) and computed tomography [Figures 1 and 2]. Maximum follow-up period was 5 years while minimum was 1 year. Mouth opening has been assessed with callipers pre-, intra- and post-operatively. Preoperative maximum inter incisal mouth opening ranged from 0 to 25 mm (with an average of 1.5 mm) [Figures 3 and 4].
Table 1.
Summary of results
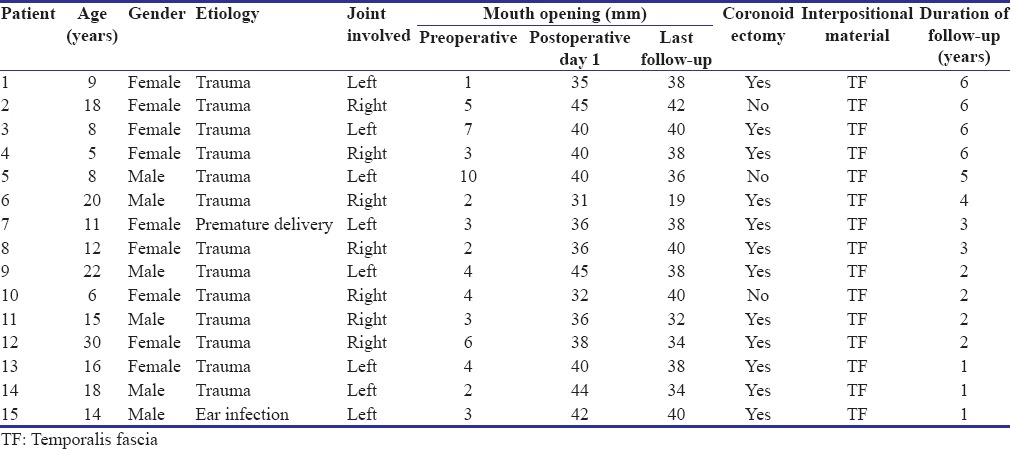
Figure 1.

Three-dimensional computed tomogram showing left temporomandibular joint ankylosis
Figure 2.

Coronal section of three-dimensional computed tomogram showing ankylotic mass
Figure 3.

Preoperative mouth opening and facial asymmetry
Figure 4.

Postoperative mouth opening
In all these patients who underwent surgical management of ankylosis, a pedicled deep temporalis fascia flap based on middle temporal branch of superficial temporal artery was used as an interpositioning material. All surgical procedures were carried out under general anesthesia administered through nasotracheal intubation using fiberoptic bronchoscope.
Al-Kayat Bramley incision was used in all these patients. Dissection was carried through subcutaneous plane down to deep temporal fascia. This fascia was carefully dissected taking care to preserve superficial temporal artery, vein, and superficial temporal branch of the facial nerve. Dissection was further carried inferiorly to reach the zygomatic arch. Deep temporal fascia was then divided, and inverted L-shaped incision was taken on zygoma, distal to articular eminence, and anterior to external auditory meatus. Ankylotic mass was exposed and excised to create a gap of 8–10 mm [Figure 5]. Recontouring of the glenoid fossa was done as required. Maximum mouth opening was measured and recorded. Ipsilateral coronoidectomy was performed in all the cases through the same extraoral approach. Contralateral coronoidectomy was done through intraoral approach only in cases where mouth opening achieved was lesser than 35 mm. An inferiorly based Temporalis fascia flap was adequately mobilized with the base of the flap lying above the zygomatic arch and interpositioned in the gap between zygomatic arch and ramus stump [Figure 6]. This flap is based on the middle temporal branch of superficial temporal artery.[11] It was secured to the posterior edge of the preauricular incision with 3-0 vicryl sutures. Drains were placed before primary closure of both preauricular and intraoral incisions. Minimal infection and hematoma formation were seen in immediate postoperative period. Patients were given physiotherapy in the form of jaw exercises from the third postoperative day.
Figure 5.
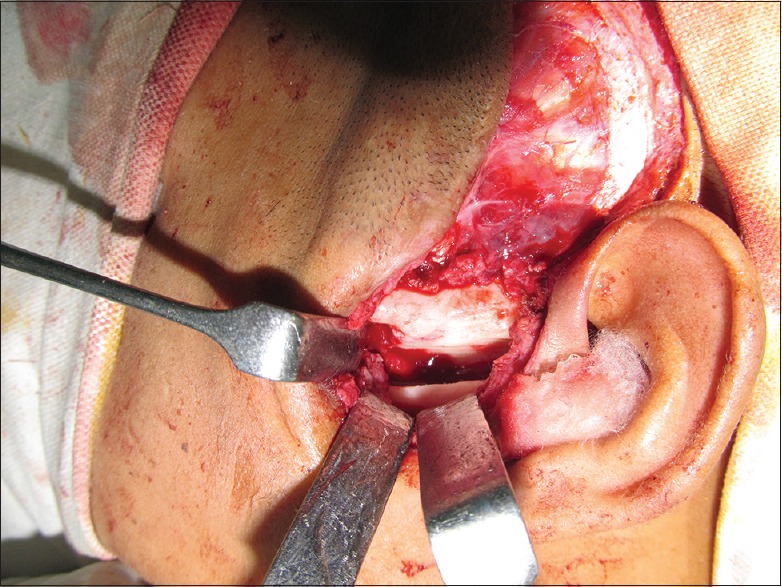
Gap arthroplasty
Figure 6.
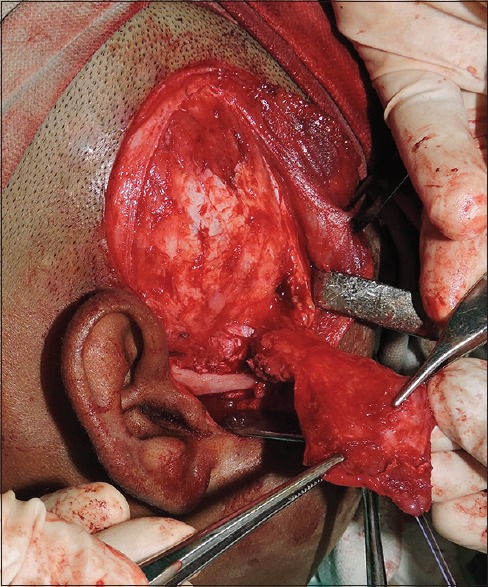
Temporalis fascia being harvested
Results
Surgical outcome of a total number of 17 patients who underwent interpositional arthroplasty for unilateral TMJ ankylosis has been reviewed; 9 left sided and 8 right sided; 10 females and 7 males; with age ranging from 5 to 30 years (mean age 14 years). Trauma (88%) was the most common cause of ankylosis in the patients reviewed. Preoperative mouth opening ranged from 0 to 10 mm (with the mean mouth opening being 4 mm). Maximum mouth opening achieved post operatively ranged from 32 to 42 mm (with an average of 37 mm). Postoperative follow-up period ranged from a minimum of 1 year to a maximum of 5 years. No patients showed signs of facial nerve palsy. Deviation to the affected side was seen in almost all the cases. Reankylosis was seen in one patient. Periodic radiographic examination with OPG showed no signs of reankylosis in the joint and the intra-articular space was well maintained in other sixteen cases.
Discussion
The high recurrence rate and the technical difficulties involved in the TMJ surgery makes it a challenging task for the surgeon. One of the surgical procedure is gap arthroplasty without interposition. Arthroplasty without interposition requires a gap of 10–20 mm.[12] Topazian reported a recurrence rate of 53%[13] for gap arthroplasty without interposition. Gap arthroplasty is not only a relatively simple procedure with short-operating time but also has disadvantages such as creation of pseudo articulation with a short ramus and an increased risk of reankylosis. Hence, interpositional gap arthroplasty is preferable. The main function of an interpositional material is to eliminate contact between two bony surfaces of the joint and avoid recurrence. Moss and Salantijn in 1969 pointed out that the muscular matrix around the mandible may affect the results of the treatment. Early treatment will restore mandibular mobility and subsequently improve facial growth and remodeling to reduce the possibility of the future facial asymmetry or retrognathia.[14]
Various interpositioning materials have been proposed and used, but none has proved to be an ideal one.
In the present review, we have evaluated surgical results of 17 patients of unilateral TMJ ankylosis. Temporalis fascia was used as an interpositional material. The flap is based on middle temporal artery which is a branch of superficial temporal artery, and we found the following advantages.
Autologous nature; therefore least immunoreactive.
Proximity to the joint, enabling excellent mobility and coverage of the arthroplasty gap, minimal donor site morbidity both cosmetically and functionally
Minimal damage to the temporal branch of the facial nerve
Good resilience and blood supply
Hollowing in the temporal region is not evident
Minimal intraoperative blood loss
Low degree of friction and good positional stability.
Although studies have shown that temporalis fascia lacks bulk, we found excellent long-term results for a follow-up period of 5 years with almost no recurrence (1 out of 17 patients).
The surgical protocol followed was the one proposed by Kaban, 1990 which included ankylotic mass resection, ipsilateral coronoidectomy, interposition of temporalis fascia, early mobilization with aggressive physiotherapy.[15]
Long-standing ankylosis may result in temporalis muscle atrophy and fibrosis. Ken et al. and Guralnick and Kaban recommended ipsilateral coronoidectomy to enhance intraoperative interincisal opening.[16,17]
Early active and long-term physiotherapy in the form of jaw exercises and a long-term follow-up is of greatest importance to prevent reankylosis.
Our experience with the temporalis fascia flap used as an interpositioning material in the surgical management of TMJ ankylosis produced good results in mouth opening, jaw function, and prevention of recurrence. In addition, temporalis fascia remains biologically viable and serves as a satisfactory TMJ lining.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.el-Sheikh MM, Medra AM, Warda MH. Bird face deformity secondary to bilateral temporomandibular joint ankylosis. J Craniomaxillofac Surg. 1996;24:96–103. doi: 10.1016/s1010-5182(96)80020-5. [DOI] [PubMed] [Google Scholar]
- 2.Kazanjian VH. Temporomandibular joint ankylosis with mandibular retrusion. Am J Surg. 1955;90:905–10. doi: 10.1016/0002-9610(55)90721-2. [DOI] [PubMed] [Google Scholar]
- 3.Laskin DM. Role of the meniscus in the etiology of posttraumatic temporomandibular joint ankylosis. Int J Oral Surg. 1978;7:340–5. doi: 10.1016/s0300-9785(78)80106-9. [DOI] [PubMed] [Google Scholar]
- 4.Miyamoto H, Kurita K, Ogi N, Ishimaru J, Goss AN. The effect of an intra-articular bone fragment in the genesis of temporomandibular joint ankylosis. Int J Oral Maxillofac Surg. 2000;29:290–5. [PubMed] [Google Scholar]
- 5.Topazian RG. Comparison of gap and interposition arthroplasty in the treatment of temporomandibular joint ankylosis. J Oral Surg. 1966;24:405–9. [PubMed] [Google Scholar]
- 6.Padgett EC, Robinson DW, Stephenson KL. Ankylosis of the temporomandibular joint. Surgery. 1948;24:426–37. [PubMed] [Google Scholar]
- 7.Alpert B. Silastic tubing for interpositional arthroplasty. J Oral Surg. 1978;36:153. [PubMed] [Google Scholar]
- 8.Estabrooks LN, Murnaine TW, Doku HC. The role of condylectomy with interpositional silicone rubber in TMJ ankylosis. J Oral Surg. 1972;34:2. doi: 10.1016/0030-4220(72)90265-4. [DOI] [PubMed] [Google Scholar]
- 9.Aneja V, Raval R, Bansal A, Kumawat V, Kaur J, Shaikh AA. Interpositional Gap Arthroplasty by Versatile Pedicled Temporalis Myofascial Flap in the Management of Temporomandibular Joint Ankylosis - A Case Series Study. J Clin Diagn Res. 2016;10:ZR01–ZR04. doi: 10.7860/JCDR/2016/20157.8741. [Epub 2016 Oct 1] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Majumdar A, Bainton R. Suture of temporalis fascia and muscle flaps in temporomandibular joint surgery. Br J Oral Maxillofac Surg. 2004;42:357–9. doi: 10.1016/j.bjoms.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 11.Abul-Hassan HS, von Drasek Ascher G, Acland RD. Surgical anatomy and blood supply of the fascial layers of the temporal region. Plast Reconstr Surg. 1986;77:17–28. [PubMed] [Google Scholar]
- 12.Chossegros C, Guyot L, Cheynet F, Blanc JL, Gola R, Bourezak Z, et al. Comparison of different materials for interposition arthroplasty in treatment of temporomandibular joint ankylosis surgery: Long-term follow-up in 25 cases. Br J Oral Maxillofac Surg. 1997;35:157–60. doi: 10.1016/s0266-4356(97)90554-4. [DOI] [PubMed] [Google Scholar]
- 13.Topazian RG. Etiology OF Ankylosis of temporomandibular joint: Analysis of 44 cases. J Oral Surg Anesth Hosp Dent Serv. 1964;22:227–33. [PubMed] [Google Scholar]
- 14.Moss ML, Salentijn L. The capsular matrix. Am J Orthod. 1969;56:474–90. doi: 10.1016/0002-9416(69)90209-7. [DOI] [PubMed] [Google Scholar]
- 15.Kaban LB, Perrott DH, Fisher K. A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 1990;48:1145–51. doi: 10.1016/0278-2391(90)90529-b. [DOI] [PubMed] [Google Scholar]
- 16.Guralnick WC, Kaban LB. Surgical treatment of mandibular hypomobility. J Oral Surg. 1976;34:343–8. [PubMed] [Google Scholar]
- 17.Kent JN, Misiek DJ, Akin RK, Hinds EC, Homsy CA. Temporomandibular joint condylar prosthesis: A ten-year report. J Oral Maxillofac Surg. 1983;41:245–54. doi: 10.1016/0278-2391(83)90267-7. [DOI] [PubMed] [Google Scholar]


