Abstract
Background:
Gingival recession involves both soft tissue and hard tissue loss. In this evolutionary era of dentistry, newer techniques have evolved for complete coverage of isolated recession defects. Since 2012, vestibular incision subperiosteal tunnel access (VISTA) technique was used with various regenerative membranes to treat multiple recession defects (MRDs). Platelet-rich fibrin (PRF) membrane, a pool of growth factors but have any added advantage to recession coverage techniques is controversial. Thus, in this case series, we compare the effect of VISTA with or without PRF-membrane for the treatment of Classes I and III MRDs.
Subjects and Methods:
Four patients between of age 30 and 40 years (two patients having bilateral Class I and another two having bilateral Class III MRDs) were selected from the Department of Periodontics, ITS Dental College, Greater Noida and designated as Case I–IV simultaneously. Recession defects at antagonist sites in each patient were corrected by VISTA approach with or without PRF-membrane. Recorded clinical parameters included recession depth, recession width, pocket probing depth, and clinical attachment level (CAL) at baseline and 6 months postoperatively.
Results:
Patients having Class I recession defects showed almost complete root coverage with VISTA technique alone and reflected no added advantage of PRF-membrane. However, patients with Class III recession defects treated with VISTA + PRF-membrane showed more reduction in recession depth and gain in CAL as compared to sites treated with VISTA only.
Conclusion:
VISTA alone is a convenient technique for treatment of Class I MRDs. Addition of PRF-membrane for Class III recession defects give better outcome in term of reduction of recession depth and gain in CAL 6 month postoperatively.
Keywords: Classes I and III multiple recession defects, platelet-rich fibrin membrane, subperiosteal tunnel, VISTA technique
Introduction
In routine dental practice “gingival recession (GR)” defects are frequently encountered complain because of functional and esthetic concern of the patients. GR is defined as the “displacement of marginal tissue apical to the cementoenamel junction (CEJ).”[1] Recession defects can be isolated or multiple. First line of treatment includes removal of etiological factors followed by surgical correction.[2] Several periodontal plastic surgical procedures have been documented for the treatment of Miller's Classes I and II recession defects and negotiate patient's discomfort due to hypersensitivity, food lodgement, fear of tooth loss, etc.[3] Evidence echos that coronally advanced flap (CAF) based procedures are considered a reliable approach for complete root coverage (CRC) while treating isolated GR defect. However, there is consistent lack of evidence for coverage of multiple recession defects (MRD).[4]
The surgical treatment for MRD include connective tissue graft,[5] guided tissue regeneration membrane,[6] enamel matrix derivative,[7] acellular dermal matrix allograft,[8] and platelet-rich fibrin[4] (PRF) membrane. Vestibular incision subperiosteal tunnel access (VISTA) is an upcoming tunnel approach for treatment of MRDs, especially for maxillary anteriors.[6] Afterward, this technique was modified using PRF membrane as an adjunct to VISTA and showed more promising results for treatment of multiple Classes I and II recession defects.[9] However, recent meta-analysis showed that PRF membrane as an adjunct did not improve recession depth and width as compared to recession coverage procedures applied alone.[10] Thus, in this case series, we evaluate the efficacy of VISTA with or without PRF membrane in the treatment of multiple Classes I and III recession defects.
Subjects and Methods
Case selection
Four systemically healthy, nonsmoker patients (two males and two females) of 30–35 years age group who reported to the Department of Periodontics, ITS Dental College, Greater Noida with a chief complaint of either compromised esthetics or sensitivity to hot and cold with multiple recession defccts were included in the study. The patients presented with bilateral Miller's Class I or III MRDs and diagnosed as a case of chronic generalized periodontitis. Female patient with anterior maxillary Class I recession defects named as Case I [Figures 1 and 2a], female patient with maxillary Class I multiple recession designate as Case II, male patient with Class III [Figure 3a] recession defects in maxillary posterior assigned as Case III, and last male patient with bilateral maxillary anterior Class III recession defect labeled as Case IV.
Figure 1.
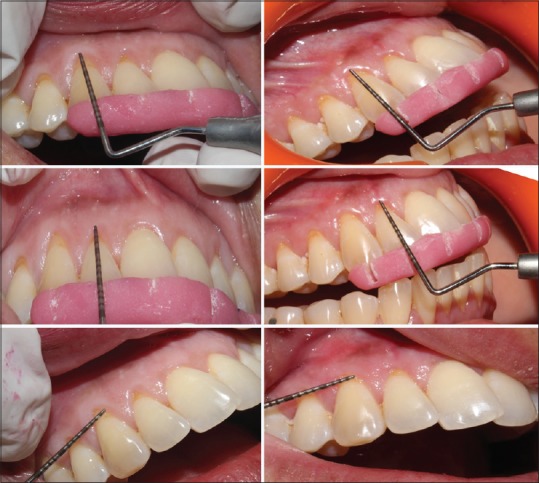
Case I: Pre- and post-operative recession depth and width
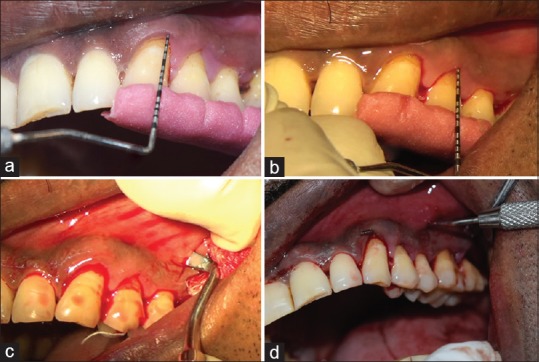
Figure 2.

Case-1 (a) preoperative view (b) subperiosteal tunnel (c) suturing (d) 1-month postoperative
Figure 3.
Vestibular incision subperiosteal tunnel access with platelet-rich fibrin membrane. (a and b) Preoperative recession depth (c) vertical incision (d) preoperation of subperiosteal tunnel
The clinical parameters were recorded at the selected sites using UNC-15 probe and acrylic surgical stent preoperatively and 6 months after surgery. These parameters were as follows: (1) Recession height (RH) [Figures 1a–d, 3a, b and Table 1], (2) width of recession defect (RW) [Figure 1e and f], (3) probing depth (PD), (4) clinical attachment level (CAL) [Table 2]. RD, PD, and CAL were recorded midbucally and RW was recorded at CEJ [Figure 1e and f]. Radiographic evaluation of bone height was done [Figure 4a–c] for the sites underwent root recession coverage procedure.
Table 1.
Comparison of Clinical Parameters between Baseline and after 6 months
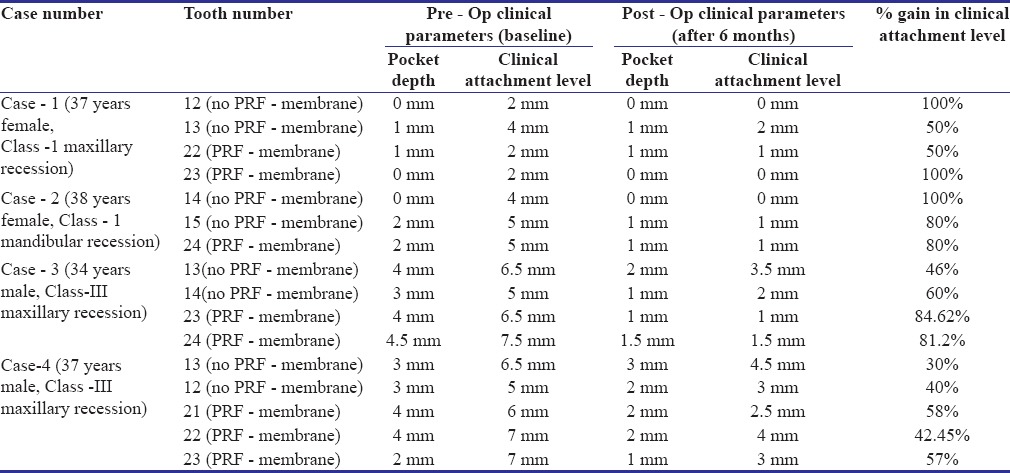
Table 2.
Comparison of clinical parameters between baseline and 6month post-operatively
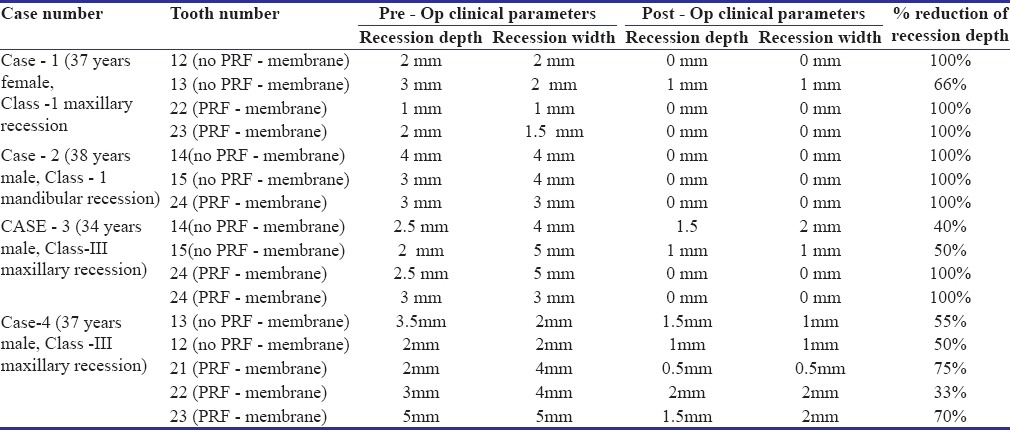
Figure 4.
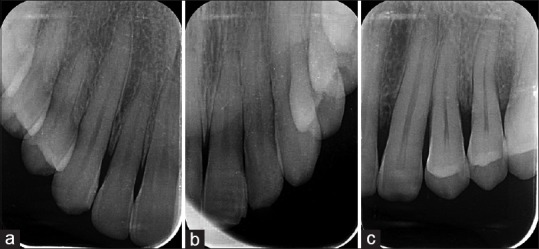
Radiographs Cases I and III
Clinical procedure
CRC protocol was explained to the willing patients and informed consent was taken. During the initials visits, complete scaling and root planning (SRP) was done in Cases I and II and SRP + curettage was done in Cases III and IV. After 15 days, patient was recalled and MRDs were treated with VISTA procedure with or without PRF on antagonist sites of the same arch. PRF membrane was prepared by squeezing the PRF clot procured through standard technique mentioned by Choukroun et al.[11] (centrifuge 10 ml of blood at 3000 rpm for 10 min) [Figure 5a]. After the surgery, repositioned gingival margin was stabilized through coronally anchor suture and composite resin button [Figure 2c and 5c]. Patient recalled after 10 days for suture removal and kept under observation and maintenance protocol for next 6 months.
Figure 5.
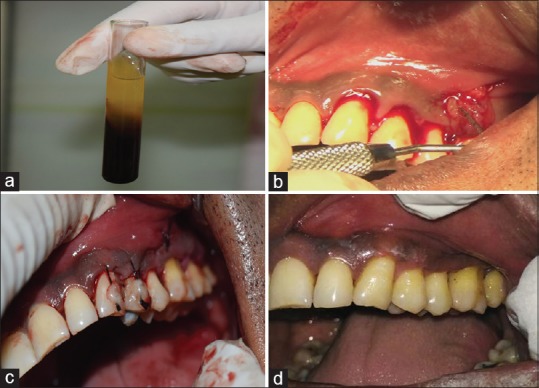
Vestibular incision subperiosteal tunnel access with platelet-rich fibrin membrane. (a) Preoperation of platelet-rich fibrin membrane (b) placement of platelet-rich fibrin membrane (c) suturing (d) 3 months postoperative
Surgical protocol
Bilateral recession defects had been surgical corrected using VISTA approach by a single operator on the same day. First, full thickness 8–10 mm vertical incision was given in the vestibule mesial or distal to the surgical site treated [Figure 3c]. This incision was not extended up to gingival margin and served as door for extension of subperiosteal tunnel. This tunnel exposes the osseous plate and extending by Orbans knife up to one or two teeth beyond the recession site undergoing surgical correction [Figures 2b and 3d]. Moreover, the subperiosteal tunnel was extended into interpapillary region without piercing the papillary tip. Slow apical movement of knife through papillary region commute to the vestibular tunnel and allow the coronal movement of mucogingival complex covering the MRDs.
This subpeiosteal tunnel was repositioned coronally and adapted passively to CEJ covering the recession defects. Coronal anchored sutures were placed engaging the 2–3 mm apical gingival margin of individual tooth using 4-0 silk suture. The suture was secured at the midcoronal point of the facial aspect of each tooth with the help of composite resin button to prevent apical relapse of the gingival margin. Once coronal stabilization was achieved, freshly prepared PRF membrane was inserted through the tunnel using the small periosteal elevator and spread it uniformly on recession defects [Figure 5b]. After complete and proper adaptation of the membrane the vertical incision was sutured for the primary closure [Figures 2c and 5c]. Complete surgical site was covered with Coe-pack [Figure 2c].
Postsurgical care
Postoperative instruction was given along with analgesic coverage and rinsing with Betadine gargle for 5 days. Patient was advised not to brush at the surgical site for next 1 month followed by gentle brushing in coronal direction till 6 months. In addition, patients were instructed to use 0.2% chlorhexidine rinses for next 21 days. These patients were kept on maintenance phase and recalled regularly [Figures 2d and 5d].
Results
All patients were cooperative, during the surgical hours and resulted in no postoperative discomfort. All selected sites remained plaque free with minimal gingival inflammation throughout the study. The recorded clinical parameters showed significant improvement in all cases.
Cases I and II of Class I MRDs are almost showed 100% coverage treated with VISTA approach with or without PRF-membrane. Meanwhile, Case III of mild chronic generalized periodontitis having multiple Class III recession defects showed 100% coverage with 80%–85% of CAL gain at site treated with VISTA + PRF-membrane as compared to sites treated with VISTA technique only displayed 50% coverage. Furthermore, Case IV of Class III recession diagnosed as a case of moderate chronic generalized periodontitis resulted in 70% root coverage on sites treated with VISTA + PRF-membrane rather than 50% coverage achieved by VISTA technique.
Discussion
GR exposes the root surface to oral environment leading to several complications. The right choice of treatment for the coverage of MRDs based on tooth anatomy, location of the tooth, measurement of the defect, gingival phenotype, and surgical skill to treat entire recession.[12] However, Chambrone et al. had reported that CAF with subepithelial connective tissue graft is gold standard for achieving CRC in maximum cases being treated of multiple recessions defects.[5]
VISTA is modified CAF introduced by Zadah et al. in 2011 for coverage of Class I multiple maxillary recession defects.[6] Grafting serve as a scaffold to support wound healing and provide better root coverage. Thus, this technique was further reinforced by PRF-membrane to increase and improve the width and thickness of keratinized gingiva for the treatment of Classes I and II recession defects.[9] Moreover, we opted only for this membrane since it is cost-effective and does not elicit any immune reaction at the surgical site. However, a systematic review by Moraschini et al. on PRF reinforced recession coverage refused any added effect of PRF-membrane for recession coverage. Hence, there is a need to compare the multiple Classes I and II recession coverage with or without PRF-membrane. We also included bilateral Class III recession defects in our series since these patients had severe hypersentivity and wanted the treatment only for the same without undergoing multiple sitting periodontal flap surgeries.
These patients were recalled regularly but final treatment outcome were compared only after 6 months from baseline as Pini-Prato et al.[13] has suggested some creeping attachment 6 months postoperatively. Each Class I recession defects in this series exhibited 100% coverage either treated with PRF or without PRF-membrane. This CRC might be attributed to maintaining standard protocol of patient selection, good gingival biotype, skilled handling of the tissue, and passive adaptation of the gingival margin to CEJ. These results advocate the applicability of VISTA technique alone provided no added advantage with PRF-membrane as suggested by Thamaraiselvan et al.[14] and Gupta et al.[15] in the treatment of multiple Classes I and II recession defects with CAF + PRF-membrane. The Class I recession cases in this series treated almost identical to Chenchev et al.[16] and Gupta et al.[9] with VISTA in combination to PRF-membrane, but 6 months postoperative results were not comparable to our study. However, PRF-membrane might be a stimulus for earlier healing response and able to attained adequate gingival thickness which was not considered in our protocol and is a drawback while doing this study.
Multiple Miller's Class III treated recession defects showed significant reduction in pocket probing depth and gain in CAL. Moreover, reduction in recession depth after manipulation of gingival margin with VISTA alone was 40%–50%, but in combination with PRF-membrane, it ranges from 50% to 80% depending on the severity of periodontal involvement of the tissue. The final gingival margin stabilization was also altered by patient's brushing technique[17] and length of the PRF-membrane.[18] This membrane is a meshwork of fibrin maintaining bed for leukocytes and platelets and releases the growth factors over a period. Moreover, it stimulates connective tissue cells leading to reduction in PD and resulted in maximum recession coverage even in the cases of Class III recession defects. These results approaches the outcome achieved by VISTA + collagen membrane,[9] connective tissue graft in treatment of multiple Class I recession defects. However, more studies with other cost-effective materials and larger sample size are still required for the treatment of Class III recession defects.
Thus, overall VISTA alone or in combination with PRF-membrane is a predictable and inexpensive approach for the treatment of Class I as well as Class III MRDs. The use of membranes including PRF as a scaffold for treatment of Class I recession defects improve the gingival phenotype and provide long-term stability in term of reduction of recession depth. These two cases treated for Class III recession depth conclude that addition of PRF-membrane resulted in a significant gain in CAL and better recession coverage outcome as compared to VISTA alone. However, more studies with large sample size and long follow-up are still required.
Conclusion
VISTA alone is a successful approach for treatment of Class- I and II multiple recession defects. Moreover along with PRF - membrane, this was proven quite well for treatment of class - III recession defects. However, more studies with more sample size are mandatory to conclude the outcome of this approach.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.American Academy of Periodontology. Glossary of Periodontal Terms. 3rd ed. Chicago: American Academy of Periodontology; 1992. [Google Scholar]
- 2.Chan HL, Chun YH, MacEachern M, Oates TW. Does gingival recession require surgical treatment? Dent Clin North Am. 2015;59:981–96. doi: 10.1016/j.cden.2015.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chambrone L, Sukekava F, Araújo MG, Pustiglioni FE, Chambrone LA, Lima LA. Root-coverage procedures for the treatment of localized recession-type defects: A Cochrane systematic review. J Periodontol. 2010;81:452–78. doi: 10.1902/jop.2010.090540. [DOI] [PubMed] [Google Scholar]
- 4.Aroca S, Keglevich T, Barbieri B, Gera I, Etienne D. Clinical evaluation of a modified coronally advanced flap alone or in combination with a platelet-rich fibrin membrane for the treatment of adjacent multiple gingival recessions: A 6-month study. J Periodontol. 2009;80:244–52. doi: 10.1902/jop.2009.080253. [DOI] [PubMed] [Google Scholar]
- 5.Chambrone LA, Chambrone L. Subepithelial connective tissue grafts in the treatment of multiple recession-type defects. J Periodontol. 2006;77:909–16. doi: 10.1902/jop.2006.050249. [DOI] [PubMed] [Google Scholar]
- 6.Zadeh HH. Minimally invasive treatment of maxillary anterior gingival recession defects by vestibular incision subperiosteal tunnel access and platelet-derived growth factor BB. Int J Periodontics Restorative Dent. 2011;31:653–60. [PubMed] [Google Scholar]
- 7.Aroca S, Keglevich T, Nikolidakis D, Gera I, Nagy K, Azzi R, et al. Treatment of class III multiple gingival recessions: A randomized-clinical trial. J Clin Periodontol. 2010;37:88–97. doi: 10.1111/j.1600-051X.2009.01492.x. [DOI] [PubMed] [Google Scholar]
- 8.Modaressi M, Wang HL. Tunneling procedure for root coverage using acellular dermal matrix: A case series. Int J Periodontics Restorative Dent. 2009;29:395–403. [PubMed] [Google Scholar]
- 9.Gupta G, Puri K, Bansal M, Khatri M, Kumar A. Platelet-rich fibrin reinforced vestibular incision subperiostal tunel access (VISTA) technique for recession coverage. Clin Adv Periodontics. 2014;7:1–13. [Google Scholar]
- 10.Moraschini V, Barboza Edos S. Use of platelet-rich fibrin membrane in the treatment of gingival recession: A systematic review and meta-analysis. J Periodontol. 2016;87:281–90. doi: 10.1902/jop.2015.150420. [DOI] [PubMed] [Google Scholar]
- 11.Choukroun J, Adda F, Schoeffler C, Vervelle A. An opportunity in perioimplantology: The PRF (in French) Implantodontie. 2001;42:55–62. [Google Scholar]
- 12.Cetiner D, Bodur A, Uraz A. Expanded mesh connective tissue graft for the treatment of multiple gingival recessions. J Periodontol. 2004;75:1167–72. doi: 10.1902/jop.2004.75.8.1167. [DOI] [PubMed] [Google Scholar]
- 13.Pini-Prato GP, Cairo F, Nieri M, Franceschi D, Rotundo R, Cortellini P. Coronally advanced flap versus connective tissue graft in the treatment of multiple gingival recessions: A split-mouth study with a 5-year follow-up. J Clin Periodontol. 2010;37:644–50. doi: 10.1111/j.1600-051X.2010.01559.x. [DOI] [PubMed] [Google Scholar]
- 14.Thamaraiselvan M, Elavarasu S, Thangakumaran S, Gadagi JS, Arthie T. Comparative clinical evaluation of coronally advanced flap with or without platelet rich fibrin membrane in the treatment of isolated gingival recession. J Indian Soc Periodontol. 2015;19:66–71. doi: 10.4103/0972-124X.145790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gupta S, Banthia R, Singh P, Banthia P, Raje S, Aggarwal N. Clinical evaluation and comparison of the efficacy of coronally advanced flap alone and in combination with platelet rich fibrin membrane in the treatment of Miller Class I and II gingival recessions. Contemp Clin Dent. 2015;6:153–60. doi: 10.4103/0976-237X.156034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chenchev IV, Atanasov D, Vicheva D, Noncheva V. Comparative evaluation of the subjective results from the treatment of gingival recessions with connective tissue graft and platelet rich fibrin membrane. IOSR J Dent Med Sci. 2016;15:73–8. [Google Scholar]
- 17.Wennström JL, Zucchelli G. Increased gingival dimensions. A significant factor for successful outcome of root coverage procedures?. A 2-year prospective clinical study. J Clin Periodontol. 1996;23:770–7. doi: 10.1111/j.1600-051x.1996.tb00608.x. [DOI] [PubMed] [Google Scholar]
- 18.Del Corso M, Sammartino G, Dohan Ehrenfest DM. Re: Clinical evaluation of a modified coronally advanced flap alone or in combination with a platelet-rich fibrin membrane for the treatment of adjacent multiple gingival recessions: A 6-month study. J Periodontol. 2009;80:1694–7. doi: 10.1902/jop.2009.090253. ccd_142_17R3. [DOI] [PubMed] [Google Scholar]


