Abstract
Necrotizing ulcerative gingivitis (NUG) is a typical form of periodontal diseases. It has an acute clinical presentation with the distinctive characteristics of rapid onset of interdental gingival necrosis, gingival pain, bleeding, and halitosis. Systemic symptoms such as lymphadenopathy and malaise could be also found. There are various predisposing factors such as stress, nutritional deficiencies, and immune system dysfunctions, especially, HIV infection that seems to play a major role in the pathogenesis of NUG. The treatment of NUG is organized in successive stages: first, the treatment of the acute phase that should be provided immediately to stop disease progression and to control patient's feeling of discomfort and pain; second, the treatment of the preexisting condition such as chronic gingivitis; then, the surgical correction of the disease sequelae like craters. Moreover, finally, maintenance phase that allows stable outcomes. This case report describes the diagnosis approach and the conservative management with a good outcome of NUG in a 21-year-old male patient with no systemic disease and probable mechanism of pathogenesis of two predisposing factors involved.
Keywords: Diagnosis, necrotizing periodontal diseases, necrotizing ulcerative gingivitis, treatment
Introduction
Necrotizing ulcerative gingivitis (NUG) is a distinct and specific form of periodontal diseases. It has an acute clinical presentation with the distinctive characteristics of rapid onset of gingival pain, interdental gingival necrosis, and bleeding.[1]
NUG has been recognized for centuries. It has been given many names: Vincent's disease, fusospirochetal gingivitis, trench mouth, acute ulcerative gingivitis, necrotizing gingivitis, and acute NUG.[1]
NUG was classically seen among military personnel during World War I, presumably due to multiple risk factors including poor oral hygiene, intense psychological stress, and malnutrition.[2]
Since then, it has appeared at much lower rates in the general population. However, it increased later on in patients with an immunocompromised condition, especially HIV-infected patients. Hence, authors (Rowland, 1999) reported that NUG may be the first sign of HIV infection.[1,2,3]
Actually and according to the recent data, the prevalence rate of NUG varies over a wide range from 6.7% in Chilean students between 12 and 21 years (Lopez et al. 2002)[4] to 0.11% in the British Armed Forces (Dufty et al. 2017).[5]
Other factors such as tobacco smoking,[3] preexisting gingivitis, and trauma have been reported as predisposing factors of NUG.[1,6]
NUG can heal without clinical sequelae.[7] Indeed, a dramatic resolution of signs and symptoms of NUG can be reached by medical treatment, mechanical debridement, or both.[1]
In this case report, we present a diagnostic, therapeutic approach and successful outcomes of a localized form of ulcerative necrotizing gingivitis.
Case Report
A 21-year-old male patient, with painful gingival inflammation evolving since 4 days, consulted urgently the Department of Periodontology, Faculty of Dentistry, University of Hassan II Morocco, in March 2015.
The patient reported that he had taken some medicines such as antiviral treatment (acyclovir) and anti-inflammatory drugs (diclofenac).
He had a poor plaque control without any parafunction and was a nonsmoker.
He had no other significant medical history or known allergies.
He had also a stressful job; he worked as a model and was under a severe diet.
The patient reported subjective malaise, chills, and difficulty in eating due to the intensive pain. We also noted during physical examination a thin, febrile, tired male, but no adenopathy was noted on cervical ganglionic area examination.
The clinical examination revealed a halitosis, erythematous, and swelling gingiva localized at the buccal side of the upper central, the upper, and lower lateral incisors and canines.
A pseudomembrane formation along the gingival margins and decapitated ulcerated papillae were also noted [Figures 1–3].
Figure 1.

Baseline front view
Figure 3.

Baseline right view
Figure 2.

Baseline left side view
A suitable probing was done seven days after emergency treatment, neither pockets nor attachment loss were found, especially on the upper anterior teeth.
X-ray examination showed a generalized periodontal ligament enlargement, a passive eruption of the right maxillary canine, an idiopathic root resorption of the lower incisors, and a marginal alveolar bone loss in the lower central incisors which might be due to occlusal trauma [Figure 4].
Figure 4.
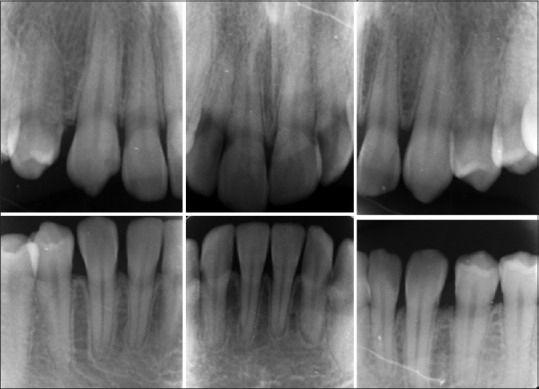
Baseline periapical radiographs
Laboratory HIV test was done, and the result was negative [Figure 5]. The diagnosis was established a NUG. The treatment was undertaken urgently: A 10 volumes diluted hydrogen peroxide was gently applied to the necrotic pseudomembranous lesions using sterile swabs in conjunction with suitable ultrasonic supragingival debridement. The patient was prescribed oral antibiotic (250 mg metronidazole every 8 h for 7 days) and oral mouth rinse (0.12% chlorhexidine twice daily for 10 days). The gingiva state was evaluated 2 days [Figure 6] and 7 days after [Figure 7] the clinical examination showed a major improvement in symptoms with almost complete resolution of the ulcerated pseudomembranous areas and reduction of erythema and swelling, and then, a subgingival debridement was conducted. In the context of global periodontal approach, gingivectomy was done in the right maxillary canine 23 [Figure 8] 2 months after healing. The patient was seen regularly, once a month. A favorable evolution was noted without any tissue sequelae but rather with the obtention of a symmetrical and homogeneous architecture of the healing gingiva [Figure 9].
Figure 5.
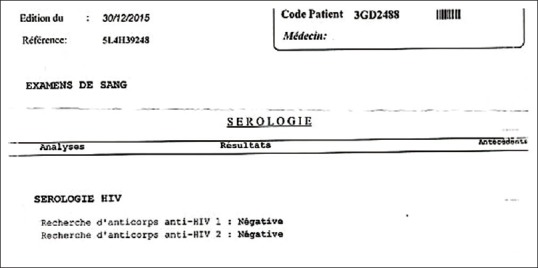
Laboratory HIV-test result
Figure 6.

Front view 2 days after emergency treatment
Figure 7.

Front view 7 days after emergency treatment
Figure 8.

Gingivectomy on the tooth 23
Figure 9.

Final front view 9-month posttreatment
Discussion
NUG was classified in several classification systems: in 1993, the World Health Organization included NUG in addition to necrotizing ulcerative periodontitis (NUP) and linear gingival erythema in the group of periodontal disease-related pathologies in HIV-positive patients.[8] After that, and according to the 1999 American Academy of Periodontics classification system, NUG was classified as necrotizing periodontal disease, with NUP. This suggestion was made since NUG and NUP might possibly be different stages of the same infection.[3,8] In 2002, Holmstrup and Westergaard proposed another classification that includes three distinct illnesses within the umbrella term of necrotizing periodontal disease: necrotizing gingivitis, when only the gum is affected; necrotizing periodontitis, if periodontal attachment tissue is also lost; and necrotizing stomatitis if the tissues involved lie beyond the mucogingival border.[8]
The diagnosis of NUG must be made fundamentally according to the presence or absence of primary clinical symptoms; the interproximal gingival necrosis often described by “punched out,” gingival bleeding with little or no provocation, and intensive pain which is a hallmark of this gingival lesion,[1,3,6] However it was found in an old data (Barnes et al 1973) that 14% of cases of acute NUG had no pain and another 40% suffered only mild pain. (Barnes et al. 1973).[9] Fetid breath or “fetor ex ore” and pseudomembrane formation may be secondary diagnostic features.[1,3,6,10] Systemic signs and symptoms as lymphadenopathy, fever, and malaise have been also reported to occur in NUG.[1,6,10] However, lymphadenopathy is an infrequent finding. Its presence is probably related to the severity of the disease since it is usually observed in advanced cases.[1] In this case report, all primary, secondary, and systemic clinical symptoms are present except lymphadenopathy, and this indicates the less severity of the case. The typically clinical appearance of NUG is related to its histopathological aspect. Four different layers have been described from the most superficial to the deepest layers of the lesion (Listgarten et al. 1965):
The bacterial area with a superficial fibrous mesh composed of degenerated epithelial cells, leukocytes, cellular rests, and a wide variety of bacterial cells, including rods, fusiforms, and spirochetes
The neutrophil-rich zone composed of a high number of leukocytes, especially neutrophils, and numerous spirochetes of different sizes and other bacterial morphotypes located between the host cells
The necrotic zone, containing disintegrated cells, together with medium- and large-size spirochetes and fusiform bacteria
The spirochetal infiltration zone, where the tissue components are adequately preserved but are infiltrated with large- and medium-size spirochetes. Other bacterial morphotypes are not found.
The microbiota composition associated with NUG and found in lesion layers includes Treponema spp., Selenomonas spp., Fusobacterium spp., and Prevotella intermedia. Other microorganisms have also been described, although these were defined as “variable” flora and were not present in all cases (Loesche et al. 1982).[11] As this typical microbiological description can also be detected in healthy, gingivitis, or periodontitis sites, the use of microbiological testing does not provide relevant diagnostic information.[7,10] NUG diagnosis may be mainly confused with some viral infections as acute herpetic gingivostomatitis and infectious mononucleosis, with bacterial infections like gonococcal or streptococcal gingivitis, and also with some mucocutaneous conditions as desquamative gingivitis, multiform erythema, pemphigus vulgaris, and others.[8,10] In the present case report, the diagnosis clinical features are evident, and the differential diagnosis might be made with acute herpetic gingivostomatitis or recurrent intraoral herpes. That might explain why the patient took antiviral drugs. The predisposing factors play a main role on NUG by the downregulation of the host immune response facilitating bacterial pathogenicity, these factors include: psychological stress and insufficient sleep, poor diet, alcohol and tobacco consumption, inadequate oral hygiene, preexisting gingivitis, and systemic condition especially HIV infection.[1,3,7,10] However, according to the recent study, diabetes was discovered to be an important predictor,[4] and it is presumably due to multiple aspects of the diabetic state including microangiopathy, delayed wound healing, impaired function of neutrophils, and disturbances in collagen formation due to glycation.[2] In the present case report, two NUG risk factors were highlighted: severe diet and psychological stress due to trying to keep an icon physical appearance. The proposed mechanisms to explain the association between psychological stress and NUG are based on reductions of the gingival microcirculation and salivary flow, increases in adrenocortical secretions which are associated with an alteration in the function of polymorphonuclear leukocytes and lymphocytes.[1,7,12,13] Besides, psychological stress alters not only the immune response but also the patient's behavior and mood, leading to inadequate oral hygiene, malnutrition, or increased tobacco consumption.[7,12] Regarding the poor diet, decreasing dietary protein results in an increase in histamine concentration and that leads to a hyperemia of the gingival due to increased capillary permeability and decreased polymorphonuclear leukocytes chemotaxis.[12] The treatment of NUG should be organized in successive stages: first, treatment of the acute phase; second, treatment of the preexisting condition; then, corrective treatment of the disease sequelae. Moreover, finally, supportive or maintenance phase. Treatment of the acute phase has two main objectives of therapy: to stop the disease process and tissue destruction and to control the patient's general feeling of discomfort and pain that interfere with nutrition and oral hygiene practices. These targets can be achieved by a careful superficial ultrasonic debridement and chemical detersion of the necrotic lesions with oxygen-releasing agents “local oxygen therapy.” The use of systemic antimicrobials may be considered in cases that show unsatisfactory response to debridement or show systemic effects (fever and/or malaise). Metronidazole (250 mg, every 8 h) may be an appropriate first choice of drug because it is active against strict anaerobes.[7,8] Other systemic drugs have also been suggested, with acceptable results, including penicillin, tetracyclines, clindamycin, amoxicillin, or amoxicillin plus clavulanate.[7] Conversely, locally delivered antimicrobials are not recommended because of the large numbers of bacteria present within the tissues, where the local drug will not be able to achieve adequate concentrations.[7] Antifungal agents are, especially, indicated in immunodepressed patients who are undergoing antibiotic therapy.[8] Once the acute phase has been controlled, treatment of the preexisting chronic condition, such as preexisting chronic gingivitis, should be started, including professional prophylaxis and/or scaling and root planning. Oral hygiene instructions and motivation should be enforced. Existing predisposing local factors, such as overhanging restorations and interdental open spaces, should be carefully evaluated and treated. Systemic predisposing factors including smoking, adequate sleep, and reduction of stress should be controlled and taken into consideration.[7,8] Sometimes, the correction of the altered gingival topography caused by the disease should be considered because gingival craters may favor plaque accumulation and disease recurrence. Gingivectomy and/or gingivoplasty procedures may be helpful for treatment of superficial craters; periodontal flap surgery, or even regenerative surgery, is more suitable options for deep craters or for NUP.[7,8] Finally, if proper maintenance is not carried out, relapses are likely to occur that may lead to a loss of attachment. Moreover, the main goal of this phase is complying with the oral hygiene practices and controlling the predisposing factors.[7,8] In the present clinical case, a satisfactory response to local and systemic treatment was obtained without any gingival sequelae. Controversially, a quick healing and spectacular papilla regeneration was achieved leading to an esthetic final result. A gingivectomy on 23 was done just to have a more esthetic symmetric gingival line. Furthermore, Patient compliance is satisfactory, he has a good plaque control and respects the appointments of controls and still on maintenance phase. The patient compliance was a positive factor in the favorable evolution of the clinical outcome.
Conclusion
NUG is a specific acute periodontal disease. The diagnosis seems evident according to the three typical clinical features as papilla necrosis, bleeding, and pain on the one hand and the identification of risk factors that alter the host response on the other hand. Treatment should be organized on successive steps, and the acute phase treatment should be provided immediately to prevent sequelae and craters in soft tissues that will lead to new relapses. Finally, a good compliance with the oral hygiene practices and maintenance do guarantee better and stable outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank the patient in this report for help and his good compliance till today.
Each author listed on the manuscript has significantly contributed and approved the submission of this version of the manuscript and takes full responsibility for the manuscript.
References
- 1.Rowland RW. Necrotizing ulcerative gingivitis. Ann Periodontol. 1999;4:65–73. doi: 10.1902/annals.1999.4.1.65. [DOI] [PubMed] [Google Scholar]
- 2.Hu J, Kent P, Lennon JM, Logan LK. Acute necrotising ulcerative gingivitis in an immunocompromised young adult. BMJ Case Rep 2015. 2015 doi: 10.1136/bcr-2015-211092. pii: Bcr2015211092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Niklaus Lang, Soskolne WA, Gary Greenstein, David Cochran, Esmonde Corbet, Huan Xin Meng, et al. Consensus Report: Necrotizing Periodontal Diseases. Annals of Periodontology. 1999;4:78. [Google Scholar]
- 4.Lopez R, Fernandez O, Jara G, Baelum V. Epidemiology of necrotizing ulcerative gingival lesions in adolescents. J Periodontal Res. 2002;37:439–44. doi: 10.1034/j.1600-0765.2002.01377.x. [DOI] [PubMed] [Google Scholar]
- 5.Dufty J, Gkranias N, Petrie A, McCormick R, Elmer T, Donos N. Prevalence and treatment of necrotizing ulcerative gingivitis (NUG) in the British Armed Forces: A case-control study. Clin Oral Investig. 2017;21:1935–44. doi: 10.1007/s00784-016-1979-9. [DOI] [PubMed] [Google Scholar]
- 6.Atout RN, Todescan S. Managing patients with necrotizing ulcerative gingivitis. J Can Dent Assoc. 2013;79:d46. [PubMed] [Google Scholar]
- 7.Herrera D, Alonso B, de Arriba L, Santa Cruz I, Serrano C, Sanz M. Acute periodontal lesions. Periodontol 2000. 2014;65:149–77. doi: 10.1111/prd.12022. [DOI] [PubMed] [Google Scholar]
- 8.Bermejo-Fenoll A, Sánchez-Pérez A. Enfermedades periodontales ne- crosantes. Med Oral Patol Oral Cir Bucal. 2004;9 Suppl:S108–19. [PubMed] [Google Scholar]
- 9.Barnes GP, Bowles WF, Carter HG. Acute necrotizing ulcerative gingivitis: A survey of 218 cases. J Periodontol. 1973;44:35–42. doi: 10.1902/jop.1973.44.1.35. [DOI] [PubMed] [Google Scholar]
- 10.Folayan MO. The epidemiology, etiology, and pathophysiology of acute necrotizing ulcerative gingivitis associated with malnutrition. J Contemp Dent Pract. 2004;5:28–41. [PubMed] [Google Scholar]
- 11.Loesche WJ, Syed SA, Laughon BE, Stoll J. The bacteriology of acute necrotizing ulcerative gingivitis. J Periodontol. 1982;53:223–30. doi: 10.1902/jop.1982.53.4.223. [DOI] [PubMed] [Google Scholar]
- 12.Folayan MO. The epidemiology, etiology, and pathophysiology of acute necrotizing ulcerative gingivitis associated with malnutrition. J Contemp Dent Pract. 2004;5:28–41. [PubMed] [Google Scholar]
- 13.Shah R, Kumbhalwar A, Vyas K, Raval C, Kothari R, Jinwala M. Stress and periodontal disease: A review. J Adv Med Dent Sci Res. 2016;4:57–9. [Google Scholar]


