Abstract
Background & objectives:
Cardiovascular disease (CVD) risk with low high-density lipoprotein cholesterol (HDL-C) and high triglycerides is common in the general population in India. As nevirapine (NVP)-based antiretroviral therapy (ART) tends to increase HDL-C, gene polymorphisms associated with HDL-C metabolism in HIV-infected adults on stable NVP-based ART were studied.
Methods:
A cross-sectional study was conducted between January 2013 and July 2014 among adults receiving NVP-based ART for 12-15 months. Blood lipids were estimated and gene polymorphisms in apolipoprotein C3 (APOC3), cholesteryl ester transfer protein (CETP) and lipoprotein lipase (LPL) genes were analyzed by real-time polymerase chain reaction. Framingham's 10-yr CVD risk score was estimated. Logistic regression was done to show factors related to low HDL-C levels.
Results:
Of the 300 patients included (mean age: 38.6±8.7 yr; mean CD4 count 449±210 cell/μl), total cholesterol (TC) >200 mg/dl was observed in 116 (39%) patients. Thirty nine per cent males and 47 per cent females had HDL-C levels below normal while 32 per cent males and 37 per cent females had TC/HDL ratio of 4.5 and 4.0, respectively. Body mass index [adjusted odds ratio (aOR)=1.70, 95% confidence interval (CI) 1.01-2.84, P=0.04] and viral load (aOR=3.39, 95% CI: 1.52-7.52, P=0.003) were negatively associated with serum HDL-C levels. The 10-yr risk score of developing CVD was 11-20 per cent in 3 per cent patients. Allelic variants of APOC3 showed a trend towards low HDL-C.
Interpretation & conclusions:
High-risk lipid profiles for atherosclerosis and cardiovascular disease were common among HIV-infected individuals, even after 12 months of NVP-based ART. Targeted interventions to address these factors should be recommended in the national ART programmes.
Key words: Antiretroviral therapy, body mass index, gene polymorphisms, high-density lipoprotein-cholesterol, HIV, nevirapine, viral load
Long-term use of antiretroviral therapy (ART) has reduced the morbidity and mortality due to HIV infection but has also led to dyslipidaemia, characterized by an increase in levels of total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), triglycerides (TG) and varying effect on high-density lipoprotein cholesterol (HDL-C)1,2,3. Alterations in these lipid levels may lead to an increased risk of cardiovascular disease (CVD), observed in both developed and resource-limited settings3,4. The changes seen in lipid levels appear to be related to both drug classes [nucleoside reverse transcriptase inhibitors (NRTIs) and non-nucleoside reverse transcriptase inhibitors (NNRTIs)] and specific agents [zidovudine and nevirapine (NVP)]5,6. For example, NVP-based regimens show larger increases in HDL-C and relative decreases in TC:HDL-C ratio than efavirenz-containing regimens and thus could be associated with a lower atherogenic lipid profile7.
HDL, a lipoprotein responsible for the efflux and transport of blood cholesterol, plays an essential role in preventing atherosclerosis and cardiovascular events8. A low level of HDL-C has been shown to be a risk factor for CVD in general population9. Both HIV infection and ART can influence HDL-C levels, with NVP being associated with greater increase in HDL-C levels than efavirenz6,10. At the same time, strong genetic influence also exists on plasma HDL-C levels. Defects in the genes coding for cholesteryl ester transfer protein (CETP), lipoprotein lipase (LPL), apolipoprotein A1, lecithin cholesterol aceyltransferase (LCAT), etc. can result in large changes in HDL-C levels as does apolipoprotein C3 (APOC3) for cholesterol8,11,12. APOC3 promoter polymorphism is also associated with a greater likelihood of metabolic syndrome and dyslipidaemia, especially higher TG and lower HDL-C, among Indian population as well, after controlling for age, race and gender13,14,15. Though functional defects of these genes are rare in the general population and mostly concern only small numbers of patients, premature truncation of the LPL protein (447 stop), polymorphism in CETP (rs4329913 and rs7202364) gene and APOC3 promoter variant (C-482T and T-455C) have been shown to be relatively frequent and account for significant changes in lipid levels in various groups of population16,17.
The high degree of risk for CVD in Indians is characterized by various combinations of either hypertriglyceridaemia with low HDL cholesterol or an increase in TC, LDL cholesterol and TC/HDL ratio18,19. Studies have shown significantly lower HDL-C among HIV-positive as compared to HIV-negative individuals (43 vs. 75%, P <0.001), especially in treatment-naïve HIV-infected individuals with low CD4 cell counts20,21,22. With immunological restoration following initiation of ART, HDL-C returns to normal range. However, we have previously reported that almost 25 per cent of HIV-infected adults have lower levels of HDL-C even after 12 months of NNRTI-based ART23. This study was aimed to look at the factors and impact of certain baseline characteristics, CVD risk scores as well as polymorphisms in APOC3, CETP and LPL genes on lipid profile of HIV-infected adults after 12-15 months of NVP-based ART.
Material & Methods
A cross-sectional study was conducted at the National Institute for Research in Tuberculosis, Chennai, India, between January 2013 and July 2014. HIV-infected adults of 18 yr and above, on an NVP-based ART regimen (dose of NVP: 200 mg twice a day along with two NRTI drugs) for the last 12-15 months, from ART centres in Government Hospital of Thoracic Medicine, Government General Hospital, Chennai, and Government Vellore Medical College and Hospital, Vellore, were approached for the participation in this study. Patients seriously ill, on efavirenz-based ART, had ART changed or interrupted for more than one month continuously any time during the preceding 18 months or on the second-line ART were not included in this study.
The Institutional Ethics committee of the National Institute for Research in Tuberculosis, Chennai, approved this study. Before enrolling into the study, informed written consent was obtained from all patients.
Study procedures
A detailed clinical, socio-demographic and personal history, including smoking and alcohol intake, was collected using a structured questionnaire. Details on drug adherence over the last one year was retrieved from patient's ART notebooks that had information on number of pills supplied, number of pills returned and number of missed doses and by a basic five-point Likert scale for self-rating of overall adherence as all the time (excellent), most of the time (very good), many times (good), occasionally (fair) and never.
Height, weight, mid-arm, waist and hip circumferences were measured. Blood pressure was recorded in the left arm in sitting posture. After an overnight fast, blood samples (10 ml) were collected for lipid profile which included TC, HDL-C, LDL-C, TG and blood glucose, measured by an automated analyzer (Olympus AU400, Japan). A 10-yr risk for coronary heart disease was estimated using the Framingham's Point scores24. Plasma samples were also subjected to viral load assay by Roche COBAS AmpliPrep/COBAS TaqMan HIV-1 Test v2.0 (USA) and CD4 cell counts by FACSCount flow cytometer (Becton Dickinson, USA). Participants were genotyped for the polymorphisms in APOC3 gene (rs2854116, rs2854117 and rs5128) by previously described primers using polymerase chain reaction (PCR) followed by sequencing assay14,25. The single nucleotide polymorphism (SNP) rs1800775 in CETP gene was determined by PCR and sequencing [primers 5'-AATGCCACAGACATTCCCCC-3' (forward), 5'-C GACCTTTCCCTTGCTCTGA-3' (reverse)] while CETP rs708272 (Taq1B) and LPL rs328 SNPs were analyzed by real-time PCR using TaqMan genotyping assay (Applied Biosystems, USA).
Study definitions
For this study, hypertriglyceridaemia was defined as fasting TG >150 mg/dl and hypercholesterolaemia as fasting cholesterol (TC) >200 mg/dl or LDL-C >130 mg/dl. HDL-C< 40 mg/dl for males and <50 mg/dl for females was defined as low HDL-C levels12. Patients were classified as hypertensive or diabetics if they had been previously diagnosed with hypertension or diabetes or if they were on medical treatment for these disorders. A TC/HDL ratio of 4.5 or below for men and 4.0 or below for women was considered acceptable. Body mass index (BMI) of >23 kg/m2 and waist circumference of >90 cm for men and >80 cm for women were considered as cut-offs for overweight and abdominal obesity, respectively, in this study26. After one year of ART, plasma viral load of <400 copies/ml was considered as virological suppression. Viral load between 400 and 1000 copies/ml was taken as blips while viral load >1000 copies/ml after one-year of ART was taken as virological failure.
Statistical analysis
Our previous study showed HDL-C levels below the lower limit of normal in about 25 per cent of HIV-infected Indians while on NNRTI-based ART23. Based on this, it was planned to enrol 300 HIV-infected patients after one year of ART, to determine the association between HDL-C levels, gene polymorphisms and other risk factors.
SPSS software version 19.0 (IBM Corp, Armonk, NY, USA) was used to perform the data analysis. The data set was checked for logical inconsistencies and omissions. All unusual values were verified; normal distribution was checked. The outcomes of interest included the lipid parameters: TC, LDL-C, HDL-C, TG and TC/HDL-C ratio. Summary statistics is presented as proportions for categorical variables and as mean with standard deviation (SD) for continuous variables. A univariate regression followed by binary logistic regression by stepwise method was constructed to look for factors independently associated with abnormal lipid profile. Adjusted odds ratio (aOR) with its 95 per cent confidence intervals (CIs) was obtained. Candidate SNPs were evaluated in a logistic regression model and mean lipid levels compared between the different allele groups using Tukey analysis of variance at 5 per cent level. Pearson's Chi-square statistics was used to compare the proportions of patients with abnormal lipid values.
Results
During the study period, 355 HIV-infected adults on NVP-based first-line ART for the past 12-15 months were screened for participation. Of them, 300 patients consented to participate in the study. Their mean age was 38.6±8.7 yr (range: 20-60 yr), mean CD4 cell count was 449±210 cell/μl and median duration of ART was 13.5 months (12-15 months); 26 per cent of the study participants were smokers; 53 per cent (159) were females (Table I). Eighty four per cent (252) had zidovudine, 8 per cent stavudine and another 8 per cent tenofovir as one of the nucleoside reverse transcriptase inhibitors in the regimen, along with lamivudine and NVP. The current National ART programme in India27 considers an optimum ART adherence level of ≥95 per cent. After one year of ART, overall adherence (based on the Likert scale of self-rating adherence) of >95 per cent was found in 72 per cent (n=216) of study participants. Another 22 per cent (n=65) were 80-95 per cent adherent to drugs. Virological suppression of <400 copies/ml was present in 89 per cent (n=268) of the patients. Three patients had viral load between 400 and 1000 copies/ml while 29 had viral load >1000 copies/ml after one year of ART.
Table I.
Demographic and clinical characteristics of the study participants on antiretroviral therapy (n=300)
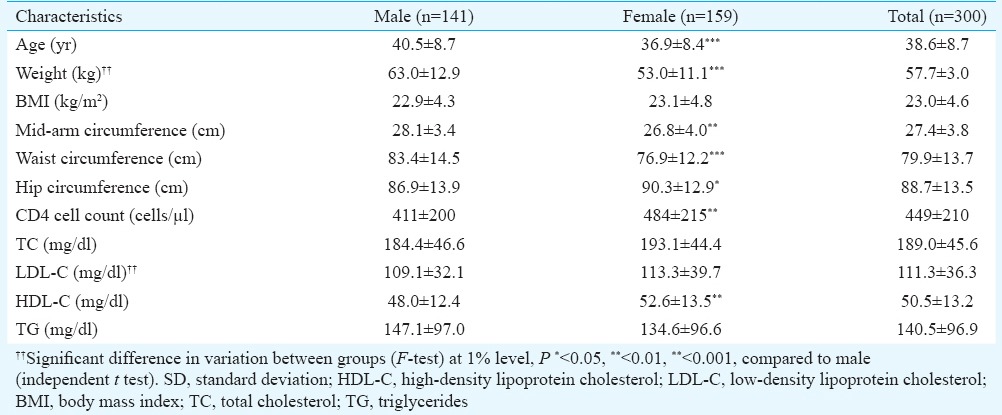
Lipid profile of participants
The mean serum TC was 189±45.6 mg/dl with hypercholesterolaemia in 116 (39%) patients (Figure). Thirty per cent of them had LDL-C of >150 mg/dl and the mean LDL-C was 111.3±36.3 mg/dl. Hypertriglyceridaemia was seen in 93 patients (31%) with mean TG level of 240.3±118.9 mg/dl. Forty one of 141 males (29%) had HDL-C <40 mg/dl while 75 of 159 females (47%) had HDL-C <50 mg/dl; 32 per cent of males and 37 per cent of females had TC/HDL-C ratio greater than the reference value of 4.5 and 4.0, respectively.
Figure.
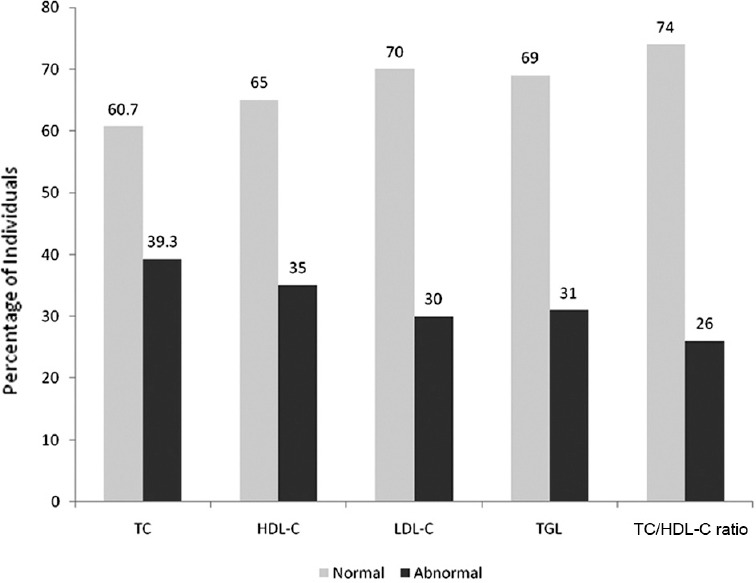
Prevalence of dyslipidaemia in HIV-infected patients on antiretroviral therapy. Abnormal cholesterol=Fasting cholesterol 200 mg/dl; Abnormal triglycerides (TG)=Fasting triglycerides >150 mg/dl. Abnormal high-density lipoprotein-cholesterol (HDL-C)= <40 mg/dl for male, <50 mg/dl for females; Abnormal Low-density lipoprotein-cholesterol (LDL-C) = >130 mg/dl and Abnormal total cholesterol (TC): HDL-C ratio = >4.5.
Factors associated with poor lipid profiles
In univariate analysis, weight >55 kg (OR=1.96, 95% CI: 1.23-3.14, P=0.005), waist circumference of >75 cm (OR=2.20, 95% CI: 1.32-3.66, P=0.002) and hip circumference >80 cm (OR=2.28, 95% CI: 1.16-4.47, P=0.017) and a detectable viral load were associated with TC level above the upper limit of normal (Table II). Similarly, weight >55 kg (OR=2.08, 95% CI: 1.26-3.41, P=0.004), mid-arm circumference >25 cm (OR=1.91, 95% CI: 1.09-3.35, P=0.025), waist circumference >75 cm (OR=3.21, 95% CI: 1.79-5.74, P=0.001) and waist:hip ratio >0.9 were associated with higher TG levels. BMI >23 kg/m2 appeared to be associated with a poorer lipid profile in terms of high TC, LDL-C, TG and higher TC/HDL-C ratio (Table II). Detectable viral load >400 copies/ml (OR=3.07, 95% CI: 1.45-6.52, P=0.002) while on treatment was significantly associated with higher odds of having abnormal HDL-C at end of one-year of ART. Alcohol consumption, higher BMI and waist circumference >75 cm were also associated with abnormal HDL-C after a year of ART though these did not reach significance. Men had a lower risk of having low HDL-C as compared to women in the similar age (OR=0.45, 95% CI 0.28-0.73, P=0.001) (Table II).
Table II.
Association of lipid profile and various factors in our study participants (n=300)
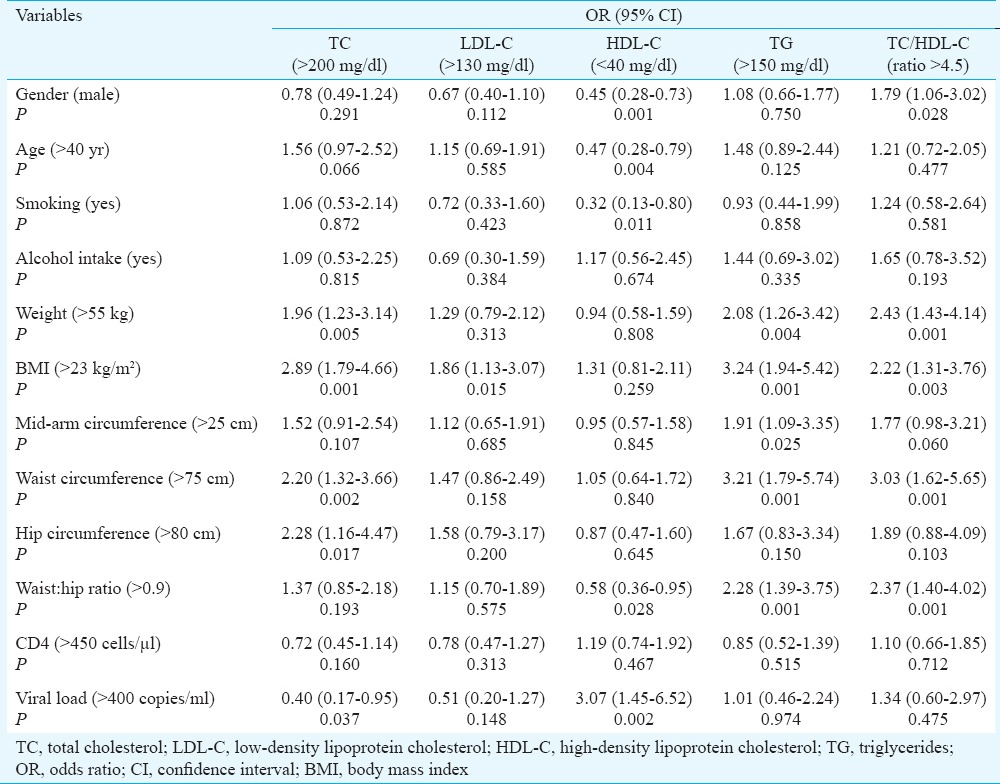
Considering gender, age, body weight, BMI, smoking status, alcohol use, waist and hip circumferences, CD4 cell count and viral load, using binary logistic regression by stepwise method, only BMI >23 kg/m2 had an independent and positive association with all abnormal serum lipid levels – TC >200 mg/dl [aOR (adjusted OR)=2.84, 95% CI: 1.76-4.60, P<0.001); LDL-C >130 mg/dl (aOR=1.83, 95% CI: 1.10-3.01, P=0.02], TGL >130 mg/dl (aOR=2.42, 95% CI: 1.37-4.28, P=0.002) and abnormal HDL-C (aOR=1.70, 95% CI: 1.02-2.84, P=0.04). High waist circumference had a positive association with TGL levels alone (aOR=2.13, 95% CI: 1.11-4.07, P<0.01), while detectable viral load was negatively associated with serum HDL-C levels (aOR=3.39, 95% CI: 1.53-7.52, P=0.003). Male gender was protective against low HDL-C in our study group (aOR 0.46, 95% CI: 0.28-0.78, P=0.003) (data not shown).
Framingham's cardiovascular risk score
The 10-yr risk of coronary heart disease was estimated using the Framingham's point score and 97 per cent (n=289) of patients had a risk of <10 per cent while 3 per cent of patients had 11-20 per cent risk of developing CVD at the end of one-year of ART.
Effect of single nucleotide polymorphisms (SNP) in various genes
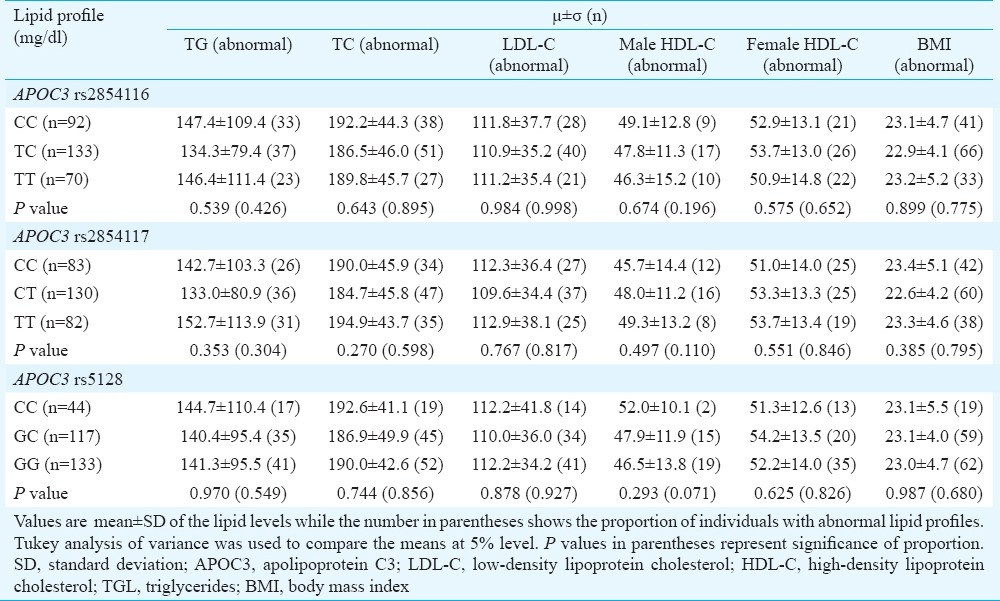
Apolipoprotein C3 (APOC3) gene polymorphisms
Homozygous carriers of C allele in rs2854116 and rs5128 displayed a trend towards higher lipid levels after 12 months of ART, when compared to heterozygous or non-carriers; in fact, the non-carriers of this allele had the lowest lipid levels among the three groups (Table IIIA). However, this difference was not significant. Further, among individuals with abnormal lipid profiles, there was no significant difference in the allelic frequencies of APOC3 related rs2854116, rs2854117 and rs5128 polymorphism (Table IIIA).
Table IIIA.
Lipid parameters between the genotype variants of apolipoprotein C3 related polymorphisms among 295 study participants
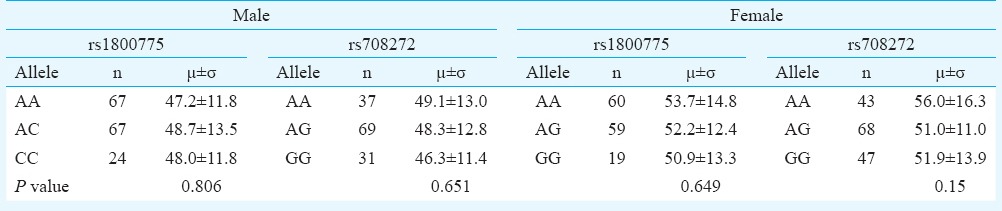
Cholesteryl ester transfer protein (CETP)-related polymorphisms
Homozygous carriers of A allele in rs708272 of CETP showed a trend towards a higher HDL-C as compared with subjects with GG genotype in both genders (Table IIIB). However, this difference was not significant.
Table IIIB.
Association between cholesteryl ester transfer protein (CETP) polymorphism and serum high-density lipoprotein cholesterol (HDL-C) levels
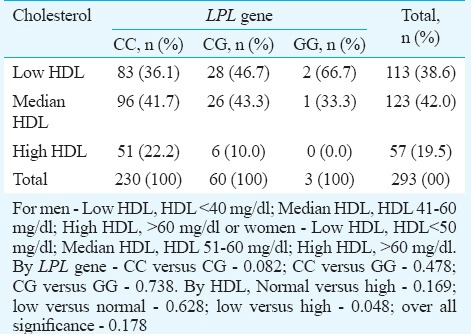
Lipoprotein lipase (LPL)-related polymorphisms
Proportion of various polymorphism of LPL gene in the low-, middle-, and upper-decile HDL-C levels did not show any significance in any particular group though a trend was seen in patients with homozygous carriers of C allele toward a low HDL-C (Table IIIC).
Table IIIC.
Association between lipoprotein lipase (LPL) polymorphism and serum high-density lipoprotein (HDL) cholesterol levels
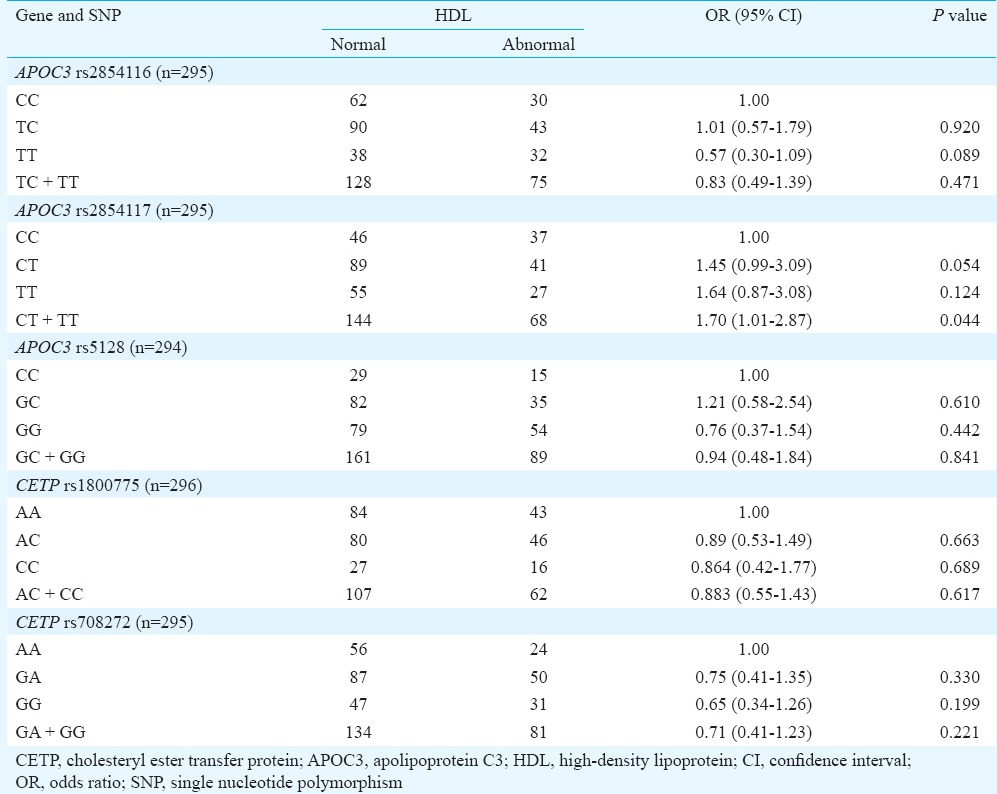
Only the heterozygous carriers of C allele in APOC3 rs2854117 (aOR1.45, 95% CI 0.99-3.09, P= 0.05) seemed to have a protective effect against abnormal HDL-C. None of the other SNPs of APOC3, CETP or LPL genes had any significant association with abnormal HDL-C (Table IV). In our study, 29 patients had detectable viral load and their drug adherence was <80 per cent. The analysis was repeated after excluding these 29 patients with virological failure, but no significant association was found with either APOC3, CETP or LPL gene polymorphisms or low HDL-C.
Table IV.
Association of genetic variants in genes associated with high-density lipoprotein (HDL)-cholesterol
Discussion
Our study revealed low HDL-C levels in 39 per cent HIV-infected patients receiving NVP-based first-line ART. Higher BMI and unsuppressed viral load were significantly associated with low levels of HDL-C after 12 months of NVP-based first-line ART. Hypercholesterolaemia (39%), raised levels of LDL-C (30%) and hypertriglyceridaemia (31%) were the other forms of dyslipidaemia seen.
Though high, occurrence of HDL-C levels below the reference value after one year of ART was much lower to the reported rate of 50.8 per cent in patients using HAART for at least six months in Ethiopia3. However, this was higher than that observed in a clinical trial cohort from the same setting as well as other studies from developing world17,22,23,28. Our patients were predominantly from a lower socio-economic background and from semi-urban setting and did not have high rates of obesity.
Multiple factors contribute to dyslipidaemia in HIV-infected individuals including HIV virus itself, chronic inflammation, individual genetic characteristics and ART-induced metabolic changes29. Higher BMI and waist circumference were associated with hypercholesterolaemia, hypertriglyceridaemia and low HDL-C levels emphasizing the potential role of lifestyle (diet and exercise) in this population. Lifestyle changes may be beneficial and can be recommended for patients on ART. Furthermore, suppressed viral load was a protective factor against low HDL-C levels. This negative association between viral load and HDL-C levels observed in our study has also been noticed in other studies, even in ART-naïve individuals, indicating the role of HIV infection per se casuing low HDL-C levels22,30,31. Hence, detectable viral load along with low HDL-C, in HIV-infected individual, after one year of stable ART, should raise the suspicion of non-adherence to ART even though the self-reporting indicates >95 per cent adherence.
A small number of patients in our study (n=8) had a 11-20 per cent 10-yr risk of developing coronary heart disease and all of them had low levels of HDL-C. Although this was a small number, all efforts should be made to normalize their HDL-C levels as for every one per cent increase in HDL-C, there is a three per cent reduction in death or myocardial infarction10. A study from north India has shown a greater prevalence of polymorphism in APOC3 promoter region (C-482T and T-455C) among non-HIV subjects with metabolic syndrome and dyslipidaemia as compared to controls (frequency of 71 and 82% vs. 43 and 54%, P=0.0001)13. However, we were not able to identify significant associations between the APOC3-related polymorphism and lipid parameters in our study. Homozygous carriers of C allele in rs5128 showed a trend towards more individuals with normal HDL-C levels when compared to heterozygous or non-carriers. Similar results have also been reported by a Spanish group where A allelic variant of the rs10892151 polymorphism was not found to be associated with serum APOC3 concentration but predisposes HIV-infected patients to less favourable lipid profile32. Considering the crucial role of CETP and LPL genes in lipid metabolism, the association of SNPs of these genes with low HDL-C levels was examined but no significant association between low HDL-C and gene polymorphisms was observed. A few other studies have shown an association between CETP and lipid metabolism16,33,34. The reports from India are varied as each has looked at different CETP polymorphisms and HDL-C metabolism35,36. In the study by Dixit et al36, lipid profile analysis did not show any significant difference in distribution among genotypes of CETP polymorphism among patients and controls. These contradictory results in different populations indicate that various mutation/polymorphisms of APOC3 and CETP are involved with HDL-C metabolism and more research is needed in this field.
A cross-sectional study design and a lack of control group were major limitations in this study. As we did not have baseline data on these individuals or a control group with similar baseline characters but without these changes at one year, we could not examine changes induced by ART use and what the baseline prevalence of dyslipidaemia was. No data were collected on dietary and other lifestyle factors that might have an impact on lipid profiles. The sample size was adequate for the lipid analysis, with a power >90 per cent, but may have been small to detect differences in gene polymorphisms.
In conclusion, our results indicated that a high proportion of HIV-infected patients had a low HDL-C level after one year of NVP-based ART. Association was found between NVP-based ART and high-risk lipid profiles for atherosclerosis and CVD raising concerns about their long-term morbidity. Targeted interventions such as periodic monitoring of lipid levels, dietary modification, physical exercise and good virological control need be recommended as part of the national ART programmes.
Acknowledgment
Authors thank the staff of the departments of Clinical Research (Ms. Ponghuzahli and Smt. Komathy), Biochemistry (Sarvshri S. Rajkumar and B. Anand Kumar), Biostatistics (Sarvshri Tamilchelvan and Kannan) and the HIV Laboratory (Dr Sudha Subramanian and Shri Murugesan) of the National Institute for Research in Tuberculosis, for their active participation in the study. Authors also thank Drs A. Raja, Vigila, Anadachitra and Aarthi, Senior ART medical officers and the staff of ART centres in Tambaram Sanatorium, Chennai and Vellore Government Hospitals for their support and cooperation and acknowledge all the patients who participated in this study. Financial support by the “Pilot Project: Brown Tufts Fogarty AIDS International Training and Research Program” (NIH Grant No. D43TW00237, CFDA Number 93.989) is acknowledged.
Footnotes
Conflicts of Interest: None.
References
- 1.Pere D, Ignacio SL, Ramón T, Fernando L, Alberto T, Pompeyo V, et al. Dyslipidemia and cardiovascular disease risk factor management in HIV-1-infected subjects treated with HAART in the Spanish VACH cohort. Open AIDS J. 2008;2:26–38. doi: 10.2174/1874613600802010026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chêne G, Angelini E, Cotte L, Lang JM, Morlat P, Rancinan C, et al. Role of long-term nucleoside-analogue therapy in lipodystrophy and metabolic disorders in human immunodeficiency virus-infected patients. Clin Infect Dis. 2002;34:649–57. doi: 10.1086/338811. [DOI] [PubMed] [Google Scholar]
- 3.Abebe M, Kinde S, Belay G, Gebreegziabxier A, Challa F, Gebeyehu T, et al. Antiretroviral treatment associated hyperglycemia and dyslipidemia among HIV infected patients at Burayu Health Center, Addis Ababa, Ethiopia: A cross-sectional comparative study. BMC Res Notes. 2014;7:380. doi: 10.1186/1756-0500-7-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grover SA, Coupal L, Gilmore N, Mukherjee J. Impact of dyslipidemia associated with Highly Active Antiretroviral Therapy (HAART) on cardiovascular risk and life expectancy. Am J Cardiol. 2005;95:586–91. doi: 10.1016/j.amjcard.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 5.van der Valk M, Kastelein JJ, Murphy RL, van Leth F, Katlama C, Horban A, et al. Nevirapine-containing antiretroviral therapy in HIV-1 infected patients results in an antiatherogenic lipid profile. AIDS. 2001;15:2407–14. doi: 10.1097/00002030-200112070-00008. [DOI] [PubMed] [Google Scholar]
- 6.Fontas E, van Leth F, Sabin CA, Friis-Møller N, Rickenbach M, d'Arminio Monforte A, et al. Lipid profiles in HIV infected patients receiving combination ART: Are different antiretroviral drugs associated with different lipid profiles? J Infect Dis. 2004;189:1056–74. doi: 10.1086/381783. [DOI] [PubMed] [Google Scholar]
- 7.van Leth F, Phanuphak P, Stroes E, Gazzard B, Cahn P, Raffi F, et al. Nevirapine and efavirenz elicit different changes in lipid profiles in antiretroviral-therapy-naive patients infected with HIV-1. PLoS Med. 2004;1:e19. doi: 10.1371/journal.pmed.0010019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bonnet E, Genoux A, Bernard J, Fauvel J, Massip P, Perret B. Impact of genetic polymorphisms on the risk of lipid disorders in patients on anti-HIV therapy. Clin Chem Lab Med. 2007;45:815–21. doi: 10.1515/CCLM.2007.140. [DOI] [PubMed] [Google Scholar]
- 9.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 10.Boden WE. High-density lipoprotein cholesterol as an independent risk factor in cardiovascular disease: Assessing the data from Framingham to the Veterans Affairs High – Density lipoprotein intervention trial. Am J Cardiol. 2000;86:19L–22L. doi: 10.1016/s0002-9149(00)01464-8. [DOI] [PubMed] [Google Scholar]
- 11.Kuivenhoven JA, Groenemeyer BE, Boer JMA, Reymer PWA, Berghuis R, Bruin T, et al. Ser447 stop mutation in lipoprotein lipase is associated with elevated HDL cholesterol levels in normolipidemic males. Arterioscler Thromb Vasc Biol. 1997;17:595–9. doi: 10.1161/01.atv.17.3.595. [DOI] [PubMed] [Google Scholar]
- 12.Sakai N, Yamashita S, Hirano K, Menju M, Arai T, Kobayashi K, et al. Frequency of exon 15 missense mutation (442D: G) in cholesteryl ester transfer protein gene in hyperalphalipoproteinemic Japanese subjects. Atherosclerosis. 1995;114:139–45. doi: 10.1016/0021-9150(94)05477-z. [DOI] [PubMed] [Google Scholar]
- 13.Miller M, Rhyne J, Chen H, Beach V, Ericson R, Luthra K, et al. APOC3 promoter polymorphisms C-482T and T-455C are associated with the metabolic syndrome. Arch Med Res. 2007;38:444–51. doi: 10.1016/j.arcmed.2006.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guettier JM, Georgopoulos A, Tsai MY, Radha V, Shanthirani S, Deepa R, et al. Polymorphisms in the fatty acid-binding protein 2 and apolipoprotein C-III genes are associated with the metabolic syndrome and dyslipidemia in a South Indian population. J Clin Endocrinol Metab. 2005;90:1705–11. doi: 10.1210/jc.2004-1338. [DOI] [PubMed] [Google Scholar]
- 15.Puppala J, Bhrugumalla S, Kumar A, Siddapuram SP, Viswa PDK, Kondawar M, et al. Apolipoprotein C3 gene polymorphisms in Southern Indian patients with nonalcoholic fatty liver disease. Indian J Gastroenterol. 2014;33:524–9. doi: 10.1007/s12664-014-0504-9. [DOI] [PubMed] [Google Scholar]
- 16.Reymer PWA, Gagné E, Groenemeyer BE, Zhang H, Forsyth I, Jansen H, et al. A lipoprotein lipase mutation (Asn291Ser) is associated with reduced HDL cholesterol levels in premature atherosclerosis. Nat Genet. 1995;10:28–34. doi: 10.1038/ng0595-28. [DOI] [PubMed] [Google Scholar]
- 17.Ridker PM, Paré G, Parker AN, Zee RYL, Miletich JP, Chasman DI. Polymorphism in the CETP gene region, HDL cholesterol, and risk of future myocardial infarction: Genomewide analysis among 18 245 initially healthy women from the Women's Genome Health Study. Circ Cardiovasc Genet. 2009;2:26–33. doi: 10.1161/CIRCGENETICS.108.817304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mahalle N, Garg MK, Naik SS, Kulkarni MV. Study of pattern of dyslipidemia and its correlation with cardiovascular risk factors in patients with proven coronary artery disease. Indian J Endocrinol Metab. 2014;18:48–55. doi: 10.4103/2230-8210.126532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mohan V, Deepa R, Rani SS, Premalatha G. Chennai Urban Population Study (CUPS No. 5). Prevalence of coronary artery disease and its relationship to lipids in a selected population in South India: The Chennai Urban Population Study (CUPS No 5) J Am Coll Cardiol. 2001;38:682–7. doi: 10.1016/s0735-1097(01)01415-2. [DOI] [PubMed] [Google Scholar]
- 20.Tang AM, Bhatnagar T, Ramachandran R, Dong K, Skinner S, Kumar MS, et al. Malnutrition in a population of HIV-positive and HIV-negative drug users living in Chennai, South India. Drug Alcohol Depend. 2011;118:73–7. doi: 10.1016/j.drugalcdep.2011.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Devanath A, Ray S, Kumar R, Prarthana BS. A study to evaluate lipid profile in treatment naïve HIV positive patients. Indian J Clin Biochem. 2014;29:45–50. doi: 10.1007/s12291-012-0295-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bernal E, Masiá M, Padilla S, Gutiérrez F. High-density lipoprotein cholesterol in HIV-infected patients: Evidence for an association with HIV-1 viral load, antiretroviral therapy status, and regimen composition. AIDS Patient Care STDS. 2008;22:569–75. doi: 10.1089/apc.2007.0186. [DOI] [PubMed] [Google Scholar]
- 23.Padmapriyadarsini C, Ramesh Kumar S, Terrin N, Narendran G, Menon PA, Ramachandran G, et al. Dyslipidemia among HIV-infected patients with tuberculosis taking once-daily nonnucleoside reverse-transcriptase inhibitor-based antiretroviral therapy in India. Clin Infect Dis. 2011;52:540–6. doi: 10.1093/cid/ciq195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Estimate of 10-year Risk for Coronary Heart Disease Framingham Point Scores. [accessed on August 20, 2015]. Available from: http://www.nhlbi.nih.gov/health-pro/guidelines/current/cholesterol-guidelines/quick-desk-reference-html/10-year-risk-framingham-table .
- 25.Hixson JE, Vernier DT, Powers PK. Detection of SstI restriction site polymorphism in human APOC3 by the polymerase chain reaction. Nucleic Acids Res. 1991;19:196. doi: 10.1093/nar/19.1.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Misra A, Vikram NK, Gupta R, Pandey RM, Wasir JS, Gupta VP. Waist circumference cutoff points and action levels for Asian Indians for identification of abdominal obesity. Int J Obes (Lond) 2006;30:106–11. doi: 10.1038/sj.ijo.0803111. [DOI] [PubMed] [Google Scholar]
- 27.Antiretroviral therapy guidelines for HIV-infected adults and adolescents including post-exposure prophylaxis. National AIDS Control Organization, Ministry of Health and Family Welfare, Government of India. 2007. [accessed on January 20, 2015]. Available from: http://www.nacoonline.org .
- 28.Bekolo CE, Nguena MB, Ewane L, Bekoule PS, Kollo B. The lipid profile of HIV-infected patients receiving antiretroviral therapy in a rural Cameroonian population. BMC Public Health. 2014;14:236. doi: 10.1186/1471-2458-14-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Malvestutto CD, Aberg JA. Management of dyslipidemia in HIV-infected patients. Clin Lipidol. 2011;15:725–34. doi: 10.2217/CLP.11.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alonso-Villaverde C, Segues T, Coll-Crespo B, Pérez-Bernalte R, Rabassa A, Gomila M, et al. High-density lipoprotein concentrations relate to the clinical course of HIV viral load in patients undergoing antiretroviral therapy. AIDS. 2003;17:1173–8. doi: 10.1097/00002030-200305230-00009. [DOI] [PubMed] [Google Scholar]
- 31.El-Sadr WM, Mullin CM, Carr A, Gibert C, Rappoport C, Visnegarwala F, et al. Effects of HIV disease on lipid, glucose and insulin levels: Results from a large antiretroviral-naive cohort. HIV Med. 2005;6:114–21. doi: 10.1111/j.1468-1293.2005.00273.x. [DOI] [PubMed] [Google Scholar]
- 32.Aragonès G, Alonso-Villaverde C, Pardo-Reche P, Rull A, Beltrán-Debón R, Rodríguez-Gallego E, et al. Antiretroviral treatment-induced dyslipidemia in HIV-infected patients is influenced by the APOC3-related rs10892151 polymorphism. BMC Med Genet. 2011;12:120. doi: 10.1186/1471-2350-12-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Radovica I, Fridmanis D, Vaivade I, Nikitina-Zake L, Klovins J. The association of common SNPs and haplotypes in CETP gene with HDL cholesterol levels in Latvian population. PLoS One. 2013;8:e64191. doi: 10.1371/journal.pone.0064191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang J, Wang LJ, Zhong Y, Gu P, Shao JQ, Jiang SS, et al. CETP gene polymorphisms and risk of coronary atherosclerosis in a Chinese population. Lipids Health Dis. 2013;12:176. doi: 10.1186/1476-511X-12-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zende PD, Bankar MP, Momin AR, Kamble PS. Study of Cholesteryl Ester Transfer Protein (CETP) I405v genotype and its association with lipid fractions in myocardial infarction patients: A case control study. J Clin Diagn Res. 2014;8:CC01–4. doi: 10.7860/JCDR/2014/7818.4441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dixit M, Bhattacharya S, Mittal B. Association of CETP TaqI and APOE polymorphisms with type II diabetes mellitus in North Indians: A case control study. BMC Endocr Disord. 2005;5:7. doi: 10.1186/1472-6823-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


