Abstract
Rabies is a neurotropic viral illness, almost always fatal, that is equally dreaded by healthcare practitioners and patients due to the dismal prognosis and limited treatment options once symptoms set in. There are hardly any reports on MRI changes in the brain in survivors of rabies encephalitis. We present the clinical course and the imaging findings on serial MRI examinations in a rare patient who survived rabies infection. Initial brain MRI done 8 days after onset of symptoms revealed bilaterally symmetrical non-enhancing areas of T1 and T2 hyperintensity in the basal ganglia, thalami, mid brain, and pons along with T2 hyperintensity and restricted diffusion in fronto-parietal cortical grey matter and left hippocampus. Subsequent MRI scans at 2 months and 5 months revealed progressive brain atrophy, leukoencephalopathy, and gliosis.
Keywords: MRI brain, rabies encephalitis, rabies survivor
Introduction
Rabies is a neurotropic viral illness that follows infection by a family of rhabdovirus. Prodromal symptoms include fever, malaise and tingling at the site of exposure initially. This is followed by CNS symptoms, which vary depending on whether the patient has paralytic or encephalitic form of the disease.
Once symptoms set in, the result is nearly always fatal with only twelve reported cases of patients surviving rabies in the world till date.[1] Two more unpublished cases of rabies survivors from Goa (India) and Chandigarh (India), respectively, were reported in a national newspaper. Most of these patients were aggressively managed with supportive care.
On a review of literature, we came across only one case report discussing sequential MRI findings in a rabies survivor.[1]
We present the clinical course and the imaging findings on serial MRI examinations in the 15th patient who survived rabies infection. As the number of patients who have survived this illness rises steadily, these findings gain importance in the follow up of rabies survivors as well as for correlating the residual disabilities in these patients.
Case History
A 14-year-old boy was brought with history of altered consciousness preceded by prodrome of fever and headache following a class III dog bite four weeks prior. He was partially immunized with three doses of rabies vaccine. However, passive immunization was not administered.
On examination, his vital signs were stable. He had a glasgow coma scale (GCS) of 11/15 (E2 M5 V4). The fundus was normal bilaterally. There was no focal motor deficit. Meningeal signs were present.
His lab parameters revealed leukocytosis with 92% polymorphs. CSF analysis revealed features of viral meningitis. Viral screen of the CSF was negative for herpes, Japanese B and West Nile viruses. Screening for dengue and malaria was also negative. His sensorium progressively worsened within 48 hours of admission to a GCS of 08/15 and he subsequently developed respiratory distress with features of pneumonia. GCS further worsened to 04/15. Thereafter, he was placed on mechanical ventilation.
Gradual improvement of pneumonitis was achieved. Albeit, no improvement in his sensorium was achieved. He also developed features of autonomic dysfunction.
Suspecting rabies encephalitis due to antecedent history of dog bite, his CSF and corneal scrapping were sent to National institute of virology (NIV) and Armed Forces Medical College (AFMC), Pune, for RT-PCR and came out positive for rabies antigen. Rabies was further confirmed by the presence of rabies virus neutralizing antibodies by RFFIT in CSF sample sent to NIMHANS, Bangalore.
The patient was continued on ventilatory support for another month. His sensorium gradually improved to a minimally conscious state over a period of 4–6 weeks. He became afebrile and started maintaining O2 saturation on room air with spontaneous eye opening by the end of 2 months.
At the time of discharge after about 6 months of hospitalization, he was interacting meaningfully with the environment, however, he was still quadriparetic and autonomic dysfunction continued.
Table 1 depicts the findings on serial MRI examinations in the case.
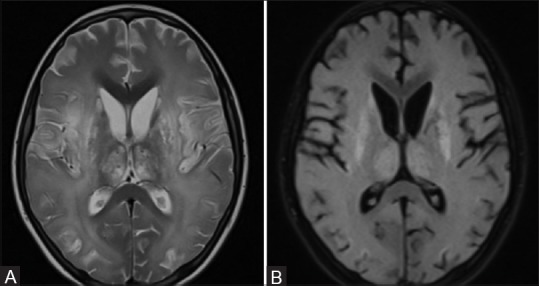
Table 1.
Findings on serial MRI in the patient
Discussion
According to a 2014 WHO report, India reports between 18,000 to 20,000 cases of rabies in a year with roughly 36% of world's rabies deaths occurring here.[2] There are two forms of the disease — encephalitic or furious (80%) and paralytic or dumb (20%).
In encephalitic rabies, it is the brain stem and the cerebrum, particularly the limbic system that is involved, while in the paralytic form the medulla and the spinal cord are mainly involved by extensive neuronal damage and inflammation. Involvement of the basal ganglia and the thalamus is usually seen late in the disease.[3]
Computed tomography (CT) scans may reveal focal or diffuse hypoattenuating areas in the basal ganglia, periventricular white matter, hippocampus, and brain stem. Some cases show pontine hemorrhages, while diffuse cerebral edema may be seen in few advanced cases.[4]
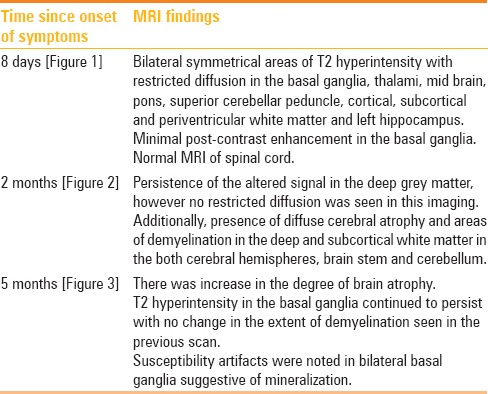
Figure 1 (A-F).
MRI Brain at day 8 after onset of symptoms (A and B) T2 weighted and FLAIR axial images reveal bilaterally symmetrical areas of hyperintensity the basal ganglia, thalami and fronto-parietal grey matter. (C) T1 weighted axial images reveal minimal hyperintensity in bilateral basal ganglia. (D) T1 weighted post-contrast axial images minimal post-contrast enhancement in the basal ganglia. (E and F) Diffusion weighted image and ADC maps reveal restricted diffusion in the fronto-parietal grey matter (Broken arrow)
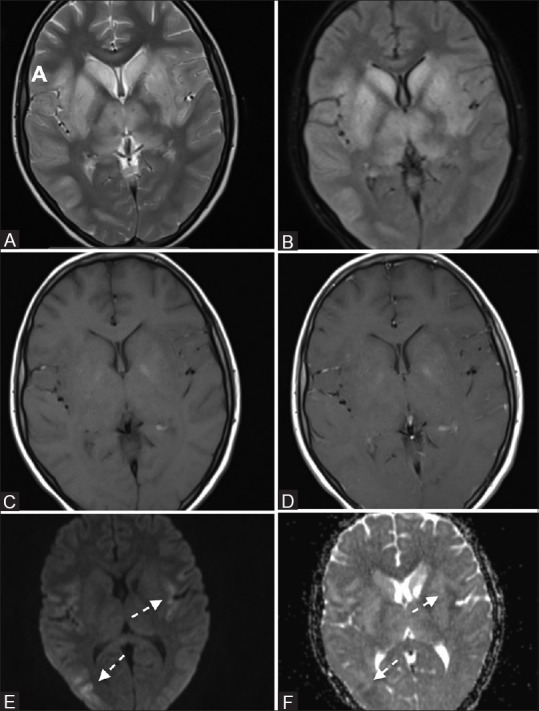
Figure 2 (A and B).
(A and B) MRI done 2 months after onset of symptoms. T2 weighted and FLAIR axial images reveal persistence of the altered signal in the deep grey matter. Also seen is presence of diffuse cerebral atrophy in the both cerebral hemispheres
MRI reveals T2 hyperintensity that depends on the form of disease.
Encephalitic rabies: Basal ganglia, thalami, hypothalami brainstem, brain stem, limbic system and spinal cord
Paralytic rabies: Spinal cord and medulla.
Abnormalities may also extend to central white matter. The location of MRI abnormalities coupled with clinical picture can help diagnose rabies. Diffusion-weighted imaging (DWI) is also known to play a role with affected areas showing increased diffusion.[5] Because of the stormy course and rapidly fatal nature of the disease, most reports of neuroimaging findings in these patients are anecdotal. Little attention, therefore, has been paid to imaging findings in naturally acquired human rabies.
Pleasure and Fischbein[6] described MR abnormalities in the brainstem and hypothalamic-pituitary system in a patient with postmortem diagnosis of rabies encephalitis. In another case of rabies encephalitis diagnosed ante mortem, Awasthi et al.[7] reported T2 as well as T1 hyperintensities in the globus pallidi, putamen, and thalami bilaterally. However, there are also studies, like the one by Laothamatas et al.,[8] who did not report any significant differences between the findings in encephalitic and paralytic forms of the disease with non-enhancing, ill defined, mild to moderate T2 hyperintensities involving the deep white matter of the brain including the temporal lobe and brain stem.
In addition to the role of conventional spin echo sequences, Rao et al.[5] commented upon the role of DWI/apparent diffusion coefficients (ADC) in imaging findings of rabies encephalitis. In their case report, DWI at b-values of 1000 s/mm2 revealed mild increase in the ADCs in the involved regions of the brain.
Jassi et al.[9] discussed MRI findings done within one week of onset of symptoms in two cases of rabies encephalitis, both of whom later succumbed to the disease. They reported T2/FLAIR hyperintensities involving the dorsal aspect of the brainstem, as well as the central white matter of the midbrain. Similar areas of altered signal were also noted in bilateral thalami, hypothalami, and hippocampi along with the cervical cord. The involved regions showed mild increase in the ADCs in the involved regions and mild associated mass effect.
Figure 3 (A-E).
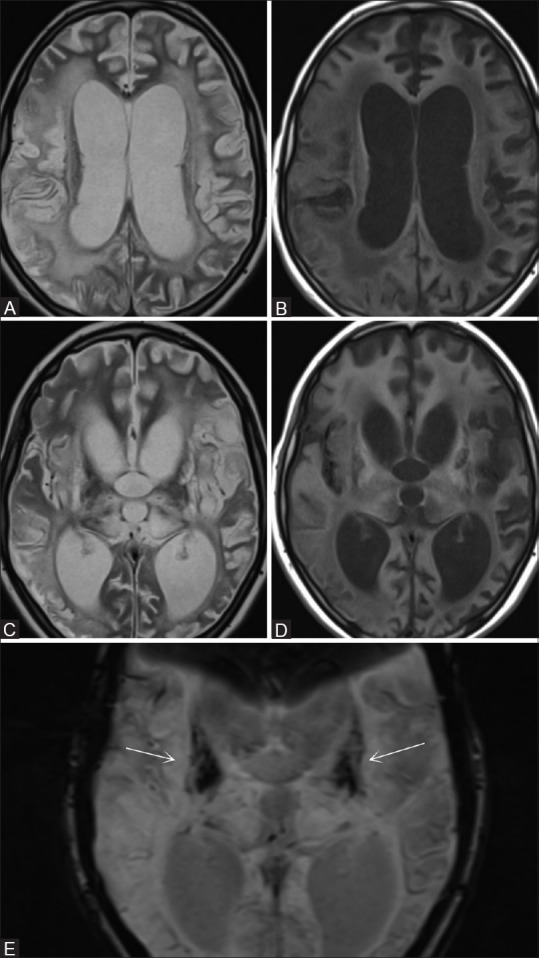
MRI done 5 months after onset of symptoms. (A-D) T2 & T1 weighted axial images reveal increase in the degree of brain atrophy and persistence of the altered signal in the basal ganglia. (E) SWI image done 5 months after onset of symptoms reveal susceptibility artifacts were noted in bilateral basal ganglia suggestive of mineralization (arrows)
The only other study on serial imaging in a rabies survivor by Netravathia et al.[1] reported patchy areas of hyperintensity in the brainstem (medulla, dorsal pons, midbrain) and the thalamus, basal ganglia, hippocampus and cortical grey matter, along with central grey matter of the spinal cord and nerve roots. Subsequent MRI at 3 months and 1 year showed resolution of the white matter changes along with progressive cerebral atrophy, leukoencephalopathy and gliosis.
Although our patient had a mixed clinical picture with features of paralytic rabies along with autonomic dysfunction, his MRI findings resembled the encephalitic form with sparing of spinal cord or medulla.
Long-term sequelae of rabies encephalitis in our patient include diffuse cerebral atrophy and demyelination with persistent T2 hyperintensities in the basal ganglia, which is similar to those reported in the study by Netravathia et al.[1] However, we also saw areas of blooming in bilateral basal ganglia suggestive of mineralization in the scan done at 5 months after onset of illness.
In spite of the fatal course, because of these sporadic cases of patients surviving human rabies, there is renewed hope in healthcare practitioners and patients alike. We are encouraged to discover newer therapeutic strategies to deal with this dreaded and otherwise fatal disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Netravathia M, Udanib V, Mani RS, Gadad V, Ashwini MA, Bhat M, et al. Unique clinical and imaging findings in a first ever documented PCR positive rabies survival patient: A case report. J Clin Virol. 2015;70:83–8. doi: 10.1016/j.jcv.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 2.Bulletin of the World Health Organization. 2014;92:230. doi: 10.2471/BLT.14.136044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mrak RE, Young L. Rabies encephalitis in humans: Pathology, pathogenesis and pathophysiology. J Neuropathol Exp Neurol. 1994;53:1–10. doi: 10.1097/00005072-199401000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Sing TM, Soo MY. Imaging findings in rabies. Australas Radiol. 1996;40:338–41. doi: 10.1111/j.1440-1673.1996.tb00415.x. [DOI] [PubMed] [Google Scholar]
- 5.Rao AS, Varma DR, Chalapathi Rao MV, Mohandas S. Case report: Magnetic resonance imaging in rabies encephalitis. Indian J Radiol Imaging. 2009;19:301–4. doi: 10.4103/0971-3026.57214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pleasure SJ, Fischbein NJ. Correlation of clinical and neuroimaging findings in a case of rabies encephalitis. Arch Neurol. 2000;57:1765–9. doi: 10.1001/archneur.57.12.1765. [DOI] [PubMed] [Google Scholar]
- 7.Awasthi M, Parmar H, Patankar T, Castillo M. Imaging findings in rabies encephalitis. AJNR Am J Neuroradiol. 2001;22:677–80. [PMC free article] [PubMed] [Google Scholar]
- 8.Laothamatas J, Hemachudha T, Mitrabhakdi E, Wannakrairot P, Tulayadaechanont S. MR Imaging in Human Rabies. AJNR Am J Neuroradiol. 2003;24:1102–9. [PMC free article] [PubMed] [Google Scholar]
- 9.Jassi P, Attri A, Dhawan R, Kakkar C, Saggar K. MR imaging in rabies encephalitis: A rare entity. Ann Indian Acad Neurol. 2016;19:125–8. doi: 10.4103/0972-2327.167712. [DOI] [PMC free article] [PubMed] [Google Scholar]


