Abstract
Introduction:
Coccydynia refers to pain in the terminal segment of the spinecaused by abnormal sitting and standing posture. Coccydynia is usually managed conservatively, however in nonresponsive patients, ganglion impar block is used as a good alternate modality for pain relief. This article studies the effect of ganglion impar block in coccydynia patients who were not relieved by conservative management.
Materials and Methods:
The study was carried out at the pain clinic in the departments of Physical Medicine and Rehabilitation and Radiology in a tertiary centre in India. It was a prospective hospital-based study, in which 35 patients with coccydynia were considered for fluoroscopy-guided trans-sacro-coccygeal ganglion impar block. The outcome assessment was done using Numerical Rating Scale (NRS) and Oswestry Disability Index (ODI) scores for a follow-up period of 6 months. Of the 35 patients, 4 were lost to follow-up. Analysis was done usingthe data from the remaining 31 patients.
Results:
The mean age of the patients suffering from chronic coccydynia was 42.9 ± 8.39 years, and patients' age range was 28–57 years. The mean score of NRS and ODI before the procedure was 7.90 ± 0.16 and 48.97 ± 1.05, respectively. The interquartile range (IQR) of NRS score remained almost unchanged during pre and postprocedure, however, IQR of ODI varied during the pre and post procedural events. The NRS and ODI scores immediately after the procedure decreased drastically showing significant pain relief in patients, and the difference of scores till the end of study was statistically significant.
Conclusion:
This study recommends the trans-sacro-coccygeal “needle inside needle” technique for local anesthetic block of the ganglion impar for pain relief in patients with coccydynia. This should be integrated with rehabilitative measures including ergonomical modification for prolonging pain free period.
Keywords: Coccydynia, ganglion impar block, NRS score, ODI score
Introduction
The term coccydynia refers to pain in the terminal segment of the spine, which was first described by Simpson in the nineteenth century.[1] It is mainly associated with abnormal mobility of the coccygeal region triggering chronic inflammation. The pain worsens with abnormal sitting posture such as leaning back while being seated, prolonged sitting as well as standing, and abrupt rising from sitting position. It can also interfere with sexual intercourse and defecation.[2] The exact incidence of coccydynia is not known, but is seen more commonly in females. Although it can present at any age, it is usually diagnosed in the fourth decade.[3] The etiologies of coccydynia are varied, however in most patients, it is usually idiopathic or followed by external or internal trauma. The traumatic events related directly with the coccydynia are direct injury, backward fall, obstructed labor, etc. Non traumatic coccydynia can result from degenerative joint or disc disease, hypermobility or hypomobility of the sacrococcygeal joint, obesity, infectious etiology, variants of coccygeal morphology, and cancers of the pelvis and anorectal region.[4] It is also important to rule out other nonorganic causes, such as somatization disorder and other psychological disorders in patients of chronic recalcitrant coccydynia.
An array of treatment options are available for this painful condition starting from conservative treatment options to modern interventional procedures. Conservative treatment such as non steroidal anti-inflammatory drugs (NSAIDs), local analgesics, hot or cold application, transcutaneous electrical nerve stimulation (TENS), modified wedge-shaped cushions (coccygeal cushions), and levator ani relaxation exercises are available.[5,6] However, in nonresponsive patients, direct injections around the coccyx, caudal epidural blocks, ganglion impar blocks, neurolysis and coccygectomy can be applied for pain relief.
There are various scales available to assess the intensity of pain such as Visual Analog Scale (VAS) and Numerical Rating Scale (NRS).[7,8] Oswestry Disability Index (ODI) is also used to measure the degree of disability and estimate the quality of life (QOL) with low back pain.[9]
Ganglion impar (Walther ganglion) is a sympathetic ganglion that is situated in the retroperitoneal space behind the rectum around the sacrococcygeal joint or directly in front of the coccyx.[3] The block of this ganglion can be performed with fluoroscopy, computerized tomography, or ultrasound guidance. The interventions used in this study have undergone modifications, and the most advanced “needle inside needle” technique is in vogue and was used in this study. This paper studies the effect of ganglion impar block in coccydynia patients who were not relieved by conservative management.
Materials and Methods
This prospective study was conducted in the department of Physical Medicine and Rehabilitation and Radiology at a tertiary centre in India after obtaining approval from the institutional ethics committee. Patients with chronic coccygeal pain for more than 3 months who did not respond to conservative treatment (NSAIDs, Modified cushion, TENS) were recruited into the study after obtaining their informed consent. The specific inclusion criteria were coccygeal pain for more than 3 months and no abnormalities on laboratory findings or imaging that explained the pain. Patients with local skin infection, who had undergone coccygectomy, sacrococcygeal joint fusion, with bleeding disorders, diabetes mellitus (uncontrolled despite medication) and pregnancy were excluded. The persons who were lost to follow-up in consecutive visits were also excluded from the analysis.
A total of 35 patients were initially enrolled who fulfilled the above inclusion and exclusion criteria and were considered for fluoroscopy-guided trans-sacro-coccygeal ganglion impar block. All the patients underwent complete work-up with all routine investigations to rule out diabetes, infection, and any coagulation abnormalities. Radiographs of coccyx in anteroposterior (AP) and lateral view was done in all patients to note any bony abnormalities. The blocks were administered as a day care procedure and the patients were discharged on the same day after observation for 1 hour to note any post-interventional complications. The procedure was done with patients in prone position, on the table of a biplane digital subtraction angiography machine (Philips Allura Clarity) with a pillow under the abdomen to overcome lumbar lordosis. The intergluteal area was prepared with sterile aseptic precautions. A sterile metallic pointer was used to locate the sacrococcygeal space, lateral fluoroscopic projection was taken, and the targeted area was marked [Figure 1]. The skin and subcutaneous tissue are injected with 1% lidocaine using a 25G needle over the sacrococcygeal disc at the superior aspect of intergluteal crease just below the sacral hiatus. A 1.5 inch 22G spinal needle was inserted at the marked site through the sacrococcygeal disc which served as the needle guide under fluoroscopy. A 2-inch 25G spinal needle was then introduced through a 22G needle and 0.2 ml of nonionic contrast solution (iohexol, omnipaque-GE) was injected. The needle placement was confirmed by the “comma sign” in the retroperitoneal space on lateral fluoroscopic projection [Figure 2]. A total volume of 3–5 ml of preservative free 0.5% bupivacine (Anawin) and 1 ml of methyl prednisolone was injected for pain relief after confirming the position of needle. Usually very little bleeding occurs post procedure. Hemostasis is achieved by applying pressure at the injection site and sterile dressing was done. After the procedure, NSAIDs and compression with ice packs were prescribed to relieve local inflammation.
Figure 1.
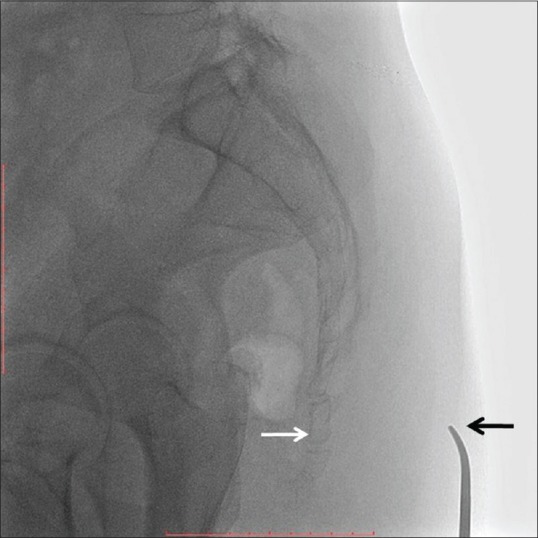
Lateral fluoroscopic view with a pointer placed on the skin surface (black arrow) to mark the sacro-coccygeal joint (white arrow)
Figure 2.
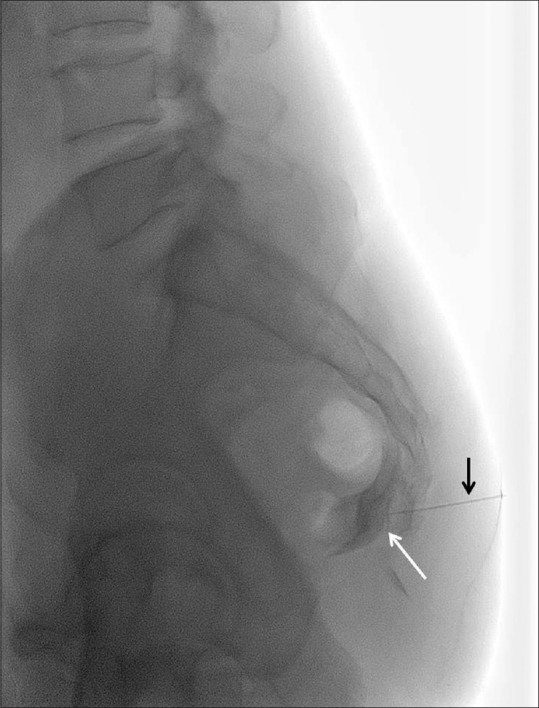
Needle position (black arrow) for injection of the local anaesthetic steroid mixture into the ganglion impar. Before injection of the mixture, a small amount of contrast is injected which forms a ‘comma’ like appearance (white arrow) in front of the sacro-coccygeal joint indicating the location of the ganglion impar
The intensity of pain was assessed using NRS before the injection and after 2, 4, 12 and 24 weeks of the procedure. The cumulative disability due to coccygeal pain was measured by ODI before the intervention and after 4, 12, and 24 weeks of the intervention. Both NRS and ODI were documented at a specified time period by an independent observer.
Four patients were lost to follow-up due to various reasons. The data from the remaining 31 patients who completed the follow-up period were considered for analysis. The patients who were not able to visit the clinic were contacted telephonically and their responses were recorded. The data were compiled from patient's records, and the patients were assessed using pretested questionnaires containing NRS and ODI scores. Patients were instructed to visit the clinic if there was unbearable pain hampering their routine activity.
The data was analyzed using SPSS version 21 (IBM, New York, United states) in which the quantitative data in the study was analyzed using t-test/Wilcoxon signed rank test, and mean alongwith standard error was calculated wherever required.
Results
In the present study, data from 31 patients who completed the period of follow-up after trans-sacro-coccygeal ganglion impar block by “needle inside needle” technique, were analyzed. The percentage of male-to-female ratio in this study was 45.2% and 54.8%, respectively. The mean age of the patients was 42.9 ± 8.39 years with the range being 28–57 years. Out of the total patients recruited for study, 38.7% (n = 12) patients had a confirmed history of trauma (falling on coccyx region). More than 50% (n = 16) of the patients had a history of travelling in the public transport system for long hours. All the patients were administered ganglion impar block only once. The block was performed successfully in all the patients in a single attempt and no difficulty was encountered during the procedure, except in one patient who had calcification of the sacrococcygeal ligament. In this patient, 1.5-inch 20G needle was used to pierce the dorsal sacrococcygeal ligament deeply, and then a 25G needle was passed through it as per “needle inside needle” technique. One patient did not have any significant improvement in the intensity of pain in the subsequent follow-up visits after the procedure. None of the patients faced any post procedural complications.
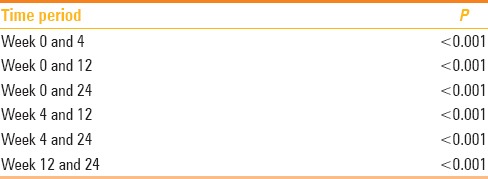
The mean score of NRS and ODI before and after the procedure was 7.90 ± 0.16 and 48.97 ± 1.05, respectively. The interquartile range (IQR) of NRS score remained almost unchanged during pre and postprocedure, however, IQR of ODI varied during the pre and post procedural event. The NRS score immediately after the procedure decreased drastically showing a significant pain relief in these patients. The same was true of ODI scores showing the effectiveness of ganglion block [Table 1]. The pain intensity was much lower post block when compared to baseline pre procedure value of both the indices throughout the 6-month follow-up period [Tables 2 and 3].
Table 1.
Mean and standard error of Numerical Rating Scaleand Oswestry Disability Indexat different periods
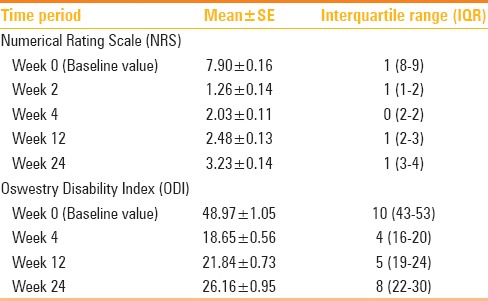
Table 2.
Comparison of Numerical Rating Scalescores at different time periods
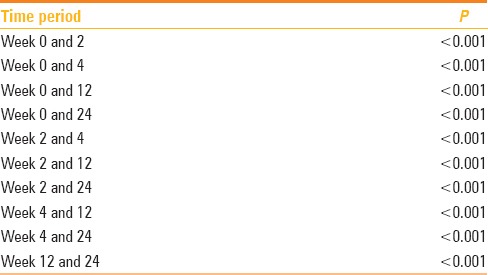
Table 3.
Comparison of Oswestry Disability Index scores at different periods
Discussion
Coccydynia is a clinical condition having varied etiology and no definitive diagnostic criteria exist till date.[10] The ganglion impar is a retroperitoneal structure at the level of the sacrococcygeal junction, which marks the termination of the paravertebral sympathetic chain. A ganglion impar block is usually considered to treat coccydynia which is non responsive to other conservative treatments. To confirm the efficacy of the block, a diagnostic ganglion impar block with local anesthetic can be given. The pain relief is achieved by the blockade of nociceptive as well as sympathetic fibers.[11] The success of the ganglion impar block may prove to be an effective treatment modality for long-term relief from coccydynia, as seen in our patients. The technique used in our study was transdiscal “needle inside needle” technique which is considered to be a relatively safe approach.
The techniques for blocking ganglion impar in the past used bent and curved needles, which are associated with significant discomfort, tissue damage, and high risk of rectal perforation.[12] Our study used a straight spinal “needle inside needle” approach for avoiding above mentioned problems and to further reduce the risk of discitis and incidence of needle breakage.[13] The trans-sacro-coccygeal “needle inside needle” approach adopted in this study is better than the classical and paramedian approach to the ganglion, and is a technically feasible method which is easy to learn and perform. There is minimal risk involved in this technique compared to surgical treatment. The complications of this technique are neuritis and inadvertent injection of the neurolytic agent into the rectum, which can be avoided by meticulous care. All the patients required only one attempt without any difficulty. The technique was originally described by Wemm and Saberski, which was further modified by Munir et al.[13,14]
The mean age in our patients was comparable to previous studies, however, there was difference with respect to gender. In previous studies, females outnumbered males, but in our study, there was an equal distribution, which might be due to the fact that females do not turn up frequently in clinics for pain relief in our part of the country due to various social reasons.[15,16] The percentage of patients presenting with post traumatic coccydynia was also comparable to the study by Gunduz et al.[15] Bupivacaine and methylprednisolone were used in our study. Other agents with which ganglion impar block has been described include lignocaine and neurolytic agents such as phenol and absolute alcohol. The NRS and ODI questionnaire was used in this study to assess the health related QOL of the coccydynia patients, which have been used rarely in other studies. The success of this modality of treatment in achieving pain relief is encouraging, however, a longer follow-up time is required to assess the efficacy of a single time injection. In addition, repeat injections and their effectiveness in patients who do not have adequate pain relief, warrant more studies with larger sample size and longer study period.
The patients were also advised other preventive measures and exercise such as pelvic floor exercises, kneeling groin stretch, and pyriformis stretching to avoid any recurrences in pain. All the patients were trained about the sitting posture while working for long hours. Obesity is an important contributing factor of coccydynia, and hence, a healthy lifestyle was promoted among patients and appropriate methods of reducing weight was offered.
The limitation of the study was the absence of a control group for comparison. The follow-up period was only 6 months considering the resources, however, further information could have been obtained if the follow up period was longer to note the lasting effect of ganglion impar block.
Conclusion
Our study shows the long-term effectiveness of ganglion impar block for patients with coccydynia in providing pain relief by the trans-sacro-coccygeal “needle inside needle” technique. The integration of ganglion impar block with other rehabilitative measures including ergonomical modification may be needed for prolonging pain free period. For generatinghigh-level evidence, larger studies with randomized control groups can be planned. This approach may also be used for neurolysis or radiofrequency ablation of the ganglion impar for palliative management of pelvic tumors causing chronic perineal pain.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lirette LS, Chaiban G, Tolba R, Eissa H. Coccydynia. An overview of the anatomy, etiology, and treatment of coccyx pain. Ochsner J. 2014;14:84–7. [PMC free article] [PubMed] [Google Scholar]
- 2.Maigne JY, Doursounian L, Chatellier G. Causes and mechanisms of common coccydynia: Role of body mass index and coccygeal trauma. Spine. 2000;25:3072–9. doi: 10.1097/00007632-200012010-00015. [DOI] [PubMed] [Google Scholar]
- 3.Gunduz OH, Sencan S, Kenis-Coskun O. Pain Relief due to Transsacrococcygeal Ganglion Impar Block in Chronic Coccygodynia: A Pilot Study. Pain Med. 2015;16:1278–81. doi: 10.1111/pme.12752. [DOI] [PubMed] [Google Scholar]
- 4.Ellinas H, Sethna NF. Ganglion impar block for management of chronic coccydynia in an adolescent. PaediatrAnaesth. 2009;19:1137–8. doi: 10.1111/j.1460-9592.2009.03155.x. [DOI] [PubMed] [Google Scholar]
- 5.Trollegaard AM, Aarby NS, Hellberg S. Coccygectomy: An effective treatment option for chronic coccydynia: Retrospective results in 41 consecutive patients. J Bone Joint Surg Br. 2010;92:242–5. doi: 10.1302/0301-620X.92B2.23030. [DOI] [PubMed] [Google Scholar]
- 6.Maigne JY, Chatellier G. Comparison of three manual coccydynia treatments: A pilot study. Spine. 2001;26:E479–83. doi: 10.1097/00007632-200110150-00024. [DOI] [PubMed] [Google Scholar]
- 7.Jensen MP, Chen C, Brugger AM. Interpretation of visual analog scale ratings and change scores: A reanalysis of two clinical trials of postoperative pain. J Pain. 2003;4:407–14. doi: 10.1016/s1526-5900(03)00716-8. [DOI] [PubMed] [Google Scholar]
- 8.McCaffery M, Pasero C. Pain: Clinical manual. 2nd ed. St. Louis, MO: Mosby; 1999. [Google Scholar]
- 9.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25:2940–52. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 10.Wallace MS, Leung AY, McBeth MD. In: Malignant Pain, Textbook of Regional Anesthesia. Prithvi Raj., editor. Pennsylvania: Churchill Livingstone Publishers; 2002. p. 585. [Google Scholar]
- 11.Toshniwal GR, Dureja GP, Prasanth SM. Transsacrococcygeal Approach to Ganglion Impar Block for Management Of Chronic Perineal Pain: A Prospective Observational Study. Pain Phys. 2007;10:661–6. [PubMed] [Google Scholar]
- 12.Munir MA, Zhang J, Ahmad M. A modified needle-inside-needle technique for the ganglion impar block. Can J Anaesth. 2015;51:915–7. doi: 10.1007/BF03018890. [DOI] [PubMed] [Google Scholar]
- 13.Nebab EG, Florence IM. An alternate needle geometry for interruption of the ganglion impar. Anesthesiology. 1997;86:1213–4. doi: 10.1097/00000542-199705000-00028. [DOI] [PubMed] [Google Scholar]
- 14.Wemm K, Jr, Saberski L. Modified approach to block the ganglion impar (Ganglion of Walther) RegAnesth. 1995;20:544. [PubMed] [Google Scholar]
- 15.Patt RB, Plancarte R. Superior hypogastric plexus block, Interventional Pain Management. In: Waldman SD, Winnie AP, editors. Philadelphia: WB Saunders; 1996. pp. 384–91. [Google Scholar]
- 16.Wallace MS, Leung AY, McBeth MD. Malignant Pain, Textbook of Regional Anesthesia. In: Prithvi Raj., editor. Pennsylvania: Churchill Livingstone Publishers; 2002. p. 585. [Google Scholar]


