Abstract
Although research has demonstrated improved outcomes for outpatients who receive peer support—such as through online health communities, support groups, and mentoring systems—hospitalized patients have few mechanisms to receive such valuable support. To explore the opportunities for a hospital-based peer support system, we administered a survey to 146 pediatric patients and caregivers, and conducted semi-structured interviews with twelve patients and three caregivers in a children’s hospital. Our analysis revealed that hospitalized individuals need peer support for five key purposes: (1) to ask about medical details—such as procedures, treatments, and medications; (2) to learn about healthcare providers; (3) to report and prevent medical errors; (4) to exchange emotional support; and (5) to manage their time in the hospital. In this paper, we examine these themes and describe potential barriers to using a hospital-based peer support system. We then discuss the unique opportunities and challenges that the hospital environment presents when designing for peer support in this setting.
Keywords: Health informatics, pediatric, hospital, patient, caregiver, peer-to-peer, peer support
ACM Classification Keywords: J.3 Life and Medical Sciences, Health, Medical Information Systems, H.5.m. Information interfaces and presentation
INTRODUCTION
In the United States, over 34 million hospital admissions occurred in 2014 [52]. For many hospitalized individuals, their time spent between admission and discharge becomes extremely overwhelming and difficult to navigate. Patients and their caregivers must learn the intricate details of the care they are receiving and the complicated structure of the hospital hierarchy. They must also monitor information handoffs among their healthcare providers and remain vigilant due to the high risk of experiencing a preventable medical error [33]. On top of this work, they need to manage the symptoms, stress, and anxiety that emerge as a result of being in the hospital. One way to alleviate these health, information, and emotional burdens is to offer patients and caregivers the support of their peers, who can guide them through the many challenges of an unfamiliar hospital environment.
Evidence indicates that patients who participate in such peer support programs experience health benefits, such as increased adherence to medication, and improved clinical outcomes [3,9,20,47]. Technology-based peer support also provides an easily accessible medium for patients to find specific, tailored information related to their experience, to increase their knowledge, to strengthen their social bonds, and to feel a sense of belonging to a community [14,38,50]. A combination of these benefits and resources can lead to increased self-management, efficacy, and empowerment in their care [21,31]. However, research in the medical and HCI fields has typically focused on peer support for patients and caregivers with chronic conditions, who manage their care activities at home or in a clinic, instead of in the hospital.
To understand the opportunities and barriers for a peer support system in a hospital setting, we conducted two studies with pediatric patients and their caregivers. The first was a survey to identify the types of advice the participants wanted to share with others who have similar hospital experiences. These results served as the foundation for our second study: semi-structured interviews that incorporated “feature cards” of a hypothetical, hospital-based peer support system. Participants reacted to these features and provided their perspectives on exchanging information and interacting with peers during their time in the hospital.
In this paper, we describe five major types of information and support that hospitalized patients and caregivers want to exchange with their peers, and examine the potential barriers to using a peer support system in the hospital. Our primary contributions consist of:
Providing a deep understanding of the informational and emotional peer support needs that patients and caregivers have, but are not currently supported during hospitalization, and
Identifying opportunities, barriers, and design considerations for a peer support system to be used in the hospital.
These contributions have implications for peer support systems to increase engagement, reduce errors, and improve health outcomes for patients and caregivers in the hospital.
BACKGROUND
When patients and caregivers are seeking knowledge and support about their health, many turn to online resources [8,12]. Tools such as mobile applications, social media, and online communities help these individuals to find relevant medical information, share ideas about managing their care, and gather the strength needed to cope with their illness [42,44]. These manifestations of informational and emotional support are valuable and distinct from the resources given by their healthcare provider [7,19].
Many types of options exist to facilitate peer support for a wide range of healthcare settings and patients, but hospital-based interventions do not always employ digital solutions. Rather, dyads of current and previous patients typically meet face-to-face for mentoring sessions [27,45]. Additionally, Jacobs and colleagues describe the role of cancer navigators, who assist cancer patients during different stages of their illness and treatment by answering questions, providing emotional support, and helping the patient apply for resources. These support services are nearly always provided in-person [24].
As one type of option outside the hospital, text messaging has been used to engage patients with their peers, especially with individuals managing chronic conditions at home, sometimes in low resource settings. For example, Franklin et al. implemented a mobile, text message support system called Sweet Talk for young patients living with type 1 diabetes to exchange “information, tips, and reminders”, customize the timing of messages to appear before a clinic visit, and establish personal goals—such as regular insulin injections, blood glucose testing, healthy eating, and exercise [13]. A similar strategy by Rotheram-Borus et al. was conducted by linking women who have diabetes with a “buddy” via text message for 12 weeks. The pairs encouraged each other’s adherence to their disease management tasks at home [43]. Both studies resulted in participants who engaged with their newfound community, and who demonstrated improved clinical outcomes.
Using increasingly popular smartphones, patients who are managing diabetes or obesity symptoms at home and between clinic visits can use dedicated mobile applications. These tools allow peers to share their daily fitness data and participate in a larger social network to promote healthy lifestyle changes—such as losing weight, exercising more, or improving eating habits [4,10].
A less common but appealing option, multi-user environments, have been explored by Bers et al., with the development of Zora, a three-dimensional environment where pediatric patients can create their own artifacts and form characters that interact with other users. Intended to help peers build a network and improve their medical adherence, this tool was designed for both diabetic patients to pass time during clinic visits, and for patients who were home from the hospital after receiving a solid organ transplant [1,2]. Similarly, Chin and Tsuei made a multi-user system for hospitalized patients with chronic illness to create narrative stories and share them with peers [5].
Websites and online forums provide additional means of support for patients and caregivers affected by a number of health issues, most notably chronic conditions—such as diabetes, obesity, cancer, and mental illness [22,28,51]. Reach Out! is one example that provides a place for young people with mental illness to discuss information and help-seeking strategies, with input and moderation by trained professionals. This program particularly helps reduce isolation of individuals who do not seek face-to-face support from their healthcare provider [48].
More recently, social media has emerged as a way to find people dealing with similar health-related problems. Facebook has allowed people to document their experiences, communicate with others through personal profiles, and create specialized “groups” [15,40]. Researchers have also analyzed YouTube-hosted health vlogs generated by patients diagnosed with cancer, HIV, and diabetes. This platform is used to document vloggers clinic or hospital visits, discuss their treatments and day-today management of their chronic illness, and share emotional struggles experienced at each significant point of their care process [23,29]. Additionally, Liu et al. found that chronically ill pediatric patients use a combination of social media, video chat, and texting to maintain a degree of normalcy, social support, and emotional support with existing friends [30]. Yet, we know little about how these tools can help hospitalized patients support each other.
In summary, the examples mentioned here represent a broad spectrum of solutions that make it easier for people to access the informational and emotional support they need, as well as share experiences and expertise acquired over time. Although some of these technologies are accessible to hospitalized patients, less is known about how the successful models of peer support tools translate to the hospital environment. Questions still remain about what the nature of peer support is among patients who share a similar hospital experience, and how to tailor this support to the specific needs of these individuals. Our research fills this knowledge gap and builds on prior work by uncovering the specific types of support that hospitalized patients and caregivers want during their stay, and are willing to share with their peers.
METHODS
In this paper, we report and discuss findings from two studies: (1) a survey, and (2) semi-structured interviews, including feedback on feature cards of a hypothetical, hospital-based peer support system. We define peers in this context as people with similar health and hospital experiences. This work was conducted with hospitalized patients and caregivers, and is part of a larger study to identify opportunities for patients and caregivers to increase engagement in their care and prevent medical errors during their hospital stay [26,35–37,41]. Results from the survey informed the development of the “feature cards” used in the interviews. Each study was approved by the authors’ Institutional Review Board.
Study Site and Consent Process
Both the surveys and interviews were conducted at Seattle Children’s Hospital in Seattle, WA. The hospital serves a broad geographic region, with pediatric patient demographics being slightly more diverse than the surrounding area’s population. This organization manages approximately 300 beds and admits over 15,000 patients per year.
For each study, consent was obtained for all participants. If the participant was between 7 and 13 years old, the caregiver—usually a parent—provided written consent, followed by verbal assent from the pediatric patient. For patients aged 14 or above, parental consent was not required, and the patients provided written assent. Patients and caregivers were often, but not always, co-present while the studies were conducted.
Survey
We developed a web-based survey instrument hosted by SurveyGizmo, which asked patients and caregivers about their experiences with an undesirable event, which we explicitly defined as an event that (1) was a small or big concern, (2) was unpleasant or caused harm, and (3) could have been avoided. Examples include: sleeping in an uncomfortable bed, experiencing a communication problem with their doctor, or receiving the wrong medication. The survey instrument went through several rounds of editing and pilot testing to ensure the questions and format were at an appropriate reading and comprehension level for eligible respondents. The final version consisted of 30 closed- and open-ended questions asking details about the event (e.g., When did the event happen? Were you a patient or caregiver at the time of the event? Please describe the event in your own words).
Recruitment occurred over a five-month period between February 2016 – July 2016. Our research team approached patients and caregivers in the hospital’s acute and intensive care units. They were considered eligible for the study if they met the following criteria: were at least 7 years old, were well enough to provide informed consent, were comfortable reading and writing in English, had spent at least one night in the hospital as part of their current stay, and had experienced an undesirable event during either the current or a previous hospital visit. A research team member would administer the survey to the consented individuals on an iPad, and was available to answer questions or help the respondent take the survey if necessary. The iPad was cleaned with sanitizing wipes before and after each use to prevent hospital infection. More information about this study and preliminary results can be read elsewhere [16].
Unlike the other survey questions that asked specific details about the participant’s undesirable event, only one question focused on peer support: “What advice would you give to others who might have had an [undesirable] event like this in the hospital?” This question was intended to elicit the respondent’s knowledge gained through their hospital experience, and explore their willingness to share this knowledge with their peers. Of the 146 survey responses, 131 (89.7%) provided a free text answer to this question. We report these answers in addition to the results of our semi-structured interviews.
Semi-Structured Interviews
To further explore perspectives that patients and caregivers have on receiving information and communicating with their peers in a broader context than hospital safety, we conducted semi-structured interviews with 15 hospitalized patients and caregivers. The interview consisted of an activity to design a patient-facing mobile application. This design activity involved multiple sets of “feature cards” inspired by envisioning cards, to draw out the values and preferences of patients and caregivers.
The themes that emerged from the survey analysis gave preliminary indications of the types of advice hospitalized individuals were compelled to share with their peers. To better understand what participants want to exchange with their peers, how they want to interact, and why they want to connect, we developed a subset of 6 feature cards that represented hypothetical components of a hospital-based peer support tool: (1) “Advice about being in the hospital” (2) “What to do when you notice a problem” (3) “Share your advice with others” (4) “Chat with another patient” (5) “Read other patient stories” and (6) “Filter patients by age, similar health issue, currently in the hospital, or other”. Examples are shown in Figure 1.
Figure 1.
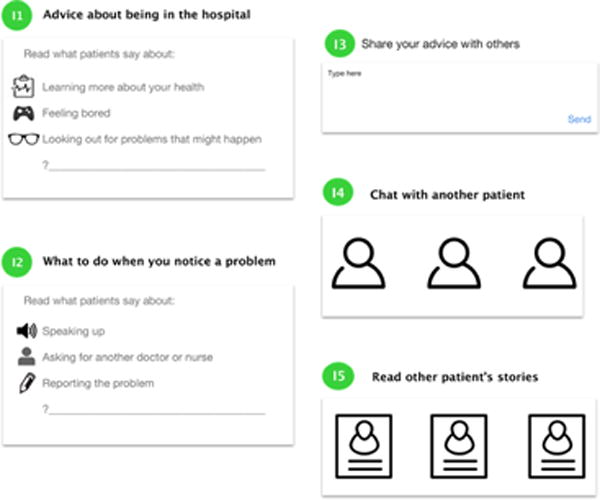
Examples of cards we showed to participants during semi-structured interviews. Each contains one or more prompts related to content or features of a hospital-based peer support system.
The research team member conducting the interview asked participants to respond to the feature cards and explain their reasoning or thought process behind their response. For example, if patients said they were interested in chatting with another patient, we would follow up by asking why they were interested and what they would want to chat with the other patient about. All interviews took place between July 2016 – August 2016 and were audio recorded and transcribed for analysis.
Participants
Survey Respondents
Demographics of the 131 survey responses we received for the question, “What advice would you give to others who might have had an [undesirable] event like this in the hospital?” are provided in Table 1. Most respondents identified as White/Caucasian and Female. One hundred twenty-three (94.6%) reported using a smartphone, tablet, or laptop device during their most recent hospital stay. Fifty-three respondents indicated that they (either as a patient or caregiver) had at least 10 overnight hospital stays in the last 5 years.
Table 1.
Demographic summary of survey respondents who answered, “What advice would you give to others who might have had an [undesirable] event like this in the hospital?”
| n | % | |
|---|---|---|
| Total survey responses | 146 | – |
| Responses to “advice” question | 131 | 89.7 |
| Patients | 51 | 38.9 |
| Caregivers | 80 | 61.1 |
| Gender (F/M) | 98/33 | 74.8/25.2 |
| Age* | – | – |
| 7–13 years | 23 | 17.6 |
| 14–18 years | 21 | 16.0 |
| 19+ years | 87 | 66.4 |
| Education | – | – |
| 8th Grade | 14 | 10.9 |
| High School/GED | 22 | 17.1 |
| Some College | 16 | 12.4 |
| 2 or 4 Year Degree | 39 | 30.3 |
| Graduate/Professional | 16 | 12.4 |
| None/No Answer | 22 | 17.1 |
| Race/Ethnicity** | – | – |
| White/Caucasian | 98 | 76.0 |
| Black/African American | 8 | 6.2 |
| Hispanic/Latin American | 16 | 12.2 |
| Asian | 17 | 13.2 |
| Native American/Pacific Islander | 11 | 8.5 |
| Other/No Answer | 12 | 9.4 |
three caregivers selected their child’s age instead of their own
respondents could select multiple categories
Interview Participants
We interviewed a total of 15 individuals. Twelve were pediatric patients, ranging in age from 7–17, divided equally between males and females. The remaining 3 were caregivers of pediatric patients between the ages of 30–39 years old, consisting of one male and two females. Race and ethnicity of these participants were as follows: 11 White/Caucasian, 1 Black/African American, 3 Hispanic/Latin American, 1 Native Hawaiian/Pacific Islander, 1 Asian. Twelve people (80%) indicated that they owned a smartphone. Three of our 15 participants had never visited the hospital before their current admission.
Data Analysis
We used a grounded theory approach to analyze both the survey and interview data [46]. The first author (SH) served as the primary coder for the survey responses. After each round of coding, SH met with the rest of the research team to discuss emergent themes, discrepancies, and codebook revisions. While interviews were conducted, three members of the research team (SH, SRM, MK) met regularly to iteratively develop a codebook based on emerging themes. After reaching saturation, SH, SRM, and MK independently coded interview transcripts. SH then compared the common threads and distinct themes of both data sets.
RESULTS
Our analysis revealed five primary themes that were consistent across our survey and interview results: (1) asking about medical details—such as procedures, treatments, or medications, (2) learning about providers, (3) reporting and preventing medical errors, (4) exchanging emotional support, and (5) managing time in the hospital. In addition, we describe potential barriers to using a hospital-based peer support system, which include (1) synchronous vs. asynchronous communication, and (2) preferences for viewing and sharing content.
To differentiate between the participants in each study discussed in this paper, we refer to survey responses as S# and interview participants as I#, followed by their status as either a patient or caregiver. During survey data collection, we assigned unique identifiers to each survey initiated, even if the response was never completed. Therefore, some S# values are greater than the number of complete responses.
Asking about Procedures, Treatments, or Medications
Patients and caregiver emphasized the importance of getting information about the patient’s care, from their healthcare providers as well as their peers. Survey respondents repeatedly encouraged their peer counterparts to ask questions and request follow-up information from doctors and nurses. S94, a pediatric patient who had unexpected complications during a surgery and whose providers did not properly follow post-surgery instructions, wanted other patients to feel comfortable requesting information about procedures and complicated medical terminology:
Don’t be afraid to ask questions before, after, or during the procedure. If you don’t understand the medical terms ask them to explain it in layman terms. Learn more of the risks involved and complications that can happen afterwards. –S94, Patient.
A caregiver, whose son experienced extreme discomfort due to an incorrectly inserted feeding tube, thought that knowledge from other patients would have been useful in identifying the source of her son’s distress. She recommended other caregivers ask for this information specifically:
Ask more questions about the tools and side effects and what other patient feedback has been. –S212, Caregiver.
When talking about information they wanted to learn from other patients, interview participants expressed interest in posing questions about procedures, treatments, and medications to patients that were currently going through or had already completed the process. I04, a patient, wanted to ask others with her same diagnosis about surgeries they had to undergo, and how well certain drugs worked. Another patient, I07, was waiting to undergo a transplant at the time we spoke to him. He also thought it was important to hear from other patients about their experiences firsthand:
Like I’m going through transplant. If there was another kid who was going through transplants, which there is, you could ask them okay, so how did it kind of feel like when you went through the transplant? –I07, Patient.
One caregiver was also interested in learning this type of information from other parents of children with the same health condition, so her own daughter’s health and symptom triggers could be normalized:
If some parents can also share that okay, this many times in a year we have to visit because of this reason, and my kid is around this age, right? So this kind of information helps in coming up with a pattern and some kind of satisfaction that okay, this is what has happened with…most other folks, it’s not only me who’s having this problem. –I15, Caregiver.
Participants in each study identified both their providers and peers as valuable sources of information. By encouraging each other to actively seek information and ask about care details, patients and caregivers can increase their knowledge, prepare for their upcoming experience, and maintain a realistic perspective of the patient’s health status.
Learning about Providers
Some of our survey respondents and interview participants wanted to talk about their healthcare providers with peers. Providers were a common topic of discussion among those who had a chronic or rare health condition, and wanted to know more information about the doctors who specialize in their care. I04, a patient, said this when talking about advice she would want to read from other patients:
I04: You could also say advice about doctors.
Interviewer: Like which doctor you have.
I04: Yeah, this doctor was better for me, this doctor I switched out because this happened. Like this doctor seemed to really know what they were doing, this doctor’s already seen what I have, has the most experience with what we have. So that would be good.
Similarly, many survey respondents shared advice for what to do when a patient’s or caregiver’s relationship with their provider is difficult. Through their own hospital experiences, respondents described the options available to a patient and caregiver that might not be commonly known. For example, one caregiver described receiving unsatisfactory care from a provider, which caused her to ask for a different doctor:
When your child is in the hospital, ask to speak to a pediatrician immediately. I didn’t know I had to request that, I assumed that since he was a child, we would of course speak to a Dr. for children. –S228, Caregiver
Respondents also encouraged other patients to facilitate communication among providers (i.e., asking providers if they had spoken to another provider), to avoid communication problems, and involve a third party such as a second opinion, hospital staff supervisor, social worker, family advocate, or legal advisor if disagreements start to affect the patient’s quality of care.
The quality of a patient or caregiver’s relationship with their provider can greatly affect their experience in the hospital. Advice on how to evaluate and maintain this relationship proved to be important for many participants, because they wanted to avoid potential conflicts and receive the best care possible.
Reporting and Preventing Medical Errors
Alerting someone to a serious problem was another consistent theme in both survey responses and interviews with patients and caregivers. One survey respondent, who was mistakenly administered too much laughing gas before a procedure, discussed the importance of reporting medical errors such as hers:
Report what happened to you. I wonder all the time if the anesthesiologist has done this to other children, especially children younger than I am who had no way of knowing what was happening to them. –S129, Patient
Information from other patients about methods for identifying and preventing errors in the hospital was also valuable for many of the pediatric patients we interviewed. For example, when I07 was asked about what advice he would want from other patients regarding their hospital stay, said: “because that way you can know what’s happening and any problems.” I12 wanted other patients’ guidance so he could consult with his doctors on how best to fix an issue. A third patient, I11, was interested in finding out what errors patients had experienced, so if she had a similar problem or noticed someone who needed medical help, she would know what to do.
In addition to these examples, advice on how to avoid errors mainly came from our survey respondents, who offered strategies such as remaining alert, paying attention to details of their care, keeping track of lab tests, and following up with their healthcare providers if needed. Many respondents also emphasized double checking medicine labels to help prevent drug-related errors such as giving a medication known to cause an allergic reaction, providing an incorrect dose, or administering the drug inappropriately.
Due to the prevalence and danger of preventable medical errors in the hospital setting, patients were aware of the need for constant vigilance and prompt reporting. Increased awareness among peers about the risks and types of error also has the potential to improve early detection and prevention.
Exchanging Emotional Support
Patients from each study discussed the idea of giving to and receiving support from their peers, by means of forming friendships, talking about their general health experiences, and offering encouragement.
Connecting with other patients who were of the same age range, health condition, or hospital was frequently mentioned as an important aspect of communicating with their peers. For many participants, this potential interaction was an opportunity to establish friendships and share mutual hospital experiences. One example was I09, a patient who traveled from out of state to be treated at the hospital. She only knew of one other person in her home state with the same diagnosis, and was excited at the prospect of talking with others like her. S233, also a pediatric patient, said she would be willing to share information about her hospital experience with another patient like herself. “I will just talk about my stay and learn about hers/his.”
I10, another patient, wanted to ask about others’ health progress and hospital stay, providing support to those who need someone to listen to them:
Interviewer: What kinds of things would you want to ask [other patients]?
I10: How they’re feeling and was it hard. And what they are going through.
Beyond sharing information about general hospital experiences, participants in both studies were compelled to offer comfort to others who go through difficult times. I12, a patient diagnosed with epilepsy, offered support to other patients struggling to manage the resulting emotional impact of having this condition:
I would say that it’s okay to have epilepsy, even though you might feel like the odd one out, you could still be a perfect person in your own way. –I12, Patient.
Sentiments like this were especially evident among survey respondents. Phrases such as “don’t be afraid”, “stay calm”, and “be strong” were frequent. Many respondents wrote messages that encouraged self-advocacy, including advice to be persistent when following up with healthcare providers, know their rights to request or turn down additional tests if needed, and to speak up when they feel uncomfortable. Others acknowledged and sympathized with the emotional impact of a stressful hospital visit:
It’s easy to feel unimportant to your doctors, especially when requests are not being acknowledged. Be your own best advocate. –S89, Patient.
When the status of the patient’s health is uncertain, both the patient and caregiver can feel increased tension, anxiety, and stress. By forming strong connections and offering reassurance, these individuals can find a way to relieve their emotional burdens with others who have gone through the same difficult situations.
Managing Time in the Hospital
During a typical hospital stay, patients and caregivers spend long stretches of time waiting for a provider to visit their room, anticipating a procedure, or recovering from treatment. Patients who responded to our survey and participated in interviews discussed advice about how to fill this time and prevent boredom. As I04 told us, “It’s a hospital, it’s not exactly Disney World.” One of our interview participants, I11, was interested in finding out more information from patients who have more hospital experience than herself:
Maybe other kids have been here longer than me and I don’t know all the places or where you can find things to do. And they could share advice about what to do in the hospital. –I11, Patient.
Patients with previous hospital experiences recommended taking advantage of existing resources to rent books, movies, television shows, or board games to play with visiting friends or family. When one of our patient participants, I05, was asked about what he would want to talk with other patients about, he responded, “Games and stuff. And like your cousins [could] play with you. And when you’re bored, you can go – some people get iPad or VS.” Alternatively, mental and physical exercises were mentioned as possible ways to avoid monotony:
Try to keep your mind busy with productive things…walk as much as possible to feel like you are doing something helpful instead of watching tv or playing on a screen. –S137, Patient.
Our participants wanted to know how to occupy their minds to distract from the physical pain and separation from family or friends. Informing patients about the resources available to them, (e.g., renting an Xbox, watching a movie) encourages these people to engage in activities outside their care and could improve their overall experience during hospitalization.
Barriers to Using a Peer Support System
The combination of survey and interview results gave us a deeper understanding of the informational and emotional peer support that hospitalized patients and caregivers need. During the interviews with our 15 participants, we also explored their perspectives about using a hospital-based peer support system. Although all participants expressed some level of interest in such a system, they also brought up concerns, which we discuss in this section.
Synchronous vs. Asynchronous Communication
During our interviews, we asked participants how they would prefer to communicate with other patients and caregivers. Several individuals wanted to interact with one or more of their peers in real time, because it was thought to be a more personal, private, and effective method of communication. Although some patients struggled to articulate why this real-time connection was important to them, it was particularly evident among patients who were interested in connecting with others experiencing similar health issues to share relevant information:
Interviewer: Would you want [communication] to be in real time?
I12: Yes. […]
Interviewer: You’d be okay with [sharing your advice with others]?
I12: Yes, because I think if I find something and others don’t, I think it would be a good thing to put out there, so other people can read about it in case they didn’t know what to do or what’s going on.
Interviewer: […] Can I ask why it being in real time would be important to you?
I12: Because, I think that in real time, it would be a lot better than any other time, because – I just don’t know.
Interviewer: You just like it better that way?
I12: Yeah.
Another patient we interviewed was under isolation protocol, which prevented her from leaving her hospital room. Physical interactions with other patients were not an option. To overcome this challenge, she mentioned the use of existing video chat tools:
Sometimes I can’t come out of my room because I’m in isolation…maybe the other kid [and me] wouldn’t be able to actually see each other physically, so you could Facetime or something like that. –I02, Patient
In contrast, a few participants explicitly mentioned their desire for asynchronous communication. I11, a younger pediatric patient, did not feel comfortable chatting with people that she did not already know in person, and preferred reading information from other patients outside of a real-time environment. One caregiver expressed some reluctance toward a live chat because it can be inconvenient when the patient needs attention:
I think real-time chat would be difficult, being in hospital, because you don’t know if your kid is upset or still recovering. If they had time and their kid is ok, then they can do real-time. –I15, Caregiver
Preferences for Viewing and Sharing Content
Despite feeling nervous about reading potentially negative hospital experiences, most interview participants still thought it was important to know this information. However, one pediatric patient preferred avoiding messages from other patients that might cause anxiety or sadness:
I01: I wouldn’t want to see that.
Interviewer: […] How come?
I01: I don’t know. Some of them are pretty sad.
Interviewer: You don’t want to see the bad [stories]?
I01: No.
Some information was also viewed as better suited for discussion with a healthcare provider instead of with another patient. For example, I04 was a patient who already felt comfortable speaking up and asking her doctor questions, so advice from other patients on doing these activities was not useful to her. I02, another pediatric patient, told us that patients should not discuss unexpected health problems with other patients, but rather with their providers or caregivers, “because they would probably know what [the] symptoms could be or any treatment or medicine you’re getting.”
Maintaining privacy was extremely valuable for caregivers. During their interviews, I14 and I15 expressed unease regarding the ability for their peers to identify them through virtual interactions. I14, who was initially not interested in exchanging information with peers, described his hesitation to communicate with other parents:
I mean you run into people in the elevators grabbing coffee and if you feel like it you socialize, but if you don’t, you just don’t, right? Yeah, I would stay anonymous. Personally, I would. –I14, Caregiver
Later in the interview, however, I14 said he was more agreeable to anonymously engaging with content from other caregivers. I15 also positively responded to the idea of anonymous interactions because it would allow people to honestly disclose information about medications or treatments without the risk of being identified.
These differing opinions about how and what to communicate with other patients begin to reveal the unique challenges that a hospital environment presents to designers of a peer support system. In the following section, we discuss opportunities and examine these challenges in more detail.
DISCUSSION
Our research builds on previous findings that examine the roles patients and caregivers take on during their hospital visits, their degree of involvement in activities related to their care, as well as their unsupported informational and emotional needs [25,26,34,35,37,41]. The results from our two studies, surveys and semi-structured interviews, identify the specific informational and emotional needs that these hospitalized individuals are willing to exchange with their peers.
Based on these findings, we describe three design considerations for a hospital-based peer support system: (1) leveraging the Electronic Health Record to match peers, (2) protecting privacy and anonymity, and (3) accommodating dynamic interactions and needs.
In the following sections, we also briefly compare two existing tools used for peer support, to demonstrate how hospital-based systems can adopt their benefits and improve upon their limitations. The first, PatientsLikeMe, is an online community that offers a place for patients and caregivers to share experiential knowledge among members. The second, Facebook, is a social media site that allows people to form groups about various health topics. Although these examples were chosen due to their recognition and previous research, we acknowledge that other technologies are currently used for the same reasons and are relevant to this work.
Leveraging the Electronic Health Record to Match Peers
Many of our survey respondents and interview participants strongly desired an open dialogue with their peers, especially with those who had similar health and hospital experiences. Properly aligning the interests and common attributes of peers is critical when forming quality interactions, and can be difficult to accomplish with existing tools. Facebook users must spend time independently seeking other individuals and groups related to their interests; the user sometimes may not know of or have access to a group, unless they receive an invitation from another group member. PatientsLikeMe forums are organized by chronic illness diagnosis, so those with similar experiences across diagnoses may be harder to identify.
Research on how to improve this process and match peers effectively is ongoing. For example, Hartzler et al. have used profiles and posts extracted from online health communities to optimize peer mentor recommendations [17,18]. In conjunction with solutions like this, a hospital-based peer support system can leverage information from the Electronic Health Record (EHR) to successfully match individuals with each other. Age, diagnosis, medications, procedures, treatment plans, and current physical location in the hospital are all examples of information stored with in the EHR. Thus, it would be possible to quickly match individuals who are interested in connecting with peers during their hospital stay by identifying their similar characteristics across these dimensions. One of our interview participants, I04, said she wanted to use a peer system that would help her find other patients of doctors who specialized in treating her rare condition, so she could speak to them in detail about the quality of care and differences in treatment protocols across providers. A system using information from the EHR could accomplish this by identifying groups of patients with the same diagnosis, healthcare provider, or hospital unit, who have also indicated an interest in connecting with peers. This would facilitate the exchange of expertise that I04 can use to further engage in her care.
Protecting Privacy and Anonymity
People have varying opinions on privacy and anonymity, as well as a range of preferences for sharing their personal health information. Success of a system used in a hospital setting is dependent on supporting these preferences. Most of our interview participants were comfortable sharing their information with others, but a few specifically mentioned their desire to only interact with a peer system anonymously. These individuals are interested in the benefits of learning from other patients and caregivers without sharing their own information; I15 also thought that having the option of anonymity would increase the value of such support by allowing peers to express more honest opinions about their hospital experiences. Although existing tools like Facebook have the option for health-related groups to be closed or open to the public, there is currently no way for users to interact with these groups anonymously.
To be sensitive to individual preferences for sharing personal and potentially identifiable health information, a hospital-based system should use an opt-in model, rather than opt-out. Users must be properly informed about the risks of sharing their information with others, and safeguards for situations that result in potentially negative consequences should also be incorporated. Possible solutions can involve the system having different levels of anonymity, customizable user profiles, or icons to represent higher-level information such as health status or hospital service (e.g., surgical, oncology, transplant), so the user can selectively choose what information they are willing to share with others. At present, Facebook incorporates selective sharing preferences, that allows users to choose what audience has access to information such as their birth date, or phone number. Having flexible security settings like Facebook helps to accommodate the broad range of preferences that might also change over time, as patients and caregivers become more familiar with their peers.
Accommodating Dynamic Interactions and Needs
The findings from our interview participants demonstrated a need to support many levels of engagement in a hospital-based peer support system. Patients like I02 and I12 valued real-time interactions with their peers, while others like I11 and I15 preferred to read content at their own time or interact with others in an asynchronous manner.
Our results also demonstrated a variety of peer support needs about the patients’ health, the hospital, and emotional support. Facilitating this support while recognizing that these needs can change over the course of a hospital stay is also important. For example, a patient might need information from peers about what to expect before a procedure, or what potential errors they need to watch for. After diagnosis or treatment, this patient might want to seek or share emotional support. During recovery, while the patient rests and waits for follow-up care, information about how to pass the time and hasten discharge might take precedence. We saw these changing needs among our study participants; I07 described wanting to know information and potential problems about his upcoming transplant, and S212 encouraged others to ask questions before undergoing a procedure. I12 was compelled to exchange emotional support after his recent epilepsy treatment. Following their surgical procedures, I11 and I04 wanted advice from peers about how to minimize boredom while confined to their hospital room.
Although some research on cancer patients have also noted differing information needs over time [11], such dynamism isn’t typically considered by peer tools. To support these various levels of interaction and peer support needs, researchers have emphasized the importance of designing for passive and active involvement in a system [32]. Although PatientsLikeMe and Facebook users can communicate synchronously or asynchronously via private messaging and timeline posts, finding relevant and accurate information across many resources and at different points of the care process poses many challenges. Prior work has also explored the use of virtual spaces where patients can access a repository of advice organized by symptom, treatment, or common struggle [6,49]. However, the cognitive and physical effort required to navigate and find relevant support is something that patients and caregivers in the hospital are not always not capable of due to medications or treatments [39]. In addition, such mappings by medical categories—such as symptoms—neglect the important dynamism during a hospital stay.
Providing synchronous features like text or video chat, coupled with a knowledge base to be accessed when convenient, would be particularly beneficial for hospitalized individuals. Users in the hospital could have the option of connecting with other patients currently in the hospital, or reading and contributing information to a knowledge base of patient and caregiver expertise. Individuals who were previously hospitalized and wanted to share their experiences could also add information by responding to a questionnaire after discharge. Allowing for multiple modes of interaction could increase the peer resources available to current patients, while supporting individual preferences for engaging in the system.
Adapting to peer support needs as they change over time, and reducing the user burden for finding relevant support are other critical components of a peer support system in the hospital environment. One way to accomplish this adaptation would be to have a user answer a series of prompts such as “do you want to learn from others about your upcoming procedure?” or “do you feel like playing a game with someone?” Based on their responses, the user could be automatically referred to the appropriate resource for information or emotional support. EHR data about diagnoses, medications, or procedures could be another way to direct the individual to appropriate peer information. This may reduce the burden for patients and caregivers to search for information on their own, across thousands of existing platforms. Topics or people of interest to the user could also be featured prominently within a tool and support easy navigation. A patient should be able to search, save, and organize information from their peers in a simple and efficient way. The type of content displayed could be adjusted based on their mood, health status, or current phase of their hospital stay. This capability would let individuals like I01, who only want to see positive experiences from other similar patients, avoid finding negative patient stories and still participate in other aspects of the peer support system.
LIMITATIONS AND FUTURE WORK
Our work provides new perspectives and opportunities for peer support in a hospital setting, but we also recognize the limitations of our studies. Because our survey purposefully included people who had experienced an undesirable event, safety issues naturally were a focus of their advice to peers. Both studies were conducted at a single pediatric hospital site in an urban setting in the United States, and might not account for the perspectives of a rural or community-hospital based population. Therefore, an important next step will be to validate these findings at different hospitals and geographic regions. In the future, we also would like to seek the opinions of healthcare providers, to explore their perspective and possible interaction with such a hospital-based peer support system. Additionally, future work should understand how the use of this system may affects patients’ engagement in their care.
CONCLUSION
In this paper, we explore the possibility of a hospital-based peer support system. Our survey with pediatric patients and caregivers offered insight into hospital safety, patient expertise, and the opportunities for a peer support system in a hospital setting. Through semi-structured interviews with hospitalized patients, and their reactions to feature cards representing aspects of a peer system, we examined the specific informational and emotional needs that a hospital-based system should support.
We conclude that supporting the specific needs and values of hospitalized individuals is essential for the success of a hospital-based peer support system. More research is needed to understand how existing peer support tools do, or do not, meet these needs. Existing non-hospital-based solutions—such as PatientsLikeMe and Facebook—have components of useful features for this patient population, including synchronous or asynchronous communication options, and customizable privacy settings. However, the hospital environment presents additional design opportunities and considerations.
A future hospital-based peer support system should consist of: (1) leveraging of EHR data for high-quality peer matches and tailored content for users, (2) allowing for opt-in privacy preferences of individuals who prefer to share or hide their personal health information, (3) providing synchronous, asynchronous, active, and passive interaction, and (4) accommodating informational and emotional needs that are likely to change over the course of a hospital stay, while ensuring the support is accessible without increasing user burden. Our design considerations should help guide technological systems and maximize the benefits of peer support networks for hospitalized patients and caregivers. Ultimately, such peer support could lead to increased empowerment, engagement, and safety for these individuals.
Acknowledgments
We would like to thank our survey respondents and interview participants, who took time out of their hospital visits to contribute to our research studies. Thank you also to Kathryn Nickel, members of the Outcomes Assessment Program at Seattle Children’s Hospital, and the Patients as Safeguards research team, including Andrew Miller, Alex Filipkowski, Cory Brown, Kelsey Aiello, and Rashmi Elera. This work was primarily funded by the Agency for Healthcare Research and Quality, grant #1R01HS022894, with additional support from the National Library of Medicine Biomedical and Health Informatics Training Grant #T15LM007442.
Footnotes
Permission to make digital or hard copies of all or part of this work for Personal or classroom use is granted without fee provided that copies are not made or distributed for profit or commercial advantage and that copies bear this notice and the full citation on the first page. Copyrights for components of this work owned by others than ACM must be honored. Abstracting with credit is permitted. To copy otherwise, or republish, to post on servers or to redistribute to lists, requires prior specific permission and/or a fee.
References
- 1.Bers Marina, Chau Clement, Satoh Keiko, Beals Laura. Virtual Communities of Care: Online Peer Networks with Post-Organ Transplant Youth. International Society of the Learning Sciences; 2007. [Google Scholar]
- 2.Bers Marina U, Gonzalez-Heydrich Joseph, DeMaso David Ray. Identity construction environments: supporting a virtual therapeutic community of pediatric patients undergoing dialysis. Proceedings of the SIGCHI conference on Human factors in computing systems - CHI ’01. 2001:380–387. http://doi.org/10.1145/365024.365302.
- 3.Campbell Sharon H, Phaneuf Marie Rose, Deane Karen. Cancer peer support programs—do they work? Patient Education and Counseling. 2004;55(1):3–15. doi: 10.1016/j.pec.2003.10.001. http://doi.org/10.1016/j.pec.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Chen Yu, Randriambelonoro Mirana E, Geissbuhler Antoine, Pu Pearl. Social Incentives in Pervasive Fitness Apps for Obese and Diabetic patients. Proceedings of the 19th ACM Conference on Computer Supported Cooperative Work and Social Computing Companion - CSCW ’16 Companion. 2016:245–248. http://doi.org/10.1145/2818052.2869093.
- 5.Chin Jui-Chih, Tsuei Mengping. Multi-user Narrative Sharing System for Children with Chronic Illness. 2009 Ninth IEEE International Conference on Advanced Learning Technologies. 2009:479–481. http://doi.org/10.1109/ICALT.2009.154.
- 6.Civan Andrea, McDonald David W, Unruh Kenton T, Pratt Wanda. Locating patient expertise in everyday life. Proceedings of the ACM 2009 International Conference on Supporting Group Work - GROUP ’09. 2009:291–300. doi: 10.1145/1531674.1531718. http://doi.org/10.1145/1531674.1531718. [DOI] [PMC free article] [PubMed]
- 7.Civan Andrea, Pratt Wanda. Threading together patient expertise. Proceedings of the American Medical Informatics Association Annual Symposium. 2007:140–144. Retrieved from https://www.semanticscholar.org/paper/Threading-Together-Patient-Expertise-Hartzler-Pratt/64eed14b34218d8626d5411c0af9e8bd4630179c/pdf. [PMC free article] [PubMed]
- 8.Cline RJ, Haynes KM. Consumer health information seeking on the Internet: the state of the art. Health Education Research. 2001;16(6):671–92. doi: 10.1093/her/16.6.671. http://doi.org/10.1093/HER/16.6.671. [DOI] [PubMed] [Google Scholar]
- 9.Dale JR, Williams SM, Bowyer V. What is the effect of peer support on diabetes outcomes in adults? A systematic review. Diabetic Medicine. 2012;29(11):1361–1377. doi: 10.1111/j.1464-5491.2012.03749.x. http://doi.org/10.1111/j.1464-5491.2012.03749.x. [DOI] [PubMed] [Google Scholar]
- 10.Du Honglu, Youngblood Michael G, Pirolli Peter. Efficacy of a Smartphone System to Support Groups in Behavior Change Programs. Proceedings of the Wireless Health 2014 on National Institutes of Health - WH ’14. 2014:1–8. http://doi.org/10.1145/2668883.2668887.
- 11.Eschler Jordan, Dehlawi Zakariya, Pratt Wanda. Self-Characterized Illness Phase and Information Needs of Participants in an Online Cancer Forum. Ninth International AAAI Conference on Web and Social Media. 2015:101–109. [Google Scholar]
- 12.Fox Susannah, Jones Sydney. The social life of health information. Washington, DC: Pew Internet & American Life Project; 2009. pp. 2009–12. [Google Scholar]
- 13.Franklin Victoria Louise, Greene Alexandra, Waller Annalu, Greene Stephen Alan, Pagliari Claudia. Patients’ Engagement with “Sweet Talk” - A Text Messaging Support System for Young People with Diabetes. Journal of Medical Internet Research. 2008;10(2):e20. doi: 10.2196/jmir.962. http://doi.org/10.2196/jmir.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frost Jeana H, Massagli Michael P. Social Uses of Personal Health Information Within PatientsLikeMe, an Online Patient Community: What Can Happen When Patients Have Access to One Another’s Data. Journal of Medical Internet Research. 2008;10:3. doi: 10.2196/jmir.1053. http://doi.org/10.2196/jmir.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Greene Jeremy A, Choudhry Niteesh K, Kilabuk Elaine, Shrank William H. Online Social Networking by Patients with Diabetes: A Qualitative Evaluation of Communication with Facebook. Journal of General Internal Medicine. 2011;26(3):287–292. doi: 10.1007/s11606-010-1526-3. http://doi.org/10.1007/s11606-010-1526-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haldar Shefali, Filipkowski Alex, Mishra Sonali R, et al. “Scared to go to the Hospital”: Inpatient Experiences with Undesirable Events. Proceedings of the American Medical Informatics Association Annual Symposium 2016. 2016:609–617. [PMC free article] [PubMed] [Google Scholar]
- 17.Hartzler Andrea L, Taylor Megan N, Park Albert, et al. Leveraging cues from person-generated health data for peer matching in online communities. Journal of the American Medical Informatics Association. 2016;23(3):496–507. doi: 10.1093/jamia/ocv175. http://doi.org/10.1093/jamia/ocv175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hartzler Andrea L, Mcdonald David W, Park Albert, Huh Jina, Weaver Charles, Pratt Wanda. Evaluating Health Interest Profiles Extracted from Patient-Generated Data. Proceedings of the American Medical Informatics Association Annual Symposium 2014. 2014:626–635. [PMC free article] [PubMed] [Google Scholar]
- 19.Hartzler Andrea, Pratt Wanda. Managing the Personal Side of Health: How Patient Expertise Differs from the Expertise of Clinicians. Journal of Medical Internet Research. 2011;13(3):e62. doi: 10.2196/jmir.1728. http://doi.org/10.2196/jmir.1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Heisler Michele, Vijan Sandeep, Makki Fatima, Piette John D. Diabetes Control With Reciprocal Peer Support Versus Nurse Care Management: A Randomized Trial. Annals of Internal Medicine. 2010;153(8):507–515. doi: 10.7326/0003-4819-153-8-201010190-00007. http://doi.org/10.7326/0003-4819-153-8-201010190-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Høybye Mette Terp, Johansen Christoffer, Tjørnhøj-Thomsen Tine. Online interaction. Effects of storytelling in an internet breast cancer support group. Psycho-Oncology. 2005;14(3):211–220. doi: 10.1002/pon.837. http://doi.org/10.1002/pon.837. [DOI] [PubMed] [Google Scholar]
- 22.Huh Jina, Ackerman Mark S. Collaborative help in chronic disease management. Proceedings of the ACM 2012 conference on Computer Supported Cooperative Work - CSCW ’12. 2012:853. doi: 10.1145/2145204.2145331. http://doi.org/10.1145/2145204.2145331. [DOI] [PMC free article] [PubMed]
- 23.Huh Jina, Liu Leslie S, Neogi Tina, Inkpen Kori, Pratt Wanda. Health Vlogs as Social Support for Chronic Illness Management. ACM Transactions on Computer-Human Interaction. 2014;21(4):23. doi: 10.1145/2630067. http://doi.org/10.1145/2630067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jacobs Maia, Clawson James, Mynatt Elizabeth D. Cancer Navigation: Opportunities and Challenges for Facilitating the Breast Cancer Journey. Proceedings of the 17th ACM Conference on Computer Supported Cooperative Work & Social Computing - CSCW ’14. 2014:1467–1478. http://doi.org/10.1145/2531602.2531645.
- 25.Kaziunas Elizabeth, Buyuktur Ayse G, Jones Jasmine, et al. Transition and Reflection in the Use of Health Information : The Case of Pediatric Bone Marrow Transplant Caregivers. Proceedings of the 18th ACM Conference on Computer Supported Cooperative Work & Social Computing -CSCW ’15. 2015:1763–1774. [Google Scholar]
- 26.Kendall Logan, Mishra Sonali R, Pollack Ari, Aaronson Barry, Pratt Wanda. Making background work visible: opportunities to address patient information needs in the hospital. Proceedings of the American Medical Informatics Association Annual Symposium 2015. 2015:1957–66. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26958295. [PMC free article] [PubMed]
- 27.Lawn Sharon, Smith Ann, Hunter Kelly. Mental health peer support for hospital avoidance and early discharge: An Australian example of consumer driven and operated service. Journal of Mental Health. 2008;17(5):498–508. http://doi.org/10.1080/09638230701530242. [Google Scholar]
- 28.Li Victor, McDonald David W, Eikey Elizabeth V, et al. Losing It Online: Characterizing Participation in an Online Weight Loss Community. Proceedings of the 18th International Conference on Supporting Group Work - GROUP ’14. 2014:35–45. http://doi.org/10.1145/2660398.2660416.
- 29.Liu Leslie S, Huh Jina, Neogi Tina, Inkpen Kori, Pratt Wanda. Health Vlogger-Viewer Interaction in Chronic Illness Management. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems - CHI ’13. 2013:49–58. doi: 10.1145/2470654.2470663. http://doi.org/10.1145/2470654.2470663. [DOI] [PMC free article] [PubMed]
- 30.Liu Leslie S, Inkpen Kori M, Pratt Wanda. “I’m Not Like My Friends”: Understanding How Children with a Chronic Illness Use Technology to Maintain Normalcy. Proceedings of the 18th ACM Conference on Computer Supported Cooperative Work & Social Computing - CSCW ’15. 2015:1527–1539. http://doi.org/10.1145/2675133.2675201.
- 31.Lorig Kate, Ritter Philip L, Laurent Diana D, et al. Online Diabetes Self-Management Program: a randomized study. Diabetes Care. 2010;33(6):1275–1281. doi: 10.2337/dc09-2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maitland Julie, Chalmers Matthew. Designing for peer involvement in weight management. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems - CHI ’11. 2011:315–324. http://doi.org/10.1145/1978942.1978988.
- 33.Makary Martin A, Daniel Michael. Medical error—the third leading cause of death in the US. BMJ. 2016;353:i2139. doi: 10.1136/bmj.i2139. http://doi.org/10.1136/bmj.i2139. [DOI] [PubMed] [Google Scholar]
- 34.McCarthy Danielle M, Ellison Emily P, Venkatesh Arjun K, et al. Emergency department team communication with the patient: The patient’s perspective. Journal of Emergency Medicine. 2013;45(2):262–270. doi: 10.1016/j.jemermed.2012.07.052. http://doi.org/10.1016/j.jemermed.2012.07.052. [DOI] [PubMed] [Google Scholar]
- 35.Miller Andrew D, Mishra Sonali R, Kendall Logan, Haldar Shefali, Pollack Ari H, Pratt Wanda. Partners in Care: Design Considerations for Caregivers and Patients During a Hospital Stay. Proceedings of the 19th ACM Conference on Computer Supported Cooperative Work and Social Computing Companion - CSCW ’16. 2016 doi: 10.1145/2818048.2819983. http://doi.org/10.1145/2818048.2819983. [DOI] [PMC free article] [PubMed]
- 36.Miller Andrew D, Pollack Ari H, Pratt Wanda, Children Seattle. Bursting the Information Bubble : Identifying Opportunities for Pediatric Patient-Centered Technology. Proceedings of the American Medical Informatics Association Annual Symposium. 2016:894–903. [PMC free article] [PubMed] [Google Scholar]
- 37.Mishra Sonali R, Haldar Shefali, Pollack Ari H, et al. “Not Just a Receiver”: Understanding Patient Behavior in the Hospital Environment. Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems - CHI ’16. 2016:3103–3114. doi: 10.1145/2858036.2858167. http://doi.org/10.1145/2858036.2858167. [DOI] [PMC free article] [PubMed]
- 38.Moorhead S Anne, Hazlett Diane E, Harrison Laura, Carroll Jennifer K, Irwin Anthea, Hoving Ciska. A New Dimension of Health Care: Systematic Review of the Uses, Benefits, and Limitations of Social Media for Health Communication. Journal of Medical Internet Research. 2013;15:4. doi: 10.2196/jmir.1933. http://doi.org/10.2196/jmir.1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Morris Dan, Karlson Amy. Dynamic Accessibility Requirements for Hospital Patients. Human Factors. 2011:1–5. [Google Scholar]
- 40.Newman Mark W, Lauterbach Debra, Munson Sean A, Resnick Paul, Morris Margaret E. It’s not that i don’t have problems, i’m just not putting them on facebook. Proceedings of the ACM conference on Computer supported cooperative work - CSCW ’11. 2011:341. http://doi.org/10.1145/1958824.1958876.
- 41.Pollack Ari H, Backonja Uba, Miller Andrew D, et al. Closing the Gap: Supporting Patients’ Transition to Self-Management after Hospitalization. Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems - CHI ’16. 2016:5324–5336. doi: 10.1145/2858036.2858240. http://doi.org/10.1145/2858036.2858240. [DOI] [PMC free article] [PubMed]
- 42.Preece Jenny. Empathic communities: reaching out across the Web. Interactions. 1998;5(2):32–43. http://doi.org/10.1145/274430.274435. [Google Scholar]
- 43.Rotheram-Borus Mary Jane, Tomlinson Mark, Gwegwe Margaret, Comulada W Scott, Kaufman Neal, Keim Marion. Diabetes buddies: peer support through a mobile phone buddy system. The Diabetes educator. 2012;38(3):357–65. doi: 10.1177/0145721712444617. http://doi.org/10.1177/0145721712444617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sarasohn-Kahn J, California Healthcare Foundation The Wisdom of Patients: Health Care Meets Online Social Media. California HealthCare Foundation. 2008 April Retrieved from http://www.chcf.org/publications/2008/04/the-wisdom-of-patients-health-care-meets-online-social-media.
- 45.Sledge William H, Lawless Martha, Sells David, Wieland Melissa, O’Connell Maria J, Davidson Larry. Effectiveness of Peer Support in Reducing Readmissions of Persons With Multiple Psychiatric Hospitalizations. Psychiatric Services. 2011;62(5):541–544. doi: 10.1176/ps.62.5.pss6205_0541. http://doi.org/10.1176/ps.62.5.pss6205_0541. [DOI] [PubMed] [Google Scholar]
- 46.Strauss Juliet M, Corbin Anselm L. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. 1998 http://doi.org/10.1017/CBO9781107415324.004.
- 47.Verheijden MW, Bakx JC, van Weel C, Koelen MA, van Staveren WA. Role of social support in lifestyle-focused weight management interventions. European Journal of Clinical Nutrition. 2005;59:S179–S186. doi: 10.1038/sj.ejcn.1602194. http://doi.org/10.1038/sj.ejcn.1602194. [DOI] [PubMed] [Google Scholar]
- 48.Webb Marianne, Burns Jane, Collin Philippa. Providing online support for young people with mental health difficulties: challenges and opportunities explored. Early Intervention in Psychiatry. 2008;2(2):108–113. doi: 10.1111/j.1751-7893.2008.00066.x. http://doi.org/10.1111/j.1751-7893.2008.00066.x. [DOI] [PubMed] [Google Scholar]
- 49.Webster Mary, Foster Emma, Comber Rob, Bowen Simon, Cheetham Tim, Balaam Madeline. Understanding the lived experience of adolescents with type 1 diabetes. Proceedings of the 14th International Conference on Interaction Design and Children - IDC ’15. 2015:140–149. http://doi.org/10.1145/2771839.2771854.
- 50.White M, Dorman SM. Receiving social support online: implications for health education. Health Education Research. 2001;16(6):693–707. doi: 10.1093/her/16.6.693. http://doi.org/10.1093/HER/16.6.693. [DOI] [PubMed] [Google Scholar]
- 51.Winzelberg Andrew J, Classen Catherine, Alpers Georg W, et al. Evaluation of an internet support group for women with primary breast cancer. Cancer. 2003;97(5):1164–1173. doi: 10.1002/cncr.11174. http://doi.org/10.1002/cncr.11174. [DOI] [PubMed] [Google Scholar]
- 52.Fast Facts on US Hospitals. 2014 Retrieved from http://www.aha.org/research/rc/stat-studies/fast-facts.shtml.


