Abstract
Objective
Compare syphilis investigation yield among patient groups using number needed to interview.
Goal
To increase investigation efficiency.
Study Design
Retrospective review of North Carolina 2015 syphilis investigations, using the number of cases needed to interview (NNTI) and the number of cases and contacts needed to interview (TNTI) to compare yield of new syphilis and HIV diagnoses between patient groups.
Results
We reviewed 1,646 early syphilis cases and 2,181 contacts; these yielded 241 new syphilis cases (NNTI=6.9; TNTI=16.4) and 38 new HIV cases (NNTI=43). Interviews of women (prevalence difference (PD)=6%, 95% CI 12–16), patients <30 years old (PD=5%, 95% CI 1–8), and patients with titer >1:16 (PD=5%, 95% CI 1–9) yielded more new syphilis cases in our adjusted model; no other patient factors increased investigation yield.
Conclusions
NNTI and TNTI are useful measures of efficiency. Prioritizing early syphilis investigation by gender, RPR titer, and age provides small increases in efficiency; no other factors increased efficiency.
Keywords: syphilis, North Carolina, NNTI, HIV, partner services, contact investigation, Southeast, South
Striking increases in syphilis have been observed across the United States since 2000. 1 These increases were first observed in larger urban areas and have since been noted more widely, including in the Southeastern U.S. A mainstay of syphilis control has been to locate and treat contacts. 2 However, given the scope of current outbreaks, it is not possible to find, interview, and treat every contact. Mathematical modeling suggests that offering treatment to 50% of partners of people with syphilis reduces syphilis prevalence. 3 Therefore, contact investigations can be prioritized for syphilis cases most likely to transmit disease to partners.
Historically, syphilis stage and age/titer categories (ie, reactor grids) have been used to prioritize contact investigation; primary and secondary stages are more likely to be associated with ongoing transmission. 4 Other options for prioritizing partner services include the use of serologic indicators of recent infection (ie, Rapid Plasmin Reagin (RPR) or Venereal Disease Research Laboratory (VDRL) titer), local disease epidemiology (eg, young men), and location of the patient in certain settings or networks (eg, reporting meeting sex partners using particular phone apps).
Ideally, partner investigation would be limited to the groups most likely to transmit disease – that is, prioritized for efficiency. Efficiency has been quantified in many ways, 5,6 including as the number of treated partners per case interview, 7 likelihood and magnitude of future transmission, 4 and number of infected partners found per case. 8,9 More recently, calculation of the number of patients needed to interview to identify a new case of disease that is, number needed to interview (NNTI), has been used to assess the efficiency of partner investigation. 10,11,12 The NNTI directly measures public health effort and can be used as a measure to compare intervention types across diseases.
This analysis assesses partner investigation efficiency among demographic and behavior groups by quantifying the number of people with syphilis needed to interview to identify a new syphilis case, and comparing this NNTI between people with primary and secondary vs. early latent syphilis and between demographic and behavioral groups. Recent syphilis increases have been concentrated among men and among men living with HIV, increasing the risk of syndemic disease transmission. 13 Therefore, we also assessed the NNTI to identify new cases of HIV from syphilis investigation. Based on previous analysis of North Carolina data 14 we hypothesize that the yield of new cases of syphilis and HIV would be similar for all early syphilis stages, but may differ by RPR titer or other demographic and risk factors.
Methods
In North Carolina, Disease Intervention Specialists (DIS) conduct interviews and offer partner investigation services to all people with primary, secondary, and presumed early latent syphilis reported to the North Carolina Division of Public Health. Index patients were defined as individuals diagnosed with early syphilis, and were asked to provide the number of and locating information for contacts during their potential infectious period (3 months for primary cases, 7 months for secondary, and 12 months for early latent); patients not interviewed either could not be located or refused. Contacts were then notified by the DIS of their exposure. All identified contacts were offered HIV and syphilis testing and treatment if exposed and not previously treated. Information collected by DIS was entered into the North Carolina Electronic Disease Surveillance System, a highly-customized Maven system (Consilience, Austin TX) used in North Carolina to capture surveillance and case investigation data for all reportable diseases.
We analyzed syphilis cases reported between January 1 and December 31, 2015. We defined a new syphilis case in a contact as an infection in a contact named by the index patient when the date of the contact’s diagnosis was within 60 days after the diagnosis date of the index patient. The total number of contacts included those that were anonymous or un-locatable as well as those for whom locating information was provided. Some people were named by more than one index patient; these were counted separately since they reflected separate case investigations. We calculated the NNTI (total index patient interviews/total new syphilis cases diagnosed in contacts) and total needed to interview (TNTI) (total index patient+contact interviews/total new syphilis cases diagnosed in contacts).
We estimated the proportion (prevalence) of index case investigations yielding new cases of syphilis and HIV. While NNTI is a simple calculation, confidence intervals for NNTI are difficult to interpret and model. 15 Prevalence difference (PD) is the inverse of NNTI and allows us to straightforwardly generate 95% confidence intervals and use models to adjust for the contribution of multiple variables. We used prevalence difference confidence intervals to assess the statistical significance of differences between groups. Generalized linear models with a binomial distribution were used to estimate PD and 95% CI for index case investigations yielding at least one new case of syphilis or HIV, and for contact investigations yielding a new diagnosis of syphilis by selected variables. The difference in the proportion and number of index case investigations that yielded at least one new case were compared by the following risk factors: stage (primary or secondary vs. early latent stage), race/ethnicity ( Black/African American vs. other race/ethnicity groups), age (<30 versus ≥30 years), gender, provider type, men reporting sex with men (MSM) vs. men reporting sex with women only, titer (≤1:16 vs. >1:16), reported history of injection drug use (IDU), report of exchanging sex for drugs or money during the infectious period and report of ever meeting sex partners online (internet or phone apps) in the past year. Because there were very few cases among Asians, Native Americans, Alaska natives, Native Hawaiians, and Pacific Islanders, these were grouped as “other race”. Provider type was categorized as high yield (>13% of contacts of index patients reported by these providers tested positive for syphilis) vs. lower yield (13% or less). High-yield provider types were: HIV counseling and testing sites, emergency departments, school-based clinics, blood banks, and “other”. Lower-yield provider types were: STD clinics, family planning and obstetrics, private doctor, correctional facility, JobCorps, and military.
We conducted a two-step modeling process. In our first model, we only included information reliably available prior to the patient interview (stage, age, gender, provider type, and titer), and assessed whether an index case interview yielded at least one new diagnosis of syphilis or HIV in a contact. The first step provides information about which patients to interview. The second step included information available following the index interview (all of the above, race/ethnicity, gender of contacts, and whether the index patient met partners online or via phone apps, reported exchanging sex or drugs for money, reported injection drug use or was a man who reported sex with men), and assessed whether any individual contact was newly diagnosed with syphilis. The second step provides information about whether to interview the contacts of an index patient with the relevant information. Some contacts were named by more than one patient or in more than one disease event. Because we were assessing interview data and interview burden, we kept all contact interviews in the second step. However, in order to count cases among contacts, we de-duplicated the number of new cases, to count each new case only once. To account for the correlation between contacts of a given case, generalized linear modeling with robust standard errors (SAS 9.4, Cary, North Carolina) was used to model these data. We retained all variables that were statistically significant in bivariate comparisons in the multivariate model.
Data used for this analysis were de-identified surveillance data. The North Carolina Department of Public Health approved this project as program evaluation not involving identifiable human subjects.
Results
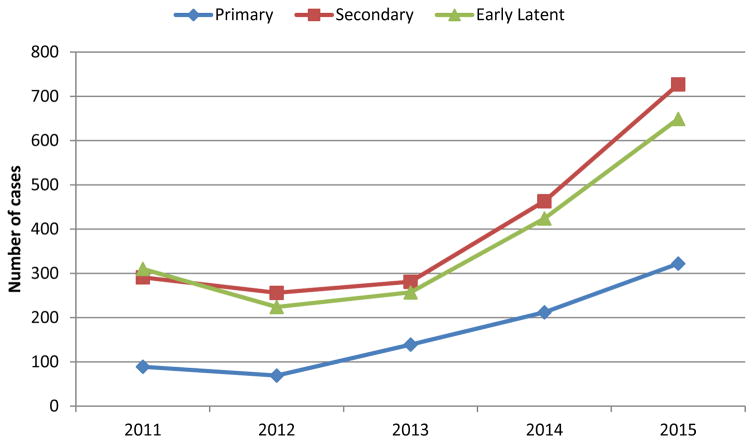
A total of 322 cases of primary syphilis, 727 cases of secondary syphilis, and 649 cases of early latent syphilis were reported in 2015 (N=1698; Figure 1). This was a 55% increase over the 1099 early syphilis cases in 2014. We excluded 52 cases missing gender information, leaving a final data set of 1646 patient records (309 primary, 700 secondary, and 637 early latent cases). DIS conducted interviews with 99% of these patients (1623 case-patients).
Figure 1.
Primary, Secondary, and Early Latent Syphilis, North Carolina, 2011–2015
The majority of index patients were men (N=1455; 88%), of whom 76% (N=1109) reported sex with men (Table 1). Seven syphilis index patients were recorded as transgender (female to male) during this period; due to this small number, no analyses on transgender people are included here, and these cases were excluded from the analysis. Half of women (N=96; 50%) and 63% of men (N=913) were diagnosed with infectious (primary or secondary) syphilis. African-Americans accounted for 66% of all index patients; 49% of index patients were <30 years of age. Stage of syphilis infection did not differ by race/ethnicity or age.
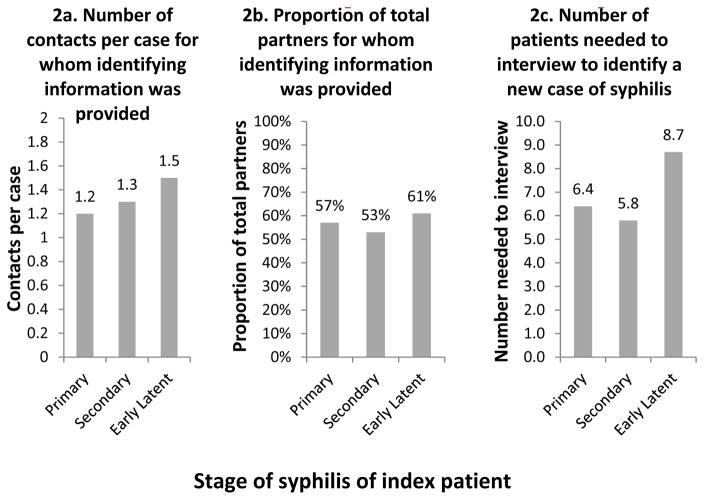
During the interviews, 3872 contacts were reported by 1407 early syphilis patients. Index patients provided identifying information for 2265 contacts. Overall, the number of contacts named per index case was 1.4; 1.2 contacts per index case were named for primary syphilis (N=368), 1.3 per index case for secondary syphilis (N=941), and 1.5 for early latent syphilis(N=956). The proportion of total contacts for whom identifying information was provided was similar for all three stages of infection; primary, 57%; secondary, 53%; early latent, 61% (Figure 2).
Figure 2.
Comparing outcomes of syphilis investigation by stage of syphilis in index patient
Two hundred and twenty (13%) of the 1646 index patient investigations yielded 241 new cases of syphilis among contacts. Similar proportions of new syphilis cases were diagnosed among contacts of index patients with primary or secondary syphilis (15%) and early latent syphilis (11%). The majority of the 241 new cases diagnosed among contacts (138 (57%)) were primary or secondary stage (ie infectious) syphilis. Most contacts with infectious syphilis were partners of index patients who also had infectious syphilis (108/138 (78%)). The number of index patient interviews needed to identify a new case of syphilis was 6.9 overall, and varied by stage: 6.4 for primary cases, 5.8 for secondary, and 8.7 for early latent (Figure 2). The total number interviewed (including contact interviews as well as index patient interviews) was 3911, and the total number needed to interview to identify one new case of syphilis was 16.2.
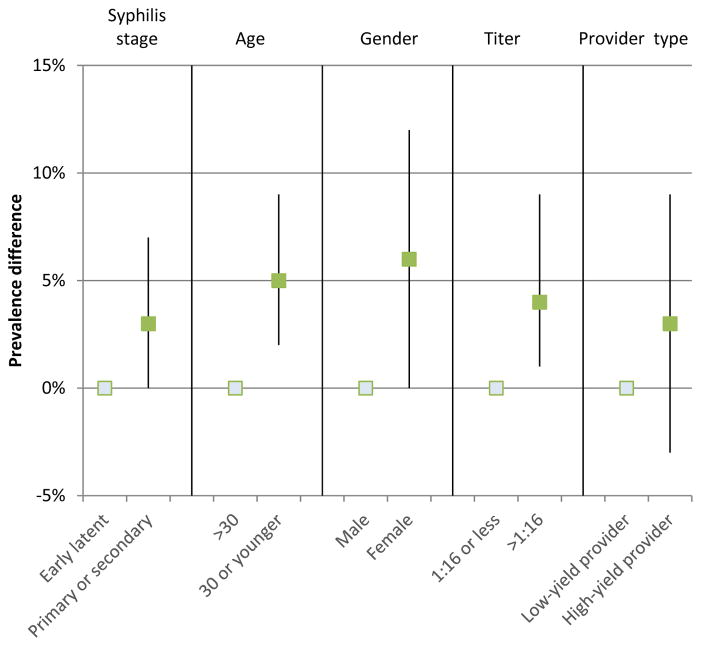
Investigations of female patients were more likely to yield new cases (19% of interviews of women compared to 13% of interviews of men yielded a new case; PD= 6%, CI 1%,13%). We did not observe a difference in case yield by index patient race nor Hispanic ethnicity. New syphilis cases were identified more often from case investigations of index patients <30 years of age, (PD compared to older people=5%, CI 1%,8%), and those with RPR titer>1:16 (PD compared to lower titer=5%, CI 1%,9%). No other factors identified a significantly increased new case yield. A multivariable model was used to identify the independent contributions of these factors to finding new cases. The significant adjusted differences in the prevalence of new cases found among index patients were: females vs. males, 6%, CI 0%,12%; RPR titer greater than 1:16 compared to 1:16 or lower, 4%, CI 1%, 9%; age less than 30, 5%, CI 2%, 9% (Figure 3). While gender was not significant, because of the importance of congenital syphilis, we retained gender in our prioritization algorithm. Prioritization of all women, men of any age with a titer >1:16, and men <30 years of age with titer 1:16 would result in interviewing 1324 patients (82% of index patients) and identifying 211 new cases (88% of new cases), for a decreased NNTI of 6.3.
Figure 3.
Adjusted prevalence differences for information available prior to interview; model outcome is the number of patient interviews yielding new cases
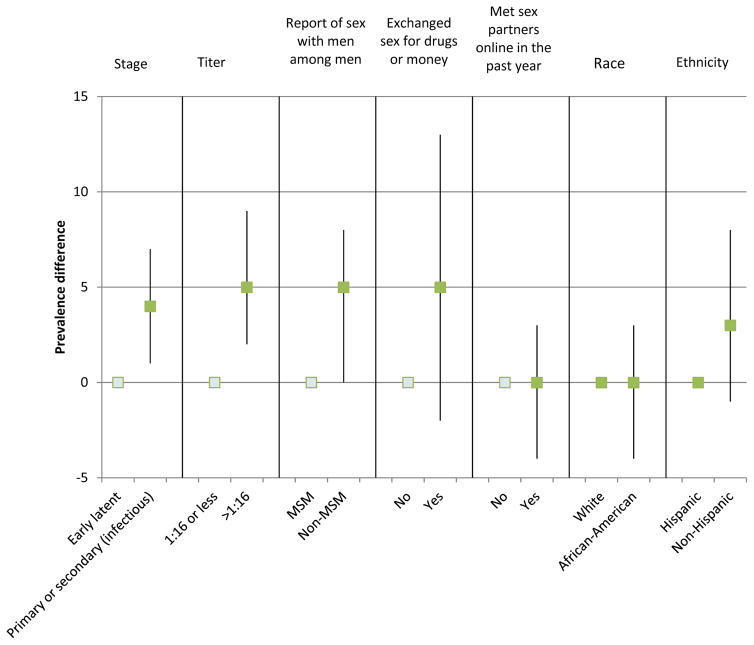
Subsequently, we assessed factors that would help prioritize which contacts of the 1324 index patients identified in the first model should be interviewed. For this step, our outcome was whether any individual contact was diagnosed with syphilis. In unadjusted analysis, stage, titer, and provider type were significant predictors of a new diagnosis of syphilis among contacts; 12% of contacts from patients seen by low-yield providers were diagnosed, compared to 19% of contacts of patients seen by high-yield providers (PD 7%, CI 1%,13%). In adjusted analysis, infectious stage (PD, 4%, CI 1%, 7%) and titer (PD 5%, CI 2%, 9%) were statistically significant predictors of new syphilis diagnoses among contacts (Figure 4). The 1324 patients prioritized in the first round of modeling named 1840 partners. Prioritizing interviews of contacts of index patients diagnosed with an infectious stage of syphilis in this group would result in interviewing 1132 contacts and identifying 159 new syphilis cases (66% of new cases).
Figure 4.
Adjusted prevalence differences for information available following interview; model outcome is number of newly diagnosed contacts
Without prioritization, we contacted 1646 index patients and 2181 contacts, and identified 233 new cases, for an NNTI of 6.9 and a TNTI of 16.2. After the first prioritization step, interviewing all female patients, male patients with titer >1:16, and male patients younger than 30 and with titer 1:16 or less would result in 1324 index patient and 1840 contact interviews, and would identify 211 (88%) of the new syphilis cases, for an NNTI of 6.3 and a TNTI of 15. After both prioritization steps, we would interview 2636 index patients and contacts and identify 159 (66%) of the new cases, for a TNTI of 16.5; therefore, we identified no additional value from the second prioritization step.
Thirty-eight contacts named by 35 original/index case patients were diagnosed with HIV as a result of syphilis partner services. The NNTI to identify at least one new case of HIV was 43 overall; TNTI was 101. All new HIV cases were diagnosed among partners of male index patients. With the exception of gender, similar patterns were seen for identifying new cases of HIV: there was no difference by stage or race/ethnicity; while there were more diagnoses among men younger than 30, the difference was small (3% of men younger than 30 and 2% of men older than 30). New diagnoses of HIV were found in a higher proportion of interviews of men reporting sex with men (3% vs 1%, PD 2%, CI 1%, 4%) and meeting sex partners online in the past year (4% vs 1%, PD 3%, CI 1%, 6%). Interviewing the group of patients identified in the first prioritizing round would identify 26/38 new HIV diagnoses (68%) for an NNTI of 51 and a TNTI of 122. The large majority of patients who reported sex with online partners or were MSM were captured in the titer>1:16 or age<30 groups; adding the remaining patients with these characteristics did not improve case-identification efficiency.
Discussion
This analysis identified gender, age and titer as indicators which increase the efficiency of syphilis case investigation; however, the efficiencies gained were small. During 2015 in North Carolina, 13% of syphilis investigations yielded a contact diagnosed with syphilis; our numbers of contacts named and new cases found were similar to those found in other studies. 8,7,16 The number of index patients needed to interview (NNTI) to identify one new case of syphilis was 6.9; however, this number does not measure the full effort of syphilis investigations. Including interviews of both the index patients and their contacts, the TNTI was more than double this number (16.2). Limiting the patients interviewed to women, men of any age with RPR titer >1:16, and men with RPR titer ≤1:16 and <30 years old reduces NNTI and TNTI, while identifying 86% of syphilis cases and 68% of HIV cases. NNTI and TNTI were both useful measures in our setting.
The NNTI to identify new cases of HIV among syphilis contacts (N=51) is within the range of nationally published numbers of people with HIV needed to interview to identify new HIV cases (range: 1.3–100). 17,5,11 This demonstrates that during our current epidemic, with high levels of HIV and syphilis coinfection, syphilis case investigation is as efficient as HIV case investigation in identifying newly-diagnosed HIV infection.
NNTI allows us to compare the value of interventions across diseases and jurisdictions. We explored the value of NNTI in defining potential efficiencies in our syphilis investigations. NNTI was originally defined as a measure of patients needed to treat; 18 however, the full burden of contact tracing and treatment for sexually transmitted diseases includes both contact and index patient interviews. To address this, we calculated TNTI. In North Carolina, NNTI and TNTI showed similar patterns, suggesting that NNTI is a reasonable proxy for TNTI. However, it is important to remember that NNTI may be less useful to describe the full burden of intervention and amount of person-time invested. If interviewing contacts was particularly low-yield in a subset of index patients (ie, a program was interviewing a particularly high number of contacts per index patient in the sub-group to diagnose a new case), TNTI could show a different pattern from NNTI and provide a more accurate depiction of the effort required to identify one new case of syphilis through partner services.
Logic suggests that primary and secondary syphilis stage should be an indicator of higher yield investigations, since syphilis transmission was likely to have been more recent, thus the index patient should have a better recall of sexual partners including their contact information. Although stage was not the most important indicator in our analysis, more new cases were identified among contacts of index patients with infectious stage as compared to early latent stage syphilis. The number of contacts identified, both named and anonymous, did not differ by stage in our analysis. Our data do not strongly support prioritizing interviews by stage among early syphilis patients.
In addition to assessing many of the traditional characteristics of syphilis index patients (stage, gender, age, titer, provider type), we analyzed two factors that are particularly relevant to the current syphilis increases in the US, 19 but have not been assessed as indicators of high-yield investigation: report of sex with men among men and use of online websites or phone apps to meet partners. We showed that, in this Southeastern US population as in other populations, 8,20 while men reporting sex with men provide locating information for a smaller proportion of total partners compared to non-MSM, the proportion of partners named and the number of new cases identified per patient interviewed were similar to the other groups in our population. Perhaps because our index patient population was largely MSM, prioritizing interviews of MSM did not significantly change our outcome.
Despite our introduction of factors characteristic of our current epidemic, our analysis confirms previous studies finding that changes to partner notification are unlikely to greatly increase efficiency, because there is too little differentiation between groups identified by our commonly-collected risk factors. 7,8,21,4,22 This may signal that the public health establishment has not understood the community we are serving well enough to be asking the right questions to efficiently find new cases of syphilis. Further conversations between the public health community, syphilis index patients and those at risk of acquiring syphilis is needed to identify additional potential factors to assess (eg, specific phone apps; being linked to many partners in a network (network centrality); and total number of partners). Alternatively, these findings may indicate that we should look elsewhere for efficiency. Potential targets might include working to decrease the gap between syphilis screenings, shown to be effective in decreasing syphilis in mathematical models, 3 or working to decrease the time to treatment among index patients and contacts.
Limitations
NNTI calculations were based on new cases diagnosed among contacts, rather than by using disposition information assigned by disease investigation staff as has been done in the past. The advantage of our method is that diagnosis is confirmed and that the complexities of how dispositions are recorded are avoided. In not using disposition, we did not differentiate between contacts treated prior to public health intervention (i.e., disease investigation disposition E) and contacts treated as a result of public health intervention (i.e., disease investigation disposition C). Our goal was to measure the yield of the total investment in investigation, and all contacts were investigated, regardless of prior treatment. For this reason, we chose to calculate NNTI based on all new cases. This analysis also does not attempt to count potential cases prevented by prophylactic treatment among contacts. Including those contacts prophylactically treated as infected, or assuming that a fraction of these would be infected, would decrease the NNTI. We did not have complete contact information; some syphilis patients are likely sex partners of other syphilis patients for whom we did not have linking information. With perfect contact information, the NNTI would be lower. Finally, given the continued cultural stigma of male-male partnerships in the Southeast, 23 it is likely that our information on sex partner choice and use of electronic means such as phone apps and websites to find partners was incomplete.
Conclusion
Syphilis partner services are an important method of case-finding for both syphilis and HIV. The traditional factors of age, gender and titer are straightforward and useful indicators of priority; we found that use of the internet or phone apps to meet partners was a less useful indicator. NNTI and TNTI indicate the resources needed to find new cases of syphilis, and are useful for understanding the level of resources needed and for increasing program efficiency. Modeling prevalence difference can help to use these tools. More work is needed to help the public health workforce recognize patient indicators that can most effectively and efficiently identify new syphilis and HIV cases.
Acknowledgments
Financial support
This project was supported by the US Centers for Disease Control and Prevention and the State of North Carolina but did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
We gratefully acknowledge the effort and contribution of the disease investigation staff whose work is analyzed here. We are also grateful to Aaron Fleischauer, Roger Follas, and Mike Cassell for thoughtful comments on the analysis.
Footnotes
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily reflect the official position of the Centers for Disease Control and Prevention, or the authors’ affiliated institutions.
Contributor Information
Erika Samoff, North Carolina Division of Public Health Communicable Disease Branch.
Anna B Cope, Centers for Disease Control and Prevention, Division of Sexually Transmitted Disease Prevention.
Jason Maxwell, North Carolina Division of Public Health Communicable Disease Branch.
Francina Thomas, North Carolina Division of Public Health Communicable Disease Branch.
Victoria L Mobley, North Carolina Division of Public Health Communicable Disease Branch.
References
- 1.Centers for Disease Control and Prevention Division of Sexually Transmitted Diseases. Sexually Transmitted Disease Surveillance 2014. Atlanta: 2014. [Google Scholar]
- 2.Rothenberg RB, Potterat JJ. Sexually Transmitted Diseases. New York: McGraw-Hill; 1990. Strategies for management of sex partners. [Google Scholar]
- 3.Gray RT, Hoare A, Prestage GP, et al. Frequent testing of highly sexually active gay men is required to control syphilis. Sex Transm Dis. 2010;37(5):298–305. doi: 10.1097/OLQ.0b013e3181ca3c0a. [DOI] [PubMed] [Google Scholar]
- 4.Kahn RH, Peterman TA, Arno J, et al. Identifying likely syphilis transmitters: implications for control and evaluation. Sex Transm Dis. 2006;33(10):630–635. doi: 10.1097/01.olq.0000216063.75575.f8. [DOI] [PubMed] [Google Scholar]
- 5.Hogben M, Collins D, Hoots B, et al. Partner services in sexually transmitted disease prevention programs: A review. Sex Transm Dis. 2015;43(2 Suppl 1):1–10. doi: 10.1097/OLQ.0000000000000328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rothenberg R. The transformation of partner notification. Clin Infect Dis. 2002;(Suppl 2):S138–45. doi: 10.1086/342101. [DOI] [PubMed] [Google Scholar]
- 7.Marcus JL, Katz MH, Katz KA, et al. Prediction model to maximize impact of syphilis partenr notification - San Francisco, 2004–2008. Sex Transm Dis. 2010;37(2):109–114. doi: 10.1097/OLQ.0b013e3181bbf985. [DOI] [PubMed] [Google Scholar]
- 8.Hoots BE, Lewis FM, Anschuetz G, et al. Would targeting increase efficiency of syphilis partner services programs? - Data from New York City, Philadelphia, Texas, and Virginia. Sex Transm Dis. 2014;41(6):407–412. doi: 10.1097/OLQ.0000000000000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peterman TA, Furness BW. Public health interventions to control syphilis. Sex Hlth. 2015;12:126–134. doi: 10.1071/SH14156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Golden MR, Stekler J, Kent JB, et al. An evaluation of HIV partner counseling and referral services using new disposition codes. Sex Transm Dis. 2009;36(2):95–101. doi: 10.1097/OLQ.0b013e31818d3ddb. [DOI] [PubMed] [Google Scholar]
- 11.Ahrens K, Kent CK, Kohn RP, et al. HIV partner notification outcomes for HIV-infected patients by duration of infection, San Francisco, 2004 to 2006. J Acquir Immune Defic Syndr. 2007 Dec;46(4):479–484. doi: 10.1097/qai.0b013e3181594c61. [DOI] [PubMed] [Google Scholar]
- 12.Brewer DD. Case-finding effectiveness of partner notification and cluster investigation for sexually transmitted diseases/HIV. Sex Transm Dis. 2005 Feb;32(2):78–83. doi: 10.1097/01.olq.0000153574.38764.0e. [DOI] [PubMed] [Google Scholar]
- 13.North Carolina Department of Health and Human Services Division of Public Health. 2015 North Carolina HIV/STD Surveillance Report. Raleigh: 2015. [Google Scholar]
- 14.Mobley V, Hilton M, Vanhoy T, et al. Comparison of the case-finding effectiveness of partner notification services for early syphilis cases in North Carolina. Presented at: 2014 STD Prevention Conference [5C 4]; Atlanta. [Google Scholar]
- 15.Altman DG. Confidence intervals for the number needed to treat. BMJ. 1998;7168:1309–1312. doi: 10.1136/bmj.317.7168.1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kohl KS, Farley TA, Ewell J, et al. Usefulness of partner notification for syphilis control. Sex Transm Dis. 1999 Apr;26(4):201–207. doi: 10.1097/00007435-199904000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Katz DA, Hogben M, Dooley SW, et al. Increasing public health partner services for human immunodeficiency virus: results of a second national survey. Sex Transm Dis. 2010;37(8):469–475. doi: 10.1097/OLQ.0b013e3181e7104d. [DOI] [PubMed] [Google Scholar]
- 18.Laupacis A, Sackett DL, Roberts RS. An assessment of clinically useful measures of the consequences of treatment. New Engl J Med. 1988;318(26):1728–1733. doi: 10.1056/NEJM198806303182605. [DOI] [PubMed] [Google Scholar]
- 19.Bernstein KT, Stephens SC, Strona FV, et al. Epidemiologic characteristics of an ongoing syphilis epidemic among men who have sex with men, San Francisco. Sex Transm Dis. 2013;40(1):11–17. doi: 10.1097/OLQ.0b013e31827763ea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Samoff E, Koumans EH, Katkowsky S, et al. Contact-tracing outcomes among male syphilis patients in Fulton County, Georgia, 2003. Sex Transm Dis. 2007;34(7):456–460. doi: 10.1097/01.olq.0000251203.34805.28. [DOI] [PubMed] [Google Scholar]
- 21.Gunn RA, Harper SL. Emphasizing infectious syphilis partner notification. Sex Transm Dis. 1998;25(4):218–219. doi: 10.1097/00007435-199804000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Engelgau MM, Woernle CH, Rolfs RT, et al. Control of epidemic early syphilis: the results of an intervention campaign using social networks. Sex Transm Dis. 1995;22(4):203–209. [PubMed] [Google Scholar]
- 23.Reif SF, Whetten K, Wilson ER, et al. HIV/AIDS in the Southern USA: A disproportionate epidemic. AIDS Care. 2014;26(3):351–359. doi: 10.1080/09540121.2013.824535. [DOI] [PubMed] [Google Scholar]