Abstract
Purpose:
To describe a case of severe rosacea with ocular involvement.
Case Report:
A 28-year-old female patient presented with extensive facial and ocular eruptions. She had a history of treatment with oral prednisolone due to the clinical diagnosis of lupus erythematosus (LE), which had resulted in transient improvement of the lesions, but was followed by exacerbation of the lesions. With the clinical diagnosis of severe oculofacial rosacea, she was successfully treated with oral doxycycline, steroid eye drops, and ocular lubricants. Histopathological features of skin biopsy were consistent with rosacea in the context of infection with Demodexfolliculorum. After four years, a relapse of the oculofacial lesions occurred, for which retreatment with oral tetracycline, steroid eye drops, and ocular lubricants was administered.
Conclusion:
Rosacea can be extremely severe and disfiguring, and it can be misdiagnosed as the pathognomonic butterfly rash of LE. Demodex carriage in rosacea is consistent and may play a significant role in the severe forms.
Keywords: Demodex Folliculorum, Lupus Erythematosus, Rosacea
INTRODUCTION
Rosacea is a common chronic skin and ocular condition,[1,2,3] characterized by intermittent periods of exacerbation and remission.[4] Rosacea affects mainly adults around the age of 30 years and predominantly affects females.[5] Reported prevalence rates of rosacea range from 0.09% to 10%.[6] The pathogenesis of rosacea is poorly understood and controversial.[7] Characteristic facial or ocular inflammation in rosacea involves both the vascular and stromal tissue of skin. A wide spectrum of clinical findings of rosacea is often observed.[8] Herein, we describe a very severe case of rosacea with exuberant facial and ocular lesions.
CASE REPORT
A 28-year-old female patient presented to our eye clinic with extensive exanthematous lesions consisting of erythematous papules, nodules, pustules, and nodulocystic eruptions involving the face, forehead, nose, and both eyes. She had previously received oral prednisolonefor lupus erythematosus (LE), which resulted in transient improvement of the lesions, followed by severe exacerbation [Figure 1].
Figure 1.

Severe papular and pustular eruptions on the forehead, face, and nose.
With the clinical diagnosis of severe oculofacial rosacea, the patient was treated with oral doxycycline (100 mg BID for two weeks), prednisolone (1% eye drops QID), and Artelac eye drops (Bausch & Lomb, UK limited; QID), leading to the improvement of the lesions [Figure 2].
Figure 2.

Improvement of severe papules and pustules on the forehead, face, nose, and in some areas of both eyes, following treatment with oral doxycycline.
All baseline laboratory investigations including the purified protein derivative (PPD) skin test and serum anti-nuclear antibody (ANA) were unremarkable. However, the erythrocyte sedimentation rate (ESR) was elevated (40 mm/hour). Histological examination of punch biopsies of facial skin lesions revealed conspicuous, superficial acute inflammation intermixed with parakeratosis, marked acanthosis with spongiosis, enlarged dilated vascular channels, foci of intradermal chronic inflammation, and presence of Demodex mites within the pilosebaceous units [Figure 3]. The histopathological features were consistent with rosacea. No histologic indicating LE was present.
Figure 3.
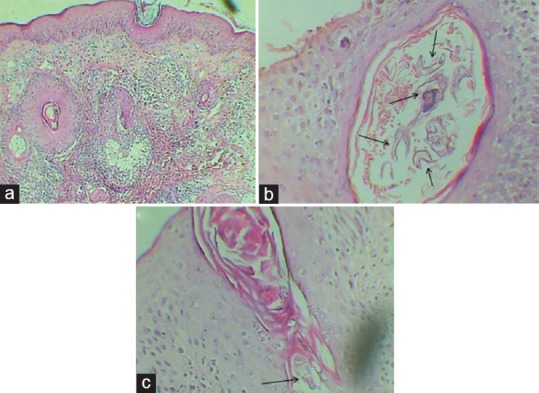
Histopathological features of skin specimens. Note the presence of intradermal chronic inflammation (a, H and E, magnification ×100) together with fragments of Demodex mites within the pilosebaceous units (b and c, H and E, magnification ×400).
After four years, she presented to our eye clinic with a new exacerbation of severe exudative papules and erythematous nodules, pustules, and nodulocystic lesions involving the face, forehead, nose, and left eye [Figures 4 and 5]. Ocular involvement consisted of perilimbal injection and distinctive inferior corneal phlyctenules. Additionally, there were mild cutaneous extrafacial lesions in the anterior part of the neck, chest, and both forearms [Figures 6a and 6b]. During the course of the exacerbation, the lesions had become densely confluent and intensely inflammatory and exudative, with a crusty surface [Figure 7].
Figure 4.

Recurrence of severe papules and erythematous nodules, pustules, and nodulocystic lesions involving the forehead, face, nose, and chin.
Figure 5.

Severe left eye conjunctivitis and inferior peripheral corneal phlyctenules.
Figure 6.

Lesions on the neck, chest, and forearm (a and b).
Figure 7.

Densely confluent, intensely inflammatory and exudative lesions, with a crusty surface.
Microbiologic investigation results were negative in terms of the presence of fungal and bacterial elements. Findings of repeat histological examination of the skin lesions was the same as in the previous study and suggestive of rosacea due to Demodexfolliculorum infection.
Therefore, the patient was treated with oral tetracycline capsule (250 mg QID for two weeks), prednisolone (1% eye drops QID for two weeks), and Artelac eye drops (TID) for several months. Gradual resolution of the lesions occurred. Two months later, facial erythema persisted, but complete resolution of the lesions was achieved on the eyes, neck, and both forearms [Figure 8]. During the last follow-up (six months later), complete resolution of the facial lesions was observed [Figure 8]. Written consent was obtained from the patient in order to present her oculofacial features via photographs in the current case report.
Figure 8.

Improvement of lesions on the face and forearm, after medication.
DISCUSSION
Rosacea is a chronic inflammatory skin condition that commonly presents with facial or ocular involvement.[9] According to the National Rosacea Society (NRS), recognition of rosacea is based mainly on clinical criteria divided into primary and secondary categories.[10] Primary criteria include transient facial erythema (flushing), nontransient erythema, papules, pustules, and telangiectasia. The presence of one or more of these signs with a central facial distribution is considered highly indicative of rosacea, as in our case. Secondary diagnostic criteria are often met with one or more of the primary features of rosacea. They include burning or stinging skin sensations, elevated red plaques without epidermal changes, dry skin appearance, edema, peripheral location, ocular manifestations, and phymatous changes. In the present case, the ocular involvement was very prominent.
There are four main rosacea subtypes: erythematotelangiectatic, papulopustular, phymatous, and ocular rosacea. Variants of rosacea, which do not strictly match the morphologic patterns or combinations seen in these rosacea subtypes, may occur.[10] Our patient had all morphologic patterns of rosacea except phymatous changes.
Patients with rosacea often present with a various symptoms and signs of the disease, so an individualized treatment plan should be tailored to a patient's unique clinical presentation and the exact pathophysiology of rosacea is poorly understood. However, most researchers now agree that the pathophysiology involves two primary factors: inflammation and vascular abnormalities. It has recently been proposed that innate immune mechanisms and changes in the regulation of the neurovascular system together initiate and perpetuate rosacea.[11] Vascular abnormalities result in blood vessel dilation with increased capillary permeability and edema, which in turn provide a favorable setting for the proliferation and colonization of Demodex mites. In the present case, the histopathological reports revealed the presence of Demodex in the hair follicles. Demodex mites are almost always present in histological samples from individuals with papulopustular rosacea. This parasite stimulates inflammation, increasing the likelihood of papulopustular or granulomatous lesions. Additional inflammatory actions, including the release of oxygen free radicals, also contribute to dermal and blood vessel damage. Both inflammatory infiltrate and vascular changes can be easily observed using routine histologic staining.[12]
Rosacea manifests in a variety of clinical presentations; therefore, various medical therapies are available to treat the various signs and symptoms. Currently, there is no cure for the condition;[13] however, a wide range of medications are used for the treatment of rosacea. Topical medications include metronidazole, azelaic acid, benzoyl peroxide, antibiotics, sulfacetamide/sulfur, and retinoids, while oral medications used for this purpose include tetracyclines, metronidazole, isotretinoin, and macrolides.[14]
Previously available medications for rosacea have all targeted the inflammatory erythematous papules and pustules frequently associated with the disease, leaving a therapeutic gap for the common manifestation of persistent facial erythema. This “facial erythema treatment gap” was easily seen in the present patient after treatment with oral tetracycline. Brimonidine tartrate (0.33% gel) was approved by the United States Food and Drug Administration for the topical treatment of persistent facial erythema associated with rosacea. With its potent vasoconstrictive effects, brimonidine gel can lead to significant reduction of persistent facial erythema in the majority of patients when applied once a day.[9]
The differential diagnosis of rosacea largely depends on the pattern of rosacea. It includes systemic and discoid LE, acne vulgaris, seborrheic dermatitis, sarcoidosis, drug reactions, viral exanthema, and other systemic flushing disorders.[15]
The clinical similarity to LE might lead to misdiagnosis, particularly in patients with elevated ANA titers.[16] Elevated ANA titers are not infrequently found in patients with rosacea. Thus, less credence should be given to an elevated ANA titer when trying to distinguish LE from rosacea.[16] LE can be ruled out by clinical manifestations and laboratory tests. The patient in the present case was seronegative, and the histologic findings were not characteristic of LE.
In conclusion, rosacea can be an extremely severe and disfiguring condition, and it can be misdiagnosed as the pathognomonic butterfly rash of LE. Demodex carriage in rosacea is consistent and may play a significant role in its the severe forms.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given her consent for her images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.van Zuuren EJ, Gupta AK, Gover MD, Graber M, Hollis S. Systematic review of rosacea treatments. J Am Acad Dermatol. 2007;56:107–115. doi: 10.1016/j.jaad.2006.04.084. [DOI] [PubMed] [Google Scholar]
- 2.Tan J, Berg M. Rosacea: Current state of epidemiology. J Am Acad Dermatol. 2013;69(6 Suppl 1):S27–35. doi: 10.1016/j.jaad.2013.04.043. [DOI] [PubMed] [Google Scholar]
- 3.Salzer S, Ruzicka T, Schauber J. Face-to-face with anti-inflammatory therapy for rosacea. Exp Dermatol. 2014;23:379–381. doi: 10.1111/exd.12401. [DOI] [PubMed] [Google Scholar]
- 4.Dessinioti C, Antoniou C. Systemic Treatment of Rosacea. In: Zouboulis CC, Katsambas AD, Kligman AM, editors. Pathogenesis and Treatment of Acne and Rosacea. Springer Berlin Heidelberg: 2014. pp. 699–705. [Google Scholar]
- 5.Chosidow O, Cribier B. Epidemiology of rosacea: updated data. Ann Dermatol Venereol. 2011;138(Suppl 3):S179–183. doi: 10.1016/S0151-9638(11)70087-4. [DOI] [PubMed] [Google Scholar]
- 6.McAleer MA, Fitzpatrick P, Powell FC. Papulopustular rosacea: Prevalence and relationship to photodamage. J Am Acad Dermatol. 2010;63:33–39. doi: 10.1016/j.jaad.2009.04.024. [DOI] [PubMed] [Google Scholar]
- 7.El-Sherif NA, El-Dibany SA. Clinical evaluation of Libyan patients with rosacea and its correlation with seropositivity to Helicobacter pylori. Journal of Dermatology & Dermatologic Surgery. 2014;18:13–16. [Google Scholar]
- 8.Crawford GH, Pelle MT, James WD. Rosacea: I. Etiology, pathogenesis, and subtype classification. J Am Acad Dermatol. 2004;51:327–341. doi: 10.1016/j.jaad.2004.03.030. [DOI] [PubMed] [Google Scholar]
- 9.Johnson AW, Johnson SM. The Role of Topical Brimonidine Tartrate Gel as a Novel Therapeutic Option for Persistent FacialErythema Associated with Rosacea. Dermatol Ther (Heidelb) 2015;5:171–181. doi: 10.1007/s13555-015-0078-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilkin J, Dahl M, Detmar M, Drake L, Feinstein A, Odom R, et al. Standard classification of rosacea: Report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. J Am Acad Dermatol. 2002;46:584–587. doi: 10.1067/mjd.2002.120625. [DOI] [PubMed] [Google Scholar]
- 11.Steinhoff M, Buddenkotte J, Aubert J, Sulk M, Novak P, Schwab VD, et al., editors. Clinical, cellular, and molecular aspects in the pathophysiology of rosacea. Journal of Investigative Dermatology Symposium Proceedings; 2011: Nature Publishing Group. doi: 10.1038/jidsymp.2011.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cribier B. Rosacea under the microscope: Characteristic histological findings. J Eur Acad Dermatol Venereol. 2013;27:1336–1343. doi: 10.1111/jdv.12121. [DOI] [PubMed] [Google Scholar]
- 13.Oltz M, Check J. Rosacea and its ocular manifestations. Optometry. 2011;82:92–103. doi: 10.1016/j.optm.2010.01.015. [DOI] [PubMed] [Google Scholar]
- 14.Tüzün Y, Wolf R, Kutlubay Z, Karakuş O, Engin B. Rosacea and rhinophyma. Clin Dermatol. 2014;32:35–46. doi: 10.1016/j.clindermatol.2013.05.024. [DOI] [PubMed] [Google Scholar]
- 15.McDonnell JK, Tomecki KJ. Rosacea: An update. Cleve Clin J Med. 2000;67:587–590. doi: 10.3949/ccjm.67.8.587. [DOI] [PubMed] [Google Scholar]
- 16.Woźniacka A, Salamon M, McCauliffe D, Sysa-Jędrzejowska A. Antinuclear antibodies in rosacea patients. Advances in Dermatology and Allergology/Postȩpy Dermatologii I Alergologii. 2013;30:1–5. doi: 10.5114/pdia.2013.33372. [DOI] [PMC free article] [PubMed] [Google Scholar]


