Abstract
Purpose
Previous studies have compared weight-bearing mechanical leg axis (MLA) measurements to non-weight-bearing measurement modalities. Most of these studies compared mean or median values and did not analyse within-person differences between measurements. This study evaluates the within-person agreement of MLA measurements between weight-bearing full-length radiographs (FLR) and non-weight-bearing measurement modalities (computer-assisted surgery (CAS) navigation or MRI).
Materials and methods
Two independent observers measured the MLA on pre- and postoperative weight-bearing FLR in 168 patients. These measurements were compared to non-weight-bearing measurements obtained by CAS navigation or MRI. Absolute differences in individual subjects were calculated to determine the agreement between measurement modalities. Linear regression was used to evaluate the possibility that other independent variables impact the differences in measurements.
Results
A difference was found in preoperative measurements between FLR and CAS navigation (mean of 2.5° with limit of agreement (1.96 SD) of 6.4°), as well as between FLR and MRI measurements (mean of 2.4° with limit of agreement (1.96 SD) of 6.9°). Postoperatively, the mean difference between MLA measured on FLR compared to CAS navigation was 1.5° (limit of agreement (1.96 SD) of 4.6°). Linear regression analysis showed that weight-bearing MLA measurements vary significantly from non-weight-bearing MLA measurements. Differences were more severe in patients with mediolateral instability (p = 0.010), age (p = 0.049) and ≥3° varus or valgus alignment (p = 0.008).
Conclusion
The clinical importance of this study lies in the finding that there are within-person differences between weight-bearing and non-weight-bearing measurement modalities. This has implications for preoperative planning, performing total knee arthroplasty (TKA), and clinical follow-up after TKA surgery using CAS navigation or patient-specific instrumentation.
Level of evidence
III.
Keywords: Total knee arthroplasty, Frontal plane limb alignment, Limb mechanical axis, Navigation, Magnetic resonance imaging, Full-leg radiographs
Introduction
Accurate lower limb alignment in total knee arthroplasty (TKA) is important to improve clinical results and prosthesis survival [8, 18, 20]. Full-length weight-bearing anteroposterior radiographs (FLR) are regarded as the gold standard for determining knee joint alignment [19].
Other modalities that measure mechanical leg axis (MLA) include intra-operative computer navigation in computer-assisted surgery (CAS) and magnetic resonance imaging (MRI) in patient-specific instrumentation (PSI). Several studies have found differences between these measurement modalities [1, 6, 11, 13, 24, 28, 30–32]. However, most of these studies compared mean or median values of the measurement modalities and did not analyse within-person measurement differences. Comparing different measurements within individuals might be of greater value, as this shows the agreement between measurement modalities themselves. Neither correlation coefficients nor regression analysis are appropriate in the analysis of measurement method comparison data [2].
The discrepancy between measurement modalities may arise from a real difference in alignment between supine and weight-bearing status of the patient [5, 29]. In addition to weight-bearing conditions, previous literature has been inconsistent in which variables influence the differences between measurement modalities [7, 17, 26, 30, 32].
In this study, the authors evaluate the within-person agreement in MLA between weight-bearing measurements (FLR) and non-weight-bearing measurements (CAS navigation or MRI). In addition, independent variables that may contribute to measurement differences across modalities are examined.
Materials and methods
This dual-centre matched cohort study was performed in two neighbouring hospitals located in the same geographical area in the Netherlands (Maastricht University Medical Center (A) and Zuyderland Medical Center (B)). A total cohort of 168 patients were analysed.
Approval of the Zuyderland Institutional Review Board was obtained for this study (16-N-66).
Study group
Patients operated for total knee arthroplasty, who were able to undergo weight-bearing FLR, were included.
The CAS cohort consisted of 84 patients. All of whom had undergone TKA surgery by two experienced knee surgeons (PF and PE) at centre A, between 2010 and 2013). These patients were matched on age and gender to 84 patients from a consecutive cohort (n = 200) who were operated from 2009 to 2011 with PSI by one experienced knee surgeon (NK) in hospital B. The first 10 patients operated with PSI were excluded from matching, as they were considered to potentially influence the outcomes due to the surgeon’s learning curve. Therefore, the total cohort consisted of 168 patients. Demographic data were comparable in both groups (Table 1).
Table 1.
Demographic data
| Characteristic | Values CAS group (n = 84) Mean ± SD (range) or n (%) |
Values PSI group (n = 84) Mean ± SD (range) or n (%) |
|---|---|---|
| Gender | ||
| Male | 47 (56%) | 47 (56%) |
| Female | 37 (44%) | 37 (44%) |
| Age | 65.8 ± 8.1 (42.6–79.3) | 64.3 ± 7.3 (48.3–77.5) |
| Side | ||
| Right | 52 (61.9%) | 52 (61.9%) |
| Left | 32 (38.1%) | 32 (38.1%) |
| Weight (kg) | 84.6 ± 13.9 (55–119) | 87.9 ± 13.3 (63–116) |
| Height (cm) | 171.3 ± 8.1 (155–190) | 171.8 ± 8.8 (150–189) |
| Body mass index (BMI) (kg/m2) | 28.7 ± 3.3 (20.6–34.8) | 29.9 ± 4.5 (21.8–45.0) |
From five patients in the CAS group, the preoperative navigation measurements were not documented. Moreover, the proximal part of the preoperative FLR of one patient in the PSI group was missing; thus, the MLA could not be measured. From one patient in the CAS group, the postoperative CAS navigation measurements were not documented due to an intra-operative malfunctioning of the CAS navigation software. Therefore, in total six patients were excluded from preoperative analysis and one patient from the postoperative analysis.
Imaging technique
Operations with CAS navigation were performed with an identical surgical technique using a Stryker knee navigation system (Stryker Precision Knee Navigation Software, Stryker Corp. Kalamazoo, Michigan USA). According to the manufacturer’s protocol, specific landmarks of the lower limb were digitized using a navigation pointer, with which the preoperative MLA was measured (non-weight bearing). After implanting the definitive prosthesis components, the postoperative MLA was measured again (non-weight bearing).
Before PSI surgery, all patients underwent an MRI scan of the lower limb following the protocol of the manufacturer. This MRI scan was used to create personalized positioning guides for aligning the TKA. The preoperative MLA was measured with software (Signature Personalized Patient Care Biomet, Warsaw, IN, USA) on non-weight-bearing MRI scan.
Radiographic analysis
All patients underwent weight-bearing FLR preoperatively. These measurements were then compared to the preoperative measurements obtained by either CAS navigation or MRI. In the CAS group, postoperative FLR (12 weeks postoperatively) were also compared to the CAS navigation measurements after insertion of the total knee prosthesis. Absolute differences between measurement modalities were calculated and analysed.
For FLR, protocols were identical in both centres. All patients were bare-footed and instructed to stand upright with heels and toes touching the ground. Lower limbs were fully extended and the patella directed anteriorly. A digital ruler was projected onto the images, and three radiographs were taken. These individual radiographs were automatically merged using the digital ruler. MLA was determined using the method described by Moreland et al. [22], which is the angle formed by the intersection of a line from the centre of the femoral head to the centre of the knee and a second line from the centre of the knee to the centre of the ankle. On postoperative FLR, the centres of the femoral and tibial prosthesis components were used instead of the bony landmarks of the knee.
Measurements in the CAS group were determined in whole numbers with the iSite Enterprise software (Philips Healthcare, Foster City, California, USA). In the PSI group, measurements were determined to within 0.1° with Pacs software (Siemens Healthcare, Munich, Federal Republic of Germany) and rounded to the nearest whole number.
In order to ensure the reliability of the FLR measurements, all FLR were analysed by two independent observers in each group (DS and PF in the CAS group, and DS and BB in the PSI group). The observers were blinded for each other’s measurements as well as the measurements performed with CAS navigation or MRI. For intra-observer reliability analysis, the same researcher measured 10 pre- and 10 postoperative FLR in the CAS group and 10 preoperative FLR in the PSI group. This was done six weeks after the initial measurements were taken.
Statistical analysis
Statistical analysis was performed using SPSS software (SPSS 21 Inc., Chicago, IL, USA).
Intra- and inter-observer reliability of radiographic MLA measurements was determined by intra-class correlation coefficients (ICCs) using a two-way random effects model for an absolute agreement definition.
To determine the agreement between measurement modalities (FLR and CAS navigation or MRI), absolute differences in individual persons were evaluated. The absolute differences between the two modalities were plotted against the average of these two measurements. The limits of agreement were used to measure the agreement between the variables and estimate the range in which 95% of the differences lie [2].
Linear regression was used to evaluate independent variables (degree of alignment deformity, body mass index (BMI), mediolateral stability during physical examination, gender, and age) that could potentially affect the differences in measurements. Statistical significance was set at p ≤ 0.05.
Results
Inter- and intra-observer reliability of radiographic measurements
All measurements of MLA on FLR demonstrated high precision with ICCs for both intra- and inter-observer reliability within a range of 0.942 and 0.989.
Agreement between measurement modalities
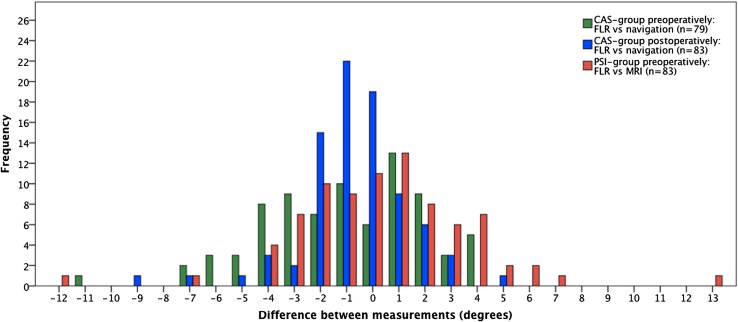
MLA measured on FLR versus measurements by CAS navigation showed differences >3° in 27.9% of the patients preoperatively and in 8.4% of patients postoperatively. MLA on preoperative FLR compared to preoperative measurements obtained by MRI showed differences >3° in 22.9% of the persons. There was a difference of ≥5° in nine patients in the CAS group and in eight patients in the PSI group. In five patients from the total cohort, a difference between 7° and 13° was observed (Fig. 1).
Fig. 1.
Frequency of differences in individual measurements of MLA for different measurement modalities. Difference represents the value measured on FLR minus the value measured by CAS navigation or MRI. MLA mechanical leg axis, CAS computer-assisted surgery, PSI patient specific instrumentation, FLR full-length radiograph, MRI magnetic resonance imaging
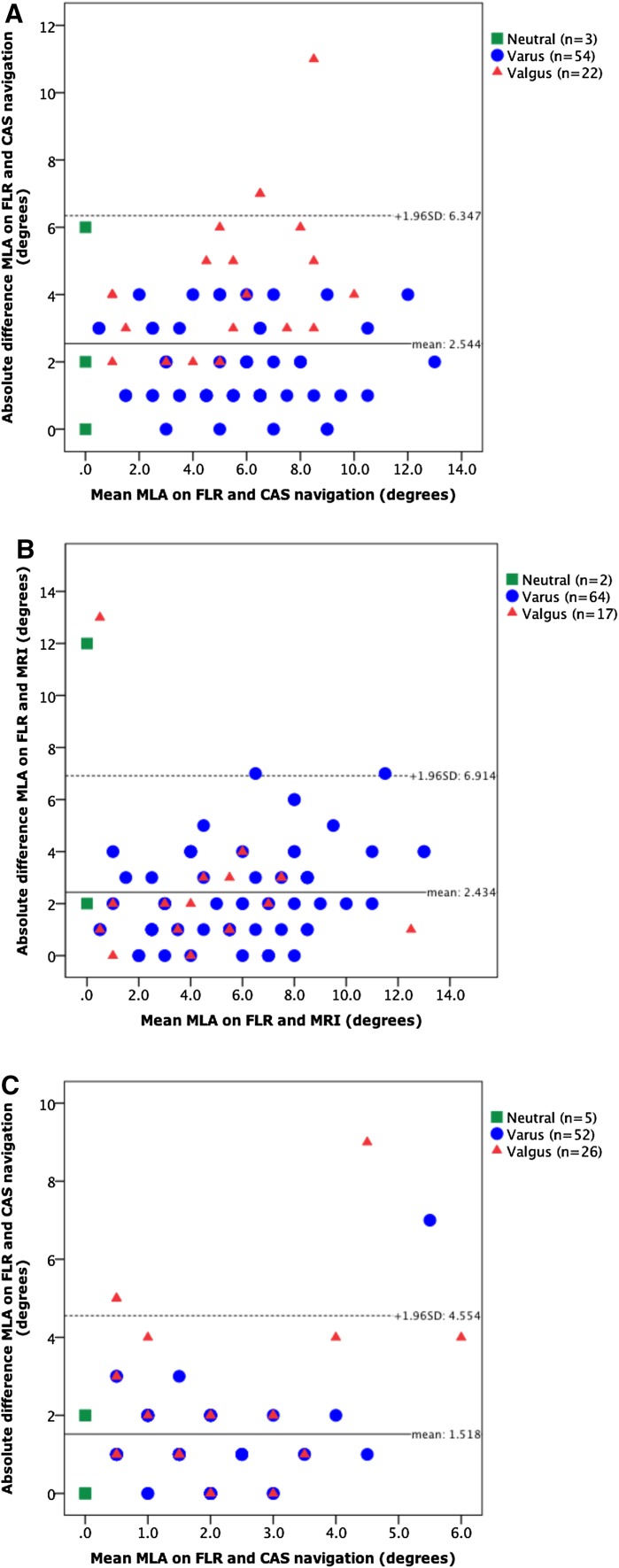
When analysing the plots based on the Bland–Altman method [2], one can observe that CAS navigation and MRI measurements differ from FLR with mean values of 2.5° and 2.4°, respectively. Postoperatively, the mean difference between MLA measured on FLR compared to CAS navigation was 1.5°. When comparing FLR with CAS navigation or MRI, the limits of agreement (1.96 SD) showed values of up to 6.4° and 6.9°, respectively, for preoperative values and 4.6° for postoperative comparison of FLR to CAS navigation (Fig. 2).
Fig. 2.
Plots with agreement of MLA measurements. Solid black lines give the mean difference in measurements and the dotted lines give the limit of agreement (mean difference ±1.96 × SD of the differences). MLA mechanical leg axis, FLR full-length radiograph, CAS computer-assisted surgery, MRI magnetic resonance imaging. a MLA on FLR versus CAS navigation preoperatively. b MLA on FLR versus MRI preoperatively. c MLA on FLR versus CAS navigation post-operatively
Factors influencing differences in measurement of MLA
Multiple linear regression analysis revealed low coefficients of determination in the CAS group (R 2 of 0.132 preoperatively and 0.122 postoperatively). Differences between measurements on FLR and CAS navigation were significantly higher in preoperative measurements when mediolateral instability (during physical examination) was present (p = 0.010) as well as with increasing age (p = 0.049). For postoperative measurements, differences became significantly higher when the MLA deviated ≥3° from neutral MLA (p = 0.008).
Regression analysis showed no significant differences (n.s.) between measurements of FLR and MRI for any of the independent variables entered in the analysis.
Discussion
The most important finding of the present study was that within-person MLA measurements were found to be different when comparing weight-bearing FLR to non-weight-bearing measurement modalities (CAS navigation or MRI).
This study shows high ICC, which is in line with previous literature (intra-observer reliability ICC range 0.91–1.00 [4, 30], inter-observer reliability ICC range 0.72–0.99 [4, 30]).
The discrepancy between measurement modalities may arise from a real difference in alignment between supine and the weight-bearing status of the patient, which has been recognized in prior research. Weight-bearing radiographs can differ up to 2.0° from radiographs in supine position [5, 29]. Willcox et al. [30] assessed the agreement between FLR and CAS navigation measurements of MLA and showed wider limits of agreement of −9.4° and 8.6° preoperatively and −5.0° to 5.4° postoperatively. This is line with the findings of the current work.
Winter et al. [31] assessed the relationship between preoperative FLR and MRI measurements of MLA and showed a correlation between the two techniques (Pearson’s correlation coefficient (r) = 0.88) and a large absolute variability in measurements in the same patient, with differences up to 8°. As previously noticed, correlation does not equate to agreement [2]. Based on the absolute differences described by Winter et al. [31], a mean difference of 2.6° could be calculated from their data, which is similar to the mean difference found in the present study (2.4°). Paternostre et al. [24] also assessed the differences in MLA measurements between FLR and MRI and found no significant difference (evaluation by Student’s t test). They found differences >3° in 23% of patients, which was similar to the current study (differences higher than 3° in 22.9% of the persons). Moreover, they stated that the difference seems to be related to higher Kellgren–Lawrence stages where deformity increased under load-bearing conditions.
In the present study, it was found that discrepancies were higher in preoperative measurements compared to postoperative measurements. Other authors have also concluded that preoperative measurements involve a higher degree of ligamentous imbalance, which may lead to greater alignment deformity while weight-bearing [23]. Knees are balanced after TKA, and therefore, the postoperative difference between weight-bearing and non-weight-bearing gets smaller [23].
In five patients, an outlying difference between 7° and 13° was observed. This could be the result of several factors such as fixed flexion deformity, incorrect placement or loosening of navigation trackers, ligamentous imbalance, and measurement or administration errors. The complete analysis was repeated without these five outliers. The results from this analysis did not differ from our previous results including outliers. Only the mean difference decreased marginally within a range of 0.1°–0.3°, as expected.
It has been noted in previous literature that the risk of inaccuracy of MLA is more likely in the presence of flexion of the knee or rotation of the leg [17, 26]. Measurements of MLA with CAS navigation or with MRI are independent from rotation or flexion since they are three-dimensional. Previous studies demonstrated that CAS navigation measurements are precise [12, 33]. The system-determined error has been described within 1° in the coronal plane [10, 25, 33]. Nonetheless, there is a potential for error since the registration process of CAS navigation is subject to inter- or intra-surgeon variations when demarcating correct landmark registration, or potential loosening of the tracker [27, 33]. For PSI, measurements are also subject to movements of the patient during scanning in MRI.
Previous literature is non-concurrent on indicating independent factors that influence MLA measurements [6, 7, 24, 28, 30–32]. In addition to weight-bearing status, variable factors may influence the measurements resulting in increased discrepancy. Our findings show that mediolateral instability and age had a significant influence on the differences between preoperative FLR and CAS navigation measurements. A ≥3° alignment deformity from neutral MLA resulted in significantly higher differences in postoperative CAS group measurements. However, these differences were only of very small clinical relevance with R 2 ranging from 0.122 to 0.284.
The present study contains some limitations. The aforementioned potential errors were not investigated in either the CAS navigation’s registration process or the MRI scan. A further shortcoming of this study is the lacking determination of flexion and rotation data. As a result, they could not be analysed as confounding variables. Another limitation of the present study results from the fact that two patient samples were used. Obtaining all three modalities (FLR, CAS navigation, and MRI) in the same patient sample would be desirable to reduce bias. Finally, other measurement modalities (e.g. computed tomography (CT), single-photon emission computed tomography (SPECT/CT) or 3D reconstructions using SterEOS software) have been evaluated in previous literature [3, 9, 14–16, 21], but were not included in the present study. Comparison of more measurement modalities in individual persons might be of added value in future research.
Conclusion
The clinical importance of this study lies in the finding that differences were observed in within-person MLA measurements. A mean difference of up to 2.5° between weight-bearing and non-weight-bearing MLA measurements has implications for preoperative planning, performing TKA, and clinical follow-up after TKA surgery using CAS navigation or PSI.
Acknowledgments
The authors wish to thank Dr. B. Winkens (Department of Methodology and Statistics, University of Maastricht) for his advice on the appropriate statistical methods used in this study.
Compliance with Ethical Standards
Conflict of interest
NP Kort is a consultant for Zimmer-Biomet. The other authors declare that they have no conflicts of interest.
Funding
No funding was received for this study.
Ethical approval
For this type of study formal consent is not required.
Informed consent
For this type of study informed consent is not required.
References
- 1.Babazadeh S, Dowsey MM, Bingham RJ, Ek ET, Stoney JD, Choong PF. The long leg radiograph is a reliable method of assessing alignment when compared to computer-assisted navigation and computer tomography. Knee. 2013;20(4):242–249. doi: 10.1016/j.knee.2012.07.009. [DOI] [PubMed] [Google Scholar]
- 2.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. doi: 10.1016/S0140-6736(86)90837-8. [DOI] [PubMed] [Google Scholar]
- 3.Boonen B, Kerens B, Schotanus MG, Emans P, Jong B, Kort NP. Inter-observer reliability of measurements performed on digital long-leg standing radiographs and assessment of validity compared to 3D CT-scan. Knee. 2016;23(1):20–24. doi: 10.1016/j.knee.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 4.Bowman A, Shunmugam M, Watts AR, Bramwell DC, Wilson C, Krishnan J. Inter-observer and intra-observer reliability of mechanical axis alignment before and after total knee arthroplasty using long leg radiographs. Knee. 2016;23(2):203–208. doi: 10.1016/j.knee.2015.11.013. [DOI] [PubMed] [Google Scholar]
- 5.Brouwer RW, Jakma TS, Bierma-Zeinstra SM, Ginai AZ, Verhaar JA. The whole leg radiograph: standing versus supine for determining axial alignment. Acta Orthop Scand. 2003;74(5):565–568. doi: 10.1080/00016470310017965. [DOI] [PubMed] [Google Scholar]
- 6.Choi WC, Lee S, An JH, Kim D, Seong SC, Lee MC. Plain radiograph fails to reflect the alignment and advantages of navigation in total knee arthroplasty. J Arthroplasty. 2011;26(5):756–764. doi: 10.1016/j.arth.2010.07.020. [DOI] [PubMed] [Google Scholar]
- 7.Dexel J, Kirschner S, Gunther KP, Lutzner J. Agreement between radiological and computer navigation measurement of lower limb alignment. Knee Surg Sports Traumatol Arthrosc. 2014;22(11):2721–2727. doi: 10.1007/s00167-013-2599-4. [DOI] [PubMed] [Google Scholar]
- 8.Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty. 2009;24(6):39–43. doi: 10.1016/j.arth.2009.04.034. [DOI] [PubMed] [Google Scholar]
- 9.Gbejuade HO, White P, Hassaballa M, Porteous AJ, Robinson JR, Murray JR. Do long leg supine CT scanograms correlate with weight-bearing full-length radiographs to measure lower limb coronal alignment? Knee. 2014;21(2):549–552. doi: 10.1016/j.knee.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 10.Graydon AJ, Malak S, Anderson IA, Pitto RP. Evaluation of accuracy of an electromagnetic computer-assisted navigation system in total knee arthroplasty. Int Orthop. 2009;33(4):975–979. doi: 10.1007/s00264-008-0586-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hauschild O, Konstantinidis L, Baumann T, Niemeyer P, Suedkamp NP, Helwig P. Correlation of radiographic and navigated measurements of TKA limb alignment: a matter of time? Knee Surg Sports Traumatol Arthrosc. 2010;18(10):1317–1322. doi: 10.1007/s00167-010-1144-y. [DOI] [PubMed] [Google Scholar]
- 12.Hauschild O, Konstantinidis L, Strohm PC, Niemeyer P, Suedkamp NP, Helwig P. Reliability of leg alignment using the OrthoPilot system depends on knee position: a cadaveric study. Knee Surg Sports Traumatol Arthrosc. 2009;17(10):1143–1151. doi: 10.1007/s00167-009-0825-x. [DOI] [PubMed] [Google Scholar]
- 13.Hinterwimmer S, Graichen H, Vogl TJ, Abolmaali N. An MRI-based technique for assessment of lower extremity deformities—reproducibility, accuracy, and clinical application. Eur Radiol. 2008;18(7):1497–1505. doi: 10.1007/s00330-008-0896-y. [DOI] [PubMed] [Google Scholar]
- 14.Hirschmann MT, Konala P, Amsler F, Iranpour F, Friederich NF, Cobb JP. The position and orientation of total knee replacement components: a comparison of conventional radiographs, transverse 2D-CT slices and 3D-CT reconstruction. J Bone Joint Surg Br. 2011;93(5):629–633. doi: 10.1302/0301-620X.93B5.25893. [DOI] [PubMed] [Google Scholar]
- 15.Holme TJ, Henckel J, Hartshorn K, Cobb JP, Hart AJ. Computed tomography scanogram compared to long leg radiograph for determining axial knee alignment. Acta Orthop. 2015;86(4):440–443. doi: 10.3109/17453674.2014.1003488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huellner MW, Strobel K. Clinical applications of SPECT/CT in imaging the extremities. Eur J Nucl Med Mol Imaging. 2014;41(1):S50–S58. doi: 10.1007/s00259-013-2533-5. [DOI] [PubMed] [Google Scholar]
- 17.Kannan A, Hawdon G, McMahon SJ. Effect of flexion and rotation on measures of coronal alignment after TKA. J Knee Surg. 2012;25(5):407–410. doi: 10.1055/s-0032-1313756. [DOI] [PubMed] [Google Scholar]
- 18.Kim YH, Park JW, Kim JS, Park SD. The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop. 2014;38(2):379–385. doi: 10.1007/s00264-013-2097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Langenbach MR, Dohle J, Zirngibl H. Determination of the axis after totalendoprosthesis of the knee: functional X-ray photography as golden standard. Z Orthop Ihre Grenzgeb. 2002;140(1):32–36. doi: 10.1055/s-2002-22088. [DOI] [PubMed] [Google Scholar]
- 20.Lotke PA, Ecker ML. Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg Am. 1977;59(1):77–79. doi: 10.2106/00004623-197759010-00013. [DOI] [PubMed] [Google Scholar]
- 21.Meijer MF, Boerboom AL, Bulstra SK, Reininga IH, Stevens M. Do CAS measurements correlate with EOS 3D alignment measurements in primary TKA? Knee Surg Sports Traumatol Arthrosc. 2016 doi: 10.1007/s00167-016-4031-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69-A(5):745–749. doi: 10.2106/00004623-198769050-00016. [DOI] [PubMed] [Google Scholar]
- 23.Panzica M, Kenawey M, Liodakis E, Brandes J, Krettek C, Hankemeier S. Effect of intraoperative weight-bearing simulation on the mechanical axis in total knee arthroplasty. Arch Orthop Trauma Surg. 2014;134(5):673–677. doi: 10.1007/s00402-014-1938-3. [DOI] [PubMed] [Google Scholar]
- 24.Paternostre F, Schwab PE, Thienpont E. The difference between weight-bearing and non-weight-bearing alignment in patient-specific instrumentation planning. Knee Surg Sports Traumatol Arthrosc. 2014;22(3):674–679. doi: 10.1007/s00167-013-2687-5. [DOI] [PubMed] [Google Scholar]
- 25.Pitto RP, Graydon AJ, Bradley L, Malak SF, Walker CG, Anderson IA. Accuracy of a computer-assisted navigation system for total knee replacement. J Bone Joint Surg Br. 2006;88-B(5):601–605. doi: 10.1302/0301-620X.88B5.17431. [DOI] [PubMed] [Google Scholar]
- 26.Radtke K, Becher C, Noll Y, Ostermeier S. Effect of limb rotation on radiographic alignment in total knee arthroplasties. Arch Orthop Trauma Surg. 2010;130(4):451–457. doi: 10.1007/s00402-009-0999-1. [DOI] [PubMed] [Google Scholar]
- 27.Robinson M, Eckhoff DG, Reinig KD, Bagur MM, Bach JM. Variability of landmark identification in total knee arthroplasty. Clin Orthop Relat Res. 2006;442:57–62. doi: 10.1097/01.blo.0000197081.72341.4b. [DOI] [PubMed] [Google Scholar]
- 28.Seo SS, Seo JH, Sohn MW, Kim YJ. Differences in measurement of lower limb alignment among different registration methods of navigation and radiographs in TKA using the OrthoPilot system. Orthopedics. 2012;35(10):50–55. doi: 10.3928/01477447-20120919-58. [DOI] [PubMed] [Google Scholar]
- 29.Specogna AV, Birmingham TB, Hunt MA, Jones IC, Jenkyn TR, Fowler PJ, Giffin JR. Radiographic measures of knee alignment in patients with varus gonarthrosis: effect of weightbearing status and associations with dynamic joint load. Am J Sports Med. 2007;35(1):65–70. doi: 10.1177/0363546506293024. [DOI] [PubMed] [Google Scholar]
- 30.Willcox NM, Clarke JV, Smith BR, Deakin AH, Deep K. A comparison of radiological and computer navigation measurements of lower limb coronal alignment before and after total knee replacement. J Bone Joint Surg Br. 2012;94(9):1234–1240. doi: 10.1302/0301-620X.94B9.28250. [DOI] [PubMed] [Google Scholar]
- 31.Winter A, Ferguson K, Syme B, McMillan J, Holt G. Pre-operative analysis of lower limb coronal alignment—a comparison of supine MRI versus standing full-length alignment radiographs. Knee. 2014;21(6):1084–1087. doi: 10.1016/j.knee.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 32.Yaffe MA, Koo SS, Stulberg SD. Radiographic and navigation measurements of TKA limb alignment do not correlate. Clin Orthop Relat Res. 2008;466(11):2736–2744. doi: 10.1007/s11999-008-0427-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yau WP, Leung A, Liu KG, Yan CH, Wong LL, Chiu KY. Interobserver and intra-observer errors in obtaining visually selected anatomical landmarks during registration process in non-image-based navigation-assisted total knee arthroplasty. J Arthroplasty. 2007;22(8):1150–1161. doi: 10.1016/j.arth.2006.10.010. [DOI] [PubMed] [Google Scholar]