Abstract
Purpose
Despite the high incidence of falls in patients with OA, few studies have explored whether falls risk is affected after patients undergo total knee arthroplasty (TKA). Therefore, the aim of this systematic review was to identify the extent of the effects of TKA on balance and incidence of falls by critically reviewing the available literature.
Methods
A systematic review of published literature sources was conducted up to March 2014. All studies assessing balance and incidence of falls after TKA (without physiotherapeutic intervention) were included. The methodological quality of each study was reviewed using the Critical Appraisal Skill Programme tool.
Results
Thirteen studies were included, comprising of ten cohort studies (Level II) and three studies with Level of evidence III.
Conclusions
Findings provide evidence that TKA improves significantly single-limb standing balance (~60%) and dynamic balance up to 1-year following surgery (Level of evidence II). Moreover, TKA influences positively fear of falling and incidence of falls by switching 54.2 % of pre-operative fallers to post-operative non-fallers (Level of evidence II–III). It is highlighted that knee extension strength, proprioception and symmetrization of postural strategies have not fully recovered post-TKA and influence balance performance. Clinically, these persistent deficits need to be mitigated by physiotherapy even before TKA takes place.
Keywords: Balance control, Falls, Falls risk, Total knee arthroplasty, Systematic review
Introduction
Balance is essential for maintaining postural stability while performing functional activities and for fall avoidance [48]. Balance (dynamic and static) is a complex function which requires integration of sensory information regarding the position of the body and the ability to make appropriate motor response to body movement [22]. More precisely, it depends on sensory inputs from somato-sensory (proprioception), visual and vestibular systems [5], as well as, response of muscles. Static balance refers to maintaining equilibrium while standing in one spot, whereas dynamic balance involves motion and is defined as maintaining equilibrium during locomotion [37]. Falls and loss of balance most commonly occur during movement-related tasks such as walking and less frequently during static activities [23].
Balance deficits have been identified as one of the integral components impairing daily living in patients with knee osteoarthritis (OA) and are associated with an increased risk of falls and poor mobility [59]. Approximately 60–80 % of patients with knee OA report knee instability, which causes activity limitations [14, 44]. Osteoarthritis has been shown to be an important risk factor for falls with more than 40 % of all patients and 64 % of female patients, with OA reporting falls within a year in America [18, 59]. Potential mechanisms causing balance impairments in this population have not yet been fully elucidated [13, 25, 39, 50, 51]. Age-related impairments in the capacities of physiological systems controlling balance is one of the potential contributory mechanisms [47]. Proprioceptive impairment of the joint sometimes precedes knee OA and deteriorates further the degeneration associated with the disease [46]. Knee pain and quadriceps’ weakness are associated with increased postural sway [8, 20, 27, 30]. However, while total knee arthroplasty (TKA) (treatment of choice for end-stage OA) aims to relieve pain, correct deformities and restore loco-motor function, it is not established whether it has an effect on patients’ balance and incidence of falls. The literature suggests that patients with knee OA undergoing TKA will often present with a substantial loss of balance control and proprioceptive acuity that is frequently precipitated by a lack of confidence [13, 25, 28, 31, 34, 35, 39, 42, 51]. Despite the high incidence of falls in this population, there is a scarcity of investigations in the literature focusing on the risk of falls and subsequent impairments in function for patients with knee OA after undergoing TKA.
Chronic knee OA pain is reduced after TKA, but little is known about the recovery of proprioceptors, neuromuscular control, joint-related stability and also about each aspect’s natural recovery after surgery. Conversely, asymmetrical gait patterns and postural sway (in the coronal plane) combined with increased forward trunk movement (in the sagittal plane), observed especially in the early post-operative period, cause balance difficulties and increased risk of falls [10, 19, 24].
Residual physical deficits have been observed up to 7-year following TKA, with significant impact on functional status (i.e. postural stability, walking speed, stair ascent/descent) [6, 17, 36, 41, 55, 56, 60, 61]. In turn, decreased muscle strength, ROM and altered movement patterns evident post-surgery affect the sensory and mechanical function of the joint. Byrne & Prentice [7] reported that TKA affects the ability of patients to step over an obstacle.
Thus, there are a number of factors that may influence the effect of TKA on balance and consequently the incidence of falls. Understanding of the mechanisms associated with the recovery of the systems that control balance and the specific residual problems after surgery may ultimately help to enhance the design of rehabilitation programmes using approaches that are justified by scientific evidence. Based on this rationale, the novel aim of this study was to conduct a systematic review in order to identify the effects of TKA on balance and on the incidence/ risk of falls.
Materials and methods
The electronic databases: the Cochrane Central Register of Controlled Trials (Cochrane Library), MEDLINE, EMBASE (via ProQuest), Biomed Central, CINAHL (via EBSCO host) and Physiotherapy Evidence Database (PEDro) were searched from January 1995 to the present (September 2014). The MEDLINE Mesh keywords used were: Balance OR stability OR postural control OR falls AND knee replacement OR knee arthroplasty in the title or abstract or keywords of the studies. Clinical trials published in the English language were included. The reference lists of all eligible papers were also screened to identify any studies that had been missing from the databases. The format of the search terms was modified appropriately for use in each database searched.
Eligibility assessment was performed independently in a standardized manner, and disagreements amongst reviewers were resolved by consensus. Therefore, studies were included if they fulfilled the following 4 criteria:
Participants underwent primary TKA.
No physiotherapeutic intervention/rehabilitation was involved after hospital discharge for TKA.
Balance, postural control and/or falls incidence was/were used as outcome measure/s.
The full paper was published in the English language.
Studies included cross-sectional, cohort and randomized controlled trials (RCTs), but excluded case studies. All cadaver or animal studies were excluded. Moreover, studies with samples involving patients with rheumatoid arthritis (RA) were excluded.
Two evaluators independently selected the studies based on titles and abstracts and excluded those not related to the subject. The full text was obtained for all papers that were considered potentially relevant. Once collected, these were reviewed by both reviewers to determine whether eligibility criteria had been fulfilled. The studies finally included were analysed according to a certain structure: author/year, sample, study design, assessment outcome measures, timeline, physiotherapy treatment, equipment and effects. The selection criteria were applied to the title and to the abstract of all articles retrieved in the search of the literature. The full text articles not excluded in the initial selection process were then evaluated for inclusion using the same eligibility criteria.
The methodological quality of each study was evaluated according to the Critical Appraisal Skills Programme (CASP) tool. This appraisal tool has been widely used in systematic reviews and is recognized to be a valid tool. The tool uses a set of 11 questions to evaluate domains such as: study design, appropriateness of design, randomization method, blinding, accuracy in the description of the sample recruitment, treatment effects, finding’ interpretation.
In the first stage, a descriptive review of studies assessing balance and falls incidence in patients after knee replacement was undertaken (Table 1).
Table 1.
Description of the included studies in the systematic review investigating balance and risk of falls in TKR patients
| Sample | Outcome measures | Timeline | Study findings | Clinically relevant findings to balance and falls | |
|---|---|---|---|---|---|
| Cho and Hwang [12] | N = 11 (11F) No CG Age: 61.7±7.3 Inclusion: Radiographic varus deformity& medial compartment OA degeneration undergoing TKR | VAS; WOMAC; varus angle; SLSB in horizontal plane force platform maximum isometric peak torque of quadriceps | Pre-TKR and 11-day post-TKR | Improvements (~60%) in SLSB in patients with varus OA knees 11-day post-TKR | Improvement in SLSB post-TKR |
| Poor pre-TKR SLSB associated with better SLSB post-TKR. | |||||
| Gage et al. [15] | EG: n= 8(2 M,6F) Age: 62.9±6.0 CG: n=9(5 M,4F) Age: 62.1±5.6 Inclusion: post-TKR patients, first right TKR, at least 6 months after surgery | EMG and kinematic responses with rotational sagittal plane perturbation platform | At least 6 months post-TKR | Dynamic balance not impaired in EG vs CG in sagittal plane | No difference between groups in dynamic balance in sagittal plane |
| Whole body COM displacement not different between groups vs joint angle displacement and EMG => different strategy to maintain balance from CG. | |||||
| EMG and kinematic responses in EG are bilateral despite unilateral joint disease | |||||
| Gage et al. [16] | EG: n = 8(6F) Age: 62.9±6.0. CG: n=9(4F) Age: 62.1±5.6 Inclusion: post-TKR patients, first right TKR, at least 6 months after surgery | EMG and kinematic responses with rotational frontal plane perturbation platform | At least 6-month post-TKR | Dynamic balance control impaired in EG vs CG in frontal plane | Impaired dynamic balance of EG vs CG in frontal plane |
| Increased COM displacement in EG vs CG | |||||
| Differences in joint angle displacement and EMG of EG vs CG => different strategy to maintain balance from CG. | |||||
| EMG and kinematic responses amongst patients are bilateral despite unilateral joint disease | |||||
| Levinger et al. [29] | EG: n = 35 (16F) Age: 67±7. CG: n=27 (14F) Age: 65±11 Inclusion: patients with knee OA who could walk independently for 45 m undergoing TKR | QoL; WOMAC; Incidental and Planned Activity Questionnaire (IPAQ), Falls Efficacy Scale (FES-I), Physiological Profile Assessment (PPA) for falls risk | Pre-TKR & 4-month post-TKR | No significant difference in falls risk between groups post-TKR | Increased risk of falls in EG compared to CG. |
| No significant difference in postural sway between groups | Impaired SLSB of EG vs CG | ||||
| QoL: significant reduced post-surgery. | |||||
| Significant improvement in WOMAC post-TKR | |||||
| Less strength and poorer proprioception for the EG post-TKR compared with the CG | |||||
| Mandeville et al. [32] | EG: n= 19(14F) Age: 64.0±7.74. CG: n=21(13F) Age: 63.1±4.26 Inclusion: end-stage OA undergoing TKR | VAS; WOMAC; obstacle overcoming; kinematic displacement on force platform during gait | Within 2 pre-TKR weeks and 6-month post-TKR | Improvement in WOMAC post-surgery | Impaired dynamic balance in EG vs controls |
| Poorer gait stability in EG (smaller displacement COM/COG) than CG | |||||
| EG and CG cross obstacles similarly | |||||
| Mauer et al. [33] | EG: n=29(19F) Age 72, 6±5,4, bilateral (BL) TKR. CG: n=27(17F) Age 70, 6±5,5. Inclusion: knee OA who could climb stairs, rise form a chair, have 20/40 vision or better undergoing TKR | Balance (SLSB for 30 s); Obstacle avoidance success rate | EG tested post-TKR: 2,75±1,29 (range: 1–5 years) | EG SLSB duration was 67% less than the CG | Impaired SLSB in EG vs CG. |
| EG 30% less obstacle avoidance success rate than the CG | Increased risk of falls in EG vs CG | ||||
| McChesney and Woolacot [11] | N=22 Age:≥70 Groups: knee OA, ankle OA, patients undergoing TKR | TJPS; EMG and kinematic responses with force platform | Not stated | Ankle & knee groups with lower TJPS showed increased COP variance. | No difference on SLSB or dynamic between groups |
| Post-TKR patients showed no reductions in any aspect of postural control. | |||||
| Quagliarella et al. [43] | N=240(142F). EG1: n=81 THR Age range: 40–80/42–82 years EG2: n=100 TKR Age range: 48–80/48–79 years CG: N=59 Age 67.4±5,9. Patients able to stand without support for 120 s. | Posturography on force plate | Pre-op; 6 months &12 months post-TKR | No statistically significant improvement in posturographic parameters in EG1 & EG2 vs CG group at follow-ups post-TKR | Standing balance did not show a clear trend towards improvement in TKR patients post-TKR |
| Statistically significant improvement in pain and function of EG1 & EG2 post-TKR | |||||
| Posturography not recommended as a method to evaluate balance in TKR patients | |||||
| Schwartz et al. [45] | n=62(52F) mAge: 73 (r: 57–83). Inclusion: Knee OA patients able to walk & follow simple instructions undergoing TKR | Dynamic & static Balance with force platform; TUG; SF-36 | Pre-TKR & 12-month post-TKR | improved knee function& QoL | Significant improvement in dynamic and functional balance; NS for static balance |
| improved dynamic balance | |||||
| Improvements in static balance measures did not reach statistical significance. | |||||
| Improved weight-bearing during squat | |||||
| Swinkels et al. [54] | n= 99(63F) Age 73.4±4.9 Inclusion: primary TKR | falls number; WOMAC; ABC-UK; GDS | Pre-TKR and 12-month post-TKR | ~45% patients fall again in the first year post-TKR | Significant switch of pre-TKR fallers becoming non-fallers post-TKR |
| Improved balance confidence, WOMAC and GDS post-TKR | |||||
| Swinkels and Allain [53] | n=22 (16F/ Age: 74,8 ± 5,2y) Inclusion: primary TKR. | falls number; WOMAC, ABC, GDS; BBS; TUG | 2–50 day pre-TKR (mean: 23) 143–218 day post-TKR (mean: 183) | 41% of patients exceeded MDC for BBS post-surgery | Functional balance improved post-TKR in 54% of patients |
| 50 % of patients exceeded MDC for TUG post-surgery | |||||
| Findings on fallers are restricted by the small sample size | |||||
| Viton et al. [57] | 20 patients EG1: N=8(3F) Age: 67 (46–77) CG N=12(6F) Inclusion: Unilateral TKR | VAS; kinetics/kinematics in side step on force platform | 15-day pre -and 12-month post-TKR | Improved VAS | SLSB improved in operated limb during tasks |
| Presented with more symmetrical posturomotor strategies | |||||
| Evidence of persisting posturomotor impairments of EG vs CG | |||||
| Increased SLSB in operated limb in EG | |||||
| Yakhdani et al. [60] | EG1: n = 14(10F) Age 61.6±10. CG: n=12(7F) Age 62.0±12.6 Inclusion: Unilateral knee ΟΑ undergoing TKR, sufficient physical condition | Dynamic balance; falls; gait variability | pre-TKR, at 6 weeks, at 6- and 12-month post-TKR | EG1: increased maximum gait speed post-TKR | Reduced risk of falls. |
| Decreased gait variability of EG post-TKR in relevance to CG | Recovery of dynamic balance | ||||
| Increased stability post-TKR |
CG control group, EG experimental group, TKR total knee replacement, mCTSIB modified clinical test for sensory interaction and balance, TJPS threshold of passive joint position sense, ABC-UK activity balance confidence scale, GDS geriatric depression scale, BBS berg balance scale, MDC minimal detectable change, COP centre of pressure, COG centre of gravity, TUG timed up and go test, NS non significant
In the next stage, the analysis involved a critical appraisal process of the studies according to the CASP tool to determine the methodological quality and to summarize findings (Table 2). Strong evidence was indicated by the availability of consistent findings in two or more high quality RCTs, moderate evidence by a high quality RCT, or two or more low quality RCTs. Limited evidence was indicated by cohort studies and case–control studies.
Table 2.
CASP Checklist for the studies included in the current systematic review
| Cho et al. [12] | Gage et al. [15] | Gage et al. [16] | Levinger et al. [29] | Mandeville et al. [32] | Mauer et al. [33] | McChesney and Woolacot [11] | Quagliarella et al. [43] | Schwartz et al. [45] | Swinkels et al. [54] | Swinkels et al. [53] | Viton et al. [57] | Yakdhani et al. [60] | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clearly focused issue | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Acceptable patient recruitment | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Randomized patient assignment | NA | ✓ | NA | ✓ | ✓ | NA | ✓ | NA | ✓ | ✓ | NA | NA | |
| Sample based on power calculation | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✓ | ✗ | ✗ |
| Patients fulfilled follow-ups | ✗ | ✓ | NA | ✓ | ✓ | NA | ✓ | ✓ | ✗ | ✗ | ✗ | ✓ | ✗ |
| Patients, examiners blinded | ✓ | ✗ | ✗ | ✗ | ✓ | NS | NS | ✗ | NA | ✓ | ✓ | NS | NS |
| Similarity of patients/groups | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | NA | ✓ | ✓ | ✓ | ✓ |
| Equal treatment of patients/groups | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Clearly specified outcome measures | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Large treatment effect | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✗ | ✗ | ✓ |
| Estimate treatment effect (CI) | ✓ | NS | NS | ✓ | ✗ | ✓ | ✗ | ✓ | ✗ | ✗ | NS | NS | NS |
| Appropriate results analysis | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Confounding factors listed | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ | ✗ | ✓ |
| Appropriate interpretation of results | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Generalization of results | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ |
| Applicable to clinical practice | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✗ | ✓ |
| Results coincide with relevant literature | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✗ | ✓ |
| Our evaluation | Reasonable. Short-term follow-up | Reasonable. Potential bias due to small sample size | Reasonable. Potential bias due to small sample size. | Good | Good | Good | Reasonable. CI not reported. | Outcome measures used not recommendable for TKA. | Reasonable. Potential bias due to large losses to follow-up | Reasonable. Considerable losses to follow-up | Reasonable. Potential bias due to small sample size | Reasonable. Potential bias due to small sample size | Reasonable. Potential bias due to small sample size |
All data extracted from the studies were analysed independently by each reviewer (MM and RP) and subsequently discussed. In any case of disagreement, further discussion was performed with a third reviewer (NG) to reach a mutual agreement.
Statistical analysis
Studies comparing static and dynamic balance pre- and post-TKA with comparable outcome measures were identified and pooled through a meta-analysis. Heterogeneity was assessed using the I2 measure. It was considered that I2<60 % was acceptable to pool data [21]. The statistical significance was considered at p < 0.05. Qualitative review of the evidence was performed when the studies could not be pooled.
Results
Search results
A total of 276 citations were identified by the search strategy, summarized in Fig. 1. Initially, 237 studies were eliminated because the title, abstract or keywords did not match the proposed theme. Of the 36 that remained, 22 were eliminated due to the non-English language used. Therefore, due to the other aforementioned exclusion criteria, 13 studies were deemed eligible and were finally included in the review.
Fig. 1.
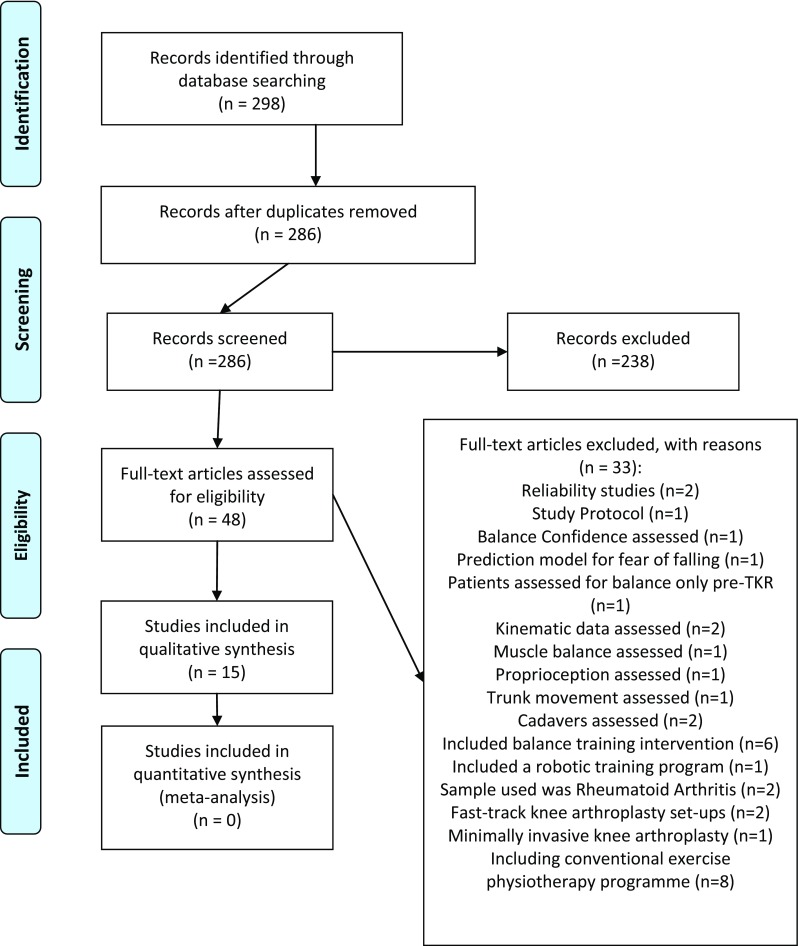
PRISMA Flow Diagram to depict search strategy results.
From: Moher D, Liberati A, Tetziaff J, Altman DG, The PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analysis: the PRISMA statement PLoS Med 6(6): e1000097. doi:10.137/journal.pmed1000097
Cohort characteristics
In all studies, patients had primary OA (grade III–IV according to the Kellgren and Lawrence system) and fulfilled criteria to undergo TKA. All knees were implanted with the same type of cemented prosthesis (unilaterally or bilaterally). No patellar component was inserted in any of the studies.
A description of the included studies, with the outcome measures used, the follow-up period and the clinically relevant findings is presented in Table 1.
Outcome measures
All studies used validated measures to assess balance parameters [48]. Functional stability limits, reactive control, control of balance during an active task, standing balance are all balance components being investigated in the studies, all linked with balance-related falls [29].
Regarding the incidence of falls after TKA, five studies included risk of falls assessment in addition to balance assessment [16, 29, 53, 54, 60]. One study used the short form of the Physical Profile Assessment (PPA) that encompasses five tests (proprioception, knee strength, postural sway in two directions and reaction time) to assess risk of falls [29].
Critical appraisal of studies’ methodological quality
Of the 13 studies included in the systematic review, 10 followed a cohort design (Level IIc), seven of which included a control group [11, 12, 29, 32, 43, 57, 60]. Three studies were observation case–control studies (Level III) [15, 16, 54]. The quality of the studies has been assessed as although all studies satisfied a similar number of criteria, their methodologies varied substantially.
All studies offered clearly defined research questions, population’ characteristics and methods of assessing balance (Table 2). In 5 studies [12, 45, 53, 54, 60], a number of participants were lost to follow-ups, implying potential bias. Only 3 studies had based their sample on a power calculation analysis [12, 53, 54]. In relation to interpretation, all studies discussed their findings based on current evidence. Generalization of findings was feasible in only 2 studies [12, 54], as in the other ones, either the sample size was not sufficient, or control group was absent.
Synthesis of results
Static balance post-TKA
Patients with TKA presented with 67 % less (p < 0.05) mean single-leg stance duration than that of healthy controls [33]. Postural sway in static single-limb stance was improved ~60 % 11 days after TKA compared to pre-surgery [12]. When balance was perturbed in a sagittal plane, no difference in balance control was observed between TKA patients and age-matched controls [15]. However, when balance was perturbed in the frontal plane, control of balance showed statistically significant impairment in TKA patients compared to controls [16].
Dynamic balance post-TKA
During a dynamic task, patients with bilateral TKA present with a mean obstacle avoidance success rate that was 32 % less than that of the control group [33]. During tasks such as stepping down, lateral steps, obstacle crossing, the success rate was increased after TKA. However, statistically significant conservative strategies (slower speed, shorter stride length, shorter base of support) (p < 0.05) were adopted resulting in increased duration of each task of up to 30 % [12, 32, 33, 45, 57].
Falls risk
After TKA, less than half (45.8 %) of pre-operative fallers continued to fall [54]. Patients who fell pre-operatively had an eightfold increase in the risk of post-operative falling [54]. A lower risk of falls was reported in 4 studies after surgery [29, 53, 54, 60]. In the PPA risk of falls, the only parameters that reached statistical significance were proprioception and knee extension strength 1-year post-surgery [29]. Balance confidence (ABC-UK) was significantly improved after TKA; however, results remained statistically significant (p < 0.001) only in patients with no history of falls pre-operatively [54]. Patients with higher ABC-UK pre-operatively reduced the odds of becoming a faller for up to 1 year post-operatively by 98 % (95 % CI 0.96–1.01, p = 0.04) [54]. Berg Balance Scale scores of fallers and non-fallers were similar both before and after TKA, although scores were improved more than the minimal detectable change (MDC) in 41 % of TKA patients [53].
Discussion
The most important finding of the present study was that TKA influences positively (a) fear of falling and incidence of falls by switching 54.2 % of pre-operative fallers to post-operative non-fallers and (b) balance for up to 1-year following surgery. The rationale for the study was that by analysing the available literature, an understanding might be promoted of how mechanisms controlling balance, compensate or respond after surgery, and in which timeline this occurs.
Thirteen studies fulfilled criteria that had been set and were ultimately used in the analysis. No study involving post-hospital discharge physiotherapy intervention or, any other type of rehabilitation training, which might otherwise confound the extent of the isolated influence of surgery was included in this review. Despite a large number of studies in this field, very few offered a high level of evidence (Level of evidence < IIc). The sample in the studies comprised of 652 individuals in total (167 being controls), with a mean age of 71.4 years; recruited patient’ characteristics were typical of middle-aged individuals undergoing TKA for knee OA and were therefore considered to be representative of TKA population. The methodological quality of the studies, as assessed by the CASP scale, was acceptable. However, due to variability in sampling procedure and the absence of power calculation analysis in most studies, external validity and therefore generalizability have been limited. Major drawbacks in the studies were the lack of randomization and the lack of a control group in some studies.
Regarding the balance effects found in most studies, there was a significant balance improvement (p < 0.001) in both tasks and confidence after TKA compared to the pre-operative state. While balance and sensori-motor performance were not fully restored after TKA, postural responses began to normalize in both quiet stance and dynamic tasks [32, 33, 57]. Static balance did not show a clear trend towards improvement [43]. Single-leg standing balance improved up to 60 % post-TKA, but remained poorer than age-matched controls for up to 1 year [12, 29, 33, 45, 57]. Dynamic and functional balance was found to be improved 6-month post-surgery but again not fully recovered compared to age-matched controls [32, 45, 53, 54, 60].
In studies investigating balance and postural control, the clinically relevant outcome would be patients’ reported falls. A 24.2 % post-operative falls rate for TKA patients was reported up to 1 year, which is less than current estimates (33 %) for community dwelling older people [53, 54]. The rate although reduced remained as high as 45.8 % for individuals identified as fallers prior to surgery. Nevertheless, there was a significant switch of fallers’ pre-TKA who became non-fallers after TKA (54.2 %) [54]. At least one fall in the first year post-TKA was recorded for 48 % of the surgical group compared with 30 % of the control group [29]. Following TKA, there was a 27 % reduction in the number of patients exceeding the cut-off point of 14 s in Timed Up and Go (TUG) [53, 54]. This time cut-off point has been proposed as a criterion for ruling out a high risk of falls in older adults [47]. Therefore, although the likelihood of falls seems to decrease after TKA, there is still a considerable amount of falls recorded post-TKA.
During TKA, the replaced knee is deprived from a variety of key proprioceptors, which have been resected (ACL, cartilage, menisci, etc.). Moreover, oscillations used by the knee joint to regulate postural control are unlikely to reach a detectable threshold by sensory receptors in the replaced knee [9]. Presumably, extra-capsular proprioceptors need to compensate for the loss, and in order to maintain stability and balance, albeit at reduced levels of capability [1, 58]. Different types of prostheses and retention of the PCL also have an impact in joint translation and mobility components [2, 4, 49]. However, different type of surgery techniques (posterior stabilization versus posterior cruciate ligament-retained) has shown contradictory findings on whether they influence balance and proprioception [3, 5, 52]. The addition of a patellar (prosthetic) component may further influence afferent sensory input; however, no relevant study was identified in the literature. Skinner et al. [49] suggested that the loss of proprioception due to arthritis was not improved by surgery. By contrast, Barrett et al. [4] claimed that when joint alignment and the ‘joint space height’ are reconstituted, the sense of position is improved, indicating that the reloading of lax collateral tissues at the time of the operation may be beneficial. Moreover, it has been shown that soft tissue balance (length-tension relationships for PCL and collateral ligaments) after surgery in both flexion and extension is important for allowing satisfactory post-operative knee proprioception [4]. Any difference in the tension of the medial and lateral collateral structures may therefore be perceived as a varus or valgus movement of the leg and may produce an antagonistic and corrective action from the hamstrings and quadriceps muscle groups, thus affecting proprioception [4]. Taking into account all the above literature, a number of factors could intrude as a result of surgery that could actually have an impact on patients’ neuro-sensory performance.
Bilateral postural responses after perturbation differ between TKA patients and age-matched controls. These differences are mostly observed in activation latency of muscles acting on the knee and in subsequent knee joint kinematics (reduced knee extension), suggesting a central postural re-organization process to protect against overly stressing the joint [15, 16, 32, 57, 60]. During walking, variability in knee kinematics is reduced and local dynamic stability again seems to be gradually restored [60]. Therefore, the mild improvements observed in balance following TKA may result from the retensioned capsuloligamentous structures and reduced pain and inflammation [52]. Patients post-operatively tend to normalize their weight distribution and develop more symmetrical posturomotor control.
Implications for clinical practice
Clinically, from a surgery perspective, correcting knee joint alignment and specifically varus deformity post-TKA has been shown to improve balance [12]. Considering the catastrophic consequences of peri-prosthetic fractures after a patients’ fall, 3D evaluations of the alignment and computer-assisted gap-balancing techniques, than conventional techniques of TKA, may produce more advantageous balance effect [26, 40]. The clinical relevance regarding rehabilitation is that patients’ training should involve rehabilitative strategies in static and dynamic tasks to achieve symmetrical weight distribution, implemented both pre- and post-TKA. Interestingly movement and weight distribution symmetry training, via the use of biofeedback, was recently introduced in the literature [62]. At the moment, there is only preliminary evidence to underpin the use of targeted sensori-motor elements within a physiotherapy programme [38]. Bilaterally observed impairments indicate that rehabilitation should include balance exercises involving both single- and double-leg stances to provoke overload and adaptation and prevent falls. Balance perturbation tasks can be more targeted towards frontal plane provocation and less in the sagittal plane [15, 16]. Moreover, knee strength and proprioception showed statistically significant improvement after TKA, whereas postural sway with eyes open and reaction time did not [29]. Finally, physiotherapy programmes should mostly incorporate the influential factors of falls (i.e. knee strength, proprioception and balance exercises with eyes closed).
Several limitations need to be considered when interpreting the findings of this review. Because of the methodological heterogeneity across the study designs (i.e. in methodological outcome measures and timing of measurements), results from a potential meta-analysis (with an I 2>85 %) would not have added consistency of evidence. Furthermore, due to methodological flaws across the studies, the level of evidence was not high enough to allow the generalization of results. More studies with robust methodologies are needed to investigate the effect of TKA on balance and falls incidence.
Conclusions
The findings of this systematic review provide moderate evidence to support that TKA influences balance positively for up to 1-year following surgery. Studies offering Level of evidence II showed up to 60 % improvement in standing balance as early as 11-day post-TKA. Moreover, TKA influences positively fear of falling and incidence of falls by switching 54.2 % of pre-operative fallers to post-operative non-fallers (Level of evidence II–III). Patterns of change (acute and chronic) and congruence amongst the interpretation of findings from the reviewed papers endorse a conceptual framework for the knee undergoing TKA surgery. The framework supports that knee extension strength, proprioception deficits and compensatory postural strategies are persisting after surgery and are acting as the potential factors contributing to why balance and falls might be linked and only partially restored after TKA.
Compliance with Ethical Standards
Conflict of Interest
No conflict of interest for any author exists.
Funding
This study was not funded.
Ethical approval
This is a systematic review so the ethical approval is not applicable.
Informed consent
This is a systematic review so the informed consent is not applicable.
References
- 1.Andriacchi TP. A functional analysis of pre and post-knee surgery: total knee arthroplasty and ACL reconstruction. J Biomech Eng. 1993;115(4B):575–581. doi: 10.1115/1.2895543. [DOI] [PubMed] [Google Scholar]
- 2.Attfield SF, Wilton TJ, Pratt DJ, Sambatakakis A. Soft-tissue balance and recovery of proprioception after total knee replacement. J Bone Joint Surg Br. 1996;78(4):540–545. [PubMed] [Google Scholar]
- 3.Baghdadi A, Abdallah A (2014) Dynamic Balance, Pain and Functional Performance in Cruciate Retaining, Posterior Stabilized and Unicompartmental Knee Arthroplasty. Paper presented at the 16th International conference on biomechanics and sports engineering, Kuala Lumpur, Malaysia, 13–14 June 2014
- 4.Barrett DS, Cobb AG, Bentley G. Joint proprioception in normal, osteoarthritic and replaced knees. J Bone Joint Surg Br. 1991;73(1):53–56. doi: 10.1302/0301-620X.73B1.1991775. [DOI] [PubMed] [Google Scholar]
- 5.Bascuas I, Tejero M, Monleón S, Boza R, MunIesa JM, Belmonte R. Balance 1 year after TKA: correlation with clinical variables. Orthopedics. 2013;36(1):6–12. doi: 10.3928/01477447-20121217-11. [DOI] [PubMed] [Google Scholar]
- 6.Brander V, Stulberg SD. Rehabilitation after hip- and knee-joint replacement. An experience- and evidence-based approach to care. Am J Phys Med Rehabil. 2006;85(11 Suppl):S98–118. doi: 10.1097/01.phm.0000245569.70723.9d. [DOI] [PubMed] [Google Scholar]
- 7.Byrne JM, Prentice SD. Swing phase kinetics and kinematics of knee replacement patients during obstacle avoidance. Gait Posture. 2003;18(1):95–104. doi: 10.1016/S0966-6362(02)00164-9. [DOI] [PubMed] [Google Scholar]
- 8.Cammarata ML, Schnitzer TJ, Dhaher YY. Does knee osteoarthritis differentially modulate proprioceptive acuity in the frontal and sagittal planes of the knee? Arthritis Rheum. 2011;63:2681–2689. doi: 10.1002/art.30436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cash RM, Gonzalez MH, Garst J, Barmada R, Stern SH. Proprioception after arthroplasty: role of the posterior cruciate ligament. Clin Orthop Relat Res. 1996;331:172–178. doi: 10.1097/00003086-199610000-00024. [DOI] [PubMed] [Google Scholar]
- 10.Chang QZ, Sohmiya M, Wada N, Tazawa M, Sato N, Yanagisawa S, Shirakura K. Alternation of trunk movement after arthroplasty in patients with osteoarthritis of the knee. J Orthop Sci. 2011;16(4):382–388. doi: 10.1007/s00776-011-0066-y. [DOI] [PubMed] [Google Scholar]
- 11.Chesney JM, Woolacott MH. The effect of age-related declines in proprioception and total knee replacement on postural control. J Gerontol. 2000;55(11):M658–M666. doi: 10.1093/gerona/55.11.M658. [DOI] [PubMed] [Google Scholar]
- 12.Cho SD, Hwang CH. Improved single-limb balance after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012;21(12):2744–2750. doi: 10.1007/s00167-012-2144-x. [DOI] [PubMed] [Google Scholar]
- 13.Duffell LD, Southgate DF, McGregor AH. Balance and gait adaptations in patients with early knee osteoarthritis. Gait Posture. 2014;39(4):1057–1081. doi: 10.1016/j.gaitpost.2014.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fitzgerald GK, Piva SR, Irrgang JJ. Reports of joint instability in knee osteoarthritis: its prevalence and relationship to physical function. Arthritis Care Res. 2004;51(6):941–946. doi: 10.1002/art.20825. [DOI] [PubMed] [Google Scholar]
- 15.Gage WH, Frank JS, Prentice SD, Stevenson P. Organisation of postural responses following a rotational support surface perturbation, after TKA: sagittal plane rotations. Gait Posture. 2007;25:112–120. doi: 10.1016/j.gaitpost.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 16.Gage WH, Frank JS, Prentice SD, Stevenson P. Postural responses following a rotational support surface perturbation following knee joint replacement: Frontal plane rotations. Gait Posture. 2008;27:286–293. doi: 10.1016/j.gaitpost.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 17.Gauchard GC, Vançon G, Meyer P, Mainard D, Perrin PP. On the role of knee joint in balance control and postural strategies: effects of total knee replacement in elderly subjects with knee osteoarthritis. Gait Posture. 2010;32(2):155–160. doi: 10.1016/j.gaitpost.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 18.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database. 2009;2:CD007146. doi: 10.1002/14651858.CD007146.pub2. [DOI] [PubMed] [Google Scholar]
- 19.Grabiner MD, Donovan S, Bareither ML, Marone JR, Hamstra-Wright K, Gatts S, Troy KL. Trunk kinematics and fall risk of older adults: translating biomechanical results to the clinic. J Electromyogr Kinesiol. 2008;18(2):197–204. doi: 10.1016/j.jelekin.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 20.Hassan BS, Doherty SA, Mockett S, Doherty M. Effect of pain reduction on postural sway, proprioception, and quadriceps strength in subjects with knee osteoarthritis. Ann Rheumatic Dis. 2002;61(5):422–428. doi: 10.1136/ard.61.5.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analysis. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hill KD, Williams SB, Chen J, Moran H, Hunt S, et al. Balance and falls risk in women with lower limb osteoarthritis or rheumatoid arthritis. JCGG. 2013;4(1):22–28. doi: 10.1016/j.apmr.2009.08.150. [DOI] [PubMed] [Google Scholar]
- 23.Hinman RS, Bennell KL, Metcalf BR, Crossley KM. Balance impairments in individuals with symptomatic knee osteoarthritis: a comparison with matched controls using clinical tests. Rheumatol (Oxford) 2002;41(12):1388–1394. doi: 10.1093/rheumatology/41.12.1388. [DOI] [PubMed] [Google Scholar]
- 24.Hunt MA, Birmingham TB, Bryant D, Jones I, Giffin JR, Jenkyn TR, Vandervoort AA. Lateral trunk lean explains variation in dynamic knee joint load in patients with medial compartment knee osteoarthritis. Osteoarthr Cartil. 2008;16(5):591–599. doi: 10.1016/j.joca.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 25.Khalaj N, Osman NA, Mokhtar AH, Mehdikhani M, Wan Abas WAB. Balance and risk of fall in individuals with bilateral mild and moderate knee osteoarthritis. PloS One. 2014;9(3):e92270. doi: 10.1371/journal.pone.0092270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim Y, Kim KI, Choi J, Lee K. Novel methods for 3D postoperative analysis of total knee arthroplasty using 2D–3D image registration. Clin Biomech (Bristol, Avon) 2011;26:384–391. doi: 10.1016/j.clinbiomech.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 27.Koralewicz LM, Engh GA. Comparison of proprioception in arthritic and age-matched normal knees. J Bone Joint Surg Am. 2000;82:1582–1588. doi: 10.2106/00004623-200011000-00011. [DOI] [PubMed] [Google Scholar]
- 28.Kul-Panza E, Berker N. Pedobarographic findings in patients with knee osteoarthritis. Am J Phys Med Rehabil. 2006;85(3):228–233. doi: 10.1097/01.phm.0000200377.52610.cd. [DOI] [PubMed] [Google Scholar]
- 29.Levinger P, Menz HB, Wee E, Feller JA, Barlett JR, Bergman NR. Physiological Risk factors for falls in people with knee osteoarthritis before and early after knee replacement surgery. Knee Surg Sports Traumatol Arthrosc. 2011;19:1082–1089. doi: 10.1007/s00167-010-1325-8. [DOI] [PubMed] [Google Scholar]
- 30.Lund H, Juul-Kristensen B, Hansen K, Christensen R, Christensen H, Danneskiold-Samsoe B, Bliddal H. Movement detection impaired in patients with knee osteoarthritis compared to healthy controls: a cross-sectional case-control study. J Musculoskelet Neuronal Interact. 2008;8:391–400. [PubMed] [Google Scholar]
- 31.Lyytinen T, Liikavainio T, Bragge T, Hakkarainen M, Karjalainen PA, Arokoski JP. Postural control and thigh muscle activity in men with knee osteoarthritis. J Electromyogr Kinesiol. 2010;20(6):1066–1074. doi: 10.1016/j.jelekin.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 32.Mandeville D, Osternig L, Chou LS. The effect of total knee replacement surgery on gait stability. Gait Posture. 2008;27:103–109. doi: 10.1016/j.gaitpost.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 33.Mauer AC, Louis BA, Draganich LF, Pandya N, Hofer J, Piotrowski GA. Bilateral total knee arthroplasty increases the propensity to trip on an obstacle. Clin Orthop Rel Res. 2005;433:160–165. doi: 10.1097/01.blo.0000150569.93262.64. [DOI] [PubMed] [Google Scholar]
- 34.Mcleland JA, Webster KE, Feller JA. Gait analysis of patients following total knee replacement: a systematic review. Knee. 2007;14(4):253–263. doi: 10.1016/j.knee.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 35.Messier SP, Royer TD, Craven TE, O’Toole ML, Burns R, Ettinger WH., Jr Long-term exercise and its effect on balance in older, osteoarthritic adults: results from the fitness, arthritis, and seniors trial (FAST) J Amer Geriatr Soc. 2000;48(2):131–138. doi: 10.1111/j.1532-5415.2000.tb03903.x. [DOI] [PubMed] [Google Scholar]
- 36.Mizner RL, Petterson SC, Clements KE, Zeni JA, Jr, Irrgang JJ, Snyder-Mackler L. Measuring functional improvement after total knee arthroplasty requires both performance-based and patient-reported assessments: a longitudinal analysis of outcomes. J Arthroplasty. 2011;26(5):728–737. doi: 10.1016/j.arth.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Morrow JR, Jackson AW, Disch JG, Mood DP. Measurement and evaluation in human performance. Champaign: Human Kinetics; 2010. pp. 301–302. [Google Scholar]
- 38.Moutzouri M, Gleeson N, Billis E, Panoutsopoulou I, Gliatis J. What is the effect of sensori-motor training on functional outcome and balance performance of patients’ undergoing TKR? Syst Rev Physiother. 2016;102(2):136–144. doi: 10.1016/j.physio.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 39.Nguyen US, Felson DT, Niu J, White DK, Segal NA, Lewis CE, Rasmussen M, Nevitt MC. The impact of knee instability with and without buckling on balance confidence, fear of falling and physical function: the Multicenter Osteoarthritis Study. Osteoarthritis Cartil. 2014;22(4):527–534. doi: 10.1016/j.joca.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pang HN, Yeo SJ, Chong HC, Chin PL, Ong J, Lo NN. Computer-assisted gap balancing technique improves outcome in total knee arthroplasty, compared with conventional measured resection technique. Knee Surg Sports Traumatol Arthrosc. 2011;19:1496–1503. doi: 10.1007/s00167-011-1483-3. [DOI] [PubMed] [Google Scholar]
- 41.Pap G, Meyer M, Weiler HT, Machner A, Awiszus F. Proprioception after total knee arthroplasty: a comparison with clinical outcome. Acta Orthop Scand. 2000;71(2):153–159. doi: 10.1080/000164700317413120. [DOI] [PubMed] [Google Scholar]
- 42.Park HJ, Ko S, Ok E, Lee JI. Factors related to standing balance in patients with knee osteoarthritis. Ann Rehab Med. 2013;17(3):373–378. doi: 10.5535/arm.2013.37.3.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Quagliarella L, Sasanelli N, Monaco V, Belgione G, Spinarelli A, Notarnicola A. Relevance of orthostatic posturography for clinical evaluation of hip and knee joint arthroplasty patients. Gait Posture. 2011;34:49–54. doi: 10.1016/j.gaitpost.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 44.Schmitt LC, Fitzgerald GK, Reisman AS, Rudolph KS. Instability, laxity, and physical function in patients with medial knee osteoarthritis. Phys Ther. 2008;88:1506–1516. doi: 10.2522/ptj.20060223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schwartz I, Kandel L, Sajina A, Litinezki D, Herman A, Mattan Y. Balance is an important predictive factor for quality of life and function after primary total knee replacement. J Bone Joint Surg Br. 2012;94-B:782–786. doi: 10.1302/0301-620X.94B6.27874. [DOI] [PubMed] [Google Scholar]
- 46.Sharma L, Pai YC, Holtkamp K, Rymer WZ. Is knee joint proprioception worse in the arthritic knee versus the unaffected knee in unilateral knee osteoarthritis? Arthritis Rheum. 1997;40:1518–1525. doi: 10.1002/art.1780400821. [DOI] [PubMed] [Google Scholar]
- 47.Shumway-Cook A, Brauer S, Woolacott M. Predicting the probability for falls in community-dwelling older adults using the timed up & go test. Phys Ther. 2000;80(9):896–903. [PubMed] [Google Scholar]
- 48.Sibley KM, Beauchamp MK, Van Ooteghem K, Straus SE, Jaglal SB. Using the systems framework for postural control to analyze the components of balance evaluated in standardized balance measures: a scoping review. Arch Phys Med Rehabil. 2015;96(1):122–132. doi: 10.1016/j.apmr.2014.06.021. [DOI] [PubMed] [Google Scholar]
- 49.Skinner HB, Barrack RL, Cook SB. Age-related decline in proprioception. Clin Orthop Relat Res. 1984;184:208–211. [PubMed] [Google Scholar]
- 50.Smith TO, King JJ, Hing CB. The effectiveness of proprioceptive-based exercise for osteoarthritis of the knee: a systematic review and meta-analysis. Rheumatol Int. 2012;32(1):3339–3351. doi: 10.1007/s00296-012-2480-7. [DOI] [PubMed] [Google Scholar]
- 51.Sorensen RR, Jørgensen MG, Rasmussen S, Skou ST. Impaired postural balance in the morning in patients with knee osteoarthritis. Gait Posture. 2014;39(4):1040–1044. doi: 10.1016/j.gaitpost.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 52.Swanik CB, Scott LM, Harry EM. Proprioception, kinesthesia and balance after total knee arthroplasty with cruciate-retaining and posterior stabilized prostheses. J Bone Joint Surg Am. 2004;86-A(2):328–334. doi: 10.2106/00004623-200402000-00016. [DOI] [PubMed] [Google Scholar]
- 53.Swinkels A, Allain T. Physical performance tests, self-reported outcomes, and accidental falls before and after total knee arthroplasty: an exploratory study. Physiother Theory Pract. 2013;29(6):432–442. doi: 10.3109/09593985.2012.755590. [DOI] [PubMed] [Google Scholar]
- 54.Swinkels A, Newman J, Allain T. A prospective observational study of falling before and after knee replacement surgery. Age Ageing. 2009;38:175–181. doi: 10.1093/ageing/afn229. [DOI] [PubMed] [Google Scholar]
- 55.Valtonen A, Pöyhönen T, Heinonen A, Sipilä S. Muscle deficits persist after unilateral knee replacement and have implications for rehabilitation. Phys Ther. 2009;89(10):1072–1079. doi: 10.2522/ptj.20070295. [DOI] [PubMed] [Google Scholar]
- 56.Van der Linden ML, Rowe PJ, Myles CM, Burnett R, Nutton RW. Knee kinematics in functional activities seven years after total knee arthroplasty. Clin Biomech (Bristol, Avon) 2007;22(5):537–542. doi: 10.1016/j.clinbiomech.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 57.Viton JM, Atlani L, Mesure S, Massion JP, Franceshi JP, Delarque A, Bardot A. Re-organisation of equilibrium and movement control strategies after total knee arthroplasty. J Rehab Med. 2002;34:12–19. doi: 10.1080/165019702317242659. [DOI] [PubMed] [Google Scholar]
- 58.Warren PJ, Olanlokun TK, Cobb AG, Bentley G. Proprioception after knee arthroplasty. The influence of prosthetic design. Clin Orthop Relat Res. 1993;297:182–187. [PubMed] [Google Scholar]
- 59.Williams SB, Brand CA, Hill KD, Hunt SB, Moran H. Feasibility and outcomes of a home-based exercise program on improving balance and gait stability in women with lower-limb osteoarthritis or rheumatoid arthritis: a pilot study. Arch Phys Med Rehabil. 2010;91(1):106–114. doi: 10.1016/j.apmr.2009.08.150. [DOI] [PubMed] [Google Scholar]
- 60.Yakhdani HR, Bafghi HA, Meijer OG, et al. Stability and variability of knee kinematics during gait in knee osteoarthritis before and after replacement surgery. Clin Biomech. 2010;25(3):230–236. doi: 10.1016/j.clinbiomech.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 61.Yoshida Y, Mizner RL, Ramsey DK, Snyder-Mackler L. Examining outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clin Biomech (Bristol, Avon) 2008;23(3):320–328. doi: 10.1016/j.clinbiomech.2007.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zeni J, Jr, Abujaber S, Flowers P, Pozzi F, Snyder-Mackler L. Biofeedback to promote movement symmetry after total knee arthroplasty: a feasibility study. J Orthop Sports Phys Ther. 2013;43(10):715–726. doi: 10.2519/jospt.2013.4657. [DOI] [PMC free article] [PubMed] [Google Scholar]


