Abstract
Background
Weight bias is an important clinical issue that the educators of tomorrow's healthcare professionals cannot afford to ignore. This study, therefore, aimed to pilot a randomized controlled trial of the effects of educational films designed to reduce weight stigmatization toward obese patients on trainee dietitians’ and doctors’ attitudes.
Methods
A pre-post experimental design with a 6-week follow-up, which consisted of an intervention group (n = 22) and a control group (n = 21), was conducted to assess the efficacy of brief anti-stigma films in reducing weight bias, and to test whether future, larger-scale studies among trainee healthcare professionals are feasible.
Results
Participants at baseline demonstrated weight bias, on both implicit and explicit attitude measures, as well as strong beliefs that obesity is under a person's control. The intervention films significantly improved explicit attitudes and beliefs toward obese people, and participant evaluation was very positive. The intervention did not significantly improve implicit anti-fat bias.
Conclusion
The current study suggests both that it is possible to conduct a substantive trial of the effects of educational films designed to reduce weight stigma on a larger cohort of trainee healthcare professionals, and that brief educational interventions may be effective in reducing stigmatizing attitudes in this population.
Key Words: Obesity, Stigma, Prejudice, Behavioural intervention, Film
Introduction
A quarter of UK adults have a BMI ≥ 30 kg/m2[1] and, if trends continue, it is estimated that by 2025 47% of men and 36% of women will be obese [2]. Healthcare professionals are, therefore, increasingly likely to come into contact with clients with obesity. Dietitians and general practitioners in particular are acknowledged by patients as having important roles in weight management [3,] and students training to become doctors and dietitians will be integral to the team of professionals responsible for directing the future management of obesity [4]. To do so effectively, they must be willing and able to engage empathically with overweight and obese people.
Obesity is a highly stigmatized condition associated with blame, and it is well established that obese people are subject to prejudice and bias as a consequence of their body weight [5,6]. Anti-fat attitudes have been reported in dietitians and even doctors specializing in obesity [e.g. [7,8,9], and, alarmingly, the next generation of dietitians and medics also appears to be affected [e.g. [10]. Attitudes are hypothetical constructs that can be thought of as a blend of beliefs and values which provide ready-made interpretations of, and reactions to, events and can predict behaviour [11,12]. Negative attitudes held by healthcare professionals may, therefore, influence their behaviour and have serious consequences for the clinical treatment of obese people, including avoidance of healthcare utilization [13,14] and the effectiveness of public health interventions [15]. A recent research synthesis highlighted a number of important ways in which attitudes of healthcare professionals can impact on the care obese patients receive. Healthcare professionals have been found to spend less time with obese patients, and there is evidence of discrimination in terms of treatment options and access to treatment, including preventive medicine. Negative attitudes can also impact on communications around obesity and patients’ willingness to engage in weight management [16].
Addressing weight bias as part of pre-registration training is essential because trainee healthcare professionals are developing attitudes that will influence their future conduct in both personal and professional realms [17]. Swift et al. [10] recently demonstrated that an appropriate target among UK trainee healthcare professionals would be their beliefs about the controllability of obesity. Such an approach is supported by attribution theory, which suggests that strong beliefs that obesity is due to a lack of personal control (and is therefore controllable) would result in weight bias [18], and is underpinned by a wide body of research [19]. Although there is a ‘striking paucity’ of research efforts to reduce weight bias, the majority of conducted attempts have been attribution-based [20]. To date, only four interventions have sought to improve beliefs and attitudes in trainee healthcare professionals by providing education about genetic and environmental factors associated with obesity as well as diet and exercise, either alone [21] or as part of multi-component interventions [22,23,24]. Although these interventions significantly improved beliefs about the causes of obesity [22,23,24] and attitudes toward obese people [21], they involved considerable resources and were found to be time-consuming: O'Brien et al. [21] required a trained facilitator, and students participated in 4 h of tutorials.
A recent systematic review of prejudice reduction strategies suggested that media interventions are promising areas for future research [25]. Given the power of audiovisual media to influence societal constructions of obesity [26] and the growing reputation of films as a useful, enjoyable, and impactful tool in behavioural medical education [27], short films may offer an alternative and inexpensive way of tackling anti-fat stigma in this population. Indeed, a study exploring the impact of anti-stigma films on medical students’ attitudes to serious mental illness and psychiatry showed promising results although recruitment difficulties resulted in a lack of statistical power [28].
This study, therefore, aimed to investigate the effects of two brief educational films, developed by the Rudd Center for Food Policy and Obesity to challenge negative attitudes to obesity, on UK medical and dietetic students’ weight bias. As recommended by Danielsdóttir et al. [20], a randomized study design was employed. The current study was conceived as a pilot and was run with the intention of testing whether all components of future, larger-scale studies in these populations, e.g. recruitment, randomization, treatment, and follow-up assessments, are feasible and compatible [29,30].
Methods
Sample
Nineteen students registered on the 4th year of the Master of Nutrition course (dietetic students) and 24 students registered on the 3rd year of the Bachelor of Medical Sciences course (medical students) at The University of Nottingham, UK, were recruited for the study.
Intervention and Control Films
Two 17-min films were shown during the intervention condition; ‘Weight Prejudice: Myths and Facts’ and ‘Weight Bias in Healthcare’ [31]. Both films have been developed by the Rudd Center for Food Policy and Obesity at Yale University, New Haven, CT, USA. ‘Weight Prejudice: Myths and Facts’ features Bene, a camcorder-toting teen who turns a class biology assignment into a lesson about weight prejudice. She opens up about her own personal experiences of being overweight and uses some expert commentary to counter common myths about the causes of obesity, e.g. that obesity is only caused by ‘eating too much and being lazy’. ‘Weight Bias in Healthcare’ is hosted by former supermodel and activist Emme and features expert commentary from professional obesity researchers as well as dramatic representation to address the bias and stigma that obese patients face in healthcare settings. This film aims to raise awareness of the sources and consequences of weight bias in healthcare. It provides a range of practical strategies to optimize the healthcare experience for obese patients, e.g. recognizing that being overweight is a product of many factors and that it is difficult to sustain significant weight loss. Both films employ several different strategies to promote stigma reduction, including i) attributions of weight controllability (e.g. communicating the complex etiology of obesity, of which individual behaviour is only one contributing factor); ii) empathy induction (e.g. showing viewers personal experiences of weight stigmatization and how it affects individuals), and iii) debunking weight-based stereotypes (e.g. directly challenging common weight-based stereotypes with scientific evidence and examples of obese persons whose behaviours are non-stereotypical). Development of the films was guided from empirical evidence regarding common public perceptions of weight-based stereotypes toward obese persons [6] as well as theoretical approaches that have been studied in the context of reduction of weight bias [19,32], with a primary emphasis on attribution theory [33,34], and to a lesser extent guidance from empathy induction techniques to promote empathic perspective-taking among viewers [35,36,37]. Both a youth and professional perspective were taken which was felt to be important for the current study as participants were in a process of transition: from young adults to practising healthcare professionals. The control film was a 34-min extract from an episode of a popular historical documentary series which was unrelated to body weight or food, but similarly educational and entertaining.
Outcome Measures
Fat Phobia Scale (F-scale) [38]: 14 pairs of adjectives are used to describe obese people (e.g. ‘lazy’ vs. ‘industrious’) and respondents are invited to indicate on a scale from 1 to 5 which adjective they feel best describes their beliefs about obese people. Responses were scored according to the instructions published by Bacon et al. [38] to give a possible range between 1 and 5, where higher scores indicate greater fat phobia. Based upon published data from a large general population, a score of 3.6 is considered to be an ‘average’ amount of fat phobia while a score of 4.4 (the 90th centile) would indicate a ‘high’ level of fat phobia [38]. Sample size in the current study (n ℋ 100) prevents assessment of internal consistency but previous research has demonstrated that the F-scale was reliable (Cronbach's alpha coefficient ≥ 0.7) in a sample of UK trainee healthcare professionals [10].
Beliefs about Obese People Scale (BOAP scale) [39]: 8 items measure beliefs about the controllability of obesity with items rated on a 6-point scale (−3 = I strongly disagree, +3 = I strongly agree). Responses were scored according to the instructions published by Allison et al. [39] to give a possible range between 0 and 48, where higher scores indicate a stronger belief that obesity is not under an obese person's control. Previous research has demonstrated that the F-scale was internally consistent (Cronbach's alpha coefficient ≥ 0.7) in a sample of UK trainee healthcare professionals [10].
The ‘Dislike’ and ‘Willpower’ subscales of the Anti-Fat Attitudes Questionnaire (AFA) [40]: The ‘Dislike’ subscale has 7 items and assesses an individual's explicit antipathy toward fat people (e.g. ‘I don't like fat people very much’). The ‘Willpower’ subscale has 3 items and assesses the belief that being overweight is a matter of personal control or lack thereof (e.g. ‘Fat people tend to be fat pretty much through their own fault’). Items are scored on a 10-point Likert scale (0 = ‘very strongly disagree’ to 9 = ‘very strongly agree’), summed and divided by the number of items used to create the subscale, giving a possible range between 0 and 9 [40]. In both cases higher scores indicate greater anti-fat bias. Previous research has demonstrated that the ‘Dislike’ and ‘Willpower’ subscales of the AFA were internally consistent (Cronbach's alpha coefficient ≥ 0.7) in a sample of Australian health promotion/public health students [21].
Bad/Good and Lazy/Motivated Implicit Associations Test (bad/good IAT and lazy/motivated IAT) [7,41]: A paper-based reaction time measure of automatic memory-based associations which asks participants to classify words into the following target category pair: ‘fat people’ versus ‘thin people’. Simultaneously, the tasks require categorization of words into one of the following descriptor category pairs: ‘good’ versus ‘bad’ (attitude measure) or ‘motivated’ versus ‘lazy’ (stereotype measure). Thus, participants completed the classification exercise both when the category pairings matched and mismatched expected associations. Participants are given 20 s to classify as many words as possible on each page. Stimuli are expected to be classified more easily when the target and descriptor category pairings match the participant's automatic, implicit associations. The variable of interest is the difference in the number of correctly classified items under the two different category pairings. A score above the neutral point (i.e. greater than 4) is considered to indicate anti-fat bias, while a score of less than 4 is considered to indicate pro-thin bias [7]. Previous research demonstrates that the IAT has predictive validity [42] as well as acceptable internal consistency and test-retest reliability [43].
Procedure
Students were given a brief description of the study during a scheduled lecture and invited to email their expression of interest to a member of the research team. On receipt, potential participants received a personalized invitation letter, a copy of the information sheet, and a consent form. As with previous studies of weight bias [10,44], the purpose of the study was withheld from participants to reduce possible social desirability bias although, as recommended by Arain et al. [45], participants were informed that they would be participating in a pilot study. Therefore, the present study was described to potential participants as ‘… a project investigating the feasibility of using short films about obesity management to support students training to become doctors or dietitians’. All responses remained confidential and students were assured that their participation or not would have no impact on any assessments. By way of a small token of appreciation participants were offered a £15 book voucher on completion of the study. This study received approval from the Nottingham University Medical School Ethics Committee.
The present study employed a single-masked, randomized control trial. To ensure similar numbers of participants in both the intervention and control groups, participants were allocated using a block randomization method [46]. At baseline, a self-completed questionnaire was used to collect data on the six outcome measures (F-scale, BOAP scale, AFA ‘Dislike’ subscale, AFA ‘Willpower’ subscale, bad/good IAT, lazy/motivated IAT), sociodemographic variables (age, gender), anthropometrics (self-reported weight and height, weight perceptions), and personal experience of weight-based teasing or prejudice/unfair treatment. Those randomized to the intervention group then watched the two anti-stigma films while those randomized to the control group watched the documentary extract. The six outcome measures were repeated immediately after viewing the intervention or control film(s). In addition, participants in the intervention group were asked to indicate ‘How useful do you think the films are to your training?’ by using a Likert scale from 1 = ‘Very useful’ to 5 = ‘not useful’ and to respond to three open-ended questions: ‘Which of the two films had more impact on your attitude towards obese people? Why?’, ‘What did you like about the films?’, ‘Was there anything in particular that you disliked about the films?’ Six weeks after the intervention, all participants were asked to complete four outcome measures (F-scale, BOAP scale, AFA ‘Dislike’ subscale, AFA ‘Willpower’ subscale) as part of an online survey.
Data Analysis
Data were double entered by two members of the research team, screened for missing values and univariate outliers [47,] and assessed for normality using Shapiro-Wilk's test. Data were analysed on an intention-to-treat basis, with repeated measures ANOVA followed by post-hoc independent and paired samples t-tests employed for parametric data, and for non-parametric data, Friedman tests followed by post-hoc independent Mann-Whitney U and Wilcoxon matched-pairs tests. All data analyses were conducted using IBM SPSS Statistics 19 (SPSS Inc., Chicago, IL, USA) by a researcher masked to allocation by status. Significance was taken as p ℋ 0.05.
Results
Sample Characteristics
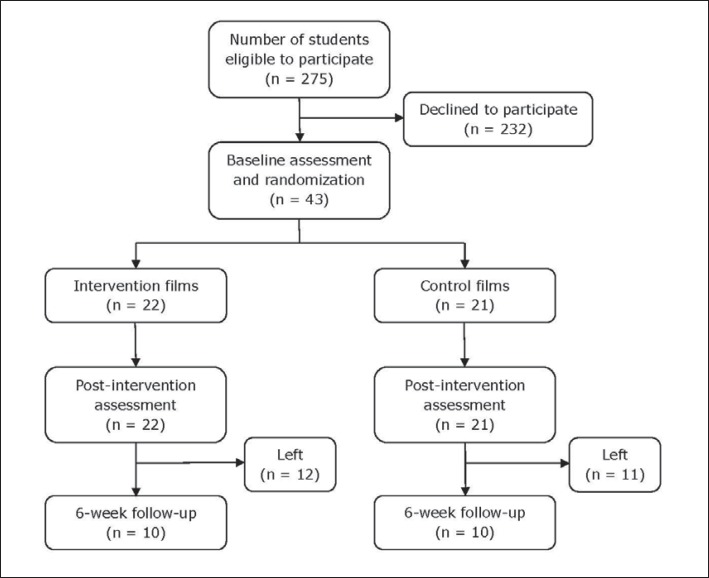
Of the 275 students eligible to participate, 43 (15.6%) took part. 22 students were allocated to the intervention group and 21 to the control group (fig. 1). On average, participants reported a healthy BMI (mean (SD) = 21.9 (3.4) kg/m2) but over a third had experienced weight-related teasing (n = 17; 39.5%). All participants perceived themselves to be in an appropriate weight category. There were no significant differences between the study groups in terms of gender or age, although participants in the intervention group were significantly more likely to be registered on the dietetics course and have a higher BMI than those in the control group (table 1).
Fig. 1.
Study profile.
Table 1.
Number of participants and demographics by study group
| Control | Intervention | |
|---|---|---|
| Sample size | 21 | 22 |
| Gender | ||
| Male | 3 (14.3%) | 4 (18.2%) |
| Female | 18 (85.7%) | 18 (81.8%) |
| Course | ||
| Dietetics | 5 (23.8%) | 14 (63.6%) |
| Medicine | 16 (76.2%) | 8 (36.4%)** |
| Mean age, years (SD) | 21.2 (0.8) | 24.6 (7.2) |
| Mean BMI, kg/m2 (SD) | 20.7 (1.7) | 23.2 (4.1)* |
Significant between-group difference at p <0.05.
Significant between-group difference at p <0.01.
Twenty participants from the original sample completed the 6-week follow-up (attrition rate = 53.5%); 10 from the intervention group and 10 from the control group. There were no significant differences in gender, course, or BMI between those who participated in the 6-week follow-up and those who did not.
F-Scale
At baseline, participants in both groups demonstrated above ‘average’ levels of fat phobia, as defined by Bacon and colleagues [38] (F-scale score mean (SD) = 3.9 (0.4) vs. 3.6 (0.6)). A repeated measure ANOVA exploring F-scale scores over time by group showed significant main effects for F-scale scores over time (F(1.75, 71.68) = 18.70; p ≤ 0.001) and group (F(1.41) = 16.93; p ≤ 0.001), as well as a significant time-by-group interaction (F(1.75, 71.68) = 8.73; p = 0.001). Post-hoc independent t-tests demonstrated significant between-group differences in F-scale score at all three time points (table 2). Post-hoc paired samples t-tests revealed that F-scale scores were significantly reduced between baseline and post-intervention in the intervention group, indicating less weight bias (t(21) = 6.049; p ℋ 0.001), but there was no difference in F-scale scores between baseline and the 6-week follow-up. No significant changes in F-scale scores between time points were apparent in the control group.
Table 2.
Outcome measure scores (mean (SD)) by study group at baseline, post-intervention, and 6-week follow-upa
| Control | Intervention | Cohen's d | |
|---|---|---|---|
| F-scale score | |||
| Baseline | 4.0 (0.5) | 3.7 (0.3)* | |
| Post-intervention | 3.9 (0.5) | 3.2 (0.3)*** | 1.69 |
| 6-week follow-up | 4.0 (0.5) | 3.6 (0.4)** | 1.32 |
| BOAP scale score | |||
| Baseline | 11.4 (4.0) | 11.2 (4.0) | |
| Post-intervention | 11.7 (3.7) | 19.9 (6.5)*** | 1.55 |
| 6-week follow-up | 11.0 (4.0) | 13.7 (6.9) | 0.51 |
| AFA ‘Dislike’ subscale score | |||
| Baseline | 2.39 (1.52) | 1.86 (1.43) | |
| Post-intervention | 2.15 (1.48) | 1.45 (1.16) | 0.52 |
| 6-week follow-up | 2.54 (1.50) | 1.57 (1.38)* | 0.74 |
| AFA ‘Willpower’ subscale score | |||
| Baseline | 5.78 (1.57) | 5.42 (1.84) | |
| Post-intervention | 5.94 (1.69) | 3.88 (1.95)** | 1.12 |
| 6-week follow-up | 5.76 (1.56) | 4.64 (1.84)* | 0.65 |
| Bad/good IAT score | |||
| Baseline | 5.0 (3.25) | 3.8 (4.36) | |
| Post-intervention | 2.7 (4.91) | 2.7 (3.33) | 0.26 |
| Lazy/motivated IAT score | |||
| Baseline | 6.7 (3.62) | 4.5 (4.96) | |
| Post-intervention | 5.4 (3.89) | 2.6 (4.19)* | 0.69 |
Sample sizes during baseline and post-intervention data collection = 22 for intervention group and 21 for control group. Sample sizes during 6-week follow-up data collection = 10 for intervention group and 10 for control group. P values represent between-group differences at baseline, post-intervention, and 6-week follow-up. Between-group differences at 6-week follow-up were analysed on an intention-to-treat basis.
Significant difference at p <0.05.
Significant difference at p <0.01.
Significant difference at p <0.001.
BOAP Scale
At baseline, participants achieved a mean BOAP scale score of 11.3/48 (SD = 4.0), suggesting strong beliefs that obesity is under a person's control. A repeated measure ANOVA exploring BOAP scale scores over time by group showed significant main effects for BOAP scale scores over time (F(1.73, 70.74) = 24.77; p ≤ 0.001) and group (F(1.41) = 7.38; p = 0.01), and a significant time-by-group interaction (F(1.73, 70.74) = 20.63; p ≤ 0.001). Post-hoc independent t-tests demonstrated significant between-group differences in BOAP scale score at the post-intervention time point only (table 2). Post-hoc paired samples t-tests revealed that in the intervention group BOAP scale scores significantly increased between baseline and post-intervention (t(21) = −7.868; p ℋ 0.001), suggesting that participants in the intervention group were significantly less likely to believe that obesity is under an obese person's control as a result of watching the anti-stigma films. This increase was sustained between baseline and 6-week follow-up (t(21) = −2.512; p ℋ 0.05). No significant changes in BOAP scale scores between time points were apparent in the control group.
AFA ‘Willpower’ Subscale
At baseline, participants achieved a mean AFA ‘Willpower’ subscale score of 5.6 (SD = 1.7). A repeated measure ANOVA exploring AFA ‘Willpower’ subscale scores over time by group showed significant main effects for AFA ‘Willpower’ subscale scores over time (F(2.82) = 6.78; p = 0.002) and group (F(1.41) = 5.88; p = 0.02), and a significant time-by-group interaction (F(2.82) = 10.178; p ℋ 0.001). There was no significant difference in scores at baseline but the intervention had lower scores than the control at both post-intervention (mean (SD): 3.88 (1.95) vs. 5.94 (1.69)) and 6-week follow-up (mean (SD): 4.64 (1.84) vs. 5.76 (1.56)) (table 2).
AFA ‘Dislike’ Subscale
At baseline, participants achieved a mean AFA ‘Dislike’ subscale score of 2.1 (SD = 1.5). AFA ‘Dislike’ subscale scores had a non-Gaussian distribution necessitating the use of non-parametric ANOVA (Friedman test). Mann-Whitney U tests demonstrated significant AFA ‘Dislike’ subscale scores between groups at the 6-week follow-up only (table 2), with the intervention group having lower levels of anti-fat bias. Friedman test revealed significant changes over time in the intervention group (χ2 = 6.029; p ℋ 0.05) but not in the control group. Post-hoc Wilcoxon matched-pairs tests revealed that in the intervention group AFA ‘Dislike’ subscale scores were significantly reduced between baseline and post-intervention (Z = −2.134; p ℋ 0.05) but not between baseline and 6-week follow-up. No significant changes in AFA ‘Dislike’ subscale scores between time points were apparent in the control group.
‘Bad/Good’ and ‘Lazy/Motivated’ IAT Scores
At baseline, participants achieved a mean ‘bad/good’ IAT score of 4.4 (SD = 3.9) and a mean ‘lazy/motivated’ IAT score of 5.5 (SD = 4.5), indicating implicit anti-fat bias as defined by Teachman and Brownell [7]. A repeated measure ANOVA exploring ‘bad/good’ and ‘lazy/motivated’ IAT scores over time-by-group showed significant main effects over time (F(1.41) = 10.98; p ℋ 0.01 and F(1.41) = 4.83; p ℋ 0.05, respectively) but no group effects and no significant time by group interactions. This may have reflected lack of statistical power to demonstrate an interaction effect as the intervention group did have better scores for lazy/motivated IAT scores (t = −2.29; df = 41; p = 0.027) than the control group post intervention.
Participant Evaluation of the Intervention
Of the 20 participants in the intervention group who responded to the question ‘How useful do you think the films are to your training?’, just over a third (35%) rated the videos as ‘useful’ or ‘very useful’, while 55% rated them as ‘a little useful’ or ‘neutral’ and 10% rated them as ‘not useful’. In response to the open question ‘What did you like about the films?’, comments from participants in the intervention group supported the focus on anti-fat stigma: ‘Got over right message’. Comments also supported the use of films as a mode of intervention: ‘Kept my attention and gave facts and figures’, ‘Short and to the point’, ‘Interesting, varied, personal’, and ‘ … playful … not boring …’ Opinion was divided as to film preference; some participants preferred the film ‘Weight Prejudice: Myths and Facts’ as it was more ‘personal’ and ‘emotive’ while others preferred ‘Weight Bias in Healthcare’ as it was more ‘objective’.
Responses to the question ‘Was there anything in particular that you disliked about the films?’ included concerns as to the extent to which the intervention films provided a balanced view of obesity's causes: ‘Only one side of the story. In some cases obesity probably does result from poor diet and inactivity’. In addition, there was felt to be a lack of practical advice on improving negative attitudes and on how to balance clinical effectiveness with patients’ needs: ‘More on how doctors can change their attitudes’, and ‘ … there could be more emphasis on how to create a constructive and supportive environment in which to help patients lose weight rather than just how to make them feel better. Reducing weight bias is important, hand on (sic) hand with an improvement in health’. Several participants suggested that they did not feel fully engaged with the scenarios as they featured only North American accents and healthcare systems: ‘British ones would have been interesting to see’.
Discussion
This research revealed weight bias among participants at baseline, on both implicit and explicit attitude measures, as well as strong beliefs that obesity is under a person's control. This is consistent with findings from previous studies investigating attitudes of practicing and trainee healthcare professionals toward obese people [e.g. [7,8,9,10]. The negative attitudes displayed by the trainee dietitians and doctors who participated in this study are of concern as they may have serious consequences for obese patients when they qualify and enter professional roles [13,14,15,16]. As a quarter of Britons are currently obese [1], weight bias is clearly an important clinical issue that the educators of tomorrow's healthcare professionals cannot afford to ignore.
The current study, however, indicates that brief, educational films may provide a feasible method of improving trainee healthcare professionals’ beliefs about and attitudes toward obese people, even some time after viewing them. Measurements from the BOAP scale and AFA ‘Willpower’ subscale suggested that improvements in beliefs about controllability – the main theme of the intervention films – were sustained over a 6-week period; an effect consistent with previous, more resource-intensive attribution-based intervention studies in medical [22] and kinesiology students [23,24]. Furthermore, explicit anti-fat bias – as measured by the F-scale and AFA ‘Dislike’ subscale – improved transiently. Therefore, this is the first study to demonstrate that short films might offer a novel, alternative way of tackling negative attitudes in this population. Once production costs have been met, short films can be made widely available for little or no cost, making this a relatively inexpensive mode of intervention.
It is, however, notable that improvement in explicit anti-fat bias was not sustained and that the intervention did not significantly improve implicit anti-fat bias – as measured by the IAT. This finding is consistent with the majority of previous intervention studies [20], although O'Brien et al. [21] have recently demonstrated that is it is possible to modify implicit and explicit anti-fat prejudice among health promotion/public health students by using a curriculum-based attribution intervention.
One explanation for the lack of sustained improvement in explicit anti-fat bias is derived from the Elaboration Likelihood Model which suggests that stronger, more stable attitude change will result from messages that are processed centrally [48]. Participant evaluation of the intervention was very positive but, arguably, participants were not encouraged to engage in in-depth analysis and integration of the information presented. Attitudes may, therefore, have only been influenced by superficial aspects of the message, e.g. source attractiveness and credibility. Future interventions employing short films may, therefore, benefit from the addition of a component which provides a meaningful motivation to process and understand the information, such as the use of guided discussions and summative assessments used by O'Brien et al. [21]. Alternatively, guided self-reflections might usefully be incorporated into the film to avoid the need for trained facilitators and to keep costs to a minimum.
An alternative explanation for the lack of sustained improvement in explicit anti-fat bias is that in the current study, assessments were conducted immediately before and after viewing the films – a period of approximately 35 min. This timing might have important implications in terms of vulnerability to demand characteristics [49], e.g. where participants viewing the anti-stigma films may report more favourable attitudes merely by virtue of remembering their scores and feeling they should report more positive attitudes. Although, as discussed by Gapinski et al. [50], demand-driven change may not be an undesirable outcome for prejudice reduction strategies, future research studies may wish to collect baseline data several days before showing participants the anti-stigma films and employing a simple cross-over study design.
The present study employed both implicit and explicit outcome measures. Although some authors consider both implicit and explicit attitude measures to be valid assessments of a given person's evaluation, albeit reflecting different components of the attitude response [51,] others consider assessment of implicit attitudes to be superior as they reflect evaluations that people are either unwilling or unable to report [52]. One explanation for the lack of improvement in implicit anti-fat bias as measured by the IAT is a lack of power. Retrospective power calculations indicated that the current study clearly did not have a sufficient sample size to detect a significant difference on the IAT (784 in each group for the bad/good IAT, and 368 in each group for the lazy/motivated IAT (p ℋ 0.05; β = 0.1)); partially a result of high standard deviations, relative to their means. Although the IATs appear to produce fairly consistent findings in the literature [20], levels of uncertainty of the magnitude observed here may indicate that these tests are not appropriate for this population. The psychometric properties of the IATs should, therefore, be explored further before inclusion as outcome measures in future full-scale studies. Future studies may also benefit from direct assessment of anti-fat behaviour [19,20] rather than reliance on implicit and explicit attitudes as proxies for discriminating behaviour.
Given the relative stability of attitudes [49] and the pervasiveness of anti-fat attitudes [5,6], it is widely recognized that interventions combining multiple attitude-change strategies may be needed to tackle the complexities of obesity stigma and translate into less biased behaviour [19,21]. The results of brief, educational films may be a useful component of future multi-component interventions. However, it is crucial that future studies are designed in such a way that they allow discrimination between the different bias reduction strategies, allowing effective individual components and/or combinations of components to be identified [19,20].
One other methodological issue that would need to be addressed in future studies is recruitment. This study employed an ‘opt-in’ method of recruitment and achieved a response rate of 15% which is somewhat lower than the 56% achieved by Kerby et al. [28] using similar methods. Furthermore, over half the participants (53.5%) were lost to follow-up. The study ran during the semester when potential participants were undertaking their own undergraduate research projects which may have made them reluctant to commit. Low response rates and high levels of attrition have important implications in terms of vulnerability to type II errors and selection bias. It is, however, important to recognize that well-conceived pilot studies will often not produce statistically significant results [30,45]. Furthermore, comparisons with existing data suggest that, at baseline, participants in the present study had similar levels of explicit weight bias as other populations of trainee healthcare professionals [10,] while those retained on the study did not differ significantly in gender, course, or BMI to those who were lost to follow-up. Future studies may wish to employ methods used by studies such as by O'Brien et al. [21], where data collection occurs as part of a compulsory in-class test with an ‘opt-out’ opportunity upon study completion. If such a strategy was employed, a simple cross-over study design would need to be employed to ensure that all students were given same the opportunities.
Although the quantitative rating of usefulness was low (just over a third rated the videos as ‘useful’ or ‘very useful’), the qualitative data collected as part of the current study suggested that the anti-stigma films were well accepted both in terms of content and as a mode of delivery. Although there were no negative comments about the interprofessional nature of the intervention or study design, there is clearly a need for future studies to develop films specific to the UK. Difficulties in understanding genetics and an overexposure to material in the media and wider society, suggesting that diet and physical activity are the primary causes and cures for obesity, have been cited as difficulties with attribution-based approaches [20,] while the qualitative data collected as part of this study also suggest that future films would benefit from more balanced, evidence-based information about causality.
Conclusion
The current study revealed weight bias among trainee healthcare professionals, on both implicit and explicit attitude measures, as well as strong beliefs that obesity is under a person's control. The intervention did, however, significantly improve explicit attitudes and beliefs toward obese people, and participant evaluation was very positive. The current study clearly suggests that the effects of brief, educational films to improve trainee healthcare professionals’ attitudes toward obesity are worthy of further exploration in a full-scale randomized control trial.
Authors’ Contributions
All named authors made an active contribution to the conception and design of the study as well as analysis and interpretation of the data. In addition, all named authors made an active contribution to the drafting of the paper, critically reviewed its content, and have approved the final version submitted for publication.
Disclosure Statement
The authors declare that they have no conflict of interests.
Acknowledgement
This research was funded by the Division of Nutritional Sciences at The University of Nottingham.
References
- 1.Department of Health Health Survey for England – 2008 Trend Tables. 2009. www.ic.nhs.uk/pubs/hse08trends. Accessed February 8, 2013.
- 2.Foresight: Tackling Obesities: Future Choices – Project Report ed 2. 2007. www.bis.gov.uk/assets/bispartners/foresight/docs/obesity/17.pdf. Accessed February 8, 2013. [DOI] [PubMed]
- 3.Tham M, Young D. The role of the General Practitioner in weight management in primary care – a cross sectional study in General Practice. BMC Fam Pract. 2008;9:66. doi: 10.1186/1471-2296-9-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Institute for Health and Clinical Excellence NICE Clinical Guidance 43. Obesity Guidance on the Prevention, Identification, Assessment and Management of Overweight and Obesity in Adults and Children. 2006. www.nice.org.uk/nicemedia/pdf/CG43NICEGuideline.pdf. Accessed February 8, 2013. [PubMed]
- 5.Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9:788–905. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- 6.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity. 2009;17:941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 7.Teachman BA, Brownell KD. Implicit anti-fat bias among health professionals: is anyone immune? Int J Obesity. 2001;25:1525–1531. doi: 10.1038/sj.ijo.0801745. [DOI] [PubMed] [Google Scholar]
- 8.Harvey EL, Summerbell CD, Kirk SFL, Hill AJ. Dietitians' views of overweight and obese people and reported management practices. J Hum Nutr Diet. 2002;15:331–347. doi: 10.1046/j.1365-277x.2002.00385.x. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz MB, Chambliss HO, Brownell KD, Blair SN, Billington C. Weight bias among healthcare professionals specializing in obesity. Obes Res. 2003;11:1033–1039. doi: 10.1038/oby.2003.142. [DOI] [PubMed] [Google Scholar]
- 10.Swift JA, Hanlon S, El-Redy L, Puhl RM, Glazebrook C. Weight bias among UK trainee dietitians, doctors, nurses and nutritionists. J Hum Nutr Diet. 2012 doi: 10.1111/jhn.12019. DOI: 10.1111/jhn.12019. [DOI] [PubMed] [Google Scholar]
- 11.Fishbein M, Ajzen I. Belief, Attitude, Intention and Behaviour: An Introduction to Theory and Research. Reading: MA, Addison-Wesley; 1975. [Google Scholar]
- 12.Hogg MA, Vaughan GM. Social Psychology: An Introduction. Hemel Hempstead: Prentice Hall/Harvester Wheatsheaf; 1995. [Google Scholar]
- 13.Amy NK, Aalborg A, Lyons P, Keranen L. Barriers to routine gynecological cancer screening for White and African-American obese women. Int J Obes. 2006;30:147–155. doi: 10.1038/sj.ijo.0803105. [DOI] [PubMed] [Google Scholar]
- 14.Puhl R, Moss-Racusin CA, Schwartz MB. Internalization of weight bias: implications for binge eating and emotional well-being. Obesity. 2007;15:19–23. doi: 10.1038/oby.2007.521. [DOI] [PubMed] [Google Scholar]
- 15.Puhl R, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health. 2010;100:1019–1028. doi: 10.2105/AJPH.2009.159491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mold F, Forbes A. Patients' and professionals' experiences and perspectives of obesity in health-care settings: a synthesis of current research. Health Expect. 2011 doi: 10.1111/j.1369-7625.2011.00699.x. DOI: 10.1111/j.1369-7625.2011.00699.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ottenritter NW. Service learning, social justice, and campus health. J Am Coll Health. 2004;52:189–191. doi: 10.3200/JACH.52.4.189-192. [DOI] [PubMed] [Google Scholar]
- 18.Crandall CS, Reser AH. Attribution and weight-based prejudice. In: Brownell KD, Puhl RM, Schwartz MB, Rudd L, editors. Weight Bias: Nature, Consequences and Remedies. New York: The Guildford Press; 2005. pp. 83–96. [Google Scholar]
- 19.Puhl RM, Brownell KD. Psychosocial origins of obesity stigma: toward changing a powerful and pervasive bias. Obes Rev. 2003;4:213–227. doi: 10.1046/j.1467-789x.2003.00122.x. [DOI] [PubMed] [Google Scholar]
- 20.Danielsdóttir S, O'Brien KS, Ciao A. Anti-fat prejudice reduction: a review of published studies. Obes Facts. 2010;3:47–58. doi: 10.1159/000277067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.O'Brien KS, Puhl R, Latner JD, Mir AS, Hunter JA. Reducing anti-fat prejudice in preservice health students: a randomized trial. Obesity. 2010;18:2138–2144. doi: 10.1038/oby.2010.79. [DOI] [PubMed] [Google Scholar]
- 22.Wiese HJ, Wilson JF, Jones RA, Neises M. Obesity stigma reduction in medical students. Int J Obesity. 1992;16:859–868. [PubMed] [Google Scholar]
- 23.Rukavina PB, Weidong L, Shen B, Sun H. A service learning based project to change implicit and explicit bias toward obese individuals in kinesiology pre-professionals. Obes Facts. 2010;3:117–126. doi: 10.1159/000302794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rukavina PB, Li W, Rowell MB. A service learning based intervention to change attitudes toward obese individuals in kinesiology pre-professionals. Soc Psych Educ. 2008;11:95–112. [Google Scholar]
- 25.Paluck EL, Green DP. Prejudice reduction: what works? A review and assessment of research and practice. Annu Rev Psychol. 2009;60:339–367. doi: 10.1146/annurev.psych.60.110707.163607. [DOI] [PubMed] [Google Scholar]
- 26.McClure KJ, Puhl RM, Heuer CA. Obesity in the news: do photographic images of obese persons influence antifat attitudes? J Health Commun. 2011;16:359–371. doi: 10.1080/10810730.2010.535108. [DOI] [PubMed] [Google Scholar]
- 27.Alexander M. Cinemeducation. Oxford: Radcliffe; 2005. [Google Scholar]
- 28.Kerby J, Calton T, BiMambro B, Flood C, Glazebrook C. Anti-stigma films and medical students' attitudes towards mental illness and psychiatry: randomized controlled trial. Psychiatr Bull. 2008;32:345–349. [Google Scholar]
- 29.Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M, on behalf of the Medical Research Council Developing and evaluating complex interventions: new guidance. 2008. www.mrc.ac.uk/Utilities/Documentrecord/index.htm?d=MRC004871. Accessed February 8, 2013.
- 30.National Institute for Health Research Evaluation, Trials and Studies Coordinating Centre Glossary www.netscc.ac.uk/glossary/#glos8. Accessed February 8, 2013.
- 31. www.yaleruddcenter.org/what_we_do.aspx?id=254.
- 32.Puhl RM, Schwartz MB, Brownell KD. Impact of perceived consensus on stereotypes about obese people: a new approach for reducing bias. Health Psychol. 2005;24:517–525. doi: 10.1037/0278-6133.24.5.517. [DOI] [PubMed] [Google Scholar]
- 33.Crandall CS, Martinez R. Culture, ideology, and anti-fat attitudes. Pers Soc Psychol B. 1996;22:1165–1176. [Google Scholar]
- 34.Crandall CS, D'Anello S, Sakalli N, Lazarus E, Nejtardt GW, Feather NT. An attribution-value model of prejudice: anti-fat attitudes in six nations. Pers Soc Psychol B. 2001;27:30–37. [Google Scholar]
- 35.Batson CD, Ahmad NY. Using empathy to improve intergroup attitudes and relations. Soc Issues Policy Rev. 2009;3:141–177. [Google Scholar]
- 36.Batson CD, Polycarpou MP, Harmon-Jones E, Imhoff HJ, Mitchener EC, Bednar LL, Klein TR, Highberger L. Empathy and attitudes: can feelings for a member of a stigmatized group improve feelings toward the group? J Pers Soc Psychol. 1997;72:105–118. doi: 10.1037//0022-3514.72.1.105. [DOI] [PubMed] [Google Scholar]
- 37.Teachman BA, Gapinski KD, Brownell KD, Rawlins M, Jeyaram S. Demonstrations of implicit anti-fat bias: the impact of providing causal information and evoking empathy. Health Psychol. 2003;22:68–78. doi: 10.1037//0278-6133.22.1.68. [DOI] [PubMed] [Google Scholar]
- 38.Bacon JG, Scheltema KE, Robinson BE. Fat Phobia Scale revisited: the short form. Int J Obes. 2001;25:252–257. doi: 10.1038/sj.ijo.0801537. [DOI] [PubMed] [Google Scholar]
- 39.Allison DB, Basile VC, Yucker HE. The measurement of attitudes toward and beliefs about obese persons. Int J Eat Disorder. 1991;10:599–607. [Google Scholar]
- 40.Crandall CS. Prejudice against fat people: ideology and self-interest. J Pers Soc Psychol. 1994;66:882–894. doi: 10.1037//0022-3514.66.5.882. [DOI] [PubMed] [Google Scholar]
- 41.Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: the Implicit Association Test. J Pers Soc Psychol. 1998;74:1464–80. doi: 10.1037//0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- 42.Bessenoff G, Sherman J. Automatic and controlled components of prejudice toward fat people: evaluation versus stereotype activation. Soc Cognition. 2000;18:329–353. [Google Scholar]
- 43.Nosek BA, Greenwald AG, Banaji MR. Understanding and using the Implicit Association Test: II. Method variables and construct validity. Pers Soc Psychol B. 2005;3:166–180. doi: 10.1177/0146167204271418. [DOI] [PubMed] [Google Scholar]
- 44.Puhl R, Wharton C, Heuer C. Weight bias among dietetics students: implications for treatment practices. J Am Diet Assoc. 2009;109:438–444. doi: 10.1016/j.jada.2008.11.034. [DOI] [PubMed] [Google Scholar]
- 45.Arain M, Campbell MJ, Cooper CL, Lancaster GA. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol. 2010;10:67. doi: 10.1186/1471-2288-10-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lachin JM, Matts JP, Wei LJ. Randomization in clinical trials: conclusions and recommendations. Control Clin Trials. 1988;9:365–374. doi: 10.1016/0197-2456(88)90049-9. [DOI] [PubMed] [Google Scholar]
- 47.Tabachinck BG, Fidell LS. Using multivariate statistics. International Students Edition. ed 4. Boston: Allyn and Bacon; 2000. [Google Scholar]
- 48.Petty RE, Cacioppo JT. The elaboration likelihood model of persuasion. In: Berkowitz L, editor. Advances in Experimental Social Psychology. New York: Academic Press; 1986. pp. 123–205. [Google Scholar]
- 49.Oppenheim AN. Questionnaire Design, Interviewing and Attitude Measurement. ed 2. London: Continuum; 1992. [Google Scholar]
- 50.Gapinski KD, Schwartz MB, Brownell KD. Can television change anti-fat attitudes and behavior? J Appl Biobehav Res. 2006;11:1–28. [Google Scholar]
- 51.Greenwald AG, Banaji MR. Implicit social cognition: attitudes, self-esteem, and stereotypes. Psychol Rev. 1995;102:4–27. doi: 10.1037/0033-295x.102.1.4. [DOI] [PubMed] [Google Scholar]
- 52.O'Brien KS, Latner JD, Halberstadt J, Hunter JA, Anderson J, Caputi P. Do antifat attitudes predict antifat behaviors? Obesity. 2008;16:S87–S92. doi: 10.1038/oby.2008.456. [DOI] [PubMed] [Google Scholar]